Abstract
Gay, bisexual and other men who have sex with men (GBMSM) and transgender individuals face heightened risks of HIV and other sexually transmitted infections (STIs). Surveillance within these populations is critical, and community testing services play a pivotal role in preventing and controlling HIV and STIs. This study investigates the trends in HIV, syphilis and hepatitis C (HCV) infections among participants in an apps-driven rapid test program from 2016 to 2023 in Barcelona, Spain, examining associated factors. Trend analysis utilized Wilcoxon-type test and associated factors were determined through multivariate logistic analysis. The prevalence of new HIV diagnosis was 1.81% (CI 1.18–2.64), active syphilis was 3.37% (CI 2.46–4.50) and acute HCV was 0.40% (CI 0.11–1.02). While infection rates showed no significant changes, there was significant increasing in sex work and chemsex and decreasing in condom use. Additionally, a peak in dating apps use for sex and a specific reduction in number of sexual partners were observed in 2020. Factors associated with HIV diagnoses included migrant status (aOR = 11.19; CI 2.58–48.53) and inconsistent condom use during the previous 12 months (aOR = 3.12; CI 1.02–9.51). For syphilis, associated factors were migrant status (aOR = 2.46; CI 1.14–5.29), inconsistent condom use (aOR = 3.38; CI 1.37–8.36), and chemsex practice during the previous 12 months (aOR = 2.80; CI 1.24–6.30). Our findings emphasize the need for tailored interventions, including culturally sensitive outreach for migrants and comprehensive strategies addressing substance use in sexual contexts. Technological innovations and targeted educational initiatives could reduce the burden of HIV and STIs within the GBMSM and transgender communities, providing valuable insights for public health strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gay, bisexual and other men who have sex with men (GBMSM), as well as transgender people, continue to face a disproportionate burden of HIV and other sexually transmitted infections (STIs). For example, they represented 40% of new HIV infections in Europe in 2021 and 68% of syphilis cases in 2019 [1, 2]. Multiple factors contribute to this disparity, including social stigma, discrimination and limited access to healthcare resources, leading to risky behaviours that increase the risk of HIV and STIs acquisition [3, 4]. Effective prevention and intervention strategies tailored to the unique challenges faced by these populations are urgently needed [5].
Surveillance within key populations, such as GBMSM and transgender individuals, plays a crucial role in improving their sexual health. It provides direct insights into infections and sexual behaviour, enabling timely responses. For instance, trend analysis of annual infection prevalence and specific variables can enhance surveillance, facilitating potential interventions in these key populations [6].
Community testing services are pivotal in preventing and controlling HIV and STIs as they can reach at-risk populations. Their significance is evident in behaviour change, increased testing frequency, viral suppression and early diagnosis of HIV and STIs [7,8,9]. International organizations recognize the importance of community-based testing for key populations, such as GBMSM, transgender individuals, migrants and sex workers [5, 10]. These services are commonly provided by community-led or peer-led organizations, often using point-of-care testing (POCT) strategies to reduce testing barriers [11].
Surveillance systems for HIV and STIs must be adaptable to specific settings and available resources. The incorporation of community testing significantly enhances the effectiveness of these systems by providing crucial and timely information [12, 13].
In recent years, dating apps and emerging technologies have gained attention as potential platforms for reaching GBMSM and transgender individuals and implementing preventive measures, complementing community efforts [14]. Their widespread use presents an opportunity to engage with these populations in innovative ways, such as promoting HIV/STI testing and providing access to essential healthcare services. Utilising these platforms, public health initiatives can directly target at-risk individuals, increase testing rates and facilitate the implementation of timely preventive strategies [5, 15, 16].
Dating apps have become essential tools for social and sexual interactions among GBMSM [17, 18]. They offer a convenient platform for individuals to connect with potential partners, leading to both personal and sexual encounters [19]. However, the use of dating apps in this population has been associated with an increased risk of acquiring HIV and other STIs, as well as engaging in higher-risk sexual behaviours, such as lower condom use and more sexual partners [20,21,22]. Furthermore, these risks extend beyond sexual behaviours, to include factors such as chemsex (the sexualized use of drugs), mental health problems and problematic use of the apps [23,24,25,26]. These factors contribute to the vulnerability of these populations to STIs, especially among those who are already HIV positive [27, 28].
The Public Health Agency of Barcelona (ASPB) has developed various interventions aimed to address the needs of GBMSM and transgender populations, such as Hepatitis A vaccination in response to outbreaks and the introduction of HIV testing in saunas in 2007 [29,30,31]. In 2015, ASPB initiated a pilot program to assess the response, acceptability and effectiveness of a POCT service for HIV and STIs testing and hepatitis A/B vaccination through dating apps [32]. This intervention expanded to community and primary health care centres between 2016 and 2019, with evaluations conducted to assess territorial differences [33]. Since 2019, the work has been centralized within the ASPB, establishing it as a “Rapid test program” for GBMSM and gender minorities. It offers regular testing services for HIV, syphilis, and hepatitis C (HCV), with the addition of papilloma virus vaccination for individuals under 27 years old. The intervention through dating apps and other technologies has intensified, with ASPB having eight active profiles on various dating apps, a WhatsApp Business account with a catalogue and automatic responses, and a website for scheduling testing appointments. Since 2021, the project also has an Instagram account, increasing participants recruited outside of dating apps.
Understanding the factors contributing to the transmission of HIV and other STIs among GBMSM, along with their temporal evolution, is crucial for developing effective prevention strategies [34]. By identifying associated factors, public health interventions can be tailored to address the specific needs of this population, reducing transmission rates and improving overall health outcomes [33, 35, 36]. This study aims to assess the annual trends in new diagnoses for HIV, acute syphilis and active HCV infection rates among GBMSM participating in ASPB’s Rapid Test Program over 8 years. Additionally, it aims to identify sociodemographic and behavioural variables associated with an increased risk for HIV, syphilis and hepatitis C infections.
Methods
This was a study conducted in the city of Barcelona, Spain. The study subjects included were GBMSM and transgender individuals who voluntarily participated in any of the actions carried out by the researchers of the rapid testing program of the ASPB between the years 2016 and 2023 [32].
From 2016 to 2019, the recruitment was initiated by the provider through the ASPB profile in the dating apps, with invitations in the form of images, sent directly to dating apps users who were close to any of the diverse spots across the city. Since 2019, the recruitment has been voluntary initiated by the users themselves, allowing them to start a conversation on any available platform or request an appointment through the website.
Participants were offered HIV (Determine™ HIV Early Detect) and syphilis (Determine™ Syphilis TP) rapid testing and in some cases, HCV rapid testing (Oraquick® HCV). Individuals were tested only for not known previous infection for HIV, syphilis and/or HCV. Hepatitis A and B vaccination was offered in those non-vaccinated. Since 2019, HPV vaccination service was introduced through advertisements on some apps, offering free vaccination to GBMSM under 27 years old, as the protocol indicates.
All tested individuals received pre- and post-test counselling during the same visit. Reactive cases were referred for confirmation to an STI specific centre, their primary care centre, or their respective hospital, following the local protocol. Access to healthcare was provided to migrants without sanitary card for any STI diagnose. Although some patients continued visiting the centre to complete vaccination or regular testing, for study purposes, we included only the first visit for each participant.
Three different questionnaires have been used during this period, each related to different grants and research objectives. Nevertheless, sociodemographic information, sexual health and some sexual behaviours have remained consistent across the surveys. Those aspects that required harmonization were categorized as either lifetime or last year, depending on the availability of data.
Variables
The dependent variables in this study were new HIV, acute syphilis and active HCV diagnoses. Independent sociodemographic variables included age as a numerical value and migrant status. Sexual health variables included any STI diagnosis the last 12 months, previous HIV testing and HIV serostatus. Behavioural variables included involvement in sex work, defined as receiving money or drugs in exchange for sex; the use of dating apps for sexual encounters; condom use during the last 12 months (always vs. not always), defining inconsistent condom use as the “not always” answer; the number of sexual partners during the last 12 months (less than 10, 10 or more); and the practice of chemsex during the last 12 months. Chemsex practice was defined as the use of methamphetamine, GHB/GBL or mephedrone with the intention of enhancing sexual experiences.
Data Analysis
This was a cross-sectional and trends analysis. For trend analysis, we calculated both the total and annual prevalence proportions of new HIV, acute syphilis, and active HCV infections. The same methodology was applied to the main sociodemographic and behavioural variables, including migration status, involvement in sex work, use of dating apps for sexual purposes, condom use, number of sexual partners, and chemsex practice. Additional trend analysis was conducted for prophylaxis pre-exposition (PrEP) usage, although this data was only available from 2021 onwards. Trend tests were performed using a Wilcoxon-type test for each variable, and graphical content was generated by including trend test p-values.
Descriptive univariate analysis was performed on the sociodemographic, sexual health and behavioural characteristics of the tested individuals, presenting proportions for categorical data and medians with interquartile range (IQR) for numerical variables. In addition, bivariate analysis was conducted to examine the relationship with the main outcome using the chi-square test, presenting proportions and p-values. Analysis for associated factors to active HCV infections were not carried out due to the small sample size of cases. Lastly, a multivariate logistic regression analysis was performed to identify factors associated with HIV/STI infections, presenting the adjusted Odds Ratios (aOR), 95% confidence intervals (CI) and p-values. For model construction, we explored all potential equations [37], adjusting for variables with > 90% confidence, age and dating apps using for sex, given its epidemiological significance.
Ethical Aspects
The study was approved by the research ethics committee of Parc de Salut Mar (No. 2016/6984/I). All data were anonymized, and informed consent was obtained. Information was handled in accordance with the data storage procedures stipulated in Organic Law 3/2018 on personal data protection and guarantee of digital rights.
Results
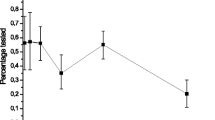
In total, 1502 tested GBMSM and transgender were included. The prevalence of new diagnoses for HIV was 1.81% (CI 1.18–2.64), 3.37% (CI 2.46–4.50) for active syphilis and 0.40% (CI 0.11–1.02) for acute HCV. Annual trends can be observed in Fig. 1. Based on the testing data, the total number of tested individuals was highest in 2020 and lowest in 2019. There were not statistically significant changes in the annual trends for HIV, syphilis or HCV infections.
Annual trends of HIV, syphilis and hepatitis C infection, demographic and behavioural variables in a rapid testing through dating apps for GBMSM in Barcelona, Spain. 2016–2023. P-values of test for trend across ordered groups. a HIV syphilis and hepatitis C proportion and number of total tested people per year; b Proportion of migrant people; c Proportion of people who reported having sex for money or goods; d Proportion of people who use dating apps for sex meetings; e Proportion of people reporting not always condom use during last 12 months; f Proportion of people reporting 10 or more sexual partners during last 12 months; g Proportion of people who reported chemsex practice (use of methamphetamine, GHB/GBL or mephedrone for sex)
According to the independent variables (Fig. 1), the proportion of migrant people showed stable trends around 50% (p = 0.187). Sex work had a significant increase across the years, rising from 10.9% in 2016 to 20.0% in 2023, with a peak of 23.7% in 2021 (p < 0.001). The use of dating apps for sexual purposes remained relatively stable at around 75%, but experienced a significant peak in 2020, reaching 86.9% (p = 0.002). Consistent use of condom decreased significantly from 44.3% in 2016 to 20.0% in 2023 (p < 0.001). The use of PrEP (not shown) did not exhibit significant changes (p = 0.234), with a proportion of 11.9% from 2021 to 2023. The number of sexual partners showed a significant decrease, with a prevalence of 64.6% of individuals having 10 or more partners in 2016 to 51.7% in 2021, with the lowest prevalence in 2019 and 2020 (p < 0.001). The practice of Chemsex experienced a substantial and sustained increase, rising from 6% in 2016 to 20.0% in 2023 (p < 0.001).
Univariate descriptive analysis is presented in Table 1. The median age of the tested users was 33 years old (IQR 26–38). Among them, 49.1% were foreign nationals, of which 69.4% were from Latin America and the Caribbean region of the World Health Organization, 9.1% from Southern Europe and 5.0% from Eastern Europe. According to health variables, 6.9% were new testers, 2.6% were people with known diagnosis of HIV and 23.0% had an STI in the previous 12 months. Behavioural variables showed that 17.0% had engaged in sex work, 77.4% had used dating apps for sexual encounters, 38.4% had consistently used condoms in the past 12 months, 45.2% had 10 or more sexual partners during the last 12 months and 10.4% had engaged in chemsex.
Bivariate analysis (Table 1) showed that variables associated with new HIV diagnoses in the sample were a higher migrant situation (p < 0.001) and lower condom usage (p = 0.010). A marginally associated variable was a higher number of sexual partners (p = 0.052). In the case of acute syphilis diagnosis, associated variables were lower condom use (p = 0.006), a higher number of sexual partners (p = 0.005), and a higher proportion of chemsex practice (p < 0.001).
Finally, in the multivariate analysis (Table 2), the associated factors with new HIV diagnosis were migrant status (aOR = 11.19; CI 2.58–48.53), and inconsistent condom use during the previous 12 months (aOR = 3.12; CI 1.02–9.51). The associated factors with acute syphilis diagnosis were migrant status (aOR = 2.46; CI 1.14–5.29), inconsistent condom use during the previous 12 months (aOR = 3.38; CI 1.37–8.36), and chemsex practice during the previous 12 months (aOR = 2.80; CI 1.24–6.30).
Discussion
Trends Analysis
The study’s results provide a comprehensive overview of the annual prevalence of new HIV, acute syphilis and active HCV infections among the tested population. Our study reveals a higher prevalence compared to the annual incidence in men within the city, with a 0.02% of HIV infection and 0.14% of syphilis in 2022 [38]. In contrast, the EMIS-2017 study reported a prevalence of 1.3% for HIV and 5.4% for syphilis among Spanish GBMSM39, which closely mirrors our findings.
The lack of significant changes in the trend of new HIV and acute syphilis diagnoses over the 8 year period, as it has been reported in the city rates [39], highlight the persistent challenges in prevention and the need for innovative interventions. Unlike European data, active HCV infections remained stable in our study [40]. This may be because HCV infections primarily affects to HIV-positive GBMSM, who were less likely to visit our facilities due to ongoing care. A recent study in Spain indicated a 0.52% prevalence among HIV-negative GBMSM, slightly higher than our findings, and identified associated factors such as the use of sexualized drugs associated with infection [41].
Notably, the number of individuals engaging with the ASPB’s Rapid Test Programme for the first time increased in 2020, during the COVID-19 pandemic. This may be attributed to increased apps usage during the COVID-19 pandemic [42] and the closure of other sexual health services, driving more consultations with ASPB’s service [43]. This increasing may, also, explain the significant peak in the use of dating apps for sexual encounters in 2020.
Analysing the trends for independent variables further enriches the study’s findings and provides an opportunity to integrate this approach into public health surveillance to enhance interventions. As previously described, integrating community-based testing data into surveillance systems could improve monitoring and provide epidemiological insights about key populations [44].
The substantial proportion of migrant individuals suggests that dating apps are an effective platform for reaching this at-risk group. Existing literature indicates that migrant individuals face limited access to health promotion programmes and a lower proportion of linkage-to-care due to factors like discrimination and violence [45]. This is particularly significant when we consider that the majority of migrants come from developing countries. Additionally, a syndemic effect of being a migrant with HIV/ST-related risk behaviours and substance use further emphasizes the need for tailored interventions [46].
The significant increase in sex work, likely facilitated by dating apps [47], is noteworthy and may be influenced by economic factors. Moreover, men’s sex work has been associated with a high prevalence of HIV and STIs, risky behaviours as substance use and low condom usage, especially among migrant sex workers [48,49,50].
The decline in consistent condom use raises concerns about safe sexual practices, aligning with previous research indicating decreasing condom use among dating app users [20]. While PrEP, introduced in Spain in 2019, may contribute to this trend, it does not fully explain the low proportion of condom use. This highlights the need for renewed efforts to promote safer sex practices, including condom use, especially when engaging with unknown sexual partners through dating apps.
Changes in the number of sexual partners also warrant consideration. The lowest proportion was observed in 2019, possibly due to a small sample size. However, the decrease in 2020 was likely a result of COVID-19 restrictions, reducing social contact [42]. In 2021, this trend reversed rapidly, but from 2022 onwards, the increase has been less pronounced, possibly influenced by the global and local Monkeypox outbreak, where sexual contact among men was associated with its spread [51].
One of the most striking findings is the significant increase in chemsex practice over the study period. The association of Chemsex with higher infection rates highlights the interconnectedness of substance use and sexual health within this population and, more broadly among dating apps users [27]. Addressing chemsex requires comprehensive strategies targeting substance abuse and sexual risk behaviours, with dating apps serving as a potential platform for such initiatives [52].
Factors Associated to HIV and Syphilis Infection
The multivariate analysis delves deeper into the factors associated with new HIV and acute syphilis diagnoses. Migrant status emerges as a prominent risk factor for both infections, underscoring the need for culturally sensitive outreach and support for migrant individuals within the GBMSM community. Specific studies on migrants who use dating apps should be conducted, considering common factors associated with their health and well-being [45].
Inconsistent condom use appears as a common risk factor, emphasizing the need for educational campaigns promoting safer sex practices, including alternatives such as PrEP. Additionally, a more comprehensive evaluation of the concept of safe sex is warranted, beyond the sole assessment of condom use.
Furthermore, the association between chemsex practice and acute syphilis diagnosis aligns with previous research demonstrating the link between substance use and STI acquisition [53]. This underscores the urgent need for interventions addressing substance use and its impact on sexual behaviours.
Limitations and Strengths
The study’s limitations should be considered in interpreting the results and planning future research. The cross-sectional design does not establish causality but provides valuable information on associations and annual trends. The geographic focus on Barcelona may limit external validity, but similar behavioural and epidemiological trends in European big cities enhance the study’s relevance [54]. Although is collected since 2021, the absence of gender identity data in the prior questionnaire is a limitation for evaluating this very important variable, necessitating changes in data collection. Harmonization of variables strengths surveillance systems, so it should be considered when developing new instruments.
Despite these limitations, the study’s strengths lie in the interventions conducted by the Public Health Agency and their epidemiological surveillance department, developing a service that goes beyond outbreak response. The implemented measures lead us to believe that these interventions are necessary, as well as being a part of the routine duties of healthcare surveillance workers. Barcelona’s unique characteristics as a destination for GBMSM migration and tourism have contributed to the rapid spread of STIs. The results encourage the continued development of better interventions for all sexually active populations, with a real-time focus on key populations. The program has also established an improved surveillance method, offering timely information on sexual behaviours among GBMSM and transgender populations in the city, which can inform future interventions.
Conclusion
The present work shows a high prevalence of new HIV and acute syphilis diagnosis among GBHSH and transgender individuals who participate in a rapid test program through social networks. Also, there were an increasing trend in sex work, chemsex and decreasing in condom use, with a peak in apps use for sex in 2020. This study provides crucial insights into the evolving landscape of HIV, syphilis and HCV infection and factors associated. The findings shed light on persistent challenges, such as low condom use, high-risk sexual behaviours, and the growing concern of chemsex. Addressing these challenges requires multifaceted interventions that combine technological innovations with targeted education and support. As well, this program has improved surveillance data, which can be used for future interventions in the city. By understanding the complex interplay of sociodemographic and behavioural factors, public health initiatives can tailor interventions to address the unique needs of the GBMSM community and work towards reducing the burden of HIV and STIs.
References
European Centre for Disease Prevention and Control/WHO Regional Office for Europe. (2022). HIV/AIDS surveillance in Europe 2022. Stockholm. https://www.ecdc.europa.eu/sites/default/files/documents/2022-Annual_HIV_Report_final.pdf
European Centre for Disease Prevention and Control. (2022). Annual epidemiological report 2019—syphilis. Stockholm. https://www.ecdc.europa.eu/sites/default/files/documents/syphilis-annual-epidemiological-report-2019.pdf
Babel, R. A., Wang, P., Alessi, E. J., Raymond, H. F., & Wei, C. (2021). Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: A scoping review. AIDS Behavior, 25, 3574–3604. https://doi.org/10.1007/s10461-021-03262-4
Poteat, T., Scheim, A., Xavier, J., Reisner, S., & Baral, S. (2016). Global epidemiology of HIV infection and related syndemics affecting transgender people. Journal of Acquired Immune Deficiency Syndromes, 72, S210.
European Centre for Disease Prevention and Control. (2021). Technologies, strategies and approaches for testing populations at risk of sexually transmitted infections in the EU/EEA. Stockholm
Leichliter, J. S., Dittus, P. J., Copen, C. E., & Aral, S. O. (2020). Trends in factors indicating increased risk for STI among key subpopulations in the United States, 2002–2015. Sex Transmitted Infections, 96, 121–123.
Fonner, V. A., Denison, J., Kennedy, C. E., O’Reilly, K., & Sweat, M. (2012). Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane Database of Systematic Reviews, 9, CD00224.
Paschen-Wolff, M. M., Restar, A., Gandhi, A. D., Serafino, S., & Sandfort, T. (2019). A systematic review of interventions that promote frequent HIV testing. AIDS Behavior, 23, 860.
Dave, S., Peter, T., Fogarty, C., Karatzas, N., Belinsky, N., & Pai, N. P. (2019). Which community-based HIV initiatives are effective in achieving UNAIDS 90–90–90 targets? A systematic review and meta-analysis of evidence (2007–2018). PLoS ONE, 14, e0219826.
World Health Organization. (2022). Consolidated guidelines on HIV, viral hepatitis and STI prevention, diagnosis, treatment and care for key populations. Geneva: WHO Guidelines.
Mullens, A. B., Duyker, J., Brownlow, C., Lemoire, J., Daken, K., & Gow, J. (2019). Point-of-care testing (POCT) for HIV/STI targeting MSM in regional Australia at community “beat” locations. BMC Health Services Research, 19, 1–10. https://doi.org/10.1186/s12913-019-3899-2
Mohammed, H., Hughes, G., & Fenton, K. A. (2016). Surveillance systems for sexually transmitted infections: A global review. Current Opinion in Infectious Diseases, 29, 64–69.
Fernàndez-López, L., Baros, S., Niedźwiedzka-Stadnik, M., Staneková, D. V., Rosińska, M., Simic, D., et al. (2021). Integration of community-based testing data into national HIV surveillance in Poland, Serbia and Slovakia within the framework of INTEGRATE project. BMC Infectious Diseases, 21, 1–10. https://doi.org/10.1186/s12879-021-06498-6
Sullivan, P. S., Jones, J., Kishore, N., & Stephenson, R. (2015). The roles of technology in primary HIV prevention for men who have sex with men. Current HIV/AIDS Reports, 12, 481–488. https://doi.org/10.1007/s11904-015-0293-5
Burns, K., Keating, P., & Free, C. (2016). A systematic review of randomised control trials of sexual health interventions delivered by mobile technologies. BMC Public Health. https://doi.org/10.1186/s12889-016-3408-z
Xin, M., Viswanath, K., Li, A. Y. C., Cao, W., Hu, Y., Lau, J. T. F., & Kit-Han Mo, P. (2020). The effectiveness of electronic health interventions for promoting HIV-preventive behaviors among men who have sex with men: meta-analysis based on an integrative framework of design and implementation features. Journal of Medical Internet Research. https://doi.org/10.2196/15977
Mustanski, B., Lyons, T., & Garcia, S. C. (2011). Internet use and sexual health of young men who have sex with men: A mixed-methods study. Archives of Sexual Behavior., 40, 289.
Alarcón-Gutiérrez, M., Palma Díaz, D., ArandoLasagabaster, M., De Olalla, G., & Rizo, P. (2022). Prevalence of dating app usage in gay, bisexual and other men who have sex with men (GBMSM). Enfermedades Emergentes, 21, 73–80.
Licoppe, C., Rivière, C. A., & Morel, J. (2016). Grindr casual hook-ups as interactional achievements. New Media & Society, 18, 2540–2558. https://doi.org/10.1177/1461444815589702
Wu, S., & Trottier, D. (2022). Dating apps: a literature review. Annals of the International Communication Association. https://doi.org/10.1080/23808985.2022.2069046
O’Connor, L., O’Donnell, K., Barrett, P., Hickson, F. C. I., McCartney, D., Quinlan, M., Mick, Q., Alicia, B., Margaret, F., & Derval, I. (2019). Use of geosocial networking applications is independently associated with diagnosis of STI among men who have sex with men testing for STIs: Findings from the cross-sectional MSM Internet Survey Ireland (MISI) 2015. Sexually Transmitted Infections., 95, 279–284.
Choi, E. P. H., Wong, J. Y. H., & Fong, D. Y. T. (2016). The use of social networking applications of smartphone and associated sexual risks in lesbian, gay, bisexual, and transgender populations: A systematic review The use of social networking appl. AIDS Care Psychological and Socio-medical Aspects of AIDS/HIV., 29, 145–155.
Hegazi, A., Lee, M., Whittaker, W., Green, S., Simms, R., Cutts, R., Nagington, M., Nathan, B., & Pakianathan, M. R. (2017). Chemsex and the city: sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. International Journal of STD & AIDS., 28, 362–366.
Bonilla-Zorita, G., Griffiths, M. D., & Kuss, D. J. (2023). Dating app use and wellbeing: An application-based pilot study employing ecological momentary assessment and objective measures of use. International Journal of Environmental Research and Public Health., 20, 5631.
Holtzhausen, N., Fitzgerald, K., Thakur, I., Ashley, J., Rolfe, M., & Pit, S. W. (2020). Swipe-based dating applications use and its association with mental health outcomes: A cross-sectional study. BMC Psychology. https://doi.org/10.1186/s40359-020-0373-1
Filice, E., Raffoul, A., Meyer, S. B., & Neiterman, E. (2019). The influence of Grindr, a geosocial networking application, on body image in gay, bisexual and other men who have sex with men: An exploratory study. Body Image, 31, 59–70.
Pakianathan, M., Whittaker, W., Lee, M., Avery, J., Green, S., & Nathan, B. (2018). Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Medicine. https://doi.org/10.1111/hiv.12629
Tomkins, A., George, R., & Kliner, M. (2019). Sexualised drug taking among men who have sex with men: A systematic review. Perspectives in Public Health, 139, 23–33.
Tortajada, C., de Olalla, P. G., Pinto, R. M., Bosch, A., & Caylà, J. (2009). Outbreak of hepatitis a among men who have sex with men in Barcelona, Spain, September 2008–March 2009. Euro Surveillance, 14, 19175. https://doi.org/10.2807/ese.14.15.19175-en
Tortajada, C., de Olalla, P. G., Diez, E., Pinto, R. M., Bosch, A., Perez, U., Milagros, S., & Caylà, J. A. (2012). Hepatitis a among men who have sex with men in Barcelona, 1989–2010: Insufficient control and need for new approaches. BMC Infectious Diseases, 12, 11.
Jacques Aviñó, C., García de Olalla, P., Díez, E., Martín, S., & Caylà, J. A. (2015). Explanation of risky sexual behaviors in men who have sex with men. Gaceta Sanitaria, 29, 252–257.
Alarcón Gutiérrez, M., FernándezQuevedo, M., Martín Valle, S., Jacques-Aviñó, C., Díez David, E., & Caylà, J. A. (2018). Acceptability and effectiveness of using mobile applications to promote HIV and other STI testing among men who have sex with men in Barcelona, Spain. Sexually Transmitted Infections, 94, 443–448.
Alarcón Gutiérrez, M., Palma Díaz, D., Alberny Iglesias, M., Ruiz Riera, R., Guayta-Escolies, R., & García de Olalla, P. (2023). Response rate, acceptability and effectiveness of an intervention offering HIV/STI testing via apps among gay, bisexual, and other men who have sex with men in Barcelona, Spain, from 2016 to 2020. AIDS Behavior. https://doi.org/10.1007/s10461-023-04165-2
Rocha, G. M., Cândido, R. C. F., de Carvalho, N. P., Carvalho, E. G. A., Costa, A. A. M., Machado, I. V., da Cruz Pimenta, M. P., de Paula Júnior, J. A., Guimarães, M. D. C., & Padua, C. A. M. (2023). Strategies to increase HIV testing among men who have sex with men and transgender women: An integrative review. BMC Infectious Diseases. https://doi.org/10.1186/s12879-023-08124-z
Jenkins Hall, W., Sun, C. J., Tanner, A. E., Mann, L., Stowers, J., & Rhodes, S. D. (2017). HIV-prevention opportunities with GPS-based social and sexual networking applications for men who have sex with men with men. AIDS Education and Prevention., 29, 38–48.
Chow, J. Y., & Klausner, J. D. (2018). Use of geosocial networking applications to reach men who have sex with men: progress and opportunities for improvement. Sexually Transmitted Infections., 94, 396–397.
Samprit, C., & Hadi, A. S. (2015). Regression analysis by example (5th ed.). Hoboken: Wiley.
Barcelona’s Public Health Agency (ASPB). (2023). Epidemiology registry (unpublished data). Barcelona.
Agència de SalutPública de Barcelona. (2022). La salut a Barcelona 2021. Barcelona: Consorci Sanitari de Barcelona.
European Centre for Disease Prevention and Control. (2022). Hepatitis C annual epidemiological report for 2021. Stockholm.
Palma, D., Alarcón, M., García de Olalla, P., Guerras, J. M., Pericas, C., & García, J. (2023). Hepatitis C antibody prevalence and active hepatitis C infection in HIV-negative gay, bisexual, and other men who have sex with men in Barcelona and Madrid, Spain (March 2018–March 2021). IJID Regions, 8, 95–104.
Shilo, G., & Mor, Z. (2020). COVID-19 and the changes in the sexual behavior of men who have sex with men: Results of an online survey. Journal Sexual Medicine, 17, 1827–1834. https://doi.org/10.1016/j.jsxm.2020.07.085
Rao, A., Rucinski, K., Jarrett, B., Ackerman, B., Wallach, S., Marcus, J., Adamson, T., Garner, A., Santos, G. M., Beyrer, C., & Howell, S. (2021). Perceived interruptions to HIV prevention and treatment services associated with COVID-19 for gay, bisexual, and other men who have sex with men in 20 countries. JAIDS Journal of Acquired Immune Deficiency Syndromes, 87(1), 644–651.
Fernàndez-López, L., Klavs, I., Conway, A., Kustec, T., Serdt, M., & Baros, S. (2021). Recommendations for collection and integration of community-based testing and linkage to care data into national surveillance, monitoring and evaluation systems for HIV, viral hepatitis and sexually transmitted infections: results from the INTEGRATE joint. BMC Infectious Disease, 21, 794. https://doi.org/10.1186/s12879-021-06499-5
Yarwood, V., Checchi, F., Lau, K., & Zimmerman, C. (2022). LGBTQI+migrants: A systematic review and conceptual framework of health, safety and wellbeing during migration. International Journal of Environmental Research and Public Health, 19, 869.
Lewis, N. M., & Wilson, K. (2017). HIV risk behaviours among immigrant and ethnic minority gay and bisexual men in North America and Europe: A systematic review. Social Science and Medicine, 179, 115–128. https://doi.org/10.1016/j.socscimed.2017.02.033
Siegel, K., Cabán, M., Brown-Bradley, C. J., & Schrimshaw, E. W. (2023). Male sex workers strategies to manage client-related risks of violence. Journal of Interpersonal Violence. https://doi.org/10.1177/08862605231176804
Liu, S., & Detels, R. (2012). Recreational drug use: an emerging concern among venue-based male sex workers in China. Sexually Transmitted Disease, 39, 251–252.
Oldenburg, C. E., Perez-Brumer, A. G., Reisner, S. L., & Mimiaga, M. J. (2015). Transactional sex and the HIV epidemic among men who have sex with men (MSM): Results from a systematic review and meta-analysis. AIDS and Behavior, 19, 2177–2183.
Mcbride, B., Shannon, K., Strathdee, S., & Goldenberg, S. M. (2021). Structural determinants of HIV/STI prevalence, HIV/STI/SRH access, and condom use among immigrant sex workers globally: A systematic review HHS public access. AIDS, 35, 1461–1477.
Ogoina, D. (2022). Sexual behaviours and clinical course of human monkeypox in Spain. The Lancet, 400, 636–637.
Platteau, T., Herrijgers, C., & de Wit, J. (2020). Digital chemsex support and care: The potential of just-in-time adaptive interventions. International Journal of Drug Policy., 85, 102927.
González-Baeza, A., Dolengevich-Segal, H., Pérez-Valero, I., Cabello, A., Téllez, M. J., & Sanz, J. (2018). Sexualized drug use (Chemsex) is associated with high-risk sexual behaviors and sexually transmitted infections in HIV-positive men who have sex with men: Data from the U-SEX GESIDA 9416 study. AIDS Patient Care and STDs, 32, 112–118.
The EMIS Network. (2019). EMIS-2017 the European men-who-have-sex-with-men internet survey key findings from 50 countries EMIS-2017. In: The European men-who-have-sex-with-men internet survey other international financial contributions for EMIS-2017: Swedish Ministry of Health for RECR. Stockholm. www.ecdc.europa.eu
Acknowledgements
Special thanks to Mireia Alberny Iglesias and Rafael Ruiz Riera, from the Catalan’s Health Department, for their support in facilities in the city’s territory. Also, to Francisca Román Urrestarazu and Manuel Fernández Quevedo for program’s support and participation in interventions. Finally, we appreciate the support of the Epidemiology Service (SEPID) and the Preventive Programs and Interventions Service (SPIP) from the Public Health Agency of Barcelona (ASPB).
Funding
Open Access Funding provided by Universitat Autonoma de Barcelona. This study was funded by the Health Research Fund (FIS) PI 16/02025 of the Instituto de Salud Carlos III of the Ministry of Science and Innovation, Government of Spain.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Conceptualization: MAG, DPD. Data curation: MAG, DPD, MLFC. Formal Analysis: MAG. Funding acquisition: PGdO, CRG. Investigation: MAG, DPD. Methodology: MAG, DPD. Project administration: CRG. Resources: CRG, PGdO. Supervision: CRG, PGdO, LFL. Writing—original draft: MAG. Writing—review & editing: MAG, DPD, MLFC, LFL, CRG, PGdO.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The study was approved by the research ethics committee of Parc de Salut Mar Nº 2016/6984/I. All data were anonymised. Information was treated in accordance with the data storage procedures stipulated in Organic Law 3/2018 on personal data protection and guarantee of digital rights.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alarcón Gutiérrez, M., Palma Díaz, D., Forns Cantón, M. et al. Trends in Sexual Health of Gay, Bisexual, and Other Men Who Have Sex with Men, and Transgender Individuals: Apps Driven Testing Program for HIV and Other STIs in Barcelona, Spain (2016–2023). J Community Health 49, 429–438 (2024). https://doi.org/10.1007/s10900-023-01310-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-023-01310-9