Abstract
Introduction
Virtual reality (VR) is becoming increasingly popular to train health-care professionals (HCPs) to acquire and/or maintain cardiopulmonary resuscitation (CPR) basic or advanced skills.
Aim
To understand whether VR in CPR training or retraining courses can have benefits for patients (neonatal, pediatric, and adult), HCPs and health-care organizations as compared to traditional CPR training.
Methods
A systematic review (PROSPERO: CRD42023431768) following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. In June 2023, the PubMed, Cochrane Library, Scopus and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases were searched and included studies evaluated in their methodological quality with Joanna Briggs Institute checklists. Data were narratively summarized.
Results
Fifteen studies published between 2013 and 2023 with overall fair quality were included. No studies investigated patients’ outcomes. At the HCP level, the virtual learning environment was perceived to be engaging, realistic and facilitated the memorization of the procedures; however, limited decision-making, team building, psychological pressure and frenetic environment were underlined as disadvantages. Moreover, a general improvement in performance was reported in the use of the defibrillator and carrying out the chest compressions. At the organizational level, one study performed a cost/benefit evaluation in favor of VR as compared to traditional CPR training.
Conclusions
The use of VR for CPR training and retraining is in an early stage of development. Some benefits at the HCP level are promising. However, more research is needed with standardized approaches to ensure a progressive accumulation of the evidence and inform decisions regarding the best training methodology in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
New digital technologies have involved every aspect of life with virtual reality (VR) as an innovative tool in training purposes [1]. Although more than 100 definitions have been established to date [2], the term VR identifies various ways of simulating real situations using computers and the aid of specifically developed interfaces [3]. Recently, VR has been included in an overarching term named ‘extended reality’ which includes augmented reality, mixed reality, and other immersive technologies [4]. All these digital technologies have been introduced and tested in different training fields, cardiopulmonary resuscitation (CPR) included, underlining their potentialities in improving and/or maintaining skills [5]. The traditional CPR-standardized face-to-face courses are still offered to provide skills that need complex retraining due to their decreasing over time; however, these traditional courses require physical, human and time resources not easily ensured by the care systems and health-care professionals (HCPs) who are immersed in complex clinical environments, requiring a continuing development of diversified competences and skills [6]. Moreover, when the initial and retraining HCPs learning needs are not provided effectively, there is an increased risk of suboptimal care resulting in poor survival outcomes from cardiac arrest [5]. Considering these issues, recently there has been a call for new CPR training, along with the recommendation for strong research in resuscitation education [7]. In this context, the VR has gained increased space due to its multiple advantages over the traditional face-to-face CPR training methods. Its immersiveness allows participants to completely experience a realistic scenario, developing the skills expected in the real world [8]. VR also ensures involvement and interactivity as compared to the traditional training methods, maximizing the memorization through the feedback received. Moreover, spaces and resources required are limited given that it can be received anywhere, even at home [9]. However, while the use of VR in the basic CPR training of lay adults has been summarized recently regarding its capacity to improve skills [10], no summary of the evidence available concerning VR CPR training among HCPs has been provided to date. Therefore, the intent of this study was to describe the state of the research in this field and detect whether VR CPR training or retraining can have benefits for patients, HCPs and the health-care system.
Methods
Study design
A systematic review was performed following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [11]. The review protocol was registered in the PROSPERO database (CRD42023431768).
Research question
The research question was: “Are there any differences in the outcomes between the traditional face-to-face CPR training methods (hereafter, traditional CPR training) and the CPR training based on VR (hereinafter, VR CPR) among HCPs?” Following the Joanna Briggs Institute methodology, the Patient, Intervention, Comparison and Outcome (PICO) framework was used [12]. Specifically, the following were considered: (a) the P as representing the HCPs in any setting; (b) the I as the basic or advanced training for neonatal, pediatric, and adult CPR using VR; (c) the C as the traditional CPR training (e.g., conventional low-fidelity manikin-based training); and d) the O as outcomes measured at the patient (e.g., mortality, neurological), HCP (e.g., satisfaction) and health-care system (e.g., efficiency) levels.
Inclusion and exclusion criteria
The following studies were eligible for inclusion: randomized controlled trial (RCT), experimental, quasi-experimental and observational primary studies including HCPs (e.g., nurses, physicians, midwives or other); working in any type of setting (e.g., hospital, community, training centers); attending CPR training with VR [13]; and published in English or Italian at any time. Studies including students in a limited proportion compared to the involved HCPs or only in the control group, were eligible. Therefore, studies including lay people or only HCP students; only concerning non-VR CPR training; as well as literature reviews, qualitative studies, letters to editors, protocols, commentaries, and books, were all excluded. The retrieved reviews were inspected manually in their references to identify potential eligible studies.
Search methods
The search was conducted in PubMed, Cochrane Library, Scopus, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases, in June 2023. The keywords (Medical Subject Headings or free text-terms) used were: “Virtual Reality”; “Healthcare Professional”; “Cardiopulmonary Resuscitation”, in combination with the Boolean operators “AND” or “OR”. The search strings are reported in the Supplementary Table 1.
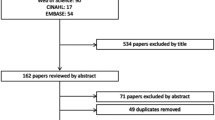
Study selection
A total of 1042 records were identified, 335 from the databases and 707 from citation searching. First, studies from the databases were screened. Duplicates (n = 78) were eliminated. During the screening process at the title and abstract levels, 213 studies were excluded as not satisfying the inclusion criteria. Subsequently, full texts were read and 31 were not eligible. Four articles did not clearly define the population (e.g., HCPs, lay people or students); therefore, the corresponding authors were contacted and only two answered allowing to exclude the articles according to the inclusion/exclusion criteria; the other two authors did not provide any answer, thus giving the impossibility to assess eligibility of the studies, these were excluded. The inclusion of one study was debated among researchers because it was not made explicit the extended reality used [14]; for this reason, it was excluded.
Articles from citation searching were also screened. From a total of 707 studies, 31 were excluded because duplicates. Of the remained, 676 were excluded because they did not satisfy the inclusion criteria. At the end, two articles were retrieved and included.
Overall, a total of 15 studies were considered (Fig. 1). The entire selection process involved two researchers (RT, AG) who worked independently; in case of disagreement a third researcher (SC) was consulted to reach consensus.
Flow diagram of the study selection process – Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [11] Legend: CINAHL, Cumulative Index to Nursing and Allied Health Literature; VR, virtual reality; CPR, cardio-pulmonary resuscitation; HCP, health-care professional; n, number
Quality assessment
The Joanna Briggs Institute checklists for randomized controlled trials [15], quasi-experimental [16], and cross-sectional studies [17], respectively were used. Some studies did not clearly indicate the design [18,19,20]: in the case of pre-post measures (even with a randomized sample), studies were considered quasi-experimental, while in the case of a single point evaluation, these were considered cross-sectional. The assessment was performed independently by two researchers (RT, SC); in the case of disagreement a third researcher (AG) was consulted to reach consensus.
Data extraction and synthesis
A data extraction table was firstly piloted in three studies and no modifications were required. Then, the data extraction process was conducted by two researchers (RT, AG) populating the grid with the following data: author(s), publication year, country where the study has been conducted; study objective and design; type of CPR (basic or advanced), training or retraining; data collection year and duration; sampling, sample, setting; virtual simulation modality, devices; main features of the CPR training offered as comparator; tools for outcome measurement; and main findings. A third researcher (AP) verified this process and resolved disagreements. Then, studies were grouped according to the CPR target population. A narrative synthesis of their main characteristics and quality was first provided [21]; then, the VR CPR training and comparison modes were described in their main features; a summary of the outcomes measured, and their metrics were then provided.
Results
Study characteristics
There were included 15 studies (Table 1) published between 2013 and 2023 and conducted in Europe [18, 19, 27,28,29], in North America [20, 24, 25, 31], in Africa [32, 33], in Asia [26, 30], and in Central America [23]; one study did not report the country [22].
Six were primarily aiming to investigate the efficacy of VR CPR training [18, 23, 25, 29, 31, 33], four its feasibility [22, 28, 29, 32], three its utility [19, 24, 30], and two its usability [20, 26]. To reach these aims, six were RCTs [22, 25, 27, 29, 31, 33], six were cross-sectional studies [19, 20, 24, 26, 28, 30], and three quasi experimental [18, 23, 32].
Basic CPR maneuvers were the target of eight studies [19, 22, 23, 26, 29, 30, 32, 33], while the remaining considered advanced CPR maneuvers [18, 20, 24, 25, 27, 28, 31]. Moreover, five studies focused on the initial CPR training [20, 22, 25, 27, 32], two the retraining [24, 33], while the remainder did not specify [18, 19, 23, 26, 28,29,30,31]. Studies were conducted mainly in hospitals [19, 22, 28,29,30, 32, 33], training centers [20, 23,24,25], and universities [18, 27]; two studies did not specify the setting [26, 31].
Regarding the targeted patients, population for which the training was intended included in 12 studies adults [18,19,20, 22,23,24,25,26,27,28,29,30]) while in three neonates [31,32,33]; no pediatric patients were included. In the neonatal field participants were only HCPs, with 274 nurses and midwives [33], and 34 physicians [31]. Differently, studies concerning adult CPR included only physicians and sub-specialty, specific participants ranging from 25 anesthesiology residents to 148 clinicians [24, 25]; other adult studies included a mixed of HCPs, as for example 40 physicians and nurses [18], or 30 CPR instructors [30]. Some studies were focused on a limited number of professionals (e.g., three nursing assistants and four nurses [22]) to 80 participants including nurses, physicians, engineers, students and researchers [29]. The age of participants ranged from 19 to 57 years and studies included primarily females (e.g., 93.2% [25]); however, five studies did not specify participants’ sex or age [20, 22, 23, 26, 31].
At the overall level, the data collection duration lasted from two years with an additional six-month follow-up to a single day [27, 33]. The remaining studies collected data over two and over three months [18, 22, 29]; however, in 11 studies the duration was not specified.
The methodological quality of the studies (Supplementary tables 2, 3 and 4) was overall fair; in the six cross-sectional studies confounding factors and strategies to deal with them were not identified [19, 20, 24, 26, 28, 30]; in five RCTs the allocation to treatment groups and the outcome assessors were not blinded [25, 27, 29, 31, 32]; in two quasi-experimental studies the control group was not identified [18, 22].
VR CPR intervention and comparison training methods
Intervention group
Almost all studies carried out the VR training using virtual 3D scenarios with the aid of additional accessories, such as a viewer [19]. Some studies also employed a high-fidelity manikin connected to a computer [19, 20, 23, 26, 29, 32], and compared the use of a very persuasive scenario with many components (visual aids, live instructions, and text messages) and a less persuasive one (only task completion messages at the end of these) [20]. In some studies, instructors were allowed to independently modify scenarios in real time [19, 24, 28].
Five studies showed an initial tutorial regarding the VR simulation [18, 22, 26, 27, 31]; which varied from a 20-s presentation to 20 min with an AI instructor [22, 26]. The total duration of the training session was usually one hour [18, 27], but the VR exposure time ranged from three or five minutes per scenario to approximately 30 min [20, 32].
Comparison group
The training methods considered as comparators were mainly the traditional CPR using a full-body or half-torso low-fidelity manikin [25, 27, 29], or a high-fidelity manikin [24]; or two different versions of the VR simulator (with and without a persuasive features) [20]. In the other two studies the comparators were not specified [23, 30]. Moreover, a pre-post comparison was performed with the same group [18, 22]; while two groups, with different qualifications and experiences, were compared within the same VR simulation [28, 31].
VR CPR outcomes
No studies investigated patient’s outcomes whereas those studies reporting HCPs outcomes were mainly based on a pre-post [18, 22], or only post- questionnaires [19, 20, 24, 26,27,28, 30, 32], through checklists filled in by observers [22, 25, 33], or specific sensors and software (e.g., feedback technology [29]).
Outcomes at the HCP level
HCP experience
At the HCP experience level, VR scenarios were considered realistic (e.g., 80% [18]; 97% [19]). Moreover, around 72% of participants perceived the environment as engaging and facilitating the memorization of the procedures; 86% considered the VR simulations a useful training and agreed to recommend it to other colleagues [27]. On the other hand, the high-fidelity simulation group reported similar satisfaction and utilization scores, but significantly better scores regarding the provided feedback (99%, Interquartile Range [IQR] 89–100) as compared to the VR group (79%, IQR 71–88, p < 0.01) [24]. Using VR has led to greater commitment and increased knowledge acquired; furthermore, the gaming approach was perceived positively [30]. However, some disadvantages emerged in using VR scenarios, including limited decision-making freedom, the lack of the possibility to build a team, as well as the absence of a real psychological pressure and a frenetic environment, as lived in the reality [28]. In this regard, the level of stress during VR simulations among residents showed higher salivary cortisol levels than consultants (+ 0.07 μg/dL, 95%, CI = 0.03–0.12, p = 0.001) [31]. During the same VR simulations, heart rates also differed between residents and consultants, with higher values for the former (85.9 hearth rate per minute, range 78–93.7) compared to the latter (78.9 hearth rate per minute, range 71.2–87.4) [31].
HCP knowledge
At the HCP knowledge level, studies comparing the number of correct questions through a pre–post test showed a statistically significant improvement [18, 22, 33]. For example, the number of correct answers per HCP participants increased on average by 4.8 (95%, CI 3.4–6.2, p < 0.001) after the virtual simulation [18].
HCP performance
Performance measured as the degree of confidence with the automated external defibrillator (e.g. improvement in the time of positioning the pads, in rhythm analysis and defibrillation) and participation in a group simulation, was higher (+ 28.6% both) after virtual simulation [22]. In contrast, 43% of participants after the traditional training were able to administer stacked shocks within one minute, whereas none of the participants in the VR group could so; moreover, the target sternotomy time was achieved in 100% of procedures in the control group and in 83% in the VR group [27]. However, in the VR group the total number of errors was lower compared to the control group (11 vs 15) [27]. The more previous training in CPR possessed by a participant the greater the percentage of correct compressions obtained in a VR CPR session (F-Ratio 14.95; p < 0.001) [23]. A total of 88% of participants using VR achieved a correct compression rate and 65% a positive result in the depth of compression applied to the manikin [19]. Better retention of skills in bag and mask ventilation at six months (-15% VR group, p = 0.10; -21% video group, p < 0.01; -27% control group, p = 0.001) was documented [33].
An improvement was also found when comparing the pre–post performances of the low-fidelity manikin group (p = 0.017 for pulseless electrical activity, PEA, p = 0.01 for ventricular fibrillation/ventricular tachycardia, VF/VT) and the persuasive VR group (p = 0.02 for PEA, p = 0.048 for VF/VT) but not for the minimally persuasive VR group (p = 0.45 for PEA, p = 0.46 for VF/VT) [25]. Different, participants in the group with the less persuasive scenario reported a perception of greater usability (p = 0.0944) and ease in interfacing with the simulation compared to the very persuasive scenario (p = 0.0813) [20]; however, the results were not statistically significant. The group with live feedback on the quality of chest compressions achieved better performance in both frequency and depth compared to the non-feedback group (35.78% vs 7.27%, p < 0.001) [29]. It was also seen that the chest compressions rate of the more experts was not influenced by the feedback, while the performances of the novices improved with the use of the feedback (112.07, SD 3.70 vs 98.39, SD 29.23, p = 0.001) [29].
Outcomes at the health-care system level
Economic Impact
At the organizational level, four studies mentioned the cost-saving opportunities that VR could have in the future, despite the initial expense for the purchase of software (as licenses) and materials (as computers, sensors) [18, 24, 28, 31]. However, only one calculated the economic impact of using VR compared to the traditional method, highlighting a significant saving of 83% for a single learner for four training sessions (132.29 dollars for VR versus 772.00 dollars for the traditional method) in terms of human resources, classrooms as well as time spent in travelling [24].
Discussion
Study characteristics
The research in the field of VR CPR has been established in the last ten years, with 15 studies, including 1,035 total participants and conducted in almost all continents, suggesting that these educational strategies can be ubiquitarian and considered also by lower-income countries. As documented in a recent systematic review, VR CPR training among adult laypersons has instead been investigated by only six studies involving a total of 731 participants between 2017 and 2021 [10].
Measuring the effectiveness, the feasibility and the utility of VR CPR has been the main intents of studies available; therefore, this research field seems to be focused around two main lines. The first is aimed at developing and introducing VR into CPR training, and the second in measuring its outcomes, both in basic and advanced CPR skills, mainly with regards to adult patients, involving HCPs in hospital settings. This substantial differences in research approaches, divided between educational impact [31], and those of digital devices design, development and piloting [20], may explain some missing elements that have emerged in the study methodology quality assessment as: study duration, mainly short or not reported; limited sample size, from a few HCPs to a maximum of 274; lack of description of the control group, or no control group established (four studies); and the poor description of the professional background, baseline competences and/or participants’ experiences. The lack of description of the HCPs expertise, should be considered as an important lack in assessing whether the outcomes are purely associated to the VR CPR or also to prior experience. Overall, studies available seem to express a research field in its early stage. Guidelines based on broad consensus regarding the elements to document in future studies to harmonize their reporting and ensure that some essential data are described (e.g., VR CPR as a refresher or first training), by differentiating those aimed at piloting the digital technologies and those at measuring their effectiveness, may increase transparency, comparability and the accumulation of the evidence produced.
Intervention and comparison group training methods
Five main considerations may be derived from VR devices and training methods documented to date in the available literature.
First, according to the extended reality recently conceptualized in this field [2], twelve studies [18,19,20, 23,24,25, 27, 28, 30,31,32,33] were based on VR, two on augmented reality [26, 29], while one used the term virtual simulation [22]. Therefore, studies available mainly used VR and augmented reality-based CPR training.
Second, while some studies have been based on relatively simple technologies [20, 29], others have implied several and complex technologies, from software created for 3D gaming to sensors connected to a computer [18, 24, 30]. On the one hand, this great heterogeneity suggests an ample creativity and innovation; on the other, it prevents comparison and conclusions regarding the outcomes.
Third, interactivity as the possible way to provide (or not) real-time feedback on participants’ performance (e.g., depth and frequency of chest compressions) and the likelihood of changing the scenario suggest that some studies embraced the main characteristics of VR, i.e. that it includes a totally immersive environment in which the person is completely isolated from the external setting and transported into a parallel reality, reproduced with the use of additional devices, such as visors or sensory gloves [19, 31].
Fourth, in all studies, the sections are short in duration, sometimes providing brief tutorials to familiarize participants with the tasks; in all cases, from the initiation to the end of the section, the CPR training seems to save time, and this may benefit the HCPs, the health-care organization and the continuing education agencies to address other learning needs. Regarding the comparisons, a wide range of training methods have been used: alongside efforts in standardizing the description of the comparator used in the studies, comparing the effectiveness of VR CPR with the most traditional training method used in daily practice may help in accumulating evidence in this field.
VR CPR outcomes
Different outcomes have been measured to date, employing several measures both subjective (e.g., self-reported participants’ satisfaction [24]) and objective (e.g., sensor for automatic detection of participants’ performance [19]), preventing the production of a cumulative synthesis of the evidence available. First, the substantial infancy of this research field may have prevented any evaluation on patient outcomes, requiring complex study designs and long follow-ups. Also, in the review concerning lay people, a few studies have investigated the association of the educational interventions with patients’ outcomes after cardiac arrest, both in the short and long term [10]. However, given that the main aims of the CPR training, regardless of the methods, is to improve health outcomes, this lack should be addressed in the future to assess the VR role in this training field.
Second, outcomes most evaluated are those at the HCP level. With this regards, Kirkpatrick’s framework has established the evaluation system of HCP educational programs as categorized into four levels, from the first and easier to assess (reactions) to the following and more complex (learning, behavioral and results) [34]. In the context of VR CPR training, the first have been documented in 13 studies [18,19,20, 22,23,24,25,26,27, 29, 31,32,33], reporting a good level of usability, appreciation, and satisfaction. One study underlined that the simulation failed to reproduce the characteristics of the real emergency scenario [28].
Learning outcomes, the second level of the Kirkpatrick’s framework [34], have been measured in all studies. Knowledge has improved, along with some evidence regarding better memory retainment of the acquired practices [18]. With the traditional CPR education, the decline in theoretical notions and practical skills occurs just two months after the end of the course, reaching a peak at six months [35]; in contrast, VR training has shown that knowledge and skills at one, three, and six months remain higher [33]. Moreover, some better performances have also been reported in terms of the decreased time needed to assess the heart rhythm and use of the defibrillator, which can be particularly useful in rare conditions, such as cardiac arrest in children [36]. Notably, two out of three studies concerning neonatal emergencies were conducted in Africa [32, 33], where the neonatal mortality rate is extremely high suggesting that VR methods of training may have a potential role in some conditions characterized by the rare occurrence of the phenomenon in the real world, issues regarding geographic accessibility, and underdeveloped economic conditions [37].
No studies investigated behavioral modifications [34], such as the extent to which the trainees apply the learning and change their behavior in real practice, immediately or months after the training. Conducting prospective studies monitoring the behavioral modification of participant HCPs after VR CPR training over time may be challenging, time-consuming and influenced by several confounding factors (e.g., having attended other training initiatives [38]). Most training interventions are evaluated only in terms of theoretical-practical knowledge achieved immediately at the end, and not in terms of changes in the medium or long term [39, 40]. In addition, only a few health-care facilities and universities use VR, and this may limit the likelihood of conducting such evaluations [41].
Alongside the lacks in behaviors modification, VR CPR training has been subjected to a little scrutiny regarding its capacity to develop decision making and team-building skills (e.g., team training and interaction with the team) [28]. Both skills have been described as fundamental in the CPR practice [41], and this limitation might affect the real-world applicability of VR in this field. Involving more participants within the same VR scenario and promoting their interaction over that between the HCPs and the VR software may be useful [28]; reproducing the chaotic environment typical lived during the emergency situations, may also increase the reality of the VR scenarios and promote the transferability of the competences gained in the real world.
Concerning the impact of the results on the health-care organization, no studies have assessed this association with VR CPR training also in this case likely due to the complexity of these investigations [42, 43]. Despite some studies reported cost-saving opportunities [18, 28, 31], only one calculated the economic impact [24]. Understanding whether VR can have benefits in terms of efficiency is essential to promote and convince of the need of an initial investment that may have important long-term cost-saving effects [44]. Producing more evidence may also inform the long-term sustainability of investments in these new technologies.
Limitations
This systematic review has several limitations. Despite the attempt to conduct an accurate systematic review by registering in advance the protocol, and strictly following the PRISMA guidelines [11], selection biases may have occurred. Moreover, to provide a broader picture on all studies available all retrieved articles have been included despite their methodological quality. In addition, the background of researchers involved in the analysis of the studies, although experts in CPR and research methodologies, may have influenced the data extraction by missing some aspects regarding the technologies used.
Conclusions
The research in the field of VR CPR training is recent and conducted in several countries, mainly focused around two aims: developing the VR technologies and methods of training; and measuring the VR CPR effectiveness or practical implementation. Studies available concern mainly adult CPR training in hospital settings, with mixed voluntary HCPs; they are not-always specified as training or retraining and limited in the sample size. Outcomes have been assessed mainly at the HCP level, investigating reactions, and effects on knowledge and performance.
At the overall level, the evidence available regarding VR CPR training is promising: however, robust studies are required to overcome the methodological gaps in this research field. Guidelines establishing the essential data that should be communicated while reporting studies are recommended. Moreover, the effectiveness of VR CPR training research on clinical outcomes (by considering also pediatric patients) should be investigated; in addition, describing changes in the performances and behavior as manifested in the management of real-world cases after having received the VR CPR training is a priority. In this context, designing more complex studies by involving several HCPs in the same scenario, connected remotely, and stimulating interactions and strategies to also investigate their decision-making processes, may be important. All these evaluations may expand the evidence available and inform decision-makers regarding long-term investments and sustainability of the VR CPR training.
Availability of data and materials
Not applicable.
References
Izard SG, Juanes JA, García Peñalvo FJ, Estella JMG, Ledesma MJS, Ruisoto P (2018) Virtual Reality as an Educational and Training Tool for Medicine. J Med Syst 42:50. https://doi.org/10.1007/s10916-018-0900-2
Fijačko N, Metličar Š, Kleesiek J, Egger J, Chang TP (2023) Virtual Reality, Augmented Reality, Augmented Virtuality, or Mixed Reality in cardiopulmonary resuscitation: Which Extended Reality am I using for teaching adult basic life support? Resuscitation 192:109973. https://doi.org/10.1016/j.resuscitation.2023.109973
Kanschik D, Bruno RR, Wolff G, Kelm M, Jung C (2023) Virtual and augmented reality in intensive care medicine: a systematic review. Ann of Intensive Care 13:81. https://doi.org/10.1186/s13613-023-01176-z
Tang YM, Chau KY, Kwok APK, Zhu T, Ma X (2022) A systematic review of immersive technology applications for medical practice and education-Trends, application areas, recipients, teaching contents, evaluation methods, and performance. Educ Res Rev 35:100429. https://doi.org/10.1016/j.edurev.2021.100429
Cheng A, Nadkarni VM, Mancini MB, Hunt EA, Sinz EH, Merchant RM, et al (2018) Resuscitation Education Science: Educational Strategies to Improve Outcomes From Cardiac Arrest: A Scientific Statement From the American Heart Association. Circulation 138(6):e82–e122. https://doi.org/10.1161/CIR.0000000000000583
Cheng A, Magid D, Auerbach M, Bhanji F, Bigham BL, Blewer AL et al (2020) Part 6: resuscitation education science: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142:S551–S579. https://doi.org/10.1161/CIR.0000000000000903
Greif R, Lockey A, Breckwoldt J, Carmona F, Conaghan P, Kuzovlev A et al (2021) European Resuscitation Council Guidelines 2021: Education for resuscitation. Resuscitation 161:388–407. https://doi.org/10.1016/j.resuscitation.2021.02.016
Semeraro F, Scapigliati A, Ristagno G, Luciani A, Gandolfi S, Lockey A et al (2017) Virtual Reality for CPR training: How cool is that? Dedicated to the "next generation". Resuscitation 121:e1–e2. https://doi.org/10.1016/j.resuscitation.2017.09.024
Al-Ansi AM, Jaboob M, Garad A, Al-Ansi A (2023) Analyzing augmented reality (AR) and virtual reality (VR) recent development in education. Social Sciences & Humanities Open 8:100532. https://doi.org/10.1016/j.ssaho.2023.100532
Alcázar Artero PM, Pardo Rios M, Greif R, Ocampo Cervantes, AB, Gijón-Nogueron G, Barcala-Furelos, R et al (2023) Efficiency of virtual reality for cardiopulmonary resuscitation training of adult laypersons: A systematic review. Medicine 102:e32736. https://doi.org/10.1097/MD.0000000000032736
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulro CD et al (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery 88:105906. https://doi.org/10.1016/j.ijsu.2021.105906
Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K et al (2015) Conducting systematic reviews of association (etiology): The Joanna Briggs Institute's approach. Int J Evid Based Healthc 13:163-9. https://doi.org/10.1097/XEB.0000000000000064
O'Connor S (2019) Virtual Reality and Avatars in Health care. Clin Nurs Res 28:523–528. https://doi.org/10.1177/1054773819845824
Drummond D, Arnaud C, Guedj R, Duguet A, de Suremain N, Petit A (2017) Google Glass for Residents Dealing with Pediatric Cardiopulmonary Arrest: A Randomized, Controlled, Simulation-Based Study. Ped Clinical Care Med 18:120–127. https://doi.org/10.1097/PCC.0000000000000977
Barker TH, Stone JC, Sears K, Klugar M, Tufanaru C, Leonardi-Bee J, Aromataris E, Munn Z (2023) The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid Synth 21:494–506. https://doi.org/10.11124/JBIES-22-00430
Johanna Briggs Institute (2020) Checklist for quasi-experimental studies. https://jbi.global/critical-appraisal-tools. Accessed 2 Apr 2024
Johanna Briggs Institute (2020) Checklist for analytical cross sectional studies. https://jbi.global/critical-appraisal-tools. Accessed 2 Apr 2024
Buttussi F, Pellis T, Cabas Vidani A, Pausler D, Carchietti E, Chittaro L (2013) Evaluation of a 3D serious game for advanced life support retraining. Int J Med Inf 82:798–809. https://doi.org/10.1016/j.ijmedinf.2013.05.007
Rodríguez-Matesanz M, Guzmán-García C, Oropesa I, Rubio-Bolivar J, Quintana-Díaz M, Sánchez-González P (2022) A New Immersive Virtual Reality Station for Cardiopulmonary Resuscitation Objective Structured Clinical Exam Evaluation. Sensors 22:4913. https://doi.org/10.3390/s22134913
Vankipuram A, Khanal P, Ashby A, Vankipuram M, Gupta A, Drumm Gurnee D (2014) Design and development of a virtual reality simulator for advanced cardiac life support training. IEEE J Biomed Health Inform 18:1478-84. https://doi.org/10.1109/JBHI.2013.2285102
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M (2006) Guidance on the conduct of narrative synthesis in systematic reviews. ESRC methods programme, V1, b92. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf. Accessed 2 Apr 2024
Brzozowski S, Kandrack M, Oermann MH, Dangerfield C, Simmons Muckler VC (2022) Virtual Simulation to Reinforce Nursing Staff Resuscitation Responses. JNPD 38:151–156. https://doi.org/10.1097/NND.0000000000000764
García Fierros FJ, Moreno Escobar JJ, Sepúlveda Cervantes G, Morales Matamoros O, Tejeida Padilla R (2021) VirtualCPR: Virtual Reality Mobile Application for Training in Cardiopulmonary Resuscitation Techniques. Sensors 21:2504. https://doi.org/10.3390/s21072504
Katz D, Shah R, Kim E, Park C, Shah A, Levine A et al (2020) Utilization of a Voice-Based Virtual Reality Advanced Cardiac Life Support Team Leader Refresher: Prospective Observational Study. J Med Internet Res 22:e17425. https://doi.org/10.2196/17425
Khanal P, Vankipuram A, Ashby A, Vankipuram M, Gupta A, Drumm-Gurnee D et al (2014) Collaborative virtual reality based advanced cardiac life support training simulator using virtual reality principles. J Biomed Inform 51:49–59. https://doi.org/10.1016/j.jbi.2014.04.005
Lee DK, Choi H, Jheon S, Jo YH, Im C W, Il SY (2022) Development of an Extended Reality Simulator for Basic Life Support Training. IEEE J Transl Eng Health Med 10:4900507. https://doi.org/10.1109/JTEHM.2022.3152365
Peek JJ, Max SA, Bakhuis W, Huig IC, Rosalia RA, Sadeghi AH et al (2023) Virtual Reality Simulator versus Conventional Advanced Life Support Training for Cardiopulmonary Resuscitation Post-Cardiac Surgery: A Randomized Controlled Trial. J Cardiovasc Dev Dis 10:67. https://doi.org/10.3390/jcdd10020067
Sadeghi AH, Peek JJ, Max SA, Smit LL, Martina BG, Rosalia RA et al (2022) Virtual Reality Simulation Training for Cardiopulmonary Resuscitation After Cardiac Surgery: Face and Content Validity Study. JMIR Serious Games 10:e30456. https://doi.org/10.2196/30456
Semeraro F, Frisoli A, Loconsole C, Bannò, F, Tammaro G, Imbriaco G (2013) Motion detection technology as a tool for cardiopulmonary resuscitation (CPR) quality training: a randomised crossover mannequin pilot study. Resuscitation 84:501-7. https://doi.org/10.1016/j.resuscitation.2012.12.006
Wong MAME, Chue S, Jong M, Benny HWK, Zary N (2018) Clinical instructors’ perceptions of virtual reality in health professionals’ cardiopulmonary resuscitation education. SAGE Open Medicine 6. https://doi.org/10.1177/2050312118799602
Chang TP, Hollinger T, Dolby T, Sherman JM (2021) Development and Considerations for Virtual Reality Simulations for Resuscitation Training and Stress Inoculation. Simul Healthc 16:e219–e226. https://doi.org/10.1097/sih.0000000000000521
Ezenwa BN, Umoren R, Fajolu IB, Hippe DS, Bucher S, Purkayastha S et al (2022) Using Mobile Virtual Reality Simulation to Prepare for In-Person Helping Babies Breathe Training: Secondary Analysis of a Randomized Controlled Trial (the eHBB/mHBS Trial). JMIR Med Educ 8:e37297. https://doi.org/10.2196/37297
Umoren R, Bucher S, Hippe DS, Ezenwa BN, Fajolu IB, Okwako FM et al (2021) eHBB: a randomised controlled trial of virtual reality or video for neonatal resuscitation refresher training in healthcare workers in resource-scarce settings. BMJ Open 11:e048506. https://doi.org/10.1136/bmjopen-2020-048506
Kirkpatrick DL, Kirkpatrick JD (2007) Implementing the Four Levels: A Practical Guide for Effective Evaluation of Training Programs. Berrett-Koehler Publishers.
Jeffers J, Eppich W, Trainor J, Mobley B, Adler M (2016) Development and Evaluation of a Learning Intervention Targeting First-Year Resident Defibrillation Skills. Pediatr Emerg Care 32:210–216. https://doi.org/10.1097/PEC.0000000000000765
Galazzi A, Bonasera Vincenti NM, Giusti GD, Brioni M, Adamini I, Laquintana D, et al (2020) The Medical Emergency Team in Italy: an overview of in-hospital emergencies response. Acta Biomed 91:9–18. https://doi.org/10.23750/abm.v91i6-S.9878
United Nations Inter-Agency Group for Child Mortality Estimation IGME (2019) Neonatal mortality rate-total 2019 https://childmortality.org/data/Central%20African%20Republic. Accessed 2 Apr 2024
Garrett B, Taverner T, Gromala D, Tao G, Cordingley E, Sun C (2018) Virtual Reality Clinical Research: Promises and Challenges JMIR Serious Games 6:e10839. https://doi.org/10.2196/10839
Penuel WR, Fishman BJ (2012) Large-scale science education intervention research we can use. J Res Sci Teach 49:281–304. https://doi.org/10.1002/tea.21001
Lie SS, Helle N, Sletteland NV, Vikman MD, Bonsaksen T (2023) Implementation of Virtual Reality in Health Professions Education: Scoping Review. JMIR Med Educ 9:e41589. https://doi.org/10.2196/41589
Kobras M, Langewand S, Murr C, Neu C, Schmid J (2016) Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation. World J Emerg Med 7:255–262. https://doi.org/10.5847/wjem.j.1920-8642.2016.04.003
Kuyt K, Park SH, Chang TP, Jung T, MacKinnon R (2021) The use of virtual reality and augmented reality to enhance cardio-pulmonary resuscitation: a scoping review. Adv Simul 6:11. https://doi.org/10.1186/s41077-021-00158-0
Della Libera C, Simon J, Larøi F, Quertemont E, Wagener A (2023) Using 360-degree immersive videos to assess multiple transdiagnostic symptoms: A study focusing on fear of negative evaluation, paranoid thoughts, negative automatic thoughts, and craving. Virtual Real 9:1–16. https://doi.org/10.1007/s10055-023-00779-y
Lin Y, Cheng A, Hecker K, Grant V, Currie GR (2018) Implementing economic evaluation in simulation-based medical education: challenges and opportunities. Med Educ 52:150–160. https://doi.org/10.1111/medu.13411
Funding
Open access funding provided by Università degli Studi di Udine within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Roberto Trevi: Conceptualization; Investigation; Writing - Original Draft; Visualization. Stefania Chiappinotto: Conceptualization; Methodology; Formal analysis; Investigation; Writing - Original Draft; Visualization. Alvisa Palese: Conceptualization; Methodology; Formal analysis; Resources; Writing - Review & Editing; Visualization; Supervision; Project administration. Alessandro Galazzi: Conceptualization; Methodology; Formal analysis; Investigation; Writing - Original Draft; Visualization; Project administration.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Trevi, R., Chiappinotto, S., Palese, A. et al. Virtual Reality for Cardiopulmonary Resuscitation Healthcare Professionals Training: A Systematic Review. J Med Syst 48, 50 (2024). https://doi.org/10.1007/s10916-024-02063-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-024-02063-1