Abstract
Transition to the postanesthesia care unit (PACU) requires timely order placement by anesthesia providers. Computerized ordering enables automated order reminder systems, but their value is not fully understood. We performed a single-center, retrospective cohort study to estimate the association between automated PACU order reminders and primary outcomes (1) on-time order placement and (2) the degree of delay in placement. As a secondary post-hoc analysis, we studied the association between late order placement and PACU outcomes. We included patients with a qualifying postprocedure order from January 1, 2019, to May 31, 2023. We excluded cases transferred directly to the ICU, whose anesthesia provider was involved in the pilot testing of the reminder system, or those with missing covariate data. Order reminder system usage was defined by the primary attending anesthesiologist’s receipt of a push notification reminder on the day of surgery. We estimated the association between reminder system usage and timely order placement using a logistic regression. For patients with late orders, we performed a survival analysis of order placement. The significance level was 0.05. Patient (e.g., age, race), procedural (e.g., anesthesia duration), and provider-based (e.g., ordering privileges) variables were used as covariates within the analyses. Reminders were associated with 51% increased odds of order placement prior to PACU admission (Odds Ratio: 1.51; 95% Confidence Interval: 1.43, 1.58; p ≤ 0.001), reducing the incidence of late PACU orders from 17.5% to 12.6% (p ≤ 0.001). In patients with late orders, the reminders were associated with 10% quicker placement (Hazard Ratio: 1.10; 95% CI 1.05, 1.15; p < 0.001). On-time order placement was associated with decreased PACU duration (p < 0.001), decreased odds of peak PACU pain score (p < 0.001), and decreased odds of multiple administration of antiemetics (p = 0.02). An order reminder system was associated with an increase in order placement prior to PACU arrival and a reduction in delay in order placement after arrival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The successful transition of care from the operating room to the post-anesthesia care unit (PACU) requires comprehensive communication between anesthesia, nursing, and surgical teams in the form of verbal hand offs as well as orders placed by the anesthesia team for necessary PACU therapies. Computerized provider order entry (CPOE) systems are frequently used for electronic placement of such orders and provide an opportunity for implementation of automated electronic reminders to encourage timely order placement. Since delays in PACU order placement can lead to delays in patient care and resulting adverse events or costs to the healthcare system, this type of reminder holds potential for improving patient outcomes.
Numerous studies have demonstrated the positive implications of CPOE in different clinical practice environments, showing that effective implementation can result in reduced errors, direct savings to the healthcare system, improved patient safety and outcomes, and decreased response and turnaround times [1,2,3,4,5,6,7,8,9,10,11,12]. However, limited data are available to study the implications of CPOE systems in the PACU setting, and specifically how reminder systems might provide value in supporting compliance with timely PACU order placement.
To mitigate delays in PACU order placement, a mobile electronic health record (EHR) reminder system was implemented at our institution in 2021. This study's aim was to estimate the association between the PACU mobile reminder system and the timeliness of PACU order placement and the degree of delay in care. We hypothesized that implementation of this reminder system would result in a greater proportion of patients having orders placed prior to arrival in PACU and more rapid order entry for those who did not have orders placed prior to arrival. Secondarily, we also studied the association of late order entry with various PACU outcomes.
Methods
Study Design/Sample
We performed a retrospective observational analysis, including subjects with an anesthetic care record from our institution’s main operating rooms who received a qualifying postprocedure order from January 1, 2019, to May 31, 2023.It is possible that anesthesia providers anticipated ICU transfers for sicker patients with higher case urgency, and thus the normal clinical flow for these cases was altered. For this reason, we excluded subjects admitted directly from the operating room (OR) to the intensive care unit (ICU). We also excluded those whose primary anesthesia attending provider participated in the pilot testing of the reminder system, and those with missing covariate data. This study was approved with a waiver for written, informed consent from the Human Subjects Research Protections Program at Vanderbilt University Medical Center and adheres to the guidelines provided in the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) statement [13].
Variables
Mobile reminder system usage was determined based on the EHR audit log of 'OR Closing’ push notifications sent to providers opted into the system and was defined for each case as “positive” (i.e., a reminder was sent for this case) if the anesthesia provider received a relevant reminder on the same day as the surgical case. The alerts were implemented using Epic System’s Haiku application (Verona, WI) and were designed to deliver a push notification to the attending anesthesiologist’s smartphone or tablet if PACU orders were not placed by the time that surgical closure began. Providers could opt out of push notifications by adjusting their application settings, or by choosing to not install the Haiku application on their personal smartphone or tablet. The study's main outcomes were (1) the incidence of patients arriving in the PACU without orders and (2) the degree of delay in order placement for those patients without orders present on arrival. To analyze the latter, we created a two-part survival variable to define (1) did patient have their order placed within 90 min of PACU start (Yes/No) and (2) minutes from PACU start to order placement. Patients who did not have their order placed within the first 90 min of their stay in PACU were considered negative for PACU order placement (i.e., lost to follow-up). This follow-up period was selected based on the distribution of time from PACU start to order placement for cases with late orders. Secondary outcomes were defined as (1) total PACU length of stay (LOS) in minutes, (2) ≥ 2 administrations of PACU antiemetics (promethazine, ondansetron, or haloperidol), and (3) peak PACU pain score.
Data Collection Methods
Data on the relevant exposure, outcomes, and covariates were electronically extracted from Clarity, a relational database populated nightly from the EHR. Covariates included patient demographics (patient age, sex, self-reported race, height, and weight), procedural variables (American Society of Anesthesiologists’ [ASA] physical status classification, case level, and anesthesia duration), and three separate provider-based variables indicating if (1) the primary attending anesthesiologist ever changed, (2) the in-room provider ever changed, or (3) an in-room provider eligible to place orders was ever present during the case.
Data Analyses
Demographic and procedural variables were summarized with median and interquartile range for continuous variables and with counts and percentages for categorical variables. Univariate groupwise comparisons were performed using the Chi-Squared test for categorical variables and Kruskal-Wallis Rank Sum test for continuous variables.
We first tested the univariate association between the PACU mobile reminder system and the incidence of patients arriving in the PACU with orders. We then estimated this association, adjusting for patient, procedural, and provider-based covariates, using a logistic regression. Next, we filtered out patients who did not have their order placed prior to PACU start and used a Cox Proportional Hazards survival model to analyze the association between the reminder system and degree of additional delay in order placement. Odds ratios (ORs) with 95% confidence intervals (CIs) quantified the effect of PACU mobile reminder system usage on the odds of arrival in PACU with orders already placed. Hazard ratios (HR) with 95% CI were reported for the association between the mobile reminder and the hazard, or the instantaneous rate of order placement. For numeric covariates, odds/hazard ratios were calculated by taking the difference in odds/hazard between the 25th and 75th percentile of the variable. Survival curves were plotted to visualize the difference in survival rates across patients who did and did not utilize the reminder system. ANOVA was utilized to test the significance of model terms. The significance level for model terms was set at 5%. Optimism-corrected concordance statistics were reported as metrics of discriminative performance of each respective model (i.e., ability of model to accurately distinguish between patients with and without the outcome of interest). Calibration plot assessed the agreement between predicted and observed outcomes, corrected for optimism (i.e., adjustment for overfitting). Restricted cubic splines were utilized to relax the linearity assumption of continuous covariates. All analyses were performed with R (Version 4.1.2; R Core Team; Vienna, Austria) and libraries used include tidyverse, knitr, Hmisc, rms, tableone, RODBC, DBI, odbc, pROC, survival, survminer, ggpubr, car, and plotly.
Post-hoc Secondary Analysis
As a post-hoc secondary analysis, we assessed the association between order placement prior to PACU admission and secondary PACU outcomes (PACU duration, administration of antiemetics, and peak pain score). Due to its distribution, we performed a linear regression of a logarithmic transformation of the total PACU length of stay variable. Logistic regression was utilized to study the second administration of antiemetics, and a proportional odds logistic regression was used to study the ordered peak PACU pain score outcome.
Results
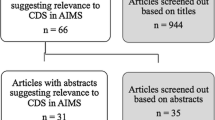
Of the 149,607 records that met our inclusion criteria, 11,257 cases went straight from the OR to the ICU, 10,841 cases had a primary attending who was involved in the initial pilot testing of the reminder system, and 662 cases were excluded for missing data (Fig. 1). There were thus 126,847 cases that were eligible for analysis. In 12.5% (n = 15,919) of cases, the primary attending provider received a push notification reminder on the day of surgery (Table 1). Overall, 88 (44.9%) attending providers received at least one ‘OR Closing’ push notification. Use of the mobile reminder system was associated with a reduced incidence of missing PACU orders on admission (12.6% vs. 17.5%; p < 0.001) and orders that were placed sooner on average (p < 0.001) (Table 2). The rate of order placement prior to PACU start was 83.2% (n = 105,485). Compared to those whose orders were late, cases with timely order placement had on average higher rates of mobile reminder system usage by the attending provider (13.2% vs. 9.4%; p < 0.001) (Table 3).
Association Between PACU Mobile Reminder Usage and the Incidence of Timely PACU Order Placement
Order reminder system usage had a univariate association with increased rate of order placement prior to PACU admission (p < 0.001). Adjusting for patient, procedural, and provider-based variables, we found that PACU mobile reminder system usage was associated with 51% increased odds (OR: 1.51; 95% CI: 1.43, 1.58; p < 0.001) of timely PACU order placement (Table 4). Overall, there was no evidence of model overfit, but it displayed poor discriminative ability (optimism-corrected concordance statistic = 0.58).
Association Between PACU Mobile Reminder Usage and Degree of Delay in Care
The records of 21,362 patients whose orders were not placed prior to PACU admission were analyzed to assess their degree of delay in order placement. There were 2,001 (9.4%) cases where the primary attending received a push notification on the day of surgery. Within this set of patients, usage of the PACU mobile reminder system was associated with 10% more rapid placement of a patient’s orders (HR: 1.10; 95% CI 1.05, 1.15; p < 0.001) (Table 5). Figure 2 shows that the delivery of a push notification reminder to the primary attending provider on the day of surgery was associated with reduced survival probability and, thus, were more likely to have order placement sooner than cases in which the primary attending did not receive a notification. The survival model displayed low corrective optimism adjustment for model performance (i.e., no evidence of overfit model) but displayed poor discriminative ability (optimism-corrected c-statistic = 0.54).
Post-Hoc Sensitivity Analysis
Order placement prior to PACU admission was associated with 3% reduced PACU duration (p = < 0.001), 8% decreased odds of multiple administrations of antiemetics (p = 0.02), and 28% reduced odds of having a higher pain score (p < 0.001) (Table 6).
Discussion
In a large retrospective sample of patients admitted to the PACU at a single academic medical center, we demonstrated an association between a mobile electronic PACU order reminder system and more timely order entry. Use of the system was associated with a greater percentage of patients arriving to the PACU with orders entered and, in those without preexisting orders, was associated with more rapid order entry during the PACU stay. In a post-hoc sensitivity analysis, order placement prior to PACU admission was associated with shorter PACU duration and decreased odds of both higher PACU pain scores and the incidence of multiple administrations of antiemetics.
Interestingly, while the reminder system was associated with increased odds of timely order placement, and on-time order placement was associated with shorter PACU durations, we found that patients whose attending utilized the system had longer median PACU durations than those who didn’t. However, this discrepancy is likely related to an interaction with one or more confounding variables. For example, we found that, other than on-time order placement, PACU length of stay was also associated with sex, race, height, weight, ASA class, case level, anesthesia duration, and provider-specific variables.
In the logistic regression analysis, the following provider-level factors were additionally associated with the placement of PACU orders prior to PACU admission: attending change during the case, in-room provider change during the case, and in-room provider with ordering privileges present during the case. Interestingly, these factors had variable effects on the outcome. A change of attending or the presence of an in-room ordering provider were both associated with greater odds of order placement, possibly because the oncoming ordering provider used the handoff as a cue to place the orders at that time. Conversely, a change in the in-room provider was associated with decreased odds of order placement. Each of these findings may be due to the distribution of responsibility for order placement amongst a group of providers, each of whom may have assumed orders were placed by another team member.
To account for other factors which may have affected the likelihood of timely PACU order placement, we additionally adjusted for anesthesia duration, case urgency, and patient ASA physical status. As expected, sicker patients and higher case urgency were associated with a decreased odds of order placement prior to PACU admission, while longer anesthesia time was associated with increased odds.
Over recent decades, the evidence supporting CPOE and electronic alerts and reminders in varying healthcare environments has grown [5, 6]. In the operating rooms, alerts embedded in anesthesia information management systems (AIMS) have been shown to improve compliance with antibiotic administration, treatment of hyperglycemia [5], and more. The transition to PACU, however, offers an additional opportunity where electronic alerts may provide operational or patient benefit. The added challenge of alerting a provider who is not actively working within the AIMS was overcome, in this case, via mobile device push notifications. Our study demonstrates a proof-of-concept that such technology can successfully reach clinicians and impact their behavior, with the potential to translate this method to other areas of healthcare.
It is also important to note that frequent push notifications can contribute to provider fatigue, leading to increased likelihood of being ignored. We attempted to mitigate these issues by allowing clinicians to add personalized user preferences and opt out of specific types of reminders. While data on changes to user preferences over time are not available, anecdotally our attending anesthesiologists have found this functionality useful.
This study has significant strengths including the inclusion of a large, diverse surgical population at a tertiary medical center operating room. The large sample size allowed increased power to detect significant differences between cases in which an order reminder system was or was not used for PACU order placement. Furthermore, the robust data collection procedures and analytic plan are easily replicated, leading to increased trustworthiness of results.
However, there were also several limitations. First, due to its single-center, retrospective design, the results of this study may not be generalizable to other patient populations. Also, we defined reminder system use as positive if the attending anesthesiologist received at least one push notification on the day of the surgery. We were unable to directly link reminders to individual surgical cases, and so our classification of cases likely included some false positives (cases in which the attending received an alert on the same day as, but not directly linked to, a specific case). Nor were we able to confirm acknowledgement of the reminder by the clinician. As a suggestion for future quality improvement initiatives, a more precise definition of system usage and reminder receipt could eliminate such bias. Similarly, the removal of cases with missing data is another potential source of bias. However, we feel that due to the relatively small number of cases with missing covariate data (< 1%), any bias that may be introduced is negligible.
In conclusion, in this single-center retrospective study, we found that an electronic reminder system was associated with timelier PACU order placement, which in turn may lead to improved patient outcomes.
Data Availability
No datasets were generated or analysed during the current study.
References
Iten, A., Perrier, A., and Lovis, C., Déploiement d'un programme de prescription informatisée: description du processus et enjeux [Deployment of a computerized physician order entry: description of the process and challenges]. Rev. Med. Suisse. 2(83):2344–6, 2348–9, 2006. French. PMID: 17112085.
Khajouei, R., and Jaspers, M. W., The impact of CPOE medication systems' design aspects on usability, workflow and medication orders: a systematic review. Methods Inf. Med. 49(1):3-19, 2010. https://doi.org/10.3414/ME0630. Epub 2009 Jul 6. PMID: 19582333.
Kadry, B,. Feaster, W. W., Macario, A., and Ehrenfeld, J. M., Anesthesia information management systems: Past, present, and future of anesthesia records. Mt. Sinai J. Med. 79:154–65, 2012.
Ehrenfeld, J. M., The current and future needs of our medical systems. J. Med. Syst. 39:16, 2015.
Ehrenfeld, J., Wanderer, J., Terekhov, M., Rothman, B., and Sandberg, W., A perioperative systems design to improve intraoperative glucose monitoring is associated with a reduction in surgical site infections in a diabetic patient population. Anesthesiology 126(3):431–440, 2017. https://doi.org/10.1097/aln.0000000000001516
Cordero, L., Kuehn, L., Kumar, R., and Mekhjian, H., Impact of computerized physician order entry on clinical practice in a newborn intensive care unit. J. Perinatol. 24(2):88–93, 2004. https://doi.org/10.1038/sj.jp.7211000
Wietholter, J., Sitterson, S., and Allison, S., Effects of computerized prescriber order entry on pharmacy order-processing time. Am. J. Health Syst. Pharm. 66(15):1394–1398, 2009. https://doi.org/10.2146/ajhp080303
Niazkhani, Z., Pirnejad, H., Berg, M., and Aarts, J., The impact of computerized provider order entry systems on inpatient clinical workflow: a literature review. J. Am. Med. Informat. Assoc. 16(4):539–549, 2009. https://doi.org/10.1197/jamia.m2419
Coma, E., Medina, M., Méndez, L., Hermosilla, E., Iglesias, M., Olmos, C., and Calero, S., Effectiveness of electronic point-of-care reminders versus monthly feedback to improve adherence to 10 clinical recommendations in primary care: a cluster randomized clinical trial. BMC Med. Inform. Decision Making 19(1), 2019. https://doi.org/10.1186/s12911-019-0976-8
Dougherty, J., and Bonfiglio, M., The future CPOE workflow: augmenting clinical decision support with pharmacist expertise. Hosp. Pharm. 54(3):149–152, 2018. https://doi.org/10.1177/0018578718791556
Page, N., Baysari, M., and Westbrook, J., A systematic review of the effectiveness of interruptive medication prescribing alerts in hospital CPOE systems to change prescriber behavior and improve patient safety. Int. J. Med. Inform. 105:22–30, 2017. https://doi.org/10.1016/j.ijmedinf.2017.05.011
Steele, A. M., and DeBrow, M., Efficiency gains with computerized provider order entry. In: Henriksen, K., Battles, J. B., Keyes, M. A., et al., (Eds.). Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 4: Technology and Medication Safety). Rockville (MD): Agency for Healthcare Research and Quality (US), 2008. Available from: https://www.ncbi.nlm.nih.gov/books/NBK43766/
von Elm, E., Altman, D. G., Egger, M., et al., Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 335(7624):806–8, 2007.
Funding
This manuscript was supported in part by NHLBI K23HL148640 (PI: Freundlich) from the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
JC: This author helped with collection and validation of the data, statistical analysis, interpretation of results, and drafting of manuscript, and approval of final version. HE: This author helped with defining of study variables, validation of data, revision of the manuscript, and approval of final version. CR: This author helped with validation of data, revision of the manuscript, and approval of final version. RF: This author helped with study conception, design, defining of study variables, validation of data, revision of the manuscript, and approval of final version. WS: This author helped with revision of the manuscript and approval of final version. JW: This author helped with study conception, design, defining of study variables, validation of data, revision of the manuscript, and approval of final version.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Clifton, J.C., Ende, H.B., Rathnam, C. et al. A Mobile Post Anesthesia Care Unit Order Reminder System Improves Timely Order Entry. J Med Syst 48, 60 (2024). https://doi.org/10.1007/s10916-024-02079-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-024-02079-7