Abstract
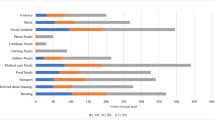
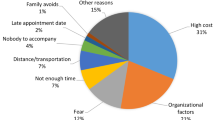
In 2018, the University of Maryland Medical Center and the Baltimore City Fire Department implemented a community paramedicine program to help medically or socially complex patients transition from hospital to home and avoid hospital utilization. This study describes how patients’ social determinants of health (SDoH) needs were identified, and measures the association between needs and hospital utilization. SDoH needs were categorized into ten domains. Multinomial logistic regression was used to measure association between identified SDoH domains and predicted risk of readmission. Poisson regression was used to measure association between SDoH domains and actual 30-day hospital utilization. The most frequently identified SDoH needs were in the Coordination of Healthcare (37.7%), Durable Medical Equipment (18.8%), and Medication (16.3%) domains. Compared with low-risk patients, patients with an intermediate risk of readmission were more likely to have needs within the Coordination of Healthcare (RRR [95% CI] 1.12 [1.01, 1.24], p = 0.032) and Durable Medical Equipment (RRR = 1.13 [1.00, 1.27], p = 0.046) domains. Patients with the highest risk for readmission were more likely to have needs in the Utilities domain (RRR = 1.76 [0.97, 3.19], p = 0.063). Miscellaneous domain needs, such as requiring a social security card, were associated with increased 30-day hospital utilization (IRR = 1.23 [0.96, 1.57], p = 0.095). SDoH needs within the Coordination of Healthcare, Durable Medical Equipment, and Utilities domains were associated with higher predicted 30-day readmission, while identification documentation and social services needs were associated with actual readmission. These results suggest where to allocate resources to effectively diminish hospital utilization.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available upon reasonable request.
Code Availability
Not applicable.
References
Hospital Readmissions Reduction Program (HRRP) | CMS. (n.d.). Retrieved March 7, 2021, from https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program
Gupta, A., Allen, L. A., Bhatt, D. L., Cox, M., DeVore, A. D., Heidenreich, P. A., & Fonarow, G. C. (2018). Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiology, 3(1), 44. https://doi.org/10.1001/jamacardio.2017.4265
Axelson, D. J., Stull, M. J., & Coates, W. C. (2018). Social determinants of health: A missing link in emergency medicine training. AEM Education and Training, 2(1), 66–68. https://doi.org/10.1002/aet2.10056
Balakrishnan, M. P., Herndon, J. B., Zhang, J., Payton, T., Shuster, J., & Carden, D. L. (2017). The association of health literacy with preventable emergency department visits: A cross-sectional study. Academic Emergency Medicine, 24(9), 1042–1050. https://doi.org/10.1111/acem.13244
Chambers, C., Chiu, S., Katic, M., Kiss, A., Redelmeier, D. A., Levinson, W., & Hwang, S. W. (2013). High utilizers of emergency health services in a population-based cohort of homeless adults. American Journal of Public Health, 103(S2), S302–S310. https://doi.org/10.2105/AJPH.2013.301397
Davis, C. I., Montgomery, A. E., Dichter, M. E., Taylor, L. D., & Blosnich, J. R. (2020). Social determinants and emergency department utilization: Findings from the Veterans Health Administration. The American Journal of Emergency Medicine, 38(9), 1904–1909. https://doi.org/10.1016/j.ajem.2020.05.078
Friedman, C. (2021). Social determinants of health, emergency department utilization, and people with intellectual and developmental disabilities. Disability and Health Journal, 14(1), 100964. https://doi.org/10.1016/j.dhjo.2020.100964
Kangovi, S., & Grande, D. (2011). Hospital readmissions—Not just a measure of quality. Journal of the American Medical Association, 306(16), 1796–1797. https://doi.org/10.1001/jama.2011.1562
Nagasako, E. M., Reidhead, M., Waterman, B., & Dunagan, C. (2014). Adding socioeconomic data to hospital readmissions calculations may produce more useful results. Health Affairs, 33(5), 786–791. https://doi.org/10.1377/hlthaff.2013.1148
Kind, A. J. H., Jencks, S., Brock, J., Yu, M., Bartels, C., Ehlenbach, W., & Smith, M. (2014). Neighborhood socioeconomic disadvantage and 30-day rehospitalization. Annals of Internal Medicine, 161(11), 765–774. https://doi.org/10.7326/M13-2946
Gregg, A., Tutek, J., Leatherwood, M. D., Crawford, W., Friend, R., Crowther, M., & McKinney, R. (2019). Systematic review of community paramedicine and EMS mobile integrated health care interventions in the United States. Population Health Management, 22(3), 213–222. https://doi.org/10.1089/pop.2018.0114
Seidl, K. L., Gingold, D. B., Stryckman, B., Landi, C., Sokan, O., Fletcher, M., & Marcozzi, D. (2021). Development of a logic model to guide implementation and evaluation of a mobile integrated health transitional care program. Population Health Management, 24(2), 275–281. https://doi.org/10.1089/pop.2020.0038
Gingold, D. B., Liang, Y., Stryckman, B., & Marcozzi, D. (2021). The effect of a mobile integrated health program on health care cost and utilization. Health Services Research, 56(6), 1146–1155. https://doi.org/10.1111/1475-6773.13773
Donzé, J. D., Williams, M. V., Robinson, E. J., Zimlichman, E., Aujesky, D., Vasilevskis, E. E., & Schnipper, J. L. (2016). International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Internal Medicine, 176(4), 496. https://doi.org/10.1001/jamainternmed.2015.8462
Hoyer, E. H., Needham, D. M., Atanelov, L., Knox, B., Friedman, M., & Brotman, D. J. (2014). Association of impaired functional status at hospital discharge and subsequent rehospitalization. Journal of Hospital Medicine, 9(5), 277–282. https://doi.org/10.1002/jhm.2152
Acknowledgements
We acknowledge the support of the Baltimore City Fire Department (BCFD), the Maryland Health Services Cost Review Commission (MHSCRC), the University of Maryland, Baltimore, Institute for Clinical & Translational Research (ICTR), and the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) grant number 1UL1TR003098. We also thank Eileen O’Brien for her editorial assistance.
Funding
We received funding internally from the University of Maryland, Baltimore, which came from the Institute for Clinical & Translational Research Accelerated Translational Incubator Pilot grant program (ID number 70), which in turn is funded by the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA), grant number UL1TR003098. In addition, we acknowledge the support of the Maryland Health Services Cost Review Commission (HSCRC), which funded the MIH-CP program. This was not an award; it was a reimbursement rate adjustment from the HSCRC, then the Maryland State Hospital Funding Commission, to the University of Maryland Medical Center for piloting a two-year MIH-CP program. We declare no other financial relationships with any organizations that might have an interest in the submitted work and no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Contributions
SN: conceptualization (support); data curation (support); writing—original draft (lead); writing—review and editing (lead). BS: conceptualization (support); data curation (lead); formal analysis (support); project administration (lead); software (lead); writing—review and editing (support). YL: formal analysis (lead); methodology (lead); writing--review and editing (support). KS: data curation (lead); software (support); writing--review and editing (support). EH: investigation (equal). CL: data curation (support); software (support). JT: investigation (equal). DM: funding acquisition (equal). DBG: conceptualization (lead); funding acquisition (equal); project administration (support); supervision (lead); writing—review and editing (support).
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial conflicts of interest to disclose.
Ethical Approval
This study was exempt by University of Maryland, Baltimore IRB HP-00086403.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table 6.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Naimi, S., Stryckman, B., Liang, Y. et al. Evaluating Social Determinants of Health in a Mobile Integrated Healthcare-Community Paramedicine Program. J Community Health 48, 79–88 (2023). https://doi.org/10.1007/s10900-022-01148-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-022-01148-7