Abstract
The global pandemic of COVID-19 has been influencing people’s lives and the cities. Not only people’s physical and mental health have been threatened, but also the city operation has been profoundly affected from different perspectives (e.g., social and economic) permanently. How cities can efficiently react and response to improve city resilience is an urgent issue to be addressed. The healthcare system as a vital part of the city systems is confronting intense pressure and many challenges under this emergent public health crisis of COVID-19, which might cause huge impacts on the whole city’s operation. Also, human beings as the direct victims of this public health crisis, their behaviour changes impacts on the healthcare system and the city could have been inevitable but have been neglected. In this context, this paper intends to study the citizen healthcare accessing behaviours changes in the post-pandemic era, and to unearth their impacts on the healthcare system and the city operation. For this purpose, first, a framework of influential factors for healthcare accessing was established based on a bidirectional “capability, opportunity, motivation, and behaviour” (COM-B) model and the comprehensive literature review. In which, 43 factors that would influence citizen healthcare accessing behaviour were identified and classified. Thus, based on the proposed framework, two cases (i.e., UK and China) were analysed in depth and compared based on a questionnaire survey to evaluate the factor importance and relationships under different scenarios. And the most influential factors based on analysis results are classified into 12 aspects (e.g., healthcare capability, policy support, information updating etc.). Further, a novel behaviour-healthcare system-city model based on the COM-B model was developed to rethink and indicate the relationships among citizen behaviour, healthcare system and city operation. The research results can be used by policymakers and researchers to improve the city resilience by enabling immediate responses to city systems and citizens behaviours confronting city emergencies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since the outbreak of COVID-19 in late 2019, the global sweeps of the pandemic have been causing massive social and economic impacts on people’s lives and the cities (Batty, 2022). Because human beings’ health has been threatened massively by this public health crisis, the healthcare system has been facing unprecedented challenges since the outbreak of the pandemic. Many countries (e.g., China, the U.S., the UK, Italy, France, and Japan) have reported a shortage of healthcare resources such as Intensive Care Unit (ICU) beds, ventilators, and trained personnel (Canas et al., 2021; Ceylan, 2020; Watanabe, 2020; White & Lo, 2020; Xie et al., 2020). Even worse, researchers have addressed the importance to focus on the physical and psychological health condition of medical practitioners under such a heavy workload caused by COVID-19, which increased the shortage of trained personnel (Shah et al., 2020). The scarcity of medical resources in the healthcare system has aggravated people’s panic or anxiety (Qiu et al., 2020).
At city level, the healthcare system is an essential and vital component of the city as it relates closely to the stability of the city operation during the public health crisis of COVID-19. Moreover, studies have indicated that adequate management of the healthcare system was one of the top concerns in the city resilience framework (Feng et al., 2020; The Rockefeller Foundation & Arup, 2014), which drives the urgent need to rethink city resilience associating with the healthcare system affected by the public health crisis like COVID-19. In existing studies related to healthcare system accessibility, (Emanuel et al., 2020) discussed the fair allocation of scarce medical resources in the time of COVID-19 with recommendations from the healthcare system perspective. For example, the priority for limited resources should aim both at saving the most lives and at maximizing improvements in individuals’ post-treatment length of life; prioritization guidelines should differ by intervention and should respond to changing scientific evidence (e.g., older persons and patients with chronic illness might need prioritization than younger patients) (Emanuel et al., 2020). Besides, the two-step floating catchment area (2SFCA) and enhanced 2SFCA (E2SFCA) methods were commonly used to analyse the spatial accessibility of healthcare with the consideration of demand–supply relationship (Mao & Nekorchuk, 2013; Wan et al., 2012). For instance, (Kang et al., 2020) used E2SFCA to optimise healthcare accessibility considering the bed-to-population ratio after the outbreak of COVID-19. (Ghorbanzadeh et al., 2021) researched on the spatial accessibility assessment of COVID-19 patients to healthcare facilities in Florida using the 2SFCA and E2SFCA. This study revealed many areas in the northwest and southern Florida have lower access compared to other locations, which provided provide valuable insights and information for state officials and decision makers (Ghorbanzadeh et al., 2021). Additionally, before the outbreak of COVID-19, individual characteristics (e.g., demographics, insurance status, needs, health status, car ownership and geographic distance) have been analysed for spatial healthcare accessibility (Comber et al., 2011; Litaker et al., 2005). However, the research gaps exist where, firstly, discussions were limited regarding the relationship between healthcare system and city operation/resilience involving multiple organisations and stakeholders, especially in the public health crisis; second, citizen reactions (i.e., the behaviour change of healthcare accessing) and the corresponding influences on the healthcare system and the city were overlooked.
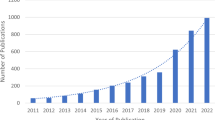
As COVID-19 has directly threatened people’s physical health, it has naturally caused people’s intention of healthcare accessing behaviours, which potentially leads to the scarcity of medical resources. From the urban study perspective, a pattern of human behaviour-related influence for city systems and thus the cities have been addressed and studied in the post-pandemic era. For example, (Kato & Matsushita, 2021) revealed the speed increase of people’s walking behaviour and more cyclists in a city of Japan, which suggested more walkable streets and bike lanes were needed in the city’s transportation system. Travel-related behaviour changes have indicated different trends towards private and public transportation in different countries (Angell & Potoglou, 2022; Zhang et al., 2021). Also, the energy consumption patterns have been proved shifting during the pandemic because of lighting use changes (Rowe et al., 2022). To further explain how the behavioural changes can affect cities, Lu et al. proposed a bidirectional interaction between human and cities shown in Fig. 1 (Lu et al., 2021). Specifically, COVID-19 and the controlling strategies profoundly affected citizen behaviours (e.g., energy/transportation/culture related behaviours), and then the behaviours can affect city systems (e.g., energy/transportation/recreational systems) through actions on building systems and facilities, where city performance can be sequentially influenced by the alter of city system eventually and re-affect citizen behaviour (Lu et al., 2021). Therefore, it is reasonable and inevitable to concentrate on healthcare accessing behaviour changes and analyse their impacts on the healthcare system and the city facing city emergencies like COVID-19.
The bidirectional interaction between human and cities based on (Lu et al., 2021)
To understand the healthcare accessing behaviour change affected by COVID-19, it is necessary to figure out the influential factors hidden behind. Accept from the direct considerations of personal physical health, medical resources availability (e.g., physicians, equipment, ICU beds) (Emanuel et al., 2020), there have been several factors mentioned in existing studies. For example, (Giezendanner et al., 2021) has indicated the healthcare accessing change regarding healthcare provider choices (e.g., pharmacies, GPs, hospitals) and the potentials for telemedicine. Psychological distress or anxiety of the infection risk in the healthcare might be an influential factor (Bavel et al., 2020). And the COVID-19 policies such as keeping social distance, shutdown of transportation, quarantine requirements for infected people and close contacts might also stop people from accessing healthcare places (Bavel et al., 2020; Chen et al., 2020; Nikiforiadis et al., 2022). In addition, before the outbreak of COVID-19, many influential factors have been studied. For instance, (Nägga et al., 2012) studied the healthcare accessing factors like living environment, education background, assistance needs for elderly aged 85. (Lee et al., 2014) studied factors such as lack of money and transportation, no availability of appointment for disabilities in a Korea. (You, 2021) analysed factors regarding greening rate, time of completion, distance to the healthcare etc. However, the abovementioned factors were too scattered and isolated to be used as a theoretical framework to directly understand the behaviour changes facing COVID-19, which impeded the analysis of behaviour changes impacts on the healthcare system and the city.
In this sense, a capability, opportunity, motivation, and behaviour (COM-B) model from psychological science field is thus used in this study to provide a fundamental and bi-directional framework. The aim is to (1) establish a comprehensive framework of influential factors for healthcare accessing behaviour based on COM-B model, (2) using the framework, to analyse in depth and compare whether the healthcare accessing behaviour has been changed in pre- and post-pandemic era for the UK and China cases, and what are the key aspects affecting the changes, and (3) how the healthcare system and thus the city are influenced and what would be the responses regarding city operation and resilience.
The following of this study is structured as follows. Section 2 introduces the COM-B model in details and demonstrates its application in this study. Section 3 introduces the research methodology, data collection and data analysis. Section 4 illustrates establishment of the proposed framework of influential factors for healthcare accessing behaviour based on COM-B model. Section 5 shows the analysis and comparison results regarding multiple scenarios in the UK and China cases. Based on the results, Section 6 discusses the relationships among the healthcare accessing behaviour, healthcare system, and the cities, and proposes a novel model of the three components to improve city resilience towards public health crisis.
2 The bi-directional COM-B model and its related studies of healthcare
Healthcare accessing is a human behaviour, and it directly relates to the usage state of city’s healthcare system. Many behavioural change interventions are potential to affect the stable operation of whole healthcare system. Examples are factors (i.e., interventions) such as personal health condition, transportation, healthcare medical capability that have been existing before the pandemic (Comber et al., 2011; Lee et al., 2014), and mask mandatory, social distance and vaccination requirements have occurred after the COVID-19 outbreak (Bavel et al., 2020; Chen et al., 2020; Nikiforiadis et al., 2022). In the psychological science research field, COM-B model has been well-established by (Michie et al., 2011) overcoming the limitations of the other 19 behaviour change frameworks (Perros et al., 2022). It has been widely employed for behaviour change studies such as diabetes, medication, energy saving behaviours (Handley et al., 2015; Jackson et al., 2014; Perros et al., 2022). After the outbreak of COVID-19, the COM-B model have also been implemented. For instance, they been used to explore pregnant women’s understanding of the behavioural restrictions and their perceived ability to comply and the most concerning impacts of the measures in the post-pandemic time (Anderson et al., 2021). The British Psychological Society’s Behavioural Science and Disease Prevention Taskforce advises using COM-B to understand and facilitate the enactment of preventative behaviours in the context of the pandemic (Chater et al., 2020; Michie & West, 2021; Michie et al., 2011). Therefore, there is great potential utility in applying COM-B for healthcare accessing behaviour study.
The COM-B model indicates that the human behaviour is influenced bi-directionally by capability, motivation, and opportunity and the interactions among them as shown in Fig. 2 (Michie et al., 2011). Besides, capability and opportunity contribute to motivation, so that having greater capability and opportunity can increase motivation and thus influence the behaviour more (Michie & West, 2021). The definitions of “capability”, “opportunity”, and “motivation” in the context of this study are explained and illustrated with existing studies as follows.
2.1 Capability
“Capability” was indicated as “the individual’s psychological and physical capability to engage in the activity concerned”, which represented having necessary knowledge or skills to achieve the activity (Anderson et al., 2021; Michie et al., 2011). In this study, it can be understood as the individual’s capacity to access the healthcare system measured by his/her personal abilities (Michie et al., 2011). For example, in previous studies, personal physical health condition (e.g., severity and emergency of the illness, chronic illness history) relates directly to the healthcare accessing behaviour (Arora & Grey, 2020; Zanobetti et al., 2012). Other non-medical capability such as lack of driving ability and lack of public transportation accessing, financial affordability have been used to measure the healthcare accessibility (Lee et al., 2014; Litaker et al., 2005). Especially in the COVID-19 situation, a large amount of digital methods (e.g., self-checking of COVID-19 symptoms and remedy advice, QR codes scanning to ensure COVID-19 negative status, vaccination verification) were used to control the infections (Liu & Stern, 2021; Wang et al., 2020; Wymant et al., 2021), which have required the capability to learn and use these digital technology. However, this has also resulted in the capability from psychological aspect where people might be equipped with low acceptance or distrust of the digital technology (Troisi et al., 2022).
2.2 Opportunity
“Opportunity” was indicated as “all the factors that lie outside the individual that make the behaviour possible or prompt it” like societal norms and environmental resources (Anderson et al., 2021; Michie et al., 2011). For healthcare accessing behaviour, the opportunity factors can be diverse. For instance, previously, (Lu et al., 2019) have addressed the medical resources opportunity like ICU bed and COVID-specific equipment usage and transfer efficiency among different levels of healthcare. (Lee et al., 2014; You, 2021) have researched on the environmental measurements of healthcare accessibility such as congestion level, comfort level, service attitude etc. Moreover, the provision of the medical resources by the built environment, which could be the spatial distribution of healthcare and public transportation plan, has been constantly focused on regarding the healthcare accessibility topic (Ghorbanzadeh et al., 2021; Mao & Nekorchuk, 2013; You, 2021). In addition, several infection controlling policies during the COVID-19 pandemic have become important opportunity factors such as mask mandatory, social distance requirement are suggested and guaranteed by the policy to eliminate the infection and potentially influence healthcare accessing behaviour (Bavel et al., 2020; Michie et al., 2011; West et al., 2020).
2.3 Motivation
“Motivation” was indicated as “all those brain process that energise the direct behaviour, not just goals and conscious decision-making” like emotional feeling and habitual process (Anderson et al., 2021; Michie et al., 2011). For example, because of the high transmission feature of COVID-19 virus (especially with the Omicron variant), hospitals or general practices (GPs) were proved to have higher infection risk (Lai et al., 2020). In this context, motivation factors for healthcare accessing behaviour can associate with feelings and impulses (Michie et al., 2011) like anxiety or fear caused by COVID-19 infection risk (Bavel et al., 2020), potential quarantine risk by becoming close contact, traffic restriction by the lockdown policy (Serafini et al., 2020). (Giezendanner et al., 2021) has conducted the research to understand whether people’s healthcare accessing behaviour have changed depending on the medical level of the healthcare provider after COVID-19 outbreak. Other factors that have been discussed previously like efficacy of general physicians’ consultation, anxiety or fear of personal information exposure and low willingness to communicate can also be categorised as motivation factors (Lee et al., 2014; Serafini et al., 2020).
In general, previous studies have indicated that the healthcare accessing behaviour can be affected by a variety of factors. However, a comprehensive framework to overview and analyse the factors has lacked, which led to the difficulty to examine the healthcare behaviour change under public health crisis such as COVID-19 (which directly “attack” human beings). In this case, COM-B model provides a fundamental way to understand how human behaviours can be affected, and to analyse the influential factors that might cause the changes. Therefore, COM-B is employed as a theoretical framework for examining the healthcare accessing behaviour changes in the COVID-19 context in this study.
3 Research methodology
The research methodology consists of three phases. The first phase is to develop a framework of healthcare accessing influential factors based on COM-B model. To start with, a comprehensive literature review was conducted to find out the factors that have been addressed related to healthcare accessing (before and after the outbreak of COVID-19). Then, the factors were categorised based on the definitions and explanations of “capability” (coded with #C1, C2, C3 …), “motivation” (coded with #M11, M12, M13 …), and “opportunity” (coded with #O1, O8, O11 …) described in Section 2. Especially, this study used a behaviour change wheel which is a wider intervention development framework of the COM-B with suggested sub-categories under “capability”, “motivation”, and “opportunity”, as a referencing framework to ensure a more comprehensive inclusion of the healthcare accessing factors (Michie et al., 2011; Perros et al., 2022).
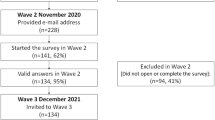
The second phase is to conduct a Likert-scale form questionnaire survey to evaluate the importance of the factors for healthcare accessing based on the developed framework in Phase 1 in the UK and China cases. There were three parts of the questionnaire for participants to fill in. The first part is demographic information including “gender”, “age group”,, “living location (i.e., the UK or China, specific location of city is not compulsory)”, and “current work/study mode (i.e., commute or work from home)”. The second and third parts asked for the degree of importance of each factor from “rare important” to “most important” in pre-pandemic scenario and post-pandemic scenario. For pre-pandemic, there were 31 factors to assess because multiple COVID-19 related factors were excluded. For post-pandemic, there were 43 factors were assessed. The data collection of the questionnaire survey is shown in Section 3.1. The collected data was analysed using Relative Importance Index (RII) method. Based on the results, different scenarios for the UK and China cases were created to analyse and compare the data in depth, i.e., (1) an overview of RII and RII rank of all factors, (2) top 15 influential factors in post-pandemic era for the UK and China case, (3) factors changing comparison between pre-pandemic and post-pandemic eras for the UK and China case, and (4) factor rank difference between the UK and China cases in the post-pandemic era. By analysis and comparison, the key aspects of concern were concluded based on the implications of factors. The data analysis details are described in Section 3.2
Lastly, based on the results of previous analysis, a novel behaviour-healthcare system-city model based on COM-B model was proposed to rethink and improve the city resilience by responding the healthcare requirements enlargement caused by the changed behaviour in the post-pandemic era. The discussions were conducted regarding the understanding of the changed healthcare accessing behaviour, impacts on the healthcare systems and city-level responses.
3.1 Data collection
The questionnaire was designed to be distributed in the UK and China. post for two weeks in March 2022. For the questionnaire distribution and data collection in China and the UK. These two countries were selected for their distinct healthcare systems, cultural backgrounds, and varied COVID-19 responses to public health crises, offering a comparative lens through which to explore the characteristics and changes of healthcare accessing behaviour. The UK, with its National Health Service (NHS), presents a model of a publicly funded healthcare system, whereas China's mixed healthcare model reflects rapid evolution and reform (Grosios et al., 2010; Sun et al., 2021). This comparative analysis aims to uncover how systemic and cultural factors influence healthcare behaviour, providing insights with broad applicability beyond the specific contexts of the UK and China.
The questionnaire was post for two weeks in March 2022. For the questionnaire distribution and data collection in both countries, the web-based Wenjuanxing platform and Google Form platform were adopted respectively (Barbieri et al., 2020). There were 76 valid respondents from China case and 44 valid respondents from the UK case. The sample sizes were regarded as large sample tests for analysis because N > 30 in each case according to Central Limit Theorem. Therefore, it can be reasonable to conduct the following analysis and discussions based on the collected samples. The demographic distributions of “Gender”, “Age group” and “Current work/study mode” shows in Table 1. Based on Table 1, in both of the cases, it shows that both female (around 60%) and male (around 40%) respondents and more young and middle group (18–30, 31–45 age groups) respondents (added up over 85%) were surveyed. But the analysis of the age group distribution potentially indicates the surveyed samples are more representative for young and middle age group populations. Based on the demographic distributions, it is also acquired that the distributions of each variant in the China and UK cases are very similar. For example, in the China case, the 18–30 age group (53.95%) and 31–45 age group (35.89%) take account for 89.84% of total respondents; in the UK case, the 18–30 age group (68.18%) and 31–45 age group (29.55%) take account for 97.73% of total respondents. The similar distributions of the age group variant (as well as gender and current work/study mode variants) indicates that the data can be analysed and compared between the China case dataset and the UK case dataset without compositional effects. Additionally, the specific living location were asked as an optional question. The top three specific locations of the total respondents were Guangdong Province (14.47%), Shanghai (13.16%), Shanxi Province (10.53%) in the China case; in the UK case, the respondents were mainly from London (15.91%), Loughborough (13.64%), and Cambridge (11.36%).
Table 2 presents the results of Cronbach’s alpha for analysing the reliability of the survey before the survey data analysis. Cronbach’s alpha for each factor category and factors overall in the post- and pre-pandemic scenarios in both the China and UK cases were calculated. The results were over 0.8, thereby indicating sufficient reliability and consistency of the survey data.
3.2 Data analysis
The data analysis method of RII is a common statistical analysis method for Likert-scale survey datasets. For example, RII method has been frequently employed in construction management research (Holt, 2014), where Gündüz et al. examined what were the delay factor for construction projects in Turkey (Gündüz et al., 2013). Rooshdi et al. used RII method to study the sustainable design and construction activities criteria for green highway (Rooshdi et al., 2018). This study adopted this analysis method innovatively to specify the ranks of the factors that have been surveyed through the Likert-scale questionnaire. Specifically, RIIs were calculated in for each factors using the Eq. (1) in IBM Statistical Package for the Social Sciences (SPSS) Statistics:
where RII is relative importance index; W is weighting given to each factor by respondents (ranging from 1 to 5, assign 1 to “rare important”, 2 to “low important”, 3 to “moderate important”, 4 to “very important”, and 5 to “most important”); A is highest weight, which is 5 in this study; N is total number of respondents.
With the calculated RII, the ranks of the factors were given for the Chinese case pre- and post-pandemic, the UK case pre- and post-pandemic respectively. Moreover, the rank comparisons between pre- and post-pandemic scenarios were conducted, where the changing rate “CR” was calculated:
Equation (2) is used if Rpost ≤ Tf:
Equation (3) is used if Rpost > Tf (because the total factors in the post-pandemic scenarios is more than in the pre-pandemic scenario):
where Rpost is the rank in post-pandemic scenario, Rpre is the rank in pre-pandemic scenario, Fd is the factor number difference between the post-pandemic and pre-pandemic (which is 13 for the China case and 12 for the UK case), Tf is the total number of the factors in pre-pandemic (which is 31 for the China case and 30 for the UK case).
Additionally, the rank difference of factors “D” between China and the UK cases in the post-pandemic scenario was calculated using Eq. (4):
where Rpost-CN is the rank in the China case, and Rpost-UK is the rank in the UK case, Tf2 is the total number of factors in the post-pandemic scenario.
4 The framework of influential factors for healthcare accessing behaviour
According to the research methodology Phase 1 (Section 3), the framework of influential factors for healthcare accessing behaviour in the post-pandemic era is established based on COM-B model in Table 3. There are 43 factors for the China case (because the factor C8 is only applicable in China) and 42 factors for the UK case. Besides, the factors directly related to COVID-19 are noted (a total of 13 factors for both the UK and China cases). The factors’ categories based on the COM-B model and sub-categories referred to the behaviour change wheel are illustrated as follows and labelled in Table 3 (Michie et al., 2011).
-
Capability: refers to physical health condition of individuals (Physical Capability), the mental decision-making processes to engage or achieve the activity (Psychological Capability), the financial affordability to achieve the activity (Financial Capability), the transportation accessibility of individuals to fulfil the activity (Transportation Capability), knowledge and intellectual background to achieve the activity (Educational Capability);
-
Opportunity: refers to the environmental resources (Outside Built Environment Opportunity), the physical environment of objects and events with which people interact (Physical Opportunity), the policy enactments that would affect human behaviour (Policy Regulation Opportunity);
-
Motivation: refers to reflective intentions, evaluations and values (Reflective Motivation), and automatic habits, emotions and instincts that direct human behaviour (Automatic Motivation) (Perros et al., 2022).
For the classification of sub-categories, although the behaviour change wheel was used as the referencing framework to guarantee a full inclusion of the factors, the sub-categories in this study did not fully align with the subcategories in the behaviour change wheel because of the different research context. For example, the sub-category of financial capability of an individual would be an influential factor for one to access healthcare, but it has not been included in the original behaviour change wheel (Michie et al., 2011). Also, the sub-categories of “modelling” or “marketing” have been mentioned in the original wheel (Michie et al., 2011), no related factors for healthcare accessing were noticed in existing studies so they were excluded in the establishment of the framework in this study. Hence, the established framework in Table 3 is an innovative COM-B model-based framework for healthcare accessing behaviour that partially adopts the sub-categories of the original behaviour change wheel.
5 Comparison and analysis of two cases: UK and China
5.1 Calculated results in general
The calculated results of all factors in the proposed framework of healthcare accessibility influential factors have been presented in Table 4. In Table 4, the RIIs and ranks of pre- and post-pandemic scenarios in the UK and China case are demonstrated for the convenience of comparison. For the factors that are only applicable in the post-pandemic scenario, the RIIs and ranks are presented with the null symbol “/”.
In analysing the geographical distribution of the respondents, we observed a significant disparity. As noted in Section 3.1, the specific living location were asked as an optional question. The top three specific locations of the total respondents are Guangdong Province (14.47%), Shanghai (13.16%), Shanxi Province (10.53%) in the China case; in the UK case, the respondents are mainly from London (15.91%), Loughborough (13.64%), and Cambridge (11.36%). Although we attempted to analyse the impact of geographical distribution on healthcare access behaviours, no significant patterns emerged from the collected dataset. Therefore, subsequent analyses will focus on a more general comparison between the UK and China cases.
5.2 Top 15 influential factors in post-pandemic scenario
To further reveal the important factors affecting citizens’ behaviour of healthcare system accessing, the top 15 factors sorted by the rank in the China case post-pandemic scenario (shown in Table 5) and in the UK case post-pandemic scenario (shown in Table 6) separately. In Tables 5 and 6, a column of “rank change” is attached to indicate whether the rank of the factor has been ascended “↑”, descended “↓”, or remained “-” comparing to the rank in pre-pandemic scenario.
In Table 5 for post-pandemic scenario for the China case, it is observed that COVID-19 related factors have become respondents’ primary considerations (6/15 factors) when considering healthcare accessibility. Amongst, the factor of whether the healthcare accept patients COVID-19 patients (i.e.O17), is the top concern. Following by that, COVID-19 related policy like indoor mask wearing and social distance keeping requirement (i.e., O14, O16), are very important to the respondents. Then, the factors regarding information updating (i.e., O12), psychological distress (i.e., M14), and medical capability (i.e., M8) are highly concerned by respondents in post-pandemic era. Further, the top 15 factors can be concluded to six aspects of concerns, which are (1) personal health condition (C2-rank 1, C3-rank 4), (2) healthcare capability (O17-rank 2, M1-rank 2, M7-rank 4, O7-rank 9, O10-rank 11, M2-rank 11, M8-rank 15), (3) policy regulation (O17-rank 2, O14-rank 6, O16-rank 14), (4) information updating (O12-rank 10), (5) policy support (financially) (C8-rank 7), (6) psychological distress (M14-rank 11).
In Table 6 for post-pandemic scenario for the UK case, it is observed that the COVID-19 related factors are less (3/15 factors) than the scenario in Chinese cities. Only factors of COVID-19 vaccination requirement, capability of self-caring at home (e.g., use COVID-19 lateral flow test), and COVID-19 equipment capability information. Similarly, we can also conclude the top 15 factors into seven aspects of concerns, which are (1) personal health condition (C2-rank 1, C3-rank 7), (2) healthcare capability (O1-rank 2, M5-rank 3, M1-rank 4, M7 rank 4, O10-rank 7, O8-rank 12, M2-rank 14), (3) policy regulation (O15-rank 6), (4) Transportation (O1-rank 7), (5) training (C12-rank 10), (6) information updating (O12-rank 10, O9-rank 13), and (7) financial support (C7-rank 15).
5.3 Factors changing between pre- and post-pandemic scenarios
To better understand the factors changing, we specify the factors that the ranks fluctuate over 16% (rank changing over or equal to ± 5). The rank change percentage and changing direction (i.e., whether the rank in post-pandemic scenario ascend, descend, or remain same comparing to the rank in pre-pandemic scenario) are presented in Table 7 and Table 8.
For the China case, there are 11 factors filtered and shown in Table 7. All the factors’ ranks descend comparing to scenario before the COVID-19 outbreak, which can be understood as “factors that are less important than before” from the respondents’ perspective. The factors changed the most (changing over -30% to -50%) relates to transportation (i.e., C10, O4), which indicate less importance of public and shared transportation, and to degree of healthcare environmental and service comfort (i.e., O8). In general, the changed factors relate to aspects of concerns for (1) healthcare non-COVID-19 capability (i.e., M2, M3, M6), (2) healthcare environment and service comfort (i.e., M5, O8), (3) financial support (i.e., C7), (4) medical level of the healthcare provider (i.e., M6), (5) transportation (i.e., C9, O4, C10, O1, O6).
For the UK case, there are 17 factors filtered and shown in Table 8. There are 4 factors’ ranks ascend (or “factors that are more important than before”) and 13 factors’ ranks descend (or “factors that are less important than before”) comparing to scenario before the COVID-19 outbreak. The most changing factors (changing over -30% to -40%) relate to public transportation (i.e., M3, C10) and availability of required pre-descriptive medicine. The ascending factors are higher medical level of healthcare provider, transfer efficiency among different medical level providers, capability of self-caring at home, and availability of private transportation infrastructure. In general, the changed factors relate to aspects of concerns are (1) medical level of healthcare provider (i.e., M7, O10), (2) training (i.e., C12), (3) healthcare environment and service comfort (i.e., O8), (4) healthcare non-COVID-19 capability (i.e., M2, M3), (5) financial support (i.e., C7, C6), (6) transportation (i.e., M4, C10, O6, O3, O5), (7) companion and communication (i.e., C4, M10), (8) digital application (i.e., C5), (9) health data security (i.e., M9).
5.4 The ranks difference of factors between the Chinese and the UK cases
It is noted that some of the factors’ ranks are very different between the two case. Table 9 displays the sorted 14 factors, ranks and the rank differences, where the factors are filtered if the rank difference is over 16% (rank difference over or equal to ± 5). If the rank difference value is positive, it indicates the factors rank higher in the UK cities scenario; If it is negative, it indicates the factors rank higher in the Chinese cities scenario.
The analysis reveals that COVID-19 related factors are valued differently (7 out of 14 factors) across countries, influenced by cultural differences. For instance, concerning factors such as whether healthcare facilities treat COVID-19 patients (O17), indoor mask mandates (O14), and the availability of public transportation infrastructure (O1), the rankings in the Chinese dataset (Rpost) are 2, 6, and 19, respectively. In contrast, in the UK case, these rankings (Rpost) are 20, 18, and 34, respectively. Additionally, regarding waiting times in healthcare facilities (M5), requirements for full COVID-19 vaccination (O15), the ability for self-care at home (C12), and the degree of comfort with medical services (O8), the Chinese case shows rankings (Rpost) of 16, 22, 26, and 28, respectively. In contrast, the rankings (Rpost) in the UK case are 3, 6, 10, and 12, respectively.
In general, the changed factors relate to aspects of concerns are related to (1) companion (i.e., C1), (2) training (i.e., C12), (3) transportation (i.e., O1, O3, O6), (4) healthcare environment and service comfort (i.e., O8, M5), (5) policy regulation (i.e., O13, O14, O15, O17), (6) healthcare capability (i.e., M8), and (7) psychological distress (i.e., M14). To conclude, the rank and the changes of the rank before and after COVID-19 indicate that that influence the healthcare accessing behaviour are affected by the cultural background in different countries.
6 Discussion of the behaviour-healthcare system-city
6.1 Citizen behaviours—changing
This study addressed the citizen behaviour change towards healthcare accessing after the COVID-19 outbreak by comparing the RII of the factors, which indicates that the changes are shaping. Moreover, based on the analysis and comparisons in the UK and China cases in Section 5, the total of 12 aspects of concerns for healthcare accessing in the post-pandemic era can be revealed and summarised in Fig. 3. According to the factors that each aspect contains, they are mapped in the COM-B model to illustrate the critical contributions in terms of capability, motivation, and opportunity.
In Fig. 3, COVID-19 regarded as a global public health crisis, has directly affected human beings, which has potentially stimulated interventions (i.e., factors) that have been studied in this research. According to the feature of the original COM-B model, capability, motivation, and opportunity can all influence behaviour and vice versa (Michie et al., 2011). This indicates that the healthcare accessing behaviour can probably be managed to achieve the desired usage state of the healthcare system by considering the 12 aspects. Especially, given capability and opportunity can have the single-headed arrow for motivation (Michie et al., 2011), which implies the enabling of capability and opportunity aspects can potentially accelerate the healthcare behaviour change influenced by motivation. For example, the effective and real-time information updating of the medical resources in the healthcare in opportunity category can possibly affect citizens’ emotional feelings (which is a partial explanation of motivation) and better influence the healthcare accessing behaviour (Anderson et al., 2021; Holmes et al., 2020). Additionally, the detailed factors in the 12 aspects affecting the healthcare accessing behaviour might vary depending on different cultural background (Section 5.4). Ideally, the cultural background influences might indicate diverse perspectives such as healthcare system differences, values, beliefs, knowledge etc. (Napier et al., 2014), which require sophisticated studies in the future.
It should be noted that motivation as a key component among all the others, most aspects under it can be enabled to some extent at the healthcare system level. For example, the medical resources regarding equipment and physicians can be re-allocated within the management of the healthcare (Emanuel et al., 2020). However, several aspects especially in capability and opportunity categories (e.g., transportation, training and education, financial capability, digital application, information updating, policy support) cannot be fully achieved solely relying on efforts at the healthcare system level. For instance, the policy support aspect for COVID-19 has been enacted at the city level and even national level so that the infection can be controlled effectively (Bavel et al., 2020). Therefore, it is revealed that, in order to gradually guide the healthcare accessing behaviour while not causing dramatic increase of healthcare usage in public health crisis, reactions should be made not only from the system-level but also from the city-level perspective.
6.2 Healthcare systems—requirements
To further unearth how the healthcare system has been influenced based on the 12 critical aspects of concerns, we figure out that the factors related to the healthcare accessing behaviour change have shown that the citizens’ requirements for the healthcare system are altering in the post-pandemic era. Specifically, the requirements can be discussed in the following 7 aspects.
Increase healthcare capability
The study results implied that citizens have been paying a lot more attention to the importance of healthcare capability, which transforms to a higher requirement for the healthcare system. First, the medical resources such as physicians, equipment, hospitalisation spaces for both COVID-19 and non-COVID-19 are highly required (i.e., the resources sufficiency is guaranteed) under the public health crisis. One evidence could be the increasing importance rank of the secondary-tertiary level of the healthcare provider (M7) and decreasing importance rank of low threshold level of healthcare providers like community hospitals and GPs (M6) in both the Chinese and the UK case. Then, the healthcare capability of the environment and services provided is still important to citizens despite of the slight rank drop in the pandemic, such as the degree of congestion (O7). In general, a more efficient and medical resources sufficient healthcare system would be urgently anticipated by citizens after the outbreak of the public health crisis.
Enact policy support
The public’s emphasis on the COVID-19 related policy regulation (O14-O17) in the healthcare system indicates the immediate system level or city level policy support made by policy makers is required for the citizens. From a short-term perspective, the policies are needed to control the infection while ensuring the regular operation of the healthcare system. From a long-term perspective, more comprehensive policy supports including but not limited to health protection, financial aid and insurance coverage, special care needed group support are required to confront the public health crisis.
Enable transportation adaptation
While the public transportation is still the important factor for healthcare accessing (O1), the decreasing importance of the public transportation and shared cars connectivity to the healthcare reflects the worry of getting infected. To ensure the stability of safe accessibility to the healthcare, proper adaptation strategies on the transportation system are required and should be enabled in time for the public’s health and welfare. In addition, abrupt traffic control and shutdown of the public transportation might cause inconvenient for healthcare accessing, where the proactive transportation plans can be highly required.
Share real-time information
The information updating of the medical resources in the healthcare system has been valued very important in this study, which required the healthcare system or even the city-level organisations to take efforts together. This can allow the public to make moves in advance and increase the public’s confidence confronting the crisis. It is extremely important as experts have indicated in the journal of The Lancet Psychiatry that “Increasing people’s confidence and clarity in what they need to do fosters adherence to health behaviours, and can help people to manage psychological distress” (Holmes et al., 2020).
Require education and training
The study results have indicated that the capability of self-caring at home (C10) has been considered as an important factor, especially in the UK cities scenario. This required proper educational information distribution and training provision from the healthcare system such as how to conduct COVID-19 lateral flow test at home and COVID-19 home treatment plans. needed. Because as the survey results have shown that the current acceptance of digital platform (C5) was still high enough for the public to rely on. The instructions notice about how to use the digital platforms for medical advice (C11) and their credibility are also important. Additionally, given the high infection risks of COVID-19 (Murray, 2022), people might consider home treatment plans for other common illnesses (e.g., influenza) and chronic illnesses (e.g., kidney failure (Hsu et al., 2021)), which require more professional instructions and trainings from the healthcare system.
Provide companion and communication assist
Although the factor of low willingness to communicate (M10) had an obvious drop in the post-pandemic scenario, it is meaningful to address it in the long-term run to improve the healthcare services, especially under the extreme circumstances for people with special needs (e.g., disability, pregnancy, elderly). Besides, the companion for patients (C1, C4) is still preferred if the infection can be prevented. Hence, more diverse methods supporting companion and communication would be expected.
Concern health data protection in the long-term run
Based on the questionnaire result, it indicated that people would partially give up the personal health information (M9) facing the public health crisis. However, the data protection is always a vital and ethical issue in the healthcare system to be addressed. In the early and middle stages of the pandemic, COVID-19 patients health status and related personal information (e.g., mobility, behaviour) were used to track close contacts for infection control (Mbunge, 2020). And as the QR codes scan for COVID-19 negative or vaccine confirmation was required, it is concerned about the data ownership and sharing among organisations, data usages etc. Therefore, more strict health data protection would be expected by citizens.
In general, the behaviour changes can possibly imply an expanded requirements in diverse categories for the healthcare system. Particularly, the categories are interrelated instead of independent, which aligns with the original behaviour change wheel framework developed based on COM-B model (Michie et al., 2011). For instance, one of the results in this study indicated the increasing importance of secondary-tertiary hospitals and the decreasing importance of community hospitals/GPs. However, Giezendanner et al. concluded that individuals seemed to change their provider choice towards more easily accessible and low-threshold medical services facing COVID-19 pandemic in Switzerland (Giezendanner et al., 2021). In this case, the real-time information sharing of medical resources, scientific facts or governmental initiatives might be contributed to remedy the psychological distress (Holmes et al., 2020; Ting et al., 2020), so that the health capability requirement expansion can be limited. Nevertheless, the enlarged comprehensive requirements for the healthcare system cannot be realised efficiently and effectively based only on system-level actions (e.g., individual hospitals’ improvements of medical capability), higher-level responses and reactions are needed beyond the system-level actions.
6.3 Cities – resilience
Rethinking the influential factors of the behaviour changes and requirements impact on the healthcare system, the city level responses and reactions are in urgent need to improve the resilience of a city confronting the public health crisis like COVI-19, or other emergent incidents. To further explain the reciprocal relationships among the citizen behaviour, healthcare system and the city operation, and illustrate how the city resilience can be enabled, a novel behaviour-healthcare system-city model based on COM-B model has been proposed (Fig. 4).
As shown in Fig. 4, first, to understand the healthcare accessing behaviour changes facing the global pandemic of COVID-19, the COM-B model originated from behavioural science field are adopted as the foundation. Key aspects of concerns behind the behaviour changes have been identified based on analysis and comparison, where it is realised that city-level efforts are required to stabilise the behaviour changes in the public health crisis. Then, to further discuss and reveal the essence of the changed aspects, we propose that the factors changing of the healthcare accessing behaviour potentially imply citizens’ requirements changing for the healthcare system as discussed in Sect. 5.2. Supporting factors of each requirement category are summarised in Fig. 4. Third, the requirements for the healthcare system can only be better fulfilled from a city level perspective (i.e., the cities responses to city system’s requirements changing). Examples are given in Table 10.
Additionally, at the city level, people with diverse background and difference opinions or feedback could be involved. Hence, the decision-making on the healthcare system can be more deliberated forming policies and strategies for city emergencies. Also, for all the city level responses mentioned above, multiple stakeholders (e.g., governors, engineers, researchers, architects, urban planners) and organisations (e.g., diverse governmental departments, research institute, technology companies, design firms and construction enterprises) in cities other than healthcare related personnel could be involved to assist decision making for the healthcare system. And each category of response is interrelated and interdependent to some extent. Therefore, a city level emergency response mechanism involving multi-stakeholders can be established to answer the sharply increase requirements of the city system. In this sense, we argue that emergencies usually negatively (“-” in Fig. 4) influence citizen behaviours and city systems. On the opposite, if the changed behaviours and requirements can be well responded at the city level, the city systems and citizens would be positively (“ + ” in Fig. 4) in terms of the healthcare system operation stability and human being health and wellness in this study. Hence, the city resilience can be greatly improved.
7 Conclusion
This research addressed the citizen healthcare accessing behaviours changes based on a well-established COM-B model from behavioural science field in the post-pandemic era, and revealed their impacts on the healthcare system and the city operation. Consequently, the comprehensive framework of influential factors for healthcare accessing behaviour has been established (Table 1), which can be used to examine behaviour changes in the public health crisis like COVID-19 and potentially in other behaviour-related healthcare research in the future. Based on the framework, a questionnaire survey was conducted to assess the importance of the influential factors to the respondents in the China and the UK cases. A total number of 120 surveyed questionnaires (76 from the China case and 44 from the UK case) were collected and analysed with RII method. Analysis and comparisons were conducted in different scenarios, where the key aspects of concerns regarding healthcare accessing behaviour changes were revealed. Based on the findings, we discussed the implications of the healthcare accessing behaviour changes, and the influences on the healthcare system and the city. Specifically, we proposed city-level efforts should be encouraged tremendously. Further, the important influential factors causing the citizens’ behaviour change have become the expanded requirements for the healthcare system, which required immediate responses at the city level confronting city emergencies like COVID-19. Finally, a novel behaviour-healthcare system-city model based on COM-B model has been proposed and discussed. The study's limitation lies in the inability to determine the specific impacts of geographical locations, as the number of respondents from each location was very limited in the datasets of both countries. Ultimately, this model can be employed to “predict the unpredictability” (Batty, 2022) by city level stakeholders in the post-pandemic era to rethink how the city resilience can be better realised combing citizen behaviour changes and city systems.
References
Anderson, E., Brigden, A., Davies, A., Shepherd, E., & Ingram, J. (2021). Pregnant women’s experiences of social distancing behavioural guidelines during the Covid-19 pandemic ‘lockdown’in the UK, a qualitative interview study. BMC Public Health, 21(1), 1–12.
Angell, C., & Potoglou, D. (2022). An insight into the impacts of COVID-19 on work-related travel behaviours in the Cardiff Capital Region and following the UK’s first national lockdown. Cities, 124, 103602. https://doi.org/10.1016/j.cities.2022.103602
Arora, T., & Grey, I. (2020). Health behaviour changes during COVID-19 and the potential consequences: A mini-review. Journal of Health Psychology, 25(9), 1155–1163.
Bai, W., Cai, H., Liu, S., Liu, H., Qi, H., Chen, X., Liu, R., Cheung, T., Su, Z., & Ng, C. H. (2021). Attitudes toward COVID-19 vaccines in Chinese college students. International Journal of Biological Sciences, 17(6), 1469.
Barbieri, D. M., Lou, B., Passavanti, M., Hui, C., Lessa, D. A., Maharaj, B., Banerjee, A., Wang, F., Chang, K., & Naik, B. (2020). A survey dataset to evaluate the changes in mobility and transportation due to COVID-19 travel restrictions in Australia, Brazil, China, Ghana, India, Iran, Italy, Norway, South Africa. United States. Data in Brief, 33, 106459.
Barrutia, J. M., & Echebarria, C. (2021). Effect of the COVID-19 pandemic on public managers’ attitudes toward digital transformation. Technology in Society, 67, 101776. https://doi.org/10.1016/j.techsoc.2021.101776
Batty, M. (2022). The COVID years: Predictable unpredictability. Environment and Planning b: Urban Analytics and City Science, 49(1), 3–6. https://doi.org/10.1177/23998083211072588
Bavel, J. J. V., Baicker, K., Boggio, P. S., Capraro, V., Cichocka, A., Cikara, M., Crockett, M. J., Crum, A. J., Douglas, K. M., & Druckman, J. N. (2020). Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour, 4(5), 460–471.
Canas, L. S., Sudre, C. H., Capdevila Pujol, J., Polidori, L., Murray, B., Molteni, E., Graham, M. S., Klaser, K., Antonelli, M., Berry, S., Davies, R., Nguyen, L. H., Drew, D. A., Wolf, J., Chan, A. T., Spector, T., Steves, C. J., Ourselin, S., & Modat, M. (2021). Early detection of COVID-19 in the UK using self-reported symptoms: A large-scale, prospective, epidemiological surveillance study. The Lancet Digital Health, 3(9), e587–e598. https://doi.org/10.1016/S2589-7500(21)00131-X
Ceylan, Z. (2020). Estimation of COVID-19 prevalence in Italy, Spain, and France. Science of the Total Environment, 729, 138817.
Chater, A. M., Arden, M., Armitage, C., Byrne-Davis, L., Chadwick, P., Drury, J., Hart, J., Lewis, L., McBride, E., & Perriard-Abdoh, S. (2020). Behavioural science and disease prevention: Psychological guidance. British Psychological Society. http://hdl.handle.net/10547/623940
Chen, Y., Wang, A., Yi, B., Ding, K., Wang, H., Wang, J., Shi, H., Wang, S., & Xu, G. (2020). Epidemiological characteristics of infection in COVID-19 close contacts in Ningbo city. Zhonghua liu xing bing xue za zhi= Zhonghua liuxingbingxue zazhi, 41(5), 667–671.
Chivu, R.-G., Popa, I.-C., Mociu, A., Savin, P.-S., Popa, R.-I., & Orzan, A.-O. (2021). Sustainable Transformation of Consumer Behavior—Vector Modeling in Determining the Decision to Choose a Medical Service in the Context of COVID-19. Sustainability, 13(23), 13025.
Comber, A. J., Brunsdon, C., & Radburn, R. (2011). A spatial analysis of variations in health access: Linking geography, socio-economic status and access perceptions. International Journal of Health Geographics, 10(1), 1–11.
Dong, L., & Bouey, J. (2020). Public mental health crisis during COVID-19 pandemic. China. Emerging Infectious Diseases, 26(7), 1616.
Emanuel, E. J., Persad, G., Upshur, R., Thome, B., Parker, M., Glickman, A., Zhang, C., Boyle, C., Smith, M., & Phillips, J. P. (2020). Fair allocation of scarce medical resources in the time of Covid-19. Mass Medical Soc, 382, 2049–2055.
Feng, X., Xiu, C., Bai, L., Zhong, Y., & Wei, Y. (2020). Comprehensive evaluation of urban resilience based on the perspective of landscape pattern: A case study of Shenyang city. Cities, 104, 102722.
Ghorbanzadeh, M., Kim, K., Ozguven, E. E., & Horner, M. W. (2021). Spatial accessibility assessment of COVID-19 patients to healthcare facilities: A case study of Florida. Travel Behaviour and Society, 24, 95–101.
Giezendanner, S., Fischer, R., Hernandez, L. D., & Zeller, A. (2021). The use of health care during the SARS-CoV-2 pandemic: Repeated cross-sectional survey of the adult Swiss general population. BMC Public Health, 21(1), 1–10.
Grosios, K., Gahan, P. B., & Burbidge, J. (2010). Overview of healthcare in the UK. EPMA Journal, 1, 529–534.
Gündüz, M., Nielsen, Y., & Özdemir, M. (2013). Quantification of delay factors using the relative importance index method for construction projects in Turkey. Journal of Management in Engineering, 29(2), 133–139.
Handley, M. A., Harleman, E., Gonzalez-Mendez, E., Stotland, N. E., Althavale, P., Fisher, L., Martinez, D., Ko, J., Sausjord, I., & Rios, C. (2015). Applying the COM-B model to creation of an IT-enabled health coaching and resource linkage program for low-income Latina moms with recent gestational diabetes: The STAR MAMA program. Implementation Science, 11(1), 1–15.
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Silver, R. C., & Everall, I. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560.
Holt, G. D. (2014). Asking questions, analysing answers: Relative importance revisited. Construction Innovation, 14(1), 2–16. https://doi.org/10.1108/CI-06-2012-0035
Hsiao, W.W.-W., Le, T.-N., Pham, D. M., Ko, H.-H., Chang, H.-C., Lee, C.-C., Sharma, N., Lee, C.-K., & Chiang, W.-H. (2021). Recent advances in novel lateral flow technologies for detection of COVID-19. Biosensors, 11(9), 295.
Hsu, C. M., Weiner, D. E., Aweh, G., Miskulin, D. C., Manley, H. J., Stewart, C., Ladik, V., Hosford, J., Lacson, E. C., & Johnson, D. S. (2021). COVID-19 among US dialysis patients: Risk factors and outcomes from a national dialysis provider. American Journal of Kidney Diseases, 77(5), 748-756. e741.
Huang, J., Wang, H., Fan, M., Zhuo, A., Sun, Y., & Li, Y. (2020). Understanding the impact of the COVID-19 pandemic on transportation-related behaviors with human mobility data. In Proceedings of the 26th ACM SIGKDD international conference on knowledge discovery & data mining (pp. 3443–3450). https://doi.org/10.1145/3394486.3412856
IHME COVID-19 Health Service Utilization Forecasting Team, & Murray, C. J. (2020). Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. MedRxiv. https://doi.org/10.1101/2020.03.27.20043752
Jackson, C., Eliasson, Â. L., Barber, N., & Weinman, J. (2014). Applying COM-B to medication adherence: A suggested framework for research and interventions. European Health Psychologist, 16(1), 7–17.
Kang, J.-Y., Michels, A., Lyu, F., Wang, S., Agbodo, N., Freeman, V. L., & Wang, S. (2020). Rapidly measuring spatial accessibility of COVID-19 healthcare resources: A case study of Illinois, USA. International Journal of Health Geographics, 19(1), 1–17.
Kato, H., & Matsushita, D. (2021). Changes in walkable streets during the COVID-19 pandemic in a suburban city in the Osaka metropolitan area. Sustainability, 13(13), 7442.
Lai, X., Wang, M., Qin, C., Tan, L., Ran, L., Chen, D., Zhang, H., Shang, K., Xia, C., Wang, S., Xu, S., & Wang, W. (2020). Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital in Wuhan. China. JAMA Network Open, 3(5), e209666–e209666. https://doi.org/10.1001/jamanetworkopen.2020.9666
Lee, J.-E., Kim, H.-R., & Shin, H.-I. (2014). Accessibility of medical services for persons with disabilities: Comparison with the general population in Korea. Disability and Rehabilitation, 36(20), 1728–1734.
Litaker, D., Koroukian, S. M., & Love, T. E. (2005). Context and healthcare access: looking beyond the individual. Medical Care, 43(6), 531–540.
Liu, Z., & Stern, R. (2021). Quantifying the traffic impacts of the COVID-19 shutdown. Journal of Transportation Engineering, Part A: Systems, 147(5). https://doi.org/10.1061/JTEPBS.0000527
Lovett, A., Haynes, R., Sünnenberg, G., & Gale, S. (2002). Car travel time and accessibility by bus to general practitioner services: A study using patient registers and GIS. Social Science & Medicine, 55(1), 97–111.
Lu, C., Zhang, Z., & Lan, X. (2019). Impact of China’s referral reform on the equity and spatial accessibility of healthcare resources: A case study of Beijing. Social Science & Medicine, 235, 112386.
Lu, Q., Xie, X., Pitt, M., & Chen, L. (2021). Enabling the possibility of creating a new smart resilient city in the post-pandemic period. In Proceedings of the 27th annual conference 2021. Beyond 2021: Rebuilding the built environment post-covid, PRRES, 191.
Mao, L., & Nekorchuk, D. (2013). Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health & Place, 24, 115–122.
Mbunge, E. (2020). Integrating emerging technologies into COVID-19 contact tracing: Opportunities, challenges and pitfalls. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(6), 1631–1636.
Michie, S., & West, R. (2021). Sustained behavior change is key to preventing and tackling future pandemics. Nature Medicine, 27(5), 749–752.
Michie, S., Van Stralen, M. M., & West, R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6(1), 1–12.
Murray, C. J. (2022). COVID-19 will continue but the end of the pandemic is near. The Lancet, 399(10323), 417–419.
Nägga, K., Dong, H.-J., Marcusson, J., Skoglund, S. O., & Wressle, E. (2012). Health-related factors associated with hospitalization for old people: Comparisons of elderly aged 85 in a population cohort study. Archives of Gerontology and Geriatrics, 54(2), 391–397.
Napier, A. D. P., Ancarno, C. P., Butler, B. P., Calabrese, J. P., Chater, A. P., Chatterjee, H. P., Guesnet, F. P., Horne, R. P., Jacyna, S. P., Jadhav, S. M. D., Macdonald, A. P., Neuendorf, U. M., Parkhurst, A. P., Reynolds, R. P., Scambler, G. P., Shamdasani, S. P., Smith, S. Z. M., Stougaard-Nielsen, J. P., Thomson, L. P., . . . Woolf, K. P. (2014). Culture and health. The Lancet (British edition), 384(9954), 1607–1639. https://doi.org/10.1016/S0140-6736(14)61603-2
Nikiforiadis, A., Mitropoulos, L., Kopelias, P., Basbas, S., Stamatiadis, N., & Kroustali, S. (2022). Exploring mobility pattern changes between before, during and after COVID-19 lockdown periods for young adults. Cities, 125, 103662.
Perros, T., Allison, A. L., Tomei, J., & Parikh, P. (2022). Behavioural factors that drive stacking with traditional cooking fuels using the COM-B model. Nature Energy, 7(9), 886–898.
Powell, T., Bellin, E., & Ehrlich, A. R. (2020). Older adults and Covid-19: The Most vulnerable, the hardest hit. Hastings Center Report, 50(3), 61–63.
Qian, M., & Jiang, J. (2020). COVID-19 and social distancing. Journal of Public Health, 30, 259–261. https://doi.org/10.1007/s10389-020-01321-z
Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry, 33(2), e100213.
Riley, W. J. (2012). Health disparities: Gaps in access, quality and affordability of medical care. Transactions of the American Clinical and Climatological Association, 123, 167.
Rooshdi, R. R. R. M., Abd Majid, M. Z., Sahamir, S. R., & Ismail, N. A. A. (2018). Relative importance index of sustainable design and construction activities criteria for green highway. Chemical Engineering Transactions, 63, 151–156.
Rowe, F., Robinson, C., & Patias, N. (2022). Sensing global changes in local patterns of energy consumption in cities during the early stages of the COVID-19 pandemic. Cities, 129, 103808. https://doi.org/10.1016/j.cities.2022.103808
Saelens, B. E., Sallis, J. F., & Frank, L. D. (2003). Environmental correlates of walking and cycling: Findings from the transportation, urban design, and planning literatures. Annals of Behavioral Medicine, 25(2), 80–91.
Serafini, G., Parmigiani, B., Amerio, A., Aguglia, A., Sher, L., & Amore, M. (2020). The psychological impact of COVID-19 on the mental health in the general population. An International Journal of Medicine, 113(8), 31–537. https://doi.org/10.1093/qjmed/hcaa201
Shah, K., Kamrai, D., Mekala, H., Mann, B., Desai, K., & Patel, R. S. (2020). Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus, 12(3). https://doi.org/10.7759/cureus.7405
Su, Y., Liu, Z., Chang, J., Deng, Q., Zhang, Y., Liu, J., & Long, Y. (2022). Measuring accessibility to healthcare using taxi trajectories data: A case study of acute myocardial infarction cases in Beijing. International Journal of Health Policy and Management, 12. https://doi.org/10.34172/ijhpm.2022.6653
Sun, S., Xie, Z., Yu, K., Jiang, B., Zheng, S., & Pan, X. (2021). COVID-19 and healthcare system in China: Challenges and progression for a sustainable future. Globalization and Health, 17(1), 1–8.
The Rockefeller Foundation & Arup (2014). City resilience framework. The Rockefeller Foundation and ARUP, 928. https://www.urban-response.org/system/files/content/resource/files/main/city-resilience-framework-arup-april-2014.pdf. Accessed 20 Mar 2024
Ting, D. S. W., Carin, L., Dzau, V., & Wong, T. Y. (2020). Digital technology and COVID-19. Nature Medicine, 26(4), 459–461.
Troisi, O., Fenza, G., Grimaldi, M., & Loia, F. (2022). Covid-19 sentiments in smart cities: The role of technology anxiety before and during the pandemic. Computers in Human Behavior, 126, 106986.
Wan, N., Zou, B., & Sternberg, T. (2012). A three-step floating catchment area method for analyzing spatial access to health services. International Journal of Geographical Information Science, 26(6), 1073–1089.
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., Choo, F. N., Tran, B., Ho, R., & Sharma, V. K. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48.
Watanabe, M. (2020). The COVID-19 pandemic in Japan. Surgery Today, 50(8), 787–793.
West, R., Michie, S., Rubin, G. J., & Amlôt, R. (2020). Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nature Human Behaviour, 4(5), 451–459.
White, D. B., & Lo, B. (2020). A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA, 323(18), 1773–1774. https://doi.org/10.1001/jama.2020.5046
Wong, S. Y. S., Zhang, D., Sit, R. W. S., Yip, B. H. K., Chung, R.Y.-N., Wong, C. K. M., Chan, D. C. C., Sun, W., Kwok, K. O., & Mercer, S. W. (2020). Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. British Journal of General Practice, 70(700), e817–e824.
Wymant, C., Ferretti, L., Tsallis, D., Charalambides, M., Abeler-Dörner, L., Bonsall, D., Hinch, R., Kendall, M., Milsom, L., & Ayres, M. (2021). The epidemiological impact of the NHS COVID-19 app. Nature, 594(7863), 408–412.
Xie, J., Tong, Z., Guan, X., Du, B., Qiu, H., & Slutsky, A. S. (2020). Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Medicine, 46(5), 837–840. https://doi.org/10.1007/s00134-020-05979-7
Yi, B. (2021). An overview of the Chinese healthcare system. Hepatobiliary surgery and nutrition, 10(1), 93–95. https://doi.org/10.21037/hbsn-2021-3
You, N. (2021). Assessing equity of the spatial distribution of primary health care facilities in Fuzhou City, China: A comprehensive method. PLoS ONE, 16(12), e0261256.
Yu, Y., Lau, M. M., Jiang, H., & Lau, J. T. (2021). Prevalence and factors of the performed or scheduled COVID-19 vaccination in a Chinese adult general population in Hong Kong. Vaccines, 9(8), 847.
Zanobetti, A., O’neill, M. S., Gronlund, C. J., & Schwartz, J. D. (2012). Summer temperature variability and long-term survival among elderly people with chronic disease. Proceedings of the National Academy of Sciences, 109(17), 6608–6613.
Zhang, N., Jia, W., Wang, P., Dung, C.-H., Zhao, P., Leung, K., Su, B., Cheng, R., & Li, Y. (2021). Changes in local travel behaviour before and during the COVID-19 pandemic in Hong Kong. Cities, 112, 103139. https://doi.org/10.1016/j.cities.2021.103139
Funding
This project was funded the UCL-Peking University Strategic Partner Funds 2021/22.
Author information
Authors and Affiliations
Contributions
Jiayi Yan: Writing – Original Draft, Investigation, Visualization; Zigeng Fang: Writing – Original Draft, Investigation, Visualization; Qiuchen Lu: Conceptualization, Methodology, Writing – Review & Editing, Supervision, Project administration, Funding acquisition; Junqing Tang: Conceptualization, Methodology, Writing – Review & Editing, Supervision, Project administration, Funding acquisition; Long Chen: Conceptualization, Methodology, Writing – Review & Editing, Supervision; Xuhui Lin: Writing – Original Draft, Investigation, Visualization;
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yan, J., Fang, Z., Chen, L. et al. Rethinking the city resilience: COM-B model-based analysis of healthcare accessing behaviour changes affected by COVID-19. J Hous and the Built Environ (2024). https://doi.org/10.1007/s10901-024-10120-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10901-024-10120-x