Abstract
This study examines whether an immigrant health advantage exists among US Whites, a group often used as a reference category in research on racial and ethnic health disparities. Using recent data from the National Health Interview Survey (2019–2022), I disaggregate non-Hispanic White adults (n = 41,752) by nativity status and use logistic regression models to assess differences in six measures of mental and physical health. The analysis includes self-reported conditions (depression, anxiety, fair/poor self-rated health) and diagnosed conditions that require interaction with the healthcare system (hypertension, diabetes, and chronic obstructive pulmonary disease, COPD). Foreign-born Whites have a significantly lower prevalence of each health outcome relative to US-born Whites. The immigrant health advantage remains significant for depression, anxiety, fair/poor health (i.e., self-reported conditions) and diagnosed hypertension, after adjusting for sociodemographic and healthcare characteristics. In contrast, the inclusion of these explanatory factors reduces the nativity gap in diagnosed diabetes and COPD to non-significance. Overall, the results indicate important variation in health among Whites that is missed in studies that focus on US-born Whites, alone. Scholars must continue to monitor the health of White immigrants, who are projected to grow to 20% of the US immigrant population in the years to come.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The health and well-being of immigrants is a topic of growing public health concern. In 2022, immigrants made up 13.9% (46.2 million) of the US population, up from 7.9% in 1990 and more than double in absolute size (19.8 million) [1, 2]. Immigrants are also diversifying the composition of US racial and ethnic populations, which has implications for population health and the healthcare system [3, 4]. To date, the majority of evidence on immigrant health has derived from research on the largest immigrant group, Hispanics (42%), and to a lesser extent, on Asian (27%) and Black (11%) immigrants [5,6,7,8,9]. The general finding in the literature is one of better health among immigrants relative to their US-born counterparts, which is often referred to as the “healthy immigrant effect” or “immigrant health advantage” [10,11,12,13].
Compared to research on racial and ethnic minorities, surprisingly little is known about the health of non-Hispanic White immigrants (hereafter White). This is an important oversight for several reasons. First, foreign-born Whites make up 17% (7.6 million) of the US immigrant population and are projected to grow to 20% (15.6 million) by 2060 [14, 15]. Not only will their numbers contribute to patterns in immigrant health, but also to patterns in overall population health via growth in the second and third generations [15]. Second, Whites are ethnically diverse and defined by the US Census as persons who trace their ancestries to “any of the original peoples of Europe, the Middle East, and North Africa” [16, 17]. When the federal government established standards for racial and ethnic categoriesFootnote 1 in 1977, western European Whites comprised over 70% of the total US population and 60% of the foreign-born White population [18,19,20]. Today, those numbers have dropped to roughly one-third each, while Middle Eastern and eastern European immigrants—who are also classified as White—have grown to comprise over one-half (53%) of the foreign-born White population (author’s calculations from US Census data, see Fig. 1 online supplement).
Odds ratios of self-reported health conditions by nativity status with 95% confidence intervals
Note: Odds ratios derived from logistic regression models in Table 2, Panel A. The unadjusted models include nativity status (Model 1) and the adjusted models include all covariates (Model 2)
The majority of immigrants from the Middle East and eastern Europe have arrived in the US since 1990, after the Iran-Iraq War (1980-89), fall of the Former Soviet Union (1991), and beginning of the first Gulf War (1991) [20]. They are linguistically, phenotypically, and culturally more diverse than their western European predecessors, and many have migrated under challenging circumstances due to political and civil unrest in their countries of origin [21,22,23]. Their contexts of migration have led to lower levels of health selection relative to immigrants arriving from more economically and politically stable regions [23,24,25]. Once in the US, these newer immigrants are incorporated into a racial stratification system that classifies them as “White,” even if they do not identify or pass as White [26, 27]. As a result, health disparities within these populations may be overlooked when aggregated into the broad White category.
Studies that disaggregate White ethnic subgroups, such as Arab Americans, have indeed found higher rates of diabetes [28, 29], heart disease [30], disability [31], cognitive limitations [32], psychological distress [11], and poorer self-rated health [33] than US-born Whites, even after accounting for compositional differences in socio-demographic characteristics (i.e., factors that might account for health disparities). Immigrants from the Former Soviet Union, who are also classified as White, likewise report higher rates of hypertension [34], disability [21, 35], and poorer self-rated health [10, 23] when compared to US-born Whites. Together, these studies suggest that the healthy immigrant effect found for other racial/ethnic groups may be weaker among Whites, at least for some White subgroups.
While informative, research on specific ethnic subgroups paints a partial picture of White immigrant health. Studies that compare all foreign-born Whites to US-born Whites are limited, and even fewer have examined multiple mental and physical health outcomes in the same analytic framework. Thus, the extent to which US- and foreign-born Whites differ across a range of outcomes is unknown. Less is also known about compositional variation among White immigrants on factors related to health, such as poverty and access to healthcare. Evaluating the compositional characteristics of Whites could provide a more complete understanding of the mechanisms driving observed health disparities. The current study addresses these questions and contributes to a nascent literature on White immigrant health. Using the most recently available data from the National Health and Interview Survey (2019–2022), I disaggregate Whites by nativity status and assess differences in six measures of mental and physical health. I center the analysis on three interrelated research questions:
RQ1) To what extent is there a nativity gap in health among Whites (i.e., do the foreign-born.
experience a health advantage over the US-born)?;
RQ2) Does the nativity gap vary across measures of mental and physical health?;
RQ3) Do compositional differences in sociodemographic and healthcare factors.
account for observed disparities in health between US- and foreign-born Whites?
Methods
Data and Measures
This study uses merged data from the 2019 to 2022 National Health Interview Survey (NHIS).Footnote 2 The data were obtained through the University of Minnesota’s Integrated Public Use Microdata Series (IPUMS) and include pooled samples from the 2019 to 2022 files with integrated sampling weights. The analytic sample includes US-born (n = 39,468) and foreign-born (n = 2,284) non-Hispanic White adults ages 25 to 64.Footnote 3 The data are publicly available and contain no identifying information on respondents, thus deemed exempt from Institutional Review Board (IRB) approval.
The dependent variables include three self-reported health conditions (where respondents evaluated their own health status) and three diagnosed health conditions (where respondents had to interact with the healthcare system to receive a diagnosis). The self-reported conditions are depression, anxiety, and self-rated health. Depression and anxiety were coded to capture respondents who reported feeling depressed or anxious/worried/nervous on a daily, weekly, or monthly basis (reference = never or a few times a year), and self-rated health identified those who reported fair or poor health (reference = excellent, very good, or good). The diagnosed health conditions are diabetes, hypertension (or high blood pressure), and chronic obstructive pulmonary disease (COPD). Each outcome is associated with several leading causes of death (e.g., heart attack, stroke) [36] and requires access to healthcare to receive a diagnoses [37, 38]. Responses were coded to identify respondents who had been diagnosed with each condition (reference = not diagnosed).
The key independent variable is nativity (reference = US-born). I also include several sets of covariates that might account for observed heterogeneity in health [10]. Socioeconomic characteristics are captured with measures for educational attainment (reference = less than high school); employment status (reference = not currently working/not in the labor force); and poverty status (reference = 5 times or more above the poverty threshold). Healthcare access includes health insurance coverage (reference = no coverage); having a usual place of care (reference = no); and having seen a doctor or other healthcare professional in the past 12 months (reference = no). Demographic and health behavior characteristics are age and age squared (continuous in years); gender; marital status; presence of children in the home; US citizenship status; region of US residence; body mass index (BMI); and smoking status. I conducted several sensitivity analyses to ensure that measurement decisions did not affect the primary results (available on request).
Analytic Strategy
Table 1 provides descriptive statistics on the key variables of interest (Table S1, online supplement, contains all variables in the analyses). I use Pearson chi-square (χ2) and Wald tests with Rao and Scott’s second-order correction to identify significant differences between US- and foreign-born Whites across health conditions (RQ1, RQ2) and sociodemographic and healthcare factors (RQ3). I then use a series of logistic regression models to estimate health outcomes, with and without adjustment for covariates, using the Bayesian Information Criteria (BIC) to identify the best model fit. Table 2 presents the odds ratios predicting self-reported health conditions in Panel A and diagnosed health conditions in Panel B (Tables S2 and S3 include the full set of covariate estimates). Figures 1 and 2 plot the odds ratios from Panels A and B to ease interpretation of findings. All analyses were conducted using R version 4.2.2 and the survey package [39] to incorporate NHIS sample weights.
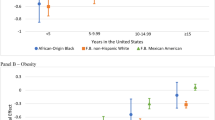
Odds ratios of diagnosed health conditions among whites by nativity status with 95% confidence intervals, National Health Interview Survey 2019–2022
Note: Odds ratios derived from logistic regression models in Table 2, Panel B. The unadjusted models include nativity status (Model 1) and the adjusted models include all covariates (Model 2)
Results
As seen in Table 1, foreign-born respondents report fewer self-reported and diagnosed health conditions than do US-born Whites, which provides initial evidence of a nativity gap in health among Whites (RQ1). Further, the prevalence of disease and size of the nativity gap varies across the six outcomes (RQ2). For self-reported conditions, one in five (19.8%) US-born Whites report experiencing depression and one in four (25%) report experiencing anxiety, compared to 14.2% and 19.5% of the foreign-born, respectively. One in ten (11.3%) US-born Whites also rate their health as “fair or poor” compared to 7.7% of foreign-born Whites. The prevalence for diagnosed conditions is highest for hypertension, with one-fourth of US-born and one-fifth of foreign-born Whites reporting being diagnosed with high blood pressure. The prevalence of diabetes and chronic obstructive pulmonary disease (COPD) are lower, as are the nativity gaps: 6.3% of US-born and 5.1% of foreign-born Whites report being diagnosed with diabetes and 4.2% and 2.5% with COPD. Though smaller, the nativity gaps for these conditions are significant.
Turning to explanatory factors, foreign-born Whites have relatively high levels of educational attainment and are bifurcated in terms of poverty status, with higher concentrations in the lowest and highest levels of poverty. There is no significant variation by nativity status for health insurance coverage, having a usual place of care, or having seen a provider in the past year. US-born Whites are more likely to be overweight or obese and be current smokers, while foreign-born Whites are more likely to be currently married, have a minor in the home, and live in the Northeast and West regions. The age and gender composition of US- and foreign-born Whites are similar, with a mean age of approximately 45 years and an equal distribution of males and females.
Table 2 presents odds ratios from logistic regression models assessing differences in self-reported (Panel A) and diagnosed conditions (Panel B). Panel A shows that the immigrant health advantage seen in Table 1 remains significant in the multivariable context and is largely impervious to adjustment for sociodemographic and healthcare factors. For example, foreign-born Whites have 37% lower odds of depression in the baseline model (OR = 0.67; CI = 0.59, 0.77) that decreases to 27% but remains significantly lower than US-born Whites in the fully adjusted model (OR = 0.73; CI = 0.61, 0.86). Changes in the nativity gap for anxiety are even smaller, decreasing from 27% lower odds in Model 1 to 23% in Model 2 (OR = 0.73; CI = 0.64, 0.83 and OR = 0.77, CI = 0.66, 0.90).
Changes in the odds of fair/poor self-rated health are most affected by the inclusion of covariates; in the unadjusted Model 1, foreign-born Whites have a 35% lower odds of reporting fair/poor health (OR = 0.65, CI = 0.55, 0.79) that drops in size and significance after adjustment for covariates (OR = 0.81, CI = 0.64–1.01). Figure 1 eases interpretation by graphing the unadjusted and adjusted odds ratios for each condition. As seen in the figure, foreign-born Whites have lower unadjusted odds of depression, anxiety, and fair/poor self-rated health that remain significantly lower than US-born Whites after the inclusion of control variables. The biggest change is for self-rated health, where the inclusion of covariates reduces the foreign-born advantage by nearly one-half. The overall pattern in Fig. 1 indicates that compositional heterogeneity in sociodemographic and healthcare factors, alone, do not fully account for the nativity gap in self-reported outcomes (RQ3).
For diagnosed medical conditions (Panel B), the immigrant advantage for diabetes and COPD seen in Table 1 disappears and is no longer statistically different from that of US-born Whites in the fully adjusted model (OR = 1.07; CI = 0.63, 1.41 for diabetes; OR = 0.88; CI = 0.60, 1.29 for lung disease). Hypertension is the only diagnosed condition where foreign-born Whites have a lower odds of diagnoses (OR = 0.70; CI = 0.62, 0.79) that remains robust after adjustment for covariates (OR = 0.78; CI = 0.66, 0.91). Figure 2 simplifies interpretation of the findings by graphing the results for each of the diagnosed conditions. As seen in the figure, the foreign-born advantage evidenced for self-reported health conditions (Fig. 1) is considerably smaller and not statistically different from US-born Whites, especially in the case of diabetes and COPD. Hypertension stands out in that the odds of reporting a diagnosis remains significantly lower for foreign-born Whites in the fully adjusted analysis.
Discussion
Inequality research often uses US-born, non-Hispanic Whites as the reference group to measure US health disparities, with less attention paid to diversity among Whites, particularly White immigrants. White immigrants make up a sizable portion (17%) of the US foreign-born population, yet are surprisingly absent in the overwhelming majority of research on US racial/ethnic inequality [4], immigrant health [24], and even in studies that examine Whiteness and White racial identity [40]. The current study addresses these oversights by disaggregating US Whites by nativity status and examining differences in six measures of health that tap into dimensions of mental and physical well-being. I used one of the only nationally-representative datasets available (NHIS) that contains detailed information on nativity and health status, with large enough sample sizes of White immigrants for analyses.
The results found an overall pattern of better health among White immigrants compared to US-born Whites, which is similar to findings of an ‘immigrant health advantage’ for other racial/ethnic groups but counter to studies that find little to no health advantage for specific White subgroups, such as Arab Americans [33]. One plausible explanation is that the foreign-born White category contains other large ethnic groups, namely Europeans, which contributes to overall averages in White immigrant health. These averages, in turn, can mask within-group heterogeneity among White immigrants. Indeed, prior studies that disaggregate White immigrants by region of birth lend support to this possibility [20, 21]. Unfortunately, the NHIS dropped the region of birth question in 2018, which I discuss in more detail below.
Beyond the general pattern of better health, there was diversity in the size of the health gap between US- and foreign-born Whites depending on the health measure in question. The efficacy of sociodemographic and healthcare factors in explaining health gaps also varied by health condition. For self-reported conditions–depression, anxiety, and fair/poor self-rated health–foreign-born Whites had a health advantage over US-born Whites that remained significant after adjustment for covariates. In fact, the odds of reporting better health were remarkably similar in the baseline and fully adjusted models, suggesting that compositional differences in sociodemographic and healthcare characteristics were not responsible for health gaps between foreign- and US-born Whites, at least not for these health conditions.
Findings for diagnosed health conditions, which required interaction with the healthcare system, were slightly more complex. First, the prevalence of diabetes and chronic obstructive pulmonary disease (COPD) were relatively low when compared with hypertension, likely due to the age composition of the sample that excluded later stages of the life course when disease prevalence is highest. Second, the inclusion of covariates reduced the nativity gap to non-significance for diabetes and COPD but did little to alter the gap in diagnosed hypertension. Symptoms associated with diabetes and COPD are more noticeable than those for hypertension, and thus may motivate health-seeking behaviors for treatment that reduce between-group disparities. Findings for hypertension were similar to those for depression, anxiety, and fair/poor self-rated health (i.e., self-reported health conditions) in that standard explanations for health disparities did not account for the better health of foreign-born Whites. These results suggest that other mechanisms not observed in the current study may be contributing to health disparities in conditions that are harder to detect (e.g., hypertension, depression).
This study is not without limitations. First, I was unable to disaggregate White immigrants by region or country of birth due to the removal of region of birth in the 2019 NHIS survey redesign. I attempted to account for this shortcoming by using duration of US residence and immigrant arrival cohort as proxy measures for region of birth but found that sample sizes were too small for meaningful analyses (e.g., 71% of foreign-born whites had resided in the US for 15 years or more, analyses available on request). It is worth noting that the redesign also affects studies that used restricted data to examine specific country-of-origin groups. Second, the current study focused on non-Hispanic Whites and excluded a smaller but growing number of Whites who identify as Hispanic. The decision was purposeful and aimed at disrupting the long-standing practice of using non-Hispanic Whites as a benchmark for measuring US racial/ethnic health disparities [41]. Moving forward, research will need to consider the role of Hispanic ethnicity in analyses of White health, especially as overall growth in the US White population is projected to result, in part, from increases in Whites of Hispanic ethnicity [15].
Conclusions
White immigrants are projected to grow to 20% of the US foreign-born population and 7% of the White population by 2060 [15], thus understanding diversity among Whites is crucial for knowledge on racial, ethnic, and immigrant health disparities. This study focuses on this question and makes several contributions to existing research. By focusing on non-Hispanic Whites, I extend recent work that underscores ethnic heterogeneity within US racial groups, most of which has concentrated on racial and ethnic minorities [4]. I also challenge the practice of using non-Hispanic Whites as a reference group to measure racial gaps in health. The practice emerged in a time of greater ethnic homogeneity among Whites (i.e., western European) and should be used with caution moving forward, especially when examining trends over time. Studies that fail to consider compositional changes among Whites could yield biased or misleading estimates of progress (or the lack thereof) toward racial/ethnic equity. Policy decisions that are based on racial comparisons are likewise implicated in findings from this study. Future research will need to continue monitoring the composition of US Whites to better specify the conditions that contribute to within- and between-group racial health disparities.
Notes
OMB Directive 15 defined race separately from Hispanic origin and established five standard categories for collecting and analyzing: White, not Hispanic; Black, not Hispanic; Hispanic, any race; Asian or Pacific Islander; and American Indian or Alaska Native.
In 2019, the NHIS underwent a major redesign with a new structure and content that prevents comparisons with prior survey years.
Focusing on this age group avoided potential confounders associated with retirement or enrollment in higher education, and sensitivity analyses with other age groupings yielded substantively similar findings.
References
Ward N, Batalova J. (2023) Frequently requested statistics on immigrants and Immigration in the United States. In: Migr Policy Inst. https://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states#demographic-educational-linguistic
Census Bureau US. (2023) 2022 American Community Survey 1-Year Estimates Press Kit. https://www.census.gov/newsroom/press-kits/2023/acs-1-year-estimates.html
Khullar D, Chokshi DA. Challenges for immigrant health in the USA—the road to crisis. Lancet. 2019;393:2168–74. https://doi.org/10.1016/S0140-6736(19)30035-2
Kauh TJ, Read JG, Scheitler AJ. Popul Res Policy Rev. 2021;40:1–7. https://doi.org/10.1007/s11113-020-09631-6. The Critical Role of Racial/Ethnic Data Disaggregation for Health Equity.
Jiang JJ, Adia AC, Nazareno J, et al. The Association between Moderate and Serious Mental Health Distress and General Health Services utilization among Chinese, Filipino, Japanese, Korean, and Vietnamese adults in California. J Racial Ethn Health Disparities. 2022;9:227–35. https://doi.org/10.1007/s40615-020-00946-w
Hamilton TG. Black immigrants and the Changing Portrait of Black America. Annu Rev Sociol. 2020;46:295–313. https://doi.org/10.1146/annurev-soc-121919-054728
Lopez MH, Moslimani M. (2024) Key facts about the nation’s 47.9 million Black Americans. https://www.pewresearch.org/short-reads/2024/01/18/key-facts-about-black-americans/
Ro A, Geronimus A, Bound J, et al. Cohort and duration patterns among Asian immigrants: comparing trends in obesity and self-rated health. Biodemography Soc Biol. 2015;61:65–80. https://doi.org/10.1080/19485565.2014.950721
Marquez-Velarde G, Miller GH, Ma G, Keith VM. Psychological distress among black immigrants by region of birth. J Immigr Minor Health. 2022;24:368–75. https://doi.org/10.1007/s10903-021-01203-w
Reynolds MM, Chernenko A, Read JG. Region of origin diversity in immigrant health: moving beyond the Mexican case. Soc Sci Med. 2016;166:102–9. https://doi.org/10.1016/j.socscimed.2016.07.018
Bulut E, Brewster KL. Psychological distress in middle eastern immigrants to the United States: a challenge to the healthy migrant model? Soc Sci Med. 2021;274:1–13. https://doi.org/10.1016/j.socscimed.2021.113765
Xi J, Takyi B, Lamptey E. Are recent immigrants larger than earlier ones at their arrival? Cohort variation in initial BMI among US immigrants, 1989–2011. J Immigr Minor Health. 2015;17:1854–62. https://doi.org/10.1007/s10903-014-0129-1
Tang Z, Du S. Revisiting the Immigrant Health Advantage: self-reported health and smoking among sexual minority immigrants. J Immigr Minor Health. 2023. https://doi.org/10.1007/s10903-023-01527-9
Pew Research Center, U.S. (2015) Modern Immigration Wave Brings 59 Million to, Driving Population Growth and Change Through 2065: Views of Immigration’s Impact on U.S. Society Mixed. https://www.pewresearch.org/hispanic/2015/09/28/chapter-1-the-nations-immigration-laws-1920-to-today/
Vespa J, Medina L, Armstrong DM. Demographic turning points for the United States: Population projections for 2020 to 2060. Washington, DC: U.S. Census Bureau; 2020.
Office of Management and Budget. Revisions to the standards for the classification of Federal Data on Race and Ethnicity. Office of Management and Budget; 1997.
Hixson L, Hepler BB, Kim MO. The White Population: 2010–2010 Census briefs. Washington, DC: US Department of Commerce, Economics and Statistics Administration; 2011.
Farley R. The new census question about ancestry: what did it tell us? Demography. 1991;28:411–29. https://doi.org/10.2307/2061465
Budiman A, Tamir C, Mora L, Noe-Bustamante L. (2018) Facts on U.S. immigrants, 2018: statistical portrait of the foreign-born population in the United States. In: Pew Res Cent. https://www.pewresearch.org/hispanic/2020/08/20/facts-on-u-s-immigrants-current-data/
Read JG, West JS, Kamis C. Immigration and health among non-hispanic whites: the impact of arrival cohort and region of birth. Soc Sci Med. 2020;246:1–9. https://doi.org/10.1016/j.socscimed.2019.112754
Engelman M, Kestenbaum BM, Zuelsdorff ML, et al. Work disability among native-born and foreign-born americans: on origins, Health, and Social Safety Nets. Demography. 2017;54:2273–300. https://doi.org/10.1007/s13524-017-0617-8
Harjanto L, Batalova J. (2022) Middle Eastern and North African immigrants in the United States. In: Migr Policy Inst. https://www.migrationpolicy.org/article/middle-eastern-and-north-african-immigrants-united-states#english-proficiency
Ro A, Fleischer NL, Blebu B. An examination of health selection among U.S. immigrants using multi-national data. Soc Sci Med. 2016;158:114–21. https://doi.org/10.1016/j.socscimed.2016.04.023
Feliciano C. Immigrant selectivity effects on health, labor market, and educational outcomes. Annu Rev Sociol. 2020;46:315–34. https://doi.org/10.1146/annurev-soc-121919-054639
Zhou M, Mahmud H. Beyond economic migration: social, historical, and political factors in US immigration. New York: New York University; 2023.
Awad GH, Abuelezam NN, Ajrouch KJ, Stiffler MJ. Lack of arab or middle eastern and north African Health data undermines Assessment of Health disparities. Am J Public Health. 2022;112:209–12. https://doi.org/10.2105/AJPH.2021.306590
Maghbouleh N, Schachter A, Flores RD. Middle Eastern and North African americans may not be perceived, nor perceive themselves, to be White. Proc Natl Acad Sci. 2022;119:e2117940119. https://doi.org/10.1073/pnas.2117940119
Abuelezam NN, El-Sayed AM, Galea S, Gordon NP. Health risks and Chronic Health conditions among arab American and white adults in Northern California. Ethn Dis. 2021;31:235–42. https://doi.org/10.18865/ed.31.2.235
Dallo FJ, Borrell LN. Self-reported diabetes and hypertension among arab americans in the United States. Ethn Dis. 2006;16:699–705.
Dallo FJ, Kindratt TB. Disparities in Chronic Disease Prevalence among non-hispanic whites: heterogeneity among Foreign-Born Arab and European americans. J Racial Ethn Health Disparities. 2016;3:590–8. https://doi.org/10.1007/s40615-015-0178-8
Read JG, Ajrouch KJ, West JS. Disparities in functional disability among arab americans by nativity, immigrant arrival cohort, and country of birth. SSM - Popul Health. 2019;7:1–9. https://doi.org/10.1016/j.ssmph.2018.100325
Kindratt TB, Dallo FJ, Zahodne LB, Ajrouch KJ. Cognitive limitations among Middle Eastern and North African immigrants. J Aging Health. 2022;34:1244–53. https://doi.org/10.1177/08982643221103712
Read JG, Amick B, Donato KM. Arab immigrants: a new case for ethnicity and health? Soc Sci Med. 2005;61:77–82. https://doi.org/10.1016/j.socscimed.2004.11.054
Yi S, Elfassy T, Gupta L, et al. Nativity, Language spoken at home, length of Time in the United States, and Race/Ethnicity: associations with Self-reported hypertension. Am J Hypertens. 2014;27:237–44. https://doi.org/10.1093/ajh/hpt209
Mehta NK, Elo IT. Migrant selection and the Health of U.S. immigrants from the Former Soviet Union. Demography. 2012;49:425–47. https://doi.org/10.1007/s13524-012-0099-7
Xu J, Murphy S, Kochanek K, Arias E. (2022) Mortality in the United States, 2021. National Center for Health Statistics (U.S.).
CDC. (2021) High Blood Pressure Symptoms and Causes. https://www.cdc.gov/bloodpressure/about.htm
CDC. (2023) Chronic Obstructive Pulmonary Disease (COPD). https://www.cdc.gov/copd/basics-about.html
Lumley T. Survey: analysis of complex survey samples. J Stat Soft. 2023;9:1–19. https://doi.org/10.18637/jss.v009.i08
McDermott M, Ferguson A. Sociology of whiteness. Annu Rev Sociol. 2022;48:257–76. https://doi.org/10.1146/annurev-soc-083121-054338
U.S. Department of Health and Human Services. 2022 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr22/index.html
Acknowledgements
This study was supported by a Pilot Grant from the Center for Population Health and Aging (CPHA) and support from the Centers on the Demography and Economics of Aging Program award number P30 AG034424 by the Division of Behavioral and Social Research at the National Institute on Aging for research. The author would like to thank Turgut Keskintürk, PhD student in the Department of Sociology at Duke University, for assistance with the analysis and results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The author has no competing interests and no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Read, J.G. Does an Immigrant Health Advantage Exist Among US Whites? Evidence from a Nationally-Representative Examination of Mental and Physical Well-Being. J Immigrant Minority Health (2024). https://doi.org/10.1007/s10903-024-01607-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s10903-024-01607-4