Abstract
To examine the impact of a co-created culturally sensitive diabetes self-management education and support (DSMES) intervention on the physical and mental health of immigrants with type 2 diabetes (T2D). Pre- and post-test among people with T2D whose primary language was Urdu, Arabic or Turkish (n = 97). Participants were offered a six-week intervention based on a person-centred approach using research-based dialogue tools to facilitate learning and reflection, which was developed in co-creation with immigrants and healthcare professionals. Data were collected at baseline, post-intervention and after 6 months and analysed using paired t-tests, Wilcoxon signed-rank tests, chi-square tests and regression models when appropriate. Several clinical outcomes were improved post-intervention, including HbA1c (P < 0.001), body fat percentage (P = 0.002), self-rated general health (P = 0.05), well-being (P = 0.004) and several self-management behaviours, e.g., physical activity (P < 0.001). Most outcomes remained improved after 6 months, but the effect on HbA1c was no longer statistically significant. Some outcomes were improved only at 6 months, including waist circumference (P < 0.001) and diabetes-related emotional distress (P < 0.001). Fatigue did not change. Attendance at more programme sessions was associated with better outcomes. The DSMES intervention developed in a co-creation process was highly effective in improving the health of immigrants with T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes self-management education and support (DSMES) is a cornerstone of effective type 2 diabetes (T2D) treatment because it facilitates knowledge and skills that are essential for implementing and sustaining self-care behaviours [1, 2]. Attendance at DSMES programmes is associated with increased quality of life, reduced morbidity and mortality, and improved glycaemic control in populations with type 2 diabetes [1, 2]. However, immigrants with type 2 diabetes attend DSMES less often and benefit from it less than do other populations [3,4,5,6,7,8,9]. This may be attributed to the fact that traditional DSMES interventions do not often take into account differences in cultural beliefs and language abilities [10, 11]. Lack of cultural sensitivity, in addition to communication difficulties, lack of referrals, unfamiliarity in navigating the healthcare system, and stigmatisation may be a barrier for immigrants when accessing DSMES [12].
Several factors indicate that culturally sensitive DSMES interventions are needed. European studies indicate that immigrant groups born in non-Western countries have a higher risk of T2D, compared to the majority population [13,14,15]. In addition, immigrant groups and their descendants are at increased risk of developing complications of diabetes [7, 16]. In Denmark, the incidence of T2D and risk of both any type of retinopathy and diabetic retinopathy requiring referral are higher among immigrants born in Asia, Sub-Saharan Africa and the Middle East, compared with native Danes [17, 18].
Few studies have investigated the potential effects of culturally sensitive DSMES specifically targeting immigrant populations in a European context [19]. No established definitions of cultural sensitivity or cultural appropriateness exist, and cultural sensitivity exemplified in studies may vary in dose, content and format. According to Resnicow et al. [20], cultural sensitivity is the incorporation of the ethnic/cultural characteristics, experiences, norms, values, behavioural patterns, beliefs and environmental and social forces of the target population into the design, delivery, and evaluation of interventions. It includes surface structures, which match intervention content to observable characteristics of the target population, e.g., language or food preferences and deep structures reflecting an understanding of cultural, social, historical, environmental, and psychological forces influencing a specific health behaviour in the target population, such as fasting practices and family involvement [20].
Active involvement of the target group through co-creation in development is a way to ensure that a DSMES intervention meets the needs, preferences and resources of the target group [21]. Co-creation processes can increase the cultural sensitivity of interventions, which may lead to improved health outcomes [20].
This study explores the impact of a co-created and culturally sensitive group-based DSMES intervention, CUlturally Sensitive TOols and Methods (CUSTOM), on clinical outcomes, self-reported physical and mental health and self-management behaviours. The target population consisted of Urdu, Arabic and Turkish-speaking immigrants with T2D and limited skills in speaking Danish.
Methods
Study Design
CUSTOM is a complex intervention consisting of interacting components in the design, complex behaviour changes in those delivering and receiving the intervention and many stakeholders [22]. It examines impact using a pre- and post-test design. Data were collected at baseline (T1), post-intervention (T2) and at 6 months follow up (T3).
Recruitment and Inclusion Criteria
Participants were referred to diabetes rehabilitation by their general practitioners and were recruited at a diabetes centre in Copenhagen, Denmark. Recruitment took place in March 2019–June 2021. At their first consultation, individuals were asked to participate in the study if an interpreter was needed. Those interested in participating were contacted by a research nurse who screened them for study eligibility.
Inclusion criteria were age ≥ 18 years, clinical diagnosis of T2D, ability to give written consent, ability and willingness to attend and participate in a group-based education intervention and Arabic, Turkish or Urdu as first language. Potential participants were excluded if they had a physical illness that could substantially reduce life expectancy, serious mental illness, significant alcohol or substance misuse or a primary diagnosis of a learning disability or were pregnant, breastfeeding or planned to become pregnant during the study period. All participants were offered written and audiotaped information about the study in their preferred language (Danish, Arabic, Turkish or Urdu).
The CUSTOM Intervention
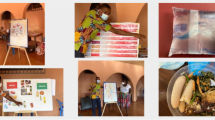
The DSMES intervention consisted of 6 weekly 2.5-h group sessions. The purpose was to support health-promoting decisions and improve daily diabetes self-management, and the intervention covered diabetes knowledge and complications, mental health, diet, exercise, blood sugar measurement and fasting. Eleven dialogue tools with images, cases, and illustrations and a comprehensive guide were developed to facilitate dialogue, learning, and reflection and promote diabetes-specific knowledge in group sessions. The intervention was delivered by an interdisciplinary team consisting of a nurse, dietician, physiotherapist and translator. Educators were trained in the theoretical foundation of CUSTOM, including cultural competence [23], a flourishing approach [24] and active listening [25]. Cultural competence includes awareness of social contexts and prejudices, the ability to transfer information to different patient groups and being flexible and creative in new situations [23]. The flourishing approach focuses on paying attention to patients’ strengths, what is going well, and successful experiences and approaches [24]. Active listening involves mirroring, in which health care professionals repeat what participants say and discuss the message of the communication with the patient [25].
CUSTOM was developed in co-creation with members of the target group, researchers from Steno Diabetes Centre Copenhagen and healthcare professionals from the Centre for Diabetes. The methodology of design thinking was used, which is a participatory approach in three phases: inspiration, ideation, and implementation [21, 26]. The project first entailed a needs assessment based on reviewing the literature, fieldwork and workshops with the target group and health care professionals. Ideation and development of the intervention were then undertaken with the active involvement of the target group in developing a prototype and prioritising and refining methods, materials, research tools and educational format. The final design phase consisted of prototype testing and refinement before implementation in practice. In workshops, the target group and health care professionals were actively involved in ideation, designing, testing, and prioritising final materials, methods, content and educational format. They also provided feedback about data collection, such as study information sheets and questionnaires. Throughout the design process, co-creation with the target group maintained a focus on cultural sensitivity in terms of both surface structure and deep structure. The intervention content and format are described in detail elsewhere [27].
Data Collection
At baseline visits, sociodemographic and background information were obtained from participants. Physical examinations and questionnaires were conducted by the research nurse 2 weeks or less before participants began the DSMES intervention, 2 weeks or less after the DSMES intervention ended and at approximately 6 months (± 21 days) after the intervention ended. The research nurse recorded participants’ questionnaire responses while they viewed the questions on printed versions. Questionnaires were translated into Arabic, Turkish and Urdu following international standards by submitting the questionnaire to forward- and back-translations and review by an academic committee [28].
Measures
Clinical Measures
HbA1c and Lipid Profile
A fingerstick blood sample of one drop was used to measure triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and glycated hemoglobin (HbA1c) measured on Alere Afinion™ HbA1c (Abbott, Chicago, IL). A strict protocol was followed for collecting blood samples and, to ensure accuracy, the HemoCue analyser was calibrated daily according to the manufacturer’s user instructions. An additional calibration was carried out monthly using a special test kit to verify measurement sensitivity and accuracy.
Bodyweight to the nearest 0.1 kg was measured with participants wearing lightweight indoor clothes and no shoes. Height without shoes to the nearest 0.1 cm was measured with a transportable wall-mounted stadiometer. Waist circumference to the nearest 0.5 cm was measured halfway between the lowest point of the costal margin and the highest point of the iliac crest at the end of expiration with participants in a standing position wearing light indoor clothing. Hip circumference to the nearest 0.1 cm was measured at the level of the greater femoral trochanter and measured at the end of expiration with participants standing. All anthropometrics were measured twice, and means were used in analyses. Body mass index (BMI) was calculated as weight/height2. Waist/hip circumference was calculated as waist circumference/hip circumference. Blood pressure was measured with participants sitting after at least 10 min of rest and without talking during measurement, which was repeated 3 times at two-minute intervals. The mean value was calculated and used in analyses. Body fat percentage was measured using the DC-360 body composition analyser (TANITA, Tokyo).
Questionnaire
Sociodemographic and Diabetes-Related Measures
Language, cohabitation status, educational level, employment status, years living in Denmark and comorbidity were assessed in the baseline questionnaire. Age, gender, diabetes duration, prescribed oral antihyperglycemic medication (types and dosages), antihypertensive medication (types and dosages), cholesterol-lowering medication (types and dosages), diabetes complications, and participation in intervention sessions were obtained from medical records.
Self-Reported Physical and Mental Health
Self-rated general health was measured using one item from the 12-item short-form health survey (SF-12) [29]. Well-being was measured using the WHO-5, which comprises five items measuring different aspects of well-being during the past 2 weeks [30]. Perceived diabetes-related emotional distress was measured using a short form of the Problem Areas in Diabetes (PAID-5) questionnaire [31]. Fatigue was measured with the Fatigue Assessment Scale (FAS), 10 items assessing symptoms of chronic fatigue [32]. When responses were missing on one or two items on WHO-5, PAID-5 or FAS, missing values were replaced by the mean value for the item among remaining participants. When three or more responses were missing, individuals were excluded from analyses including these scales.
Health Behaviours and Diabetes Self-Management
Smoking habits and alcohol consumption were measured using questions from the Danish National Health Profile [33, 34]. Diabetes self-management activities were measured using selected items from the Summary of Diabetes Self-Care Activities (SDSCA) scale [35].
Statistical Analysis
Descriptive statistics were used to assess baseline population characteristics. Changes between baseline and the end of the intervention and between baseline and 6 months were assessed with paired t-tests for approximately normally distributed continuous data, Wilcoxon signed-rank tests for non-normally distributed data and chi-square tests for categorical data. Results were expressed as means and standard deviations (SD) for normally distributed continuous data, medians and inter-quartile range (IQR) for non-normally distributed continuous data and counts and percentages for categorical data. Participants were included in analyses if they had a baseline assessment and an assessment at the end of the intervention or at 6 months. The relationship between DSMES attendance and outcome measures was assessed with general linear models (GLM) for continuous measures and logistic regression model for categorical measures. Residuals were approximately normally distributed, and variance in GLM estimates was generally homogenous. Statistical analyses were performed using SAS Studios version 3.8. The level of significance was set at P < 0.05 for all tests.
Implications of the COVID-19 Pandemic on the Study
The COVID-19 pandemic had some implications for the study. Initially, the intention was to include a control group with individuals in the target group attending other DSMES interventions in five municipalities in the Capital Region, Denmark. However, the pandemic substantially limited both recruitment to and execution of education interventions in the municipalities; as a result, data from the control group could not be included in the study.
Results
Sample Characteristics
A total of 120 individuals were invited to participate in the intervention, of whom 97 participated in the baseline assessment. Twelve were lost to follow up between baseline and the end of the intervention, while another 12 were lost to follow up after 6 months, resulting in a response rate of 75%.
Participants included more women than men, and mean age was 59 years. Most participants had no or limited education and were out of work (Table 1). One in five participants had been diagnosed with type 2 diabetes less than a year previously, while two in five had been diagnosed with diabetes more than 10 years previously. Most participants were prescribed antihyperglycemic medications, and the majority reported having both diabetes complications and comorbid conditions. Sixty-one (63%) participants completed five or six sessions of the intervention and 69 (71%) completed at least four sessions.
Clinical Outcomes, Self-Reported Physical and Mental Health and Self-Management
Changes from Baseline to Intervention End
Most clinical outcomes improved from baseline to the end of the intervention; HbA1c, weight, BMI, total cholesterol/HDL-C ratio, and body fat percentage improved significantly (Table 2). With regard to mental and physical health and self-management, significant improvements were seen in self-rated general health, well-being, and self-management activities of healthy diet, physical activity, and foot care. Nonsignificant improvements were observed for diabetes-related emotional distress, fatigue and checking blood sugar from baseline to end of intervention.
Changes from Baseline to Follow-Up
After 6 months, weight, BMI, body fat percentage, waist circumference, hip circumference, and HDL-cholesterol were significantly improved (Table 3). HbA1c and total cholesterol/HDL-C ratio also improved at 6 months follow up, albeit not to a statistically significant degree. Waist/hip ratio, systolic blood pressure, diastolic blood pressure, total cholesterol, LDL-C, and triglycerides remained unchanged at 6 months.
Healthy diet and physical activity were significantly improved at 6 months (Table 3). No changes were observed in well-being, fatigue and the self-management activities of foot care and taking diabetes medication at 6 months.
Attendance
There was a general tendency for frequency of DSMES attendance to be associated with improved outcomes at both the end of the intervention and follow up (Table 4). Some variables reached statistical significance.
Discussion
A co-created and culturally sensitive DSMES intervention improved clinical outcomes and self-reported mental and physical health among Urdu-, Turkish- and Arabic-speaking immigrants with type 2 diabetes in Denmark. Several outcomes, including HbA1c, weight, BMI, self-rated general health and the self-management activities of healthy diet and physical activity, significantly improved from pre- to post-intervention and from pre-intervention to follow up at 6 months. In addition, outcomes such as waist and hip circumference and diabetes-related emotional distress that were not significantly different at the end of the intervention were significantly improved at 6 months. In addition, more frequent DSMES session attendance tended to be associated with improved outcomes. Finally, we found very poor psychosocial health among the population at baseline, underscoring the need to consider immigrants from the target group as a hardly reached group that needs DSMES interventions targeted to their needs, perspectives, and preferences.
DSMES interventions targeting immigrants have shown limited effects in reducing HbA1c levels [36]. This could be related to a limited focus on cultural sensitivity in these interventions compared with the present study. A 2014 review showed that culturally appropriate health education targeting ethnic minority groups with type 2 diabetes has short‐ to medium‐term effects on glycaemic control, diabetes knowledge and healthy lifestyles [19]. However, previous studies did not find significant psychosocial improvements such as quality-of-life measures to the same extent we did. Notably, a vast majority (24/33 or 72%) of the review studies were conducted in the US and may not correspond to European and Danish healthcare structures or migration history. Moreover, previous studies also differ from ours in terms of defining and ensuring cultural sensitivity. Most studies do not describe how they provide or ensure cultural sensitivity [36] and the categorisation of cultural appropriateness or culturally sensitivity differs substantially within studies. For example, a review defined cultural appropriateness very broadly with one criterion being the delivery of an intervention to same-sex groups [19]. Notably, a recent UK study of a culturally tailored DSMES intervention drawing on co-design methods and targeting an ethnic minority group showed positive effects on several outcomes, including HbA1c, BMI and physical activity, compared to a control group [37].
How do we Maintain Effects After 6 Months?
The challenge with lifestyle changes is often maintain them over the long term. Previous studies have found that long-term lifestyle improvements among people with T2D, particularly behavioural changes such as diet and exercise, are often harder to achieve [38, 39]. In our study, many outcomes remained improved at 6 months, and some positive outcomes were only observed at 6 months.
CUSTOM is a complex interdisciplinary intervention consisting of several interacting components and based on person-centred theories, such as the flourishing approach. These characteristics may have contributed to the long-term effects we observed. A recent review similarly found that diabetes self-management educational interventions based on person-centred values, empowerment approach and relevant self-efficacy theory were more successful in obtaining positive outcomes [38]. Another review emphasised the advantage of community-based health promotion, establishing close ties between health care providers and community members [40].
In addition, several educational strategies may explain the positive outcomes we observed, such as using a visual representation of sessions to enhance participant retention; 71% of participants completed at least four sessions. Additional facilitators may have included clarifying the roles of interpreters, educators and participants and articulating why active involvement of the target group was important to benefitting from the intervention. The intervention focused both on physical and psychological aspects of diabetes, recognising the importance of mental health issues. In addition, active involvement of the target group through co-creation during design was likely to have ensured insight into and incorporated preferences of the target population for surface structures and deeper structures and forces influencing health behaviour.
Strengths and Limitations
Study strengths include a high participation rate, limited loss to follow-up, relatively long follow-up time and the combination of clinical and self-reported outcome measures. It should, however, be noted that HbA1c as a clinical measure of glycaemic control is associated with some uncertainty due to its variability over time and these variations in themselves have a health effect [41, 42]. Another study limitation was the lack of a control group, which precludes exploring causal relations. Performance bias cannot be ruled out because it was impossible to blind participants. The generalisability of our findings may be affected by heterogeneity between and within immigrant groups.
Conclusion
The co-created and culturally sensitive CUSTOM DSMES program was highly effective in improving short- and longer-term physical and mental health among persons speaking Urdu, Turkish and Arabic with T2D. Co-creation processes ensured the activation of local resources, which is recommended as a means to reducing ethnic health inequities. The theory, methods and tools of the CUSTOM program incorporate the preferences, needs and values of the target groups that would not have been identified or addressed by an exclusively researcher-driven process.
Data Availability
Data supporting the findings of this study are not publicly available due to privacy concerns of the participants. For further information, contact the corresponding author.
Code Availability
Code for data cleaning and analysis is available from the corresponding author upon request.
References
Beck, J., Greenwood, D. A., Blanton, L., Bollinger, S. T., Butcher, M. K., Condon, J. E., & Wang, J. (2021). 2017 national standards for diabetes self-management education and support. Science of Diabetes Self-Management and Care, 47(1), 14–29. https://doi.org/10.1177/0145721720987926
Chrvala, C. A., Sherr, D., & Lipman, R. D. (2016). Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Education and Counseling. https://doi.org/10.1016/j.pec.2015.11.003
Ahlmark, N. (2015). Control and recognition in diabetes management: Social practices and meanings surrounding diabetes management in training and everyday life of Arab immigrants in Denmark : PhD Thesis
Coonrod, B. A., Betschart, J., & Harris, M. I. (1994). Frequency and determinants of diabetes patient education among adults in the U.S. population. Diabetes Care, 17(8), 852–858. https://doi.org/10.2337/diacare.17.8.852
Hempler, N. F., Nicic, S., Ewers, B., & Willaing, I. (2015). Dietary education must fit into everyday life: A qualitative study of people with a Pakistani background and type 2 diabetes. Patient Preference and Adherence, 9, 347–354. https://doi.org/10.2147/PPA.S77380
Johansen, K. S., Rasmussen, P. S., & Christiansen, A. H. (2012). Hvem deltager og hvem deltager ikke i patient-uddannelse. Kora
Lanting, L. C., Joung, I. M. A., Mackenbach, J. P., Lamberts, S. W. J., & Bootsma, A. H. (2005). Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: A review. Diabetes Care. https://doi.org/10.2337/diacare.28.9.2280
Wierenga, M., & Wuethrich, K. (1995). Diabetes program attrition: Differences between two cultural groups. Health Values: The Journal of Health Behavior, Education & Promotion, 19(3), 12–21.
Plöckinger, U., Topuz, M., Langer, M., & Reuter, T. (2010). Problems of diabetes management in the immigrant population in Germany. Diabetes Research and Clinical Practice, 87(1), 77–86. https://doi.org/10.1016/j.diabres.2009.07.009
Oomen, J. S., Owen, L. J., & Suggs, L. S. (1999). Culture counts: Why current treatment models fail Hispanic women with type 2 diabetes. The Diabetes Educator, 25(2), 220–225. https://doi.org/10.1177/014572179902500207
Choudhury, S. M., Brophy, S., Fareedi, M. A., Zaman, B., Ahmed, P., & Williams, D. R. R. (2008). Intervention, recruitment and evaluation challenges in the Bangladeshi community: Experience from a peer lead educational course. BMC Medical Research Methodology. https://doi.org/10.1186/1471-2288-8-64
Szczepura, A. (2005). Access to health care for ethnic minority populations. Postgraduate Medical Journal. https://doi.org/10.1136/pgmj.2004.026237
Jervelund, S. S., Malik, S., Ahlmark, N., Villadsen, S. F., Nielsen, A., & Vitus, K. (2017). Morbidity, self-perceived health and mortality among non-western immigrants and their descendants in Denmark in a life phase perspective. Journal of Immigrant and Minority Health. https://doi.org/10.1007/s10903-016-0347-9
Ujcic-Voortman, J. K., Schram, M. T., Jacobs-Van Der Bruggen, M. A., Verhoeff, A. P., & Baan, C. A. (2009). Diabetes prevalence and risk factors among ethnic minorities. European Journal of Public Health, 19(5), 511–515. https://doi.org/10.1093/eurpub/ckp096
Meeks, K. A. C., Freitas-Da-Silva, D., Adeyemo, A., Beune, E. J. A. J., Modesti, P. A., Stronks, K., & Agyemang, C. (2016). Disparities in type 2 diabetes prevalence among ethnic minority groups resident in Europe: A systematic review and meta-analysis. Internal and Emergency Medicine. https://doi.org/10.1007/s11739-015-1302-9
Sivaprasad, S., Gupta, B., Gulliford, M. C., Dodhia, H., Mohamed, M., Nagi, D., & Evans, J. R. (2012). Ethnic variations in the prevalence of diabetic retinopathy in people with diabetes attending screening in the United Kingdom (DRIVE UK). PLoS ONE, 7(3), e32182. https://doi.org/10.1371/journal.pone.0032182
Andersen, G. S., Kamper-Jørgensen, Z., Carstensen, B., Norredam, M., Bygbjerg, I. C., & Jørgensen, M. E. (2016). Diabetes among migrants in Denmark: Incidence, mortality, and prevalence based on a longitudinal register study of the entire Danish population. Diabetes Research and Clinical Practice. https://doi.org/10.1016/j.diabres.2016.09.020
Oya, J., Jørgensen, M. E., Lund-Andersen, H., Carstensen, B., & Andersen, G. S. (2018). Incidence of diabetic eye disease among migrants: A cohort study of 100,000 adults with diabetes in Denmark. Diabetes Research and Clinical Practice. https://doi.org/10.1016/j.diabres.2018.08.021
Attridge, M., Creamer, J., Ramsden, M., Cannings-John, R., & Hawthorne, K. (2014). Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD006424.pub3
Resnicow, K., Baranowski, T., Ahluwalia, J. S., & Braithwaite, R. L. (1999). Cultural sensitivity in public health: Defined and demystified. Ethnicity and Disease, 9(1), 10–21.
Brown, T. & Wyatt, J. (2010). Design Thinking for Social Innovation By Tim Brown & Jocelyn Wyatt Stanford Social Innovation Review. Stanford Social Innovation Review
Craig, P., Dieppe, P., Macintyre, S., Mitchie, S., Nazareth, I., & Petticrew, M. (2008). Developing and evaluating complex interventions: The new medical research council guidance. BMJ. https://doi.org/10.1136/bmj.a1655
Seeleman, C., Suurmond, J., & Stronks, K. (2009). Cultural competence: A conceptual framework for teaching and learning. Medical Education, 43(3), 229–237. https://doi.org/10.1111/j.1365-2923.2008.03269.x
Greenberg, R. G., & Bertsch, H. B. (2014). A Flourishing Approach to Mental Health in Patients With Diabetes, 1:33–36
Clabby, J., & O’Connor, R. (2004). Teaching learners to use mirroring: Rapport lessons from neurolinguistic programming. Family Medicine, 36(8), 541–543.
Brown, T. (2008). Design thinking by Tim brown. Harvard Business Review, 86(6), 84.
Hempler, N. F., Christensen, N. I., & Laursen, D. H. (2018). Koncept for uddannelse målrettet etniske minoriteter med type 2 diabetes. Center for Diabetes, Københavns Kommune and Steno Diabetes Center Copenhagen, Region Hovedstaden
Chaves, F. F., Reis, I. A., Pagano, A. S., & de Torres, H. (2017). Translation, cross-cultural adaptation and validation of the diabetes empowerment scale—short form. Revista de saude publica. https://doi.org/10.1590/S1518-8787.2017051006336
Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. https://doi.org/10.1097/00005650-199603000-00003
Topp, C. W., Østergaard, S. D., Søndergaard, S., & Bech, P. (2015). The WHO-5 well-being index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167–176. https://doi.org/10.1159/000376585
McGuire, B. E., Morrison, T. G., Hermanns, N., Skovlund, S., Eldrup, E., Gagliardino, J., & Snoek, F. J. (2010). Short-form measures of diabetes-related emotional distress: The problem areas in diabetes scale (PAID)-5 and PAID-1. Diabetologia, 53(1), 66–69. https://doi.org/10.1007/s00125-009-1559-5
De Vries, J., Michielsen, H., Van Heck, G. L., & Drent, M. (2004). Measuring fatigue in sarcoidosis: The fatigue assessment scale (FAS). British Journal of Health Psychology, 9(3), 279–291. https://doi.org/10.1348/1359107041557048
Jensen, H. A. R., Ekholm, O., Davidsen, M., & Christensen, A. I. (2019). The Danish health and morbidity surveys: Study design and participant characteristics. BMC Medical Research Methodology. https://doi.org/10.1186/s12874-019-0733-9
Sundhedsstyrelsen. (2022). Danskernes sundhed—Den Nationale Sundhedsprofil 2021. Retrieved from https://www.sst.dk/da/Udgivelser/2022/Danskernes-sundhed
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950. https://doi.org/10.2337/diacare.23.7.943
Navodia, N., Wahoush, O., Tang, T., Yost, J., Ibrahim, S., & Sherifali, D. (2019). Culturally tailored self-management interventions for South Asians with type 2 diabetes: A systematic review. Canadian Journal of Diabetes. https://doi.org/10.1016/j.jcjd.2019.04.010
Goff, L. M., Rivas, C., Moore, A., Beckley-Hoelscher, N., Reid, F., & Harding, S. (2021). Healthy Eating and Active Lifestyles for Diabetes (HEAL-D), a culturally tailored self-management education and support program for type 2 diabetes in black-British adults: A randomized controlled feasibility trial. BMJ Open Diabetes Research and Care, 9(1), e002438. https://doi.org/10.1136/bmjdrc-2021-002438
Olesen, K., Folmann Hempler, N., Drejer, S., Valeur Baumgarten, S., & Stenov, V. (2020). Impact of patient-centred diabetes self-management education targeting people with type 2 diabetes: An integrative review. Diabetic Medicine. https://doi.org/10.1111/dme.14284
Franz, M. J., Boucher, J. L., Rutten-Ramos, S., & VanWormer, J. J. (2015). Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: A systematic review and meta-analysis of randomized clinical trials. Journal of the Academy of Nutrition and Dietetics, 115(9), 1447–1463. https://doi.org/10.1016/j.jand.2015.02.031
Han, H. R., McKenna, S., Nkimbeng, M., Wilson, P., Rives, S., Ajomagberin, O., & Sharps, P. (2019). A systematic review of community health center based interventions for people with diabetes. Journal of Community Health. https://doi.org/10.1007/s10900-019-00693-y
Critchley, J. A., Carey, I. M., Harris, T., DeWilde, S., & Cook, D. G. (2019). Variability in glycated hemoglobin and risk of poor outcomes among people with type 2 diabetes in a large primary care cohort study. Diabetes Care, 42(12), 2237–2246. https://doi.org/10.2337/dc19-0848
Forbes, A., Murrells, T., Mulnier, H., & Sinclair, A. J. (2018). Mean HbA 1c, HbA 1c variability, and mortality in people with diabetes aged 70 years and older: A retrospective cohort study. The Lancet Diabetes and Endocrinology, 6(6), 476–486. https://doi.org/10.1016/S2213-8587(18)30048-2
Acknowledgements
We would thank like to thank all the participants in the study, both patients and HCPs. We are very grateful to Ida Louisa Güntelberg who recruited participants and collected data and to Sara Rudbæk Larsen for contributing to the statistical analyses. The authors acknowledge Jennifer Green, Caduceus Strategies, for proofreading the manuscript.
Funding
The development of the education intervention was funded by Steno Diabetes Center Copenhagen. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NFH conceptualised the study. CG, IW, LBR and DHL contributed to the design and conduction of the study. SW, LB, NFH and SW curated the data. CG, SW, KO, IW and NFH undertook data analysis and interpreted the data. CF, MN and NFH drafted the first manuscript. All authors critically reviewed, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflict of interest in this work.
Ethical Approval
The study was approved by the Ethics Committee of the Capital Region, Denmark (H-18050166) and the Danish Data Protection Agency (Capital Region, Denmark (VD-2019-77).
Consent to Participate
The study was undertaken at the Centre for Diabetes, Copenhagen. Before any tests or examinations, participants signed written informed consent to participate.
Consent for Publication
We confirm that all patient/personal identifiers in the paper have been removed or disguised. Persons are not identifiable and cannot be identified through the details of the study. The written consent signed by participants included a separate statement regarding consent to use data for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Research Support: The development of the education intervention was funded by Steno Diabetes Center Copenhagen. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hempler, N.F., Fagt, C., Olesen, K. et al. Improving Health and Diabetes Self-Management in Immigrants with Type 2 Diabetes Through a Co-Created Diabetes Self-Management Education and Support Intervention. J Community Health 48, 141–151 (2023). https://doi.org/10.1007/s10900-022-01151-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-022-01151-y