Abstract
During the last years, Greece has become the entry point of a high number of migrants and asylum seekers. The aim of this study was to assess the access to selected fields of primary healthcare, to emergency medical care, secondary healthcare and essential medicines among populations living in reception, temporary accommodation, and detention centres (migrant camps) in Greece. An online cross-sectional survey was conducted based on a self-administered questionnaire. Participants included indviduals working or volunteering in migrant camps in Greece. 64 individuals participated in this study. The most common health problem among people residing in migrant camps was mental health conditions. The access to each field of primary healthcare was assessed as minimum to non-existent by most of the participants. 47.2% assessed the access to emergency medical care as minimum/non-satisfactory, while 60.8% assessed the access to secondary healthcare as minimum to non-existent. Most participants assessed the access to all the medicines categories as minimum or moderate. Access to both primary and secondary health was given a lower grade in the East-Aegean islands compared to the mainland. Major health inequalities among populations residing in Greek migrant camps were highlighted in this study. A change in the current migration policies of Greece and the European Union is urgently needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last two decades, the numbers of forcibly displaced populations have dramatically increased worldwide, from 33.9 million in 1997 to 65.6 million0 in 2016 and 82.4 million in 2020. The most common causes of such population movements are the long-term conflicts and violence in countries such as Syria, Afghanistan, Iraq, South Sudan, and Sudan [1] [2]. From 2014 onwards, a significantly increased number of forcibly displaced populations have been risking their lives in their effort to reach the south European coasts, while European countries face a phenomenon with political, social, humanitarian, and public health implications [3]. Only in 2015, 857.363 immigrants and asylum seekers reached Greece [4]. To respond to these numbers, the first accommodation centres, also called “hotspots”, were created in Greek islands in the same year [5]. People entering Greece were first routed to reception and identification centres. Following the required identification and registration procedures, those eligible for asylum were moved to temporary accommodation centres in the mainland. From there, refugees could resume their journey in Europe, most often to countries such as Germany, Austria, and Sweden [6] [7] [8]. However, several international developments, including the EU-Turkey deal, the (partial) border closure and fence building by several countries, led to the confinement of thousands of people in overcrowded centres, which were initially built to accommodate a much lower number of people only temporarily [6] [9] [10].
The National Healthcare Service (NHS) in Greece was already exhausted from the several years of economic crisis and strong austerity measures preceding the increased influx of migrants. The arrival of immigrants and their needs for healthcare provision only highlighted the existing gaps in healthcare [7] [8] [11]. As a result, several Non-Governmental Organisations (NGOs) offered healthcare and humanitarian assistance to the incoming populations, along with the local authorities [7].
Greece was not prepared to bear the increased burden on the NHS imposed by the large number of incoming populations seeking asylum, in combination with the ongoing effects of the economic crisis [8]. According to the World Health Organisation (WHO), immigrants’ and refugees’ health is generally complicated and affected by numerous factors in the countries of origin and destination, as well as during the journey [12]. Immigrants and refugees usually undertake dangerous journeys leaving their country of origin, and those who do arrive in Greece must often live under poor conditions [13]. The aim of the present study was to assess the level of access to selected fields of primary healthcare services, to emergency medical care, secondary healthcare services and essential medicines, as published by the WHO [14], among populations residing in reception and identification, temporary accommodation, and detention centres (further referred to as migrant camps) in Greece.
Methods
Study Design, Participants, and Procedure
This was a cross-sectional study. The referent population included healthcare and non-healthcare professionals working or volunteering in at least one migrant camp in an island or the mainland of Greece. Inclusion criteria were English language literacy, working or volunteering experience in a migrant camp in Greece, willingness to complete the questionnaire and agreement with the terms of use of provided data.
The data were collected using an online self-administered questionnaire. Data collection lasted from 20 September 2019 up to and including the 30 April 2020. The self-administered questionnaire was uploaded on a survey platform (SurveyMonkey Inc., San Mateo, California, USA), which could be accessed by the participants through a link. It was not possible to estimate the total number of individuals working/volunteering in migrant camps in Greece. Therefore, convenience sampling was used to approach the sample of this study. Specific organisations (governmental and non-governmental) active in providing healthcare services in Greek migrant camps and individuals from the network of the researchers were contacted and asked to participate and further forward the questionnaire to their networks. The online questionnaire was also distributed through social media, and particularly to groups popular among individuals offering healthcare and/or non-healthcare-related services to migrant/refugee populations in Greece.
Instruments and Outcomes
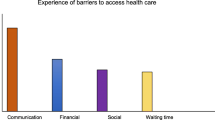
First, a pilot qualitative study was conducted, to identify the major healthcare fields with problematic access in Greek migrant camps. This included three in-depth interviews with three individuals with working/volunteering experience in Greek migrant camps. Interviews were conducted in Greek and included open-end questions, concerning the main barriers and inequalities that were identified in the literature. After transcription of the interviews and content analysis, four fields were identified, the access to which would be studied in the questionnaire: primary healthcare, secondary healthcare, emergency healthcare, and essential medicines. For primary healthcare, eight fields were identified: access to physician, paediatrician, dentist, midwife, family planning and contraception services, antenatal and perinatal care, neonatal care, and psychologist. Furthermore, five main barriers to primary healthcare were highlighted: understaffing, lack of satisfactory facilities, language/lack of translator, cultural barriers, and lack of knowledge regarding procedures. Additionally, 5 main barriers to secondary healthcare emerged: language/lack of translator, cultural barriers, lack of knowledge regarding procedures, location-inability to reach the secondary healthcare facility and long waiting times.
The questions of the questionnaire were first written in Greek. Translation and back-translation followed to ensure accuracy. Content validity was evaluated by an experts panel that evaluated the questionnaire, based on its clarity, completeness, accuracy, relevance, neutrality, and specificity.
The questionnaire consisted of seven sections and contained 49 closed-ended questions. The first section included socio-demographic questions and one question regarding the most common health problem inside the camp. The second section included questions regarding access to the identified fields of primary healthcare. The available answers were based on a 5-point Likert scale. Additionally, the choice “Not applicable” was available for participants with no knowledge/experience in the respective area. The third section included questions regarding the most common barriers to respective primary healthcare fields. The next section included questions regarding access to emergency medical care (5-point Likert scale and “Not applicable” option, as described above) and the average waiting time after calling for an ambulance. The fifth section included questions regarding access to secondary healthcare (5-point Likert scale and “Not applicable” option, as described above), the most common barriers (possibility to choose more than one answers and/or choose “Other” and use the free-text field, as described above) and the waiting time for identification as “vulnerable” and transfer to a specialised medical care facility, according to the respective needs. The following section concerned access to essential medicines (5-point Likert scale and “Not applicable” option, as described above), as published by the World Health Organisation [14]. In the last section, participants were asked to grade access to primary and secondary healthcare services, respectively, from 1 to 10 (Supplementary file 1).
Statistical Analysis
Continuous variables with normal distribution are presented as mean ± standard deviation (SD) while continuous variables with not normal distribution as median (IQR). All types of access were evaluated based on a 5-point Liker scale (“no access”, “minimum/non-satisfactory”, “moderate”, “satisfactory”, “full access”).
Results
Sample Characteristics and Most Common Health Problems in Migrant Camps
The online survey was visited 97 times and was completed by 64 individuals, who participated in the study and filled in either the whole or part of the questionnaire. The socio-demographic characteristics of the sample are presented in Table 1. The mean age was 38.6 ± 12.9 years. Most of the participants (40.6%) belonged to the age group of 31–40 years, and almost half of them had Greek nationality (46.9%). Most worked in a Reception and Identification or a Temporary Accommodation Centre (42.2% and 53.1%, respectively). The majority of participants (73.4%) worked at an NGO, while 88.2% of the participants working at a Governmental Organisation (GO) had Greek nationality. Respondents were distributed between the mainland (53.1%) and East-Aegean islands (46.9%). More than half of the sample (60.9%) had healthcare-related roles. Mental health conditions emerged as the most common health problem among people residing in migrant camps (56.3%). Communicable diseases were the next most prevalent response (29.7%). Non-communicable diseases followed (7.8%), while 4.7% of the respondents stated that the did not know.
Access to Primary Healthcare
The majority assessed the access to a physician, paediatrician, midwife, psychologist, and antenatal and perinatal care as minimum/non-satisfactory (50.9%, 42.1%, 33.3%, 42.1% and 42.1%, respectively), while access to a psychologist was assessed as minimum or non-existent by 64.9% of the respondents. Most stated that there was no access to a dentist, family planning and contraception advice services and neonatal care (50.9%, 36.8% and 43.9%, respectively). Regarding the main barriers to primary healthcare, the most common ones for all fields were understaffing (ranging from 49.1 to 75.4%) and lack of satisfactory facilities (ranging from 31.6 to 59.6%) (Table 2). With a total of 49 respondents, the median grading of primary healthcare services was 5 (IQR 3–7).
Access to Emergency Medical Care and Secondary Healthcare
A total of 47.2% of the respondents assessed the access to emergency medical care as minimum/non-satisfactory. The average waiting time after calling for an ambulance was more than 30 min according to 61.5% of the respondents (Table 3). The access to secondary healthcare was minimum or non-existent for 60.8% of the respondents, with the most common barriers being location/inability to reach the secondary healthcare facility (60.8%), language/lack of translator and long waiting times (56.9) (Table 3). As regards to the waiting time for identification as “vulnerable”, 27.5% and 29.4%, stated that this was less than 6 months and 6–12 months, respectively (Table3). With a total of 49 respondents, the median grading of access to secondary healthcare was 3 (IQR 2–6).
Access to Essential Medicines
For each category of medicines, access was assessed as minimum by most of the respondents (ranging from 26.0 to 54.0%), except for solutions correcting water, electrolyte and acid–base disturbances, the access to which was assessed as moderate by the majority (28.0%). Non-existent access was the highest for medicines for mental and behavioural disorders (34.0%), vitamins and minerals (24.0%), vaccines (24.0%) and ophthalmological preparations (20%) (Table 4).
Differences Based on the Location of the Camp and the Type of Organisation
The median grades of both primary and secondary healthcare services was lower in East-Aegean islands (3 and 2, respectively) compared to the mainland (6 and 5, respectively). Similarly, the median grades of both primary and secondary healthcare services were lower from respondents working at an NGO (4 and 2.5, respectively), compared to a GO (7 and 6, respectively) (Supplementary Table 1).
Discussion
This study aimed to assess the access to selected categories of healthcare and to essential medicines, among populations residing in migrant camps in Greece. Most respondents assessed access to each studied field of primary healthcare as minimum/non-satisfactory, or non-existent. Similar findings were made for access to emergency medical care and secondary healthcare, with most of the respondents assessing them as minimum/non-satisfactory. Access to essential medicines also appeared problematic, with most of the respondents assessing it as minimum or moderate for each medicine category.
This study’s results highlighted mental health conditions as the most common health problem among people residing in Greek migrant camps. This is not a surprising finding, as 3–4% of adult populations affected by emergencies will experience a severe and 15–20% a mild/moderate mental disorder 12 months after the emergency [15]. High prevalence of mental health conditions has also been reported among individuals residing in the Calais and Moria migrant camps [16] [17], as well as refugees/asylum seekers residing in different countries outside their country of origin [18]. This finding underlines the urgent need of access to psychological services among migrant populations, during what has been described as a mental health crisis [19] [20]. Alarmingly, more than half of the respondents stated that access to a psychologist is either minimum or non-existent.
The herein reported low rates of access to selected fields of primary healthcare and the identified barriers to primary healthcare among migrants/refugees in Greece, have also been observed in other studies [6] [21], while socio-cultural differences and changes in the healthcare provisions over time have also been reported [22]. Of note, the overall grading of access to primary healthcare was lower in East-Aegean islands, compared to the mainland. These findings are in line with the results of a recent research, that reported significant understaffing in severely overpopulated migrant camps on Greek islands, with some camps even operating with no doctors or midwifes on-site [23].
Secondary healthcare provision to individuals residing in migrant camps is a more complicated process, as it is highly regulated by the Greek law and is provided in healthcare facilities outside the camp. Almost 2/3 of the respondents assessed the access to secondary healthcare as minimum to non-existent. Although quantitative data are not available on this topic, the struggles of asylum seekers, immigrants, and refugees in accessing healthcare services in Greece have been thoroughly described and justify this study’s observations. Bureaucracy, austerity, understaffing, gaps in laws and regulations and changes in immigration policies over the years, have left vulnerable individuals, asylum seekers, unaccompanied children and children born in Greece from parents with irregular status having no access to public health services and treatment for chronic illnesses [24] [25]. The most common barriers to secondary healthcare in this study have also been identified in literature focusing on the refugee populations in Greece [7] [8]. It comes as no surprise that access to secondary healthcare was given a lower grade from participants in East-Aegean islands, compared to the mainland. Healthcare services on Greek islands had already been significantly compromised due to the long-lasting austerity [26] and only deteriorated following the large influx of asylum seekers and the creation of migrant camps [8] [23] [27]. Important to note is the fact that Greek islands host a disproportionate number of asylum seekers, compared to the mainland [23].
Interestingly, access to both primary and secondary healthcare were given a lower grade from participants working at NGOs, compared to GOs. This finding may reveal the increased struggles NGOs face to provide healthcare in migrant camps. Several NGOs have reported difficulties in the creation and maintenance of registrations in Greece, referring to the high costs, increased bureaucracy, and inability to provide and maintain expensive high-quality healthcare [7]. Of note, most participants working at a GO had a Greek nationality. It can be assumed that many of them had experience working under governmental projects and may have given higher grades due to their long-term customisation and adjustment within the Greek NHS.
Another concerning finding of this study relates to the access to emergency medical care, which was assessed as minimum by almost half of the of the respondents, while more than half stated that the average waiting time after calling an ambulance exceeded 30 min. Although no quantitative data are available in the literature to the best of our knowledge, the Emergency Medical Service in Greece has been deeply affected by the long austerity, a problem that is more prominent in rural areas and islands [28] and supports this study’s observations.
The access to essential medicines was not satisfactory, as assessed by the majority of this study’s participants. Higher percentages for no access were recorded for medicines for mental and behavioural disorders, vitamins and minerals, ophthalmological preparations, and vaccines. To the best of our knowledge, there are no quantitative data on this topic, and considering the number of individual medicines included in each category, it is difficult to compare our results with those of other sources. Nevertheless, unvaccinated individuals have been identified in refugee camps in Turkey [29]. As there is a high variability among the incoming populations, regarding the country of origin and age, the vaccination status of migrants is often insufficient, based on the vaccination policies in the countries of destination [30] [31] [32]. This fact further highlights the need for full access to essential vaccines, especially considering the living conditions in overpopulated camps and the resulting easy transmission of vaccine-preventable diseases. The inefficient access to medicines for mental and behavioural disorders and the reported high prevalence of mental health disorders is another alarming observation of this study.
The significance of the current study lies in the collected quantitative data on an important and pressing matter that is mainly studied qualitatively in the literature. Our results revealed the overall inefficient healthcare coverage of individuals residing in overpopulated migrant camps in Greece. Attention needs to be given by Greek governments, which should acknowledge the urgency of comprehensive and inclusive laws and regulations on healthcare provision to vulnerable individuals, asylum seekers and refugees. Furthermore, the European Union needs to adjust its views and policies on the urgent matter of migration, realising that this phenomenon will persist for years to come, thus short-term emergency plans are no longer suitable for its management. It is obvious and largely acknowledged that the detention of migrants, asylum seekers and refugees in overpopulated camps is not sustainable. This becomes even more apparent, following the recent fire in the infamous Moria camp, which left thousands vulnerable in the face of no water supply, sewage system, proper hygiene, and medical care during the global COVID-19 pandemic [33].
The education of health professionals treating people in transit is critical and shall address health issues typical in populations residing in other parts of the world, as well as cultural differences, and managing special situations, such as post-traumatic stress disorder and human trafficking. Such education programmes are available in Australia, the USA and Canada [34,35,36]. Digital tools should also be considered, as they can provide an efficient and often cost-effective way for people in transit to address some of their problems and potentially educate themselves on their rights. A smartphone-based, self-help app was created in the Arabic language and was evaluated in refugees with post-traumatic stress [37]. While digital tools can be a cost-effective and efficient way to assist the needs of populations in transit, attention should be given to the accessibility of such tools and digital literacy in the target population.
Further larger studies are needed to better describe, understand, and manage this complicated and multifactorial issue. The gaps in all levels and types of healthcare should be investigated in parallel with the health status, morbidity, and mortality rates among the migrant camps’ residents. Additionally, the unsatisfactory access to essential medicines should be studied in combination with the morbidity levels, especially including chronic illnesses and the potential lack of treatment while in the camps.
This study revealed some interesting findings regarding access to healthcare services and essential medicines among people residing in Greek migrant camps. However, it has the following limitations. The sample size was small, as the targeted population was hard to reach, and the often-busy schedule of potential participants made them less eager to fill in our questionnaire. The response rate of this online survey cannot be estimated since it is not possible to ascertain how many individuals might have seen the survey or its links but declined to participate. The selection bias is also acknowledged, as the individuals willing to participate are likely to have a more critical view on the access of migrants to healthcare and consider this as a significant problem. This online survey collected healthcare access information by individuals with healthcare-related and non-healthcare-related roles. It must be acknowledged that the former might be biased, as they are also partly assessing their own services. Additionally, the barriers described herein only relate to the healthcare services that are indeed available to migrants. The perspective of the affected individuals (migrants) could provide further views of barriers not addressed in this study’s results. The questionnaire was only available in English, for convenience reasons, which might have inhibited some individuals from participating in the study and potentially lowered the number of the sample. Most respondents worked at NGOs, due to significant difficulties in getting in contact with the respective GOs. Also, the study’s participants had different educational backgrounds, i.e., not all were medically trained. Finally, although a “Not applicable” option was always available, we cannot be sure that all respondents had full knowledge of the topic they were commenting on.
Conclusion
The results of this study revealed important health inequalities and lack of access to critical fields of healthcare and essential medicines among populations residing in migrant camps in Greece. Comprehensive changes in the migration policies and regulations are urgently needed in Greece and the European Union, along with the decongestion and improvement of living conditions in Greek migrant camps and the efficient staffing of medical care positions. Furthermore, efficient communication and collaboration between all bodies involved in the reception and accommodation of migrant populations is necessary.
Data Availability
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
References
UNHCR, “Global Trends. Forced Displacement in 2016”. https://www.unhcr.org/5943e8a34.pdf. Accessed 03 Sep 2021.
UNHCR, “Global Trends. Forced displacement in 2020”. https://www.unhcr.org/60b638e37/unhcr-global-trends-2020. Accessed 03 Sep 2021.
UNHCR, “The sea route to Europe: The Mediterranean passage in the age of refugees”. 2015 https://www.unhcr.org/5592bd059.pdf. Accessed 03Sep 2021.
IOM, “Mixed Migration Flows in the Mediterranean and Beyond. Compilation of available data and information. Reporting period 2015.” https://www.iom.int/sites/g/files/tmzbdl486/files/situation_reports/file/Mixed-Flows-Mediterranean-and-Beyond-Compilation-Overview-2015.pdf. Accessed 03 Sep 2021.
GCR. “Reception and identification procedure. Greece. The European Union policy framework: ‘hotspots’.” 2021. https://asylumineurope.org/reports/country/greece/asylum-procedure/access-procedure-and-registration/reception-and-identification-procedure/. Accessed 03 Sep 2021.
Blitz BK, d’Angelo A, Kofman E, Montagna N. Health challenges in refugee reception: dateline europe 2016. Int J Environ Res Public Health. 2017;14(12):1484.
Gunst M, Jarman K, Yarwood V, Rokadiya S, Capsaskis L, Orcutt M, et al. Healthcare access for refugees in Greece: challenges and opportunities. Health Policy. 2019;123(9):818–24.
Kotsiou OS, Kotsios P, Srivastava DS, Kotsios V, Gourgoulianis KI, Exadaktylos AK. Impact of the refugee crisis on the greek healthcare system: a long road to Ithaca. Int J Environ Res Public Health. 2018;15(8):1790.
Hermans MPJ, Kooistra J, Cannegieter SC, Rosendaal FR, Mook-Kanamori DO, Nemeth B. Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos Greece. Eur J Epidemiol. 2017;32(9):851–4.
MSF. “Obstacle Course to Europe: A Policy-Made Humanitarian Crisis at EU Borders”. 2016. https://www.msf.org/sites/msf.org/files/msf_obstacle_course_to_europe_0.pdf. Accessed 03 Sep 2021.
MIPEX. “Migrant Integration Policy Index - Health Strand - Country Report - Greece”. 2016. https://eea.iom.int/publications/mipex-health-strand-country-report-greece. Accessed 03 Sep 2021.
WHO. “Report on the health of refugees and migrants in the WHO European Region: no public health without refugee and migrant health”. 2018. https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846-eng.pdf?sequence=1&isAllowed=y. Accessed 03 Sep 2021.
Daynes L. The health impacts of the refugee crisis: a medical charity perspective. Clin Med (Lond). 2016;16(5):437–40.
WHO. “WHO model list of essential medicines, 20th list (March 2017, amended August 2017)”. 2017. https://apps.who.int/iris/bitstream/handle/10665/273826/EML-20-eng.pdf?sequence=1&isAllowed=y. Accessed 03 Sep 2021.
WHO. “Assessing mental health and psychosocial needs and resources - Toolkit for humanitarian settings”. 2012. https://apps.who.int/iris/bitstream/handle/10665/76796/9789241548533_eng.pdf?sequence=1. Last Accessed 03 Sep 2021.
Isakjee A, Dhesi S, Davies T. An environmental health assessment of the new migrant camp in Calais. Birmingham: University of Birmingham; 2015.
van de Wiel W, Castillo-Laborde C, Francisco Urzúa I, Fish M, Scholte WF. Mental health consequences of long-term stays in refugee camps: preliminary evidence from Moria. BMC Public Health. 2021;21(1):1290.
Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. 2020;17(9):e1003337.
MSF. “Overwhelmed: The mental health crisis among child refugees in Greece”. 2020. https://blogs.msf.org/bloggers/kate%C5%99ina/overwhelmed-mental-health-crisis-among-child-refugees-greece. Accessed 03 Sep 2021.
UNHCR. “Q&A: ‘Before the pandemic, refugee mental health was severely overlooked. Now it’s a full-blown crisis’.” 2020. https://www.unhcr.org/news/latest/2020/10/5f7ec72a4/qa-pandemic-refugee-mental-health-severely-overlooked-its-full-blown-crisis.html. Accessed 03 Sep 2021.
Hémono R, Relyea B, Scott J, Khaddaj S, Douka A, Wringe A. “The needs have clearly evolved as time has gone on.”: a qualitative study to explore stakeholders’ perspectives on the health needs of Syrian refugees in Greece following the 2016 European Union-Turkey agreement. Confl Health. 2018;12:1–9.
Joseph L (2018). Barriers to healthcare access for refugees in Greece. 11th European Public Health Conference: Poster walks. P. 407
RSA. “Structural failure: why Greece΄s reception system failed to provide sustainable solutions”. 2019. https://rsaegean.org/wp-content/uploads/2019/06/201906-STRUCTURAL-FAILURE-Why-Greece’s-reception-system-failed-f.pdf. Accessed 03 Sep 2021.
Amnesty International. “Amnesty International public statement - “Greece must immediately ensure that asylum-seekers, unaccompanied children and children of irregular migrants have free access to the public health system”.” 2019. https://www.amnesty.org/download/Documents/EUR2512132019ENGLISH.PDF. Accessed 03 Sep 2021.
Amnesty International. “Greece: resuscitation required – The Greek health system after a decade of austerity”. 2020. https://www.amnesty.org/en/documents/eur25/2176/2020/en/. Accessed 03 Sep 2021.
Oikonomidou E, Anastasiou F, Dervas D, Patri F, Karaklidis D, Moustakas P, et al. Rural primary care in Greece: working under limited resources. Int J Qual Health Care. 2010;22(4):333–7.
Kerasidou A, Kingori P, Legido-Quigley H. “You have to keep fighting”: maintaining healthcare services and professionalism on the frontline of austerity in Greece. Int J Equity Health. 2016;15(1):118.
Kotsiou OS, Srivastava DS, Kotsios P, Exadaktylos AK, Gourgoulianis KI. The emergency medical system in greece: Opening aeolus’ bag of winds. Int J Environ Res Public Health. 2018;15(4):745.
Tayfur I, Günaydin M, Suner S. Healthcare Service access and utilization among syrian refugees in Turkey. Ann Glob Health. 2019;85(1):42.
de Monléon JV, Regnier F, Ajana F, Baptiste C, Callamand P, Cheymol J, et al. Mise à jour des vaccinations de l’enfant arrivant de l’étranger (adopté, réfugié ou migrant) en France [Catch-up vaccination of worldwide newcoming (adopted, refugee or migrant) children in France]. Arch Pediatr. 2014;21(3):329–34.
Mipatrini D, Stefanelli P, Severoni S, Rezza G. Vaccinations in migrants and refugees: a challenge for European health systems a systematic review of current scientific evidence. Pathog Glob Health. 2017;111(2):59–68.
Nakken CS, Skovdal M, Nellums LB, Friedland JS, Hargreaves S, Norredam M. Vaccination status and needs of asylum-seeking children in Denmark: a retrospective data analysis. Public Health. 2018;158:110–6.
RSA. “Lesvos-Moria nightmare for thousands of refugees”. 2020. https://rsaegean.org/en/lesvos-moria-nightmare-for-thousands-of-refugees/. Accessed 03 Sep 2021.
Victoria State Government. Department of Health. Refugee and asylum seeker health and wellbeing. 2022. https://www.health.vic.gov.au/populations/refugee-and-asylum-seeker-health-and-wellbeing#refugee-and-asylum-seekers-health-and-wellbeing. Accessed 29 Jun 2022.
Harvard Program in Refugee Trauma. Global Mental Health: Trauma and Recovery Certificate Program. 2022. https://hprt-cambridge.org/education/gmh/overview/. Accessed 29 Jun 2022.
Immigrant and Refugee Mental Health Project. https://irmhp-psmir.camhx.ca/. Accessed 29 Jun 2022.
Röhr S, Jung FU, Pabst A, Grochtdreis T, Dams J, Nagl M, et al. A self-help app for syrian refugees with posttraumatic stress (Sanadak): randomized controlled trial. JMIR Mhealth Uhealth. 2021;9(1):e24807.
Acknowledgements
We would like to thank all the participants of this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EF, designed the survey, collected data, analyzed the data, drafted the original manuscript, and interpreted the results; MP, designed the survey, drafted the original manuscript, and interpreted the results, KG, Analyzed the data, drafted the original manuscript, and interpreted the results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
NonE.
Ethical Approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. The study protocol and all procedures involving research study participants were approved by the institutional ethics committee of the European University of Cyprus. Potential participants were informed regarding the terms of use of the provided data by the researcher. Only following agreement with the terms of data use, could someone proceed to the questionnaire and participate in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farmakioti, E., Pylli, M. & Giannakou, K. Access to Healthcare Services and Essential Medicines in GREEK Migrant Camps: an Online Cross-Sectional Study. J Immigrant Minority Health 25, 580–588 (2023). https://doi.org/10.1007/s10903-022-01425-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-022-01425-6