Abstract
A myriad of organ-specific complications have been observed with COVID-19. While racial/ethnic minorities have been disproportionately burdened by this disease, our understanding of the unique risk factors for complications among a diverse population of cancer patients remains limited. This is a multi-institutional, multi-ethnic cohort study evaluating COVID-19 complications among cancer patients. Patients with an invasive cancer diagnosis and confirmed SARS-CoV-2 infection were identified from March to November 2020. Demographic and clinical data were obtained and a multivariate logistic regression was employed to evaluate the impact of demographic and clinical factors on COVID-19 complications. The study endpoints were evaluated independently and included any complication, sepsis, pulmonary complications and cardiac complications. A total of 303 patients were evaluated, of whom 48% were male, 79% had solid tumors, and 42% were Hispanic/Latinx (Hispanic). Malignant hematologic cancers were associated with a higher risk of sepsis (OR 3.93 (95% CI 1.58–9.81)). Male patients had a higher risk of sepsis (OR 4.42 (95% CI 1.63–11.96)) and cardiac complications (OR 2.02 (95% CI 1.05–3.89)). Hispanic patients had a higher odds of any complication (OR 2.31 (95% CI 1.18–4.51)) and other race was associated with a higher odds of cardiac complications (OR 2.41 (95% CI 1.01–5.73)). Clinically, fever, cough, and ≥2 co-morbidities were independently significantly associated with any complication. This analysis evaluated covariates that can significantly predict a myriad of complications among a multi-ethnic cohort of cancer patients. The conclusions drawn from this analysis elucidate a mechanistic understanding of differential illness severity from COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, the current COVID-19 pandemic has disproportionately affected minority communities [1]. Despite this observation, racial/ethnic minorities remain underrepresented in published COVID-19 clinical research studies [2, 3]. Research to date has shown that certain demographic factors, such as race/ethnicity, have an impact on clinical severity and outcomes [4,5,6,7,8]. Among the general population infected with SARS-CoV-2, Hispanic/Latinx (Hispanic) ethnicity was observed to be strongly associated with a need for mechanical ventilation [9], whereas non-white ethnicity is strongly associated with critical care admission [8]. However, the impact of race and ethnicity in a cancer specific population remains underexamined. Patients with cancer may be particularly vulnerable to the morbidity and mortality associated with COVID-19 disease given underlying co-morbidities and potential immunosuppression from their disease and its treatment.
Individuals with an invasive cancer diagnosis and COVID-19 have been found to have an increased risk of all-cause mortality [10]. Given that COVID-19 can manifest with a myriad of complications, this study leverages a multi-institutional, multi-ethnic cohort to identify the unique risk factors for COVID-19 complications among a diverse population of patients with cancer.
Methods
This is a multi-institutional, multi-ethnic cohort study among patients with cancer. Patients with an invasive cancer diagnosis and a positive serologic or molecular SARS-CoV-2 test result were identified at participating sites (the University of California San Francisco (UCSF), and the University of California San Diego (UCSD)). Demographic and clinical data were collected manually from the electronic health record from March 1 to November 30, 2020, and populated in a REDCap database [11, 12]. This study was deemed exempt from review by the UCSF institutional review board (IRB) and received local IRB approval at UCSD.
Outcomes
We evaluated demographic, disease and treatment factors for their effects on four independent primary endpoints attributed to a COVID-19 diagnosis: “any complication”, sepsis, pulmonary complications, and cardiac complications were identified through manual chart review. Pulmonary complications were defined as respiratory failure, pneumonitis, acute respiratory distress syndrome (ARDS), pulmonary embolism, pleural effusion, or empyema. Cardiovascular complications were defined as hypotension, myocardial infarction, other cardiac ischemia, atrial fibrillation, ventricular fibrillation, other cardiac arrhythmia, cardiomyopathy, congestive heart failure, deep venous thrombosis, superficial venous thrombosis, cerebrovascular accident, or thrombosis. Patients with documented septicemia in the electronic health record were denoted as sepsis events. Lastly “other” complications were collected including gastrointestinal, bleeding, neurologic, systemic, or renal. Patients with “other”, sepsis, pulmonary complications, or cardiac complications were reported as “any complication”. Severity of COVID-19 outcomes for this study cohort defined as outpatient, hospitalization (non-ICU), ICU admission, and mortality is reported separately [13].
Statistical Analysis
Descriptive statistics were employed to summarize the baseline demographic and clinical characteristics of the study cohort. The frequency of clinical presentation characteristics were stratified by COVID-19 complications. A multivariate logistic regression model was generated to evaluate the relationship between patient-level covariates such as cancer history, cancer status, sex, race, age, BMI, treatment history, co-morbidity and COVID-19 presentation. The number of co-morbidities was calculated through manual chart review. The odds ratio for the independent primary endpoints were determined. Facility and environmental factors were controlled for in the model as splines by including average number of COVID-19 cases in the last 7 days per facility.
Results
Patient Characteristics
The study cohort included 303 patients with an invasive cancer diagnosis and a positive serologic or molecular SARS-CoV-2 test result. The clinical and demographic characteristics of patients are summarized overall and by outcome in Table 1. Overall, 147 (48%) were identified as male and 118 (29%) were older adults (≥65 years old). The patient race/ethnicity distribution included 104 (34%) non-Hispanic (NH) white, 21 (7%) NH Black patients, 126 (42%) Hispanic, 27 (9%) Asian, and 25 (8%) other/unknown. The primary language for a subset 71 (23%) of patients was Spanish. The insurance distribution for the study cohort was 75 (25%) Medicaid, 104 (34%) Medicare, 95 (31%) commercial, or other 29 (10%). A total of 106 (35%) had a body mass index (BMI) ≥30 and 182 (60%) had ≥2 co-morbidities. The baseline chronic diseases among the study cohort included pulmonary disease n = 71 (23%), cardiovascular disease n = 150 (50%), renal disease n = 39 (13%), and autoimmune disease n = 13 (4%).
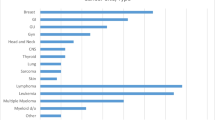
The majority of patients had solid tumors (n = 240, 79%) while the remaining had malignant hematologic cancers (n = 63, 21%). The cancer type distribution is summarized in the supplementary Table 1. Among the study cohort, at the time of COVID-19 diagnosis, 140 (46%) patients were in remission, 80 (26%) had stable disease or response on current therapy, and 54 (18%) had documented cancer progression on most recent clinical evaluation in the medical record. A total of 84 (28%) patients were considered immunosuppressed at time of COVID-19 diagnosis. The majority (n = 171, 56%) of patients had prior surgery and a smaller subset had prior radiation therapy (n = 77, 25%). A large proportion of patients (n = 207, 68%) had prior systemic therapy including myelosuppressive therapy (n = 128, 42%), hormone therapy (n = 48, 16%), and targeted therapy (n = 61, 20%).
COVID-19 Presentation Characteristics
As shown in Table 2 the initial COVID-19 presentation characteristics varied by organ-specific complications. The majority of patients presented afebrile (n = 166, 55%), with active cough (n = 176, 58%), symptomatic (n = 204, 67%), and without a known COVID-19 exposure (n = 265, 88%). A subset (n = 22, 7%) had asymptomatic screening testing. Among the 137 (45%) patients who presented with fever, 68 (50%) had complications overall, 19 (14%) had sepsis, 56 (41%) had pulmonary complications, and 28 (20%) had cardiac complications. Among the 176 (58%) patients with cough, 90 (51%) had any complication, 22 (13%) had sepsis, 73 (42%) had pulmonary complication, and 44 (25%) had cardiac complications. The frequency of presentation varied over time with the peak presentation occurring in July 2021 (n = 71, 23%).
Multivariate Logistic Regression
As shown in Table 3, patients with malignant hematologic cancers had a significantly higher risk of sepsis (OR 3.93 (95% CI 1.58–9.81)). Male patients had a greater risk of sepsis (OR 4.42 (95% CI 1.63–11.96)) and cardiac complications (OR 2.02 (95% CI 1.05–3.89)). There was a clear association between race/ethnicity and the risk of complications. Specifically, Hispanic patients had a higher risk of any complication (OR 2.31 (95% CI 1.18–4.51)) and other minority race group (non-Hispanics and non-whites) was associated with a higher odds of cardiac complications (OR 2.41 (95% CI 1.01–5.73)). Clinically, fever, cough, and ≥2 co-morbidities were independently significantly associated with any complication. Having ≥2 co-morbidities was also observed to be significantly associated with sepsis (OR 4.16 (95% CI 1.24–13.96)) and pulmonary complications (OR 2.48 (95% CI 1.27–4.84)). The effect of facility level COVID-19 7 day prior positivity rate was not significant in the model.
Discussion
This study suggests that the clinical and demographic characteristics of cancer patients at time of initial COVID-19 presentation affects the likelihood of subsequent complications. In this analysis, Hispanic patients were observed to have twice the risk of developing any complication from COVID-19 compared to NH white patients. This increased risk has also been observed on a population level. As of July 2021, the Centers for Disease Control reports that Hispanic persons have twice the rate of COVID-19 and almost three times the rate of hospitalization due to COVID-19 compared to NH white persons [14]. The unique risks among Hispanic cancer patients with COVID-19 observed in this study confirmed previous reports by Grivas and colleagues who observed that Hispanic ethnicity was associated with higher COVID-19 illness severity compared to NH white patients [15].
This study also observed that male patients had four times the risk of sepsis after COVID-19 infection. A “sex-bias” in COVID-19 illness severity and mortality has previously been reported [12]. In a meta-analysis published by Desai and colleagues, cancer subtype (hematologic versus solid) and male sex were identified as factors that contribute to higher mortality estimates for hospitalized patients with cancer and COVID-19 [15]. In a pooled analysis of 2968 cancer patients, male sex was identified as having a higher risk of severe illness and death attributable to COVID-19 [17]. Sex-based differences in sepsis outcomes have also previously been reported, with women having a significantly better prognosis in the setting of sepsis [18]. These observations suggest that the previously reported increased COVID-19 associated mortality among male patients may be driven by an increased risk for sepsis after COVID-19 infection. In this study cohort, 21 (7%) patients had deaths attributed to COVID-19, though mortality was found to be associated with an active cancer diagnosis and advanced age (65+) rather than male sex [13]. A future analysis with a larger sample size will need to further examine this association.
Other clinical factors were shown to predict risk for complications such as multi-morbidity (≥2 co-morbidities) which was observed to be independently significantly associated with any complication, sepsis, and pulmonary complications. The notion that multimorbidity leads to adverse outcomes at time of COVID-19 infection has also been suggested by prior research. Moey and colleagues identified that patients with cancer and comorbid cardiovascular disease are at an increased risk of COVID-19 associated mortality [19]. The COVID-19 and Cancer Consortium (CCC19) study identified cardiovascular and pulmonary comorbidities to predict higher risk of COVID-19 severity among cancer patients with active disease [15]. Similarly, Borno and colleagues reported that patients in this study cohort with multi-morbidity had higher odds of hospitalization (citation).
Additionally, this analysis demonstrated that unique clinical presentation factors such as fever and cough may be associated with organ-specific complications. A systematic review and meta-analysis of 148 COVID-19 research studies identified fever and cough as the most common symptoms among adults infected with SARS-CoV2 [19]. The present study observed that symptoms of fever independently predict a higher odds of any complications and pulmonary complications. Robilotti and colleagues have previously reported that fever and cough are associated with a higher risk of hospitalization and severe respiratory illness among cancer patients [21]. Moreover, presence of cough in this study cohort was identified as a predictor of ICU hospitalization [13].
This study’s primary strength is that it leverages an ethnically diverse cohort to identify risk factors for COVID19 complications. Evaluating predictors of independent complications begins to provide a mechanistic understanding of differences in mortality previously reported among cancer patients with a COVID-19 diagnosis. The primary weakness of this analysis is its retrospective nature and limited sample size. Tumor types were grouped as solid or malignant hematologic cancers, therefore unique risk factors by disease type could not be elucidated in this dataset. Additionally, this study has limited follow-up therefore did not evaluate long-term complications of COVID-19 among cancer patients. Despite these limitations, to our knowledge this is the first analysis to evaluate multiple organ-specific complications among a diverse patient population.
Conclusions
This analysis evaluated covariates that can significantly predict a myriad of complications among a multi-ethnic cohort of cancer patients. The conclusions drawn from this analysis elucidate a mechanistic understanding of differential illness severity from COVID-19. Observations from this analysis may help inform mitigation strategies to reduce adverse outcomes among minority populations. Future research will evaluate complications by tumor type and identify risk factors for long-term complications from COVID-19 among cancer patients.
References
Anyane-Yeboa A, Sato T, Sakuraba A. Racial disparities in COVID-19 deaths reveal harsh truths about structural inequality in America. J Intern Med. 2020. https://doi.org/10.1111/joim.13117.
Rabow M, Wang C, Zhang S, Tahir PM, Small EJ, Borno HT. Examining reporting and representation of patients with cancer in COVID-19 clinical trials. Cancer Rep (Hoboken). 2021. https://doi.org/10.1002/cnr2.1355.
Borno HT, Zhang S, Gomez S. COVID-19 disparities: an urgent call for race reporting and representation in clinical research. Contemp Clin trials Commun. 2020;19:100630. https://doi.org/10.1016/j.conctc.2020.100630.
Imam Z, Odish F, Gill I, O’Connor D, Armstrong J, Vanood A, Ibironke O, Hanna A, Ranski A, Halalau A. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med. 2020;288(4):469–76. doi:https://doi.org/10.1111/joim.13119.
Cecconi M, Piovani D, Brunetta E, Aghemo A, Greco M, Ciccarelli M, Angelini C, Voza A, Omodei P, Vespa E, Pugliese N, Parigi TL, Folci M, Danese S, Bonovas S. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for Covid-19 infection in Lombardy Italy. J Clin Med. 2020. https://doi.org/10.3390/jcm9051548.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. https://doi.org/10.1016/S0140-6736(20)30211-7.
ElGohary GM, Hashmi S, Styczynski J, Kharfan-Dabaja MA, Alblooshi RM, de la Cámara R, Mohmed S, Alshaibani A, Cesaro S, Abd El-Aziz N, Almaghrabi R, Gergis U, Majhail NS, El-Gohary Y, Chemaly RF, Aljurf M, El Fakih R. The risk and prognosis of COVID-19 infection in cancer patients: a systematic review and meta-analysis. Hematol/oncol stem cell ther. 2020;S1658–3876(20):30122–9. https://doi.org/10.1016/j.hemonc.2020.07.005.
Galloway JB, Norton S, Barker RD, Brookes A, Carey I, Clarke BD, Jina R, Reid C, Russell MD, Sneep R, Sugarman L, Williams S, Yates M, Teo J, Shah AM, Cantle F. A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study. J Infect. 2020;81(2):282–8.
Mani VR, Kalabin A, Valdivieso SC, Murray-Ramcharan M, Donaldson B. New York inner city hospital COVID-19 experience and current data: retrospective analysis at the epicenter of the American coronavirus outbreak. J Med Internet Res. 2020;22(9):e20548.
Lee LYW, Cazier J-B, Angelis V, Arnold R, Bisht V, Campton NA, Chackathayil J, Cheng VWT, Curley HM, Fittall MW, Freeman-Mills L, Gennatas S, Goel A, Hartley S, Hughes DJ, Kerr D, Lee AJX, Lee RJ, McGrath SE, Middleton CP, Murugaesu N, Newsom-Davis T, Okines AFC, Olsson-Brown AC, Palles C, Pan Y, Pettengell R, Powles T, Protheroe EA, Purshouse K, Sharma-Oates A, Sivakumar S, Smith AJ, Starkey T, Turnbull CD, Várnai C, Yousaf N, Kerr R, Middleton G. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. The Lancet. 2020;395(10241):1919–26. https://doi.org/10.1016/S0140-6736(20)31173-9.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:https://doi.org/10.1016/j.jbi.2019.103208.
Borno HT, Kim M-O, Hong JC, Yousefi S, Lin A, Tolstykh I, Zhang S, McKay RR, Harismendy O, Cinar P, Rugo H, Koshkin VS, Rabow M, Wang C, Bailey A, Small EJ. COVID-19 Outcomes among patients with cancer: observations from the university of california cancer consortium COVID-19 project outcomes registry. Oncologist. 2022;27(5):398–406. https://doi.org/10.1093/oncolo/oyac038.
Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity. 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 2 July 2021
Grivas P, Khaki AR, Wise-Draper TM, French B, Hennessy C, Hsu CY, Shyr Y, Li X, Choueiri TK, Painter CA, Peters S, Rini BI, Thompson MA, Mishra S, Rivera DR, Acoba JD, Abidi MZ, Bakouny Z, Bashir B, Bekaii-Saab T, Berg S, Bernicker EH, Bilen MA, Bindal P, Bishnoi R, Bouganim N, Bowles DW, Cabal A, Caimi PF, Chism DD, Crowell J, Curran C, Desai A, Dixon B, Doroshow DB, Durbin EB, Elkrief A, Farmakiotis D, Fazio A, Fecher LA, Flora DB, Friese CR, Fu J, Gadgeel SM, Galsky MD, Gill DM, Glover MJ, Goyal S, Grover P, Gulati S, Gupta S, Halabi S, Halfdanarson TR, Halmos B, Hausrath DJ, Hawley JE, Hsu E, Huynh-Le M, Hwang C, Jani C, Jayaraj A, Johnson DB, Kasi A, Khan H, Koshkin VS, Kuderer NM, Kwon DH, Lammers PE, Li A, Loaiza-Bonilla A, Low CA, Lustberg MB, Lyman GH, McKay RR, McNair C, Menon H, Mesa RA, Mico V, Mundt D, Nagaraj G, Nakasone ES, Nakayama J, Nizam A, Nock NL, Park C, Patel JM, Patel KG, Peddi P, Pennell NA, Piper-Vallillo AJ, Puc M, Ravindranathan D, Reeves ME, Reuben DY, Rosenstein L, Rosovsky RP, Rubinstein SM, Salazar M, Schmidt AL, Schwartz GK, Shah MR, Shah SA, Shah C, Shaya JA, Singh SRK, Smits M, Stockerl-Goldstein KE, Stover DG, Streckfuss M, Subbiah S, Tachiki L, Tadesse E, Thakkar A, Tucker MD, Verma AK, Vinh DC, Weiss M, Wu JT, Wulff-Burchfield E, Xie Z, Yu PP, Zhang T, Zhou AY, Zhu H, Zubiri L, Shah DP, Warner JL, Lopes G. Association of clinical factors and recent anticancer therapy with COVID-19 severity among patients with cancer: a report from the COVID-19 and cancer consortium. Ann Oncol. 2021;32(6):787–800. https://doi.org/10.1016/j.annonc.2021.02.024.
Desai A, Gupta R, Advani S, Ouellette L, Kuderer NM, Lyman GH, Li A. Mortality in hospitalized patients with cancer and coronavirus disease 2019: a systematic review and meta-analysis of cohort studies. Cancer. 2021;127(9):1459–68. https://doi.org/10.1002/cncr.33386.
Park R, Chidharla A, Mehta K, Sun W, Wulff-Burchfield E, Kasi A. Sex-bias in COVID-19-associated illness severity and mortality in cancer patients: a systematic review and meta-analysis. EClinicalMed. 2020. https://doi.org/10.1016/j.eclinm.2020.100519.
Schroder J, Kahlke V, Staubach KH, Zabel P, Stuber F. Gender differences in human sepsis. Arch Surg. 1998;133(11):1200–5. https://doi.org/10.1001/archsurg.133.11.1200.
Moey Melissa YY, Shah D, French B, DeCara J, Chouieri T, Dent S, Akhter N, Ismail-Khan R, Morgans A, Nohria A, CLINICAL CHARACTERISTICS AND OUTCOMES IN CARDIO-ONCOLOGY PATIENTS WITH COVID-19. Analysis from the covid-19 and cancer consortium (CCC19) database. J Am Coll Cardiol. 2021;77(18_Supplement_1):3133. https://doi.org/10.1016/S0735-1097(21)04488-0.
Grant MC, Geoghegan L, Arbyn M, Mohammed Z, McGuinness L, Clarke EL, Wade RG. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): a systematic review and meta-analysis of 148 studies from 9 countries. PLoS ONE. 2020;15(6):e0234765-e. https://doi.org/10.1371/journal.pone.0234765.
Robilotti EV, Babady NE, Mead PA, Rolling T, Perez-Johnston R, Bernardes M, Bogler Y, Caldararo M, Figueroa CJ, Glickman MS, Joanow A, Kaltsas A, Lee YJ, Lucca A, Mariano A, Morjaria S, Nawar T, Papanicolaou GA, Predmore J, Redelman-Sidi G, Schmidt E, Seo SK, Sepkowitz K, Shah MK, Wolchok JD, Hohl TM, Taur Y, Kamboj M. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020;26(8):1218–23. https://doi.org/10.1038/s41591-020-0979-0.
Funding
University of California (Research Grants Program Office, RGPO) Emergency COVID-19 Funding (R00RG3155)
Author information
Authors and Affiliations
Contributions
HTB prepared primary manuscript; all co-authors provided critical feedback; MOK and IT provided statistical analysis; SY, JCH, OH, RRMc, PR, HR, MR, CW and SZ collected data.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borno, H.T., Kim, MO., Tolstykh, I. et al. Assessing Unique Risk Factors for COVID-19 Complications Among Cancer Patients: A Multi-ethnic Cohort Study. J Immigrant Minority Health 25, 624–633 (2023). https://doi.org/10.1007/s10903-022-01413-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-022-01413-w