Abstract
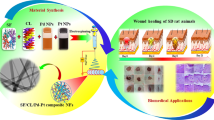
Different wounds take a while to heal, and the process is frequently accompanied by bacterial infection and scar formation. This study aimed to fabricate polyurethane (PU) fibers through electrospinning, utilizing a mixture of THF and DMF solvents in a 90:10 ratio. Subsequently, these fibers were coated with different concentrations of hyaluronic acid (HA) and silver (Ag) nanoparticles (NPs) using the hydrothermal treatment to create biocompatible and antibacterial scaffolds applicable to wound management. Pristine samples served as a basis for comparison. Following high-temperature usage during the hydrothermal coating, the Field emission scanning electron microscopy (FE-SEM) results showed defect-free morphology. However, the fibers’ diameter significantly increased by layer of HA. In particular, the diameter of the PU fibers was 1.87 ± 1.1 µm, whereas the fibers with the maximum amount of HA (0.5%) had an enlargement of 4.43 ± 1.4 µm in fiber diameter. The Fourier transform infrared (FTIR) spectroscopy demonstrated the presence of distinctive functional groups, supporting the hypothesis that HA and Ag NPs were efficaciously coated on PU fibers. Moreover, HA-coated fibers improved hydrophilicity, mechanical strength, thermal stability, degradability, and biomineralization. Notably, the Ag-coated scaffolds exhibited antibacterial activity against E. coli and S. aureus. The MTT assay, DAPI staining, and FE-SEM results after culturing HEK 293T cells have demonstrated the biocompatibility of the nanocomposite fibers. In other words, the developed HA and Ag NPs coated PU fibers by hydrothermal technique would be a futuristic method for promoting tissue healing and imparting antibacterial ability in curing skin wounds.















Similar content being viewed by others
References
Hussain Z, Thu HE, Shuid AN, Katas H, Hussain F (2017) Recent advances in polymer-based wound dressings for the treatment of diabetic foot ulcer: an overview of state-of-the-art. Curr Drug Targets 19(5):527–550. https://doi.org/10.2174/1389450118666170704132523
Sharifi S, Hajipour MJ, Gould L, Mahmoudi M (2021) Nanomedicine in healing chronic wounds: opportunities and challenges. Mol Pharm 18(2):550–575. https://doi.org/10.1021/ACS.MOLPHARMACEUT.0C00346/ASSET/IMAGES/LARGE/MP0C00346_0009.JPEG
Rather AH, Wani TU, Khan RS, Pant B, Park M, Sheikh FA (2021) Prospects of polymeric nanofibers loaded with essential oils for biomedical and food-packaging applications. Int J Mol Sci 22(8):4017. https://doi.org/10.3390/IJMS22084017
Jiang T, Carbone EJ, Lo KWH, Laurencin CT (2015) Electrospinning of polymer nanofibers for tissue regeneration. Prog Polym Sci 46:1–24. https://doi.org/10.1016/J.PROGPOLYMSCI.2014.12.001
Wang X, Ding B, Li B (2013) Biomimetic electrospun nanofibrous structures for tissue engineering. Mater Today 16(6):229–241. https://doi.org/10.1016/J.MATTOD.2013.06.005
Rahmati M et al (2021) Electrospinning for tissue engineering applications. Prog Mater Sci 117:100721. https://doi.org/10.1016/j.pmatsci.2020.100721
Gabriel LP, Rodrigues AA, Macedo M, Jardini AL, MacielFilho R (2017) Electrospun polyurethane membranes for tissue engineering applications. Mater Sci Eng C 72:113–117. https://doi.org/10.1016/j.msec.2016.11.057
Tetteh G, Khan AS, Delaine-Smith RM, Reilly GC, Rehman IU (2014) Electrospun polyurethane/hydroxyapatite bioactive Scaffolds for bone tissue engineering: The role of solvent and hydroxyapatite particles. J Mech Behav Biomed Mater 39:95–110. https://doi.org/10.1016/J.JMBBM.2014.06.019
Honarkar H (2017) Waterborne polyurethanes: a review. J Dispersion Sci Technol 39(4):507–516. https://doi.org/10.1080/01932691.2017.1327818
Mani MP, Jaganathan SK, Ismail AF (2019) Appraisal of electrospun textile scaffold comprising polyurethane decorated with ginger nanofibers for wound healing applications. J Ind Text 49(5):648–662. https://doi.org/10.1177/1528083718795911/ASSET/IMAGES/LARGE/10.1177_1528083718795911-FIG2.JPEG
Pant B, Park M, Ojha GP, Kim DU, Kim HY, Park SJ (2017) Electrospun salicylic acid/polyurethane composite nanofibers for biomedical applications. Int J Polym Mater Polym Biomater 67(12):739–744. https://doi.org/10.1080/00914037.2017.1376200
Lee MJ et al (2019) Curcumin-loaded biodegradable polyurethane scaffolds modified with gelatin using 3D printing technology for cartilage tissue engineering. Polym Adv Technol 30(12):3083–3090. https://doi.org/10.1002/PAT.4740
Kim SE et al (2009) Electrospun gelatin/polyurethane blended nanofibers for wound healing. Biomed Mater 4(4):044106. https://doi.org/10.1088/1748-6041/4/4/044106
Mistry P et al (2021) Fabrication and characterization of starch-TPU based nanofibers for wound healing applications. Mater Sci Eng C 119:111316. https://doi.org/10.1016/J.MSEC.2020.111316
Ahmadi P, Nazeri N, Derakhshan MA, Ghanbari H (2021) Preparation and characterization of polyurethane/chitosan/CNT nanofibrous scaffold for cardiac tissue engineering. Int J Biol Macromol 180:590–598. https://doi.org/10.1016/J.IJBIOMAC.2021.03.001
Dehghan-Manshadi N, Fattahi S, Hadizadeh M, Nikukar H, Moshtaghioun SM, Aflatoonian B (2019) The influence of elastomeric polyurethane type and ratio on the physicochemical properties of electrospun polyurethane/silk fibroin hybrid nanofibers as potential scaffolds for soft and hard tissue engineering. Eur Polym J 121:109294. https://doi.org/10.1016/J.EURPOLYMJ.2019.109294
Anilkumar TV, Muhamed J, Jose A, Jyothi A, Mohanan PV, Krishnan LK (2011) Advantages of hyaluronic acid as a component of fibrin sheet for care of acute wound. Biologicals 39(2):81–88. https://doi.org/10.1016/J.BIOLOGICALS.2011.01.003
Ebrahimi-Hosseinzadeh B et al (2016) In vivo evaluation of gelatin/hyaluronic acid nanofiber as burn-wound healing and its comparison with ChitoHeal gel. Fibers Polym 17(6):820–826. https://doi.org/10.1007/S12221-016-6259-4/METRICS
Törrönen K, Nikunen K, Kärnä R, Tammi M, Tammi R, Rilla K (2014) Tissue distribution and subcellular localization of hyaluronan synthase isoenzymes. Histochem Cell Biol 141(1):17–31. https://doi.org/10.1007/S00418-013-1143-4/FIGURES/9
Knopf-Marques H et al (2016) Hyaluronic acid and its derivatives in coating and delivery systems: applications in tissue engineering, regenerative medicine and immunomodulation. Adv Healthc Mater 5(22):2841–2855. https://doi.org/10.1002/ADHM.201600316
Xing F et al (2020) Hyaluronic acid as a bioactive component for bone tissue regeneration: Fabrication, modification, properties, and biological functions. Nanotechnol Rev 9(1):1059–1079. https://doi.org/10.1515/NTREV-2020-0084/ASSET/GRAPHIC/J_NTREV-2020-0084_FIG_005.JPG
Bazmandeh AZ, Mirzaei E, Ghasemi Y, Kouhbanani MAJ (2019) Hyaluronic acid coated electrospun chitosan-based nanofibers prepared by simultaneous stabilizing and coating. Int J Biol Macromol 138:403–411. https://doi.org/10.1016/J.IJBIOMAC.2019.07.107
Castro KC, Campos MGN, Mei LHI (2021) Hyaluronic acid electrospinning: challenges, applications in wound dressings and new perspectives. Int J Biol Macromol 173:251–266. https://doi.org/10.1016/J.IJBIOMAC.2021.01.100
Huerta-Angeles G et al (2016) Synthesis of photo-crosslinkable hyaluronan with tailored degree of substitution suitable for production of water resistant nanofibers. Carbohydr Polym 137:255–263. https://doi.org/10.1016/J.CARBPOL.2015.10.077
Xu X, Jha AK, Harrington DA, Farach-Carson MC, Jia X (2012) Hyaluronic acid-based hydrogels: from a natural polysaccharide to complex networks. Soft Matter 8(12):3280–3294. https://doi.org/10.1039/C2SM06463D
Deng Y et al (2014) Peptide-decorated polyvinyl alcohol/hyaluronan nanofibers for human induced pluripotent stem cell culture. Carbohydr Polym 101(1):36–39. https://doi.org/10.1016/J.CARBPOL.2013.09.030
Villarreal-Gómez LJ et al (2021) Antimicrobial effect of electrospun nanofibers loaded with silver nanoparticles: influence of Ag incorporation method. J Nanomater. https://doi.org/10.1155/2021/9920755
Umair Wani T et al (2023) Titanium dioxide functionalized multi-walled carbon nanotubes, and silver nanoparticles reinforced polyurethane nanofibers as a novel scaffold for tissue engineering applications. J Ind Eng Chem 121:200–214. https://doi.org/10.1016/J.JIEC.2023.01.024
Nqakala ZB, Sibuyi NRS, Fadaka AO, Meyer M, Onani MO, Madiehe AM (2021) Advances in nanotechnology towards development of silver nanoparticle-based wound-healing agents. Int J Mol Sci 22(20):11272. https://doi.org/10.3390/IJMS222011272
Phongtongpasuk S, Poadang S (2016) Green synthesis of silver nanoparticles using pomegranate peel extract. Adv Mater Res 1131:227–230. https://doi.org/10.4028/WWW.SCIENTIFIC.NET/AMR.1131.227
Abolhassani S, Alipour H, Alizadeh A, Nemati MM, Najafi H, Alavi O (2022) Antibacterial effect of electrospun polyurethane-gelatin loaded with honey and ZnO nanoparticles as potential wound dressing. J Ind Text 51(1 suppl):954S-968S. https://doi.org/10.1177/15280837211069871/ASSET/IMAGES/LARGE/10.1177_15280837211069871-FIG2.JPEG
Lee SJ et al (2014) Chitosan/polyurethane blended fiber sheets containing silver sulfadiazine for use as an antimicrobial wound dressing. J Nanosci Nanotechnol 14(10):7488–7494. https://doi.org/10.1166/JNN.2014.9581
Abdal-Hay A, Hamdy AS, Khalil KA (2015) Fabrication of durable high performance hybrid nanofiber scaffolds for bone tissue regeneration using a novel, simple in situ deposition approach of polyvinyl alcohol on electrospun nylon 6 nanofibers. Mater Lett 147:25–28. https://doi.org/10.1016/J.MATLET.2015.02.005
Abdal-Hay A, Salam Hamdy A, Morsi Y, Abdelrazek Khalil K, Hyun Lim J (2014) Novel bone regeneration matrix for next-generation biomaterial using a vertical array of carbonated hydroxyapatite nanoplates coated onto electrospun nylon 6 nanofibers. Mater Lett 137:378–381. https://doi.org/10.1016/J.MATLET.2014.09.034
Abdal-Hay A, Hussein KH, Casettari L, Khalil KA, Hamdy AS (2016) Fabrication of novel high performance ductile poly(lactic acid) nanofiber scaffold coated with poly(vinyl alcohol) for tissue engineering applications. Mater Sci Eng C 60:143–150. https://doi.org/10.1016/J.MSEC.2015.11.024
Rather AH et al (2023) Polyurethane and cellulose acetate micro-nanofibers containing rosemary essential oil, and decorated with silver nanoparticles for wound healing application. Int J Biol Macromol 226:690–705. https://doi.org/10.1016/J.IJBIOMAC.2022.12.048
Cui X et al (2008) Hyaluronan-assisted photoreduction synthesis of silver nanostructures: from nanoparticle to nanoplate. J Phys Chem C 112(29):10730–10734. https://doi.org/10.1021/JP8014029
Shamaila S et al (2016) Advancements in nanoparticle fabrication by hazard free eco-friendly green routes. Appl Mater Today 5:150–199. https://doi.org/10.1016/J.APMT.2016.09.009
Lamour G et al (2010) Contact angle measurements using a simplified experimental setup. J Chem Educ 87(12):1403–1407. https://doi.org/10.1021/ED100468U
Hasanzadeh E et al (2019) Preparation of fibrin gel scaffolds containing MWCNT/PU nanofibers for neural tissue engineering. J Biomed Mater Res Part A 107(4):802–814. https://doi.org/10.1002/JBM.A.36596
Kokubo T, Takadama H (2006) How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 27(15):2907–2915. https://doi.org/10.1016/J.BIOMATERIALS.2006.01.017
Mi HY, Jing X, Salick MR, Cordie TM, Peng XF, Turng LS (2014) Morphology, mechanical properties, and mineralization of rigid thermoplastic polyurethane/hydroxyapatite scaffolds for bone tissue applications: Effects of fabrication approaches and hydroxyapatite size. J Mater Sci 49(5):2324–2337. https://doi.org/10.1007/S10853-013-7931-3/FIGURES/13
Shamshi Hassan M et al (2013) Bimetallic Zn/Ag doped polyurethane spider net composite nanofibers: a novel multipurpose electrospun mat. Ceram. Int 39(3):2503–2510. https://doi.org/10.1016/J.CERAMINT.2012.09.009
Samie M, Khan AF, Hardy JG, Yameen MA (2022) Electrospun antibacterial composites for cartilage tissue engineering. Macromol Biosci 22(9):2200219. https://doi.org/10.1002/MABI.202200219
He X et al (2014) Uniaxially aligned electrospun all-cellulose nanocomposite nanofibers reinforced with cellulose nanocrystals: Scaffold for tissue engineering. Biomacromol 15(2):618–627. https://doi.org/10.1021/BM401656A/SUPPL_FILE/BM401656A_SI_001.PDF
Koosha M, Raoufi M, Moravvej H (2019) One-pot reactive electrospinning of chitosan/PVA hydrogel nanofibers reinforced by halloysite nanotubes with enhanced fibroblast cell attachment for skin tissue regeneration. Colloids Surf B Biointerfaces 179:270–279. https://doi.org/10.1016/J.COLSURFB.2019.03.054
Sheikh FA, Zargar MA, Tamboli AH, Kim H (2016) A super hydrophilic modification of poly(vinylidene fluoride) (PVDF) nanofibers: by in situ hydrothermal approach. Appl Surf Sci 385:417–425. https://doi.org/10.1016/J.APSUSC.2016.05.111
Yu M, Jambhrunkar S, Thorn P, Chen J, Gu W, Yu C (2012) Hyaluronic acid modified mesoporous silica nanoparticles for targeted drug delivery to CD44-overexpressing cancer cells. Nanoscale 5(1):178–183. https://doi.org/10.1039/C2NR32145A
Hu Y et al (2017) Biomimetic mineralized hierarchical hybrid scaffolds based on in situ synthesis of nano-hydroxyapatite/chitosan/chondroitin sulfate/hyaluronic acid for bone tissue engineering. Colloids Surf B Biointerfaces 157:93–100. https://doi.org/10.1016/J.COLSURFB.2017.05.059
Zhuo F, Abourehab MAS, Hussain Z (2018) Hyaluronic acid decorated tacrolimus-loaded nanoparticles: Efficient approach to maximize dermal targeting and anti-dermatitis efficacy. Carbohydr Polym 197:478–489. https://doi.org/10.1016/J.CARBPOL.2018.06.023
Hafezi M, Safarian S, Khorasani MT, Abu Osman NA (2016) Polyurethane/58S bioglass nanofibers: synthesis, characterization, and in vitro evaluation. RSC Adv 6(42):35815–35824. https://doi.org/10.1039/C5RA24786A
Choi Y, Nirmala R, Lee JY, Rahman M, Hong ST, Kim HY (2013) Antibacterial ciprofloxacin HCl incorporated polyurethane composite nanofibers via electrospinning for biomedical applications. Ceram Int 39(5):4937–4944. https://doi.org/10.1016/J.CERAMINT.2012.11.088
Unnithan AR et al (2012) Wound-dressing materials with antibacterial activity from electrospun polyurethane–dextran nanofiber mats containing ciprofloxacin HCl. Carbohydr Polym 90(4):1786–1793. https://doi.org/10.1016/J.CARBPOL.2012.07.071
Yan S et al (2019) Directed assembly of robust and biocompatible silk fibroin/hyaluronic acid composite hydrogels. Compos Part B Eng 176:107204. https://doi.org/10.1016/J.COMPOSITESB.2019.107204
Pan S-F, Ke X-X, Wang T-Y, Liu Q, Zhong L-B, Zheng Y-M (2018) Synthesis of silver nanoparticles embedded electrospun PAN nanofiber thin-film composite forward osmosis membrane to enhance performance and antimicrobial activity. Ind Eng Chem Res. https://doi.org/10.1021/acs.iecr.8b04893
Cakic SM, Stamenkovic JV, Djordjevic DM, Ristic IS (2009) Synthesis and degradation profile of cast films of PPG-DMPA-IPDI aqueous polyurethane dispersions based on selective catalysts. Polym Degrad Stab 94(11):2015–2022. https://doi.org/10.1016/J.POLYMDEGRADSTAB.2009.07.015
Nirmala R, Kalpana D, Navamathavan R, Lee YS, Kim HY (2013) Preparation and characterizations of silver incorporated polyurethane composite nanofibers via electrospinning for biomedical applications. J Nanosci Nanotechnol 13(7):4686–4693. https://doi.org/10.1166/JNN.2013.7192
Zarei M, Samimi A, Khorram M, Abdi MM, Golestaneh SI (2021) Fabrication and characterization of conductive polypyrrole/chitosan/collagen electrospun nanofiber scaffold for tissue engineering application. Int J Biol Macromol 168:175–186. https://doi.org/10.1016/J.IJBIOMAC.2020.12.031
Li Q, Li M, Zhu P, Wei S (2012) In vitro synthesis of bioactive hydroxyapatite using sodium hyaluronate as a template. J Mater Chem 22(38):20257–20265. https://doi.org/10.1039/C2JM33624C
Kalwar K, Hu L, Li DL, Shan D (2018) AgNPs incorporated on deacetylated electrospun cellulose nanofibers and their effect on the antimicrobial activity. Polym Adv Technol 29(1):394–400. https://doi.org/10.1002/PAT.4127
Silhavy TJ, Kahne D, Walker S (2010) The bacterial cell envelope. Cold Spring Harb Perspect Biol 2(5):a000414. https://doi.org/10.1101/CSHPERSPECT.A000414
Pazos-Ortiz E et al (2017) Dose-dependent antimicrobial activity of silver nanoparticles on polycaprolactone fibers against gram-positive and gram-negative bacteria. J Nanomater. https://doi.org/10.1155/2017/4752314
Sofi H, Akram T, Tamboli A (2021) journal of, and undefined 2019, Novel lavender oil and silver nanoparticles simultaneously loaded onto polyurethane nanofibers for wound-healing applications. Elsevier, Accessed Jan, 26 2021 https://www.sciencedirect.com/science/article/pii/S0378517319306350
Lu B et al (2017) In situ reduction of silver nanoparticles by chitosan-l-glutamic acid/hyaluronic acid: enhancing antimicrobial and wound-healing activity. Carbohydr Polym 173:556–565. https://doi.org/10.1016/J.CARBPOL.2017.06.035
Acknowledgements
This work was supported by the Science and Engineering Research Board (SERB) research grants (CRG/2020/000113). Anjum Hamid is grateful for Maulana Azad National Fellowship.
Author information
Authors and Affiliations
Contributions
AHR and FAS wrote the manuscript. RSK and TUW did the editing. MR and AQ did the characterization. SR supervised the work. HM, AHJ and SM did the analysis and helped to review the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rather, A.H., Khan, R.S., Wani, T.U. et al. Hydrothermal Modification of Polyurethane Fibers Using Hyaluronic Acid and Silver Nanoparticles for Wound Healing. J Polym Environ (2024). https://doi.org/10.1007/s10924-023-03146-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10924-023-03146-9