Abstract
Extreme heat is the leading cause of w eather-related mortality in the U.S. Extreme heat also affects human health through heat stress and can exacerbate underlying medical conditions that lead to increased morbidity and mortality. In this study, data on emergency department (ED) visits for heat-related illness (HRI) and other selected diseases were analyzed during three heat events across North Carolina from 2007 to 2011. These heat events were identified based on the issuance and verification of heat products from local National Weather Service forecast offices (i.e. Heat Advisory, Heat Watch, and Excessive Heat Warning). The observed number of ED visits during these events were compared to the expected number of ED visits during several control periods to determine excess morbidity resulting from extreme heat. All recorded diagnoses were analyzed for each ED visit, thereby providing insight into the specific pathophysiological mechanisms and underlying health conditions associated with exposure to extreme heat. The most common form of HRI was heat exhaustion, while the percentage of visits with heat stroke was relatively low (<10 %). The elderly (>65 years of age) were at greatest risk for HRI during the early summer heat event (8.9 visits per 100,000), while young and middle age adults (18–44 years of age) were at greatest risk during the mid-summer event (6.3 visits per 100,000). Many of these visits were likely due to work-related exposure. The most vulnerable demographic during the late summer heat event was adolescents (15–17 years of age), which may relate to the timing of organized sports. This demographic also exhibited the highest visit rate for HRI among all three heat events (10.5 visits per 100,000). Significant increases (p < 0.05) in visits with cardiovascular and cerebrovascular diseases were noted during the three heat events (3–8 %). The greatest increases were found in visits with hypotension during the late summer event (23 %) and sequelae during the early summer event (30 %), while decreases were noted for visits with hemorrhagic stroke during the middle and late summer events (13–24 %) and for visits with aneurysm during the early summer event (15 %). Significant increases were also noted in visits with respiratory diseases (5–7 %). The greatest increases in this category were found in visits with pneumonia and influenza (16 %), bronchitis and emphysema (12 %), and COPD (14 %) during the early summer event. Significant increases in visits with nervous system disorders were also found during the early summer event (16 %), while increases in visits with diabetes were noted during the mid-summer event (10 %).



Similar content being viewed by others
References
National Oceanic and Atmospheric Administration. (2015). Natural hazard statistics. National Weather Service, Office of Climate, Water, and Weather Services. http://www.nws.noaa.gov/om/hazstats.html.
Centers for Disease Control and Prevention. (2006). Heat-related deaths—United States, 1999–2003. Morbidity and Mortality Weekly Report, 55(29), 796–798.
Harvard Medical School. (2005). Climate change futures: Health, ecological and economic dimensions. Cambridge, MA: Center for Health and the Global Environment, Harvard Medical School.
Hajat, S., O’Connor, M., & Kosatsky, T. (2010). Health effects of hot weather: From awareness of risk factors to effective health protection. Lancet, 375, 856–863.
Basu, R. (2009). High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environmental Health, 8(1), 40. doi:10.1186/1476-069X-8-40.
Sanchez, C. A., Thomas, K. E., Malilay, J., & Annest, J. L. (2010). Nonfatal natural and environmental injuries treated in emergency departments, United States, 2001–2004. Family & Community Health, 33(1), 3–10.
Noe, R. S., Jin, J. O., & Wolkin, A. F. (2012). Exposure to natural cold and heat: Hypothermia and hyperthermia Medicare claims, United States, 2004–2005. American Journal of Public Health, 102, 11–18.
Howe, A. S., & Boden, B. P. (2007). Heat-related illness in athletes. American Journal of Sports Medicine, 35(8), 1384–1395.
Naughton, M. P., Henderson, A., Mirabelli, M. C., Kaiser, R., Wilhelm, J. L., Kieszak, S. M., et al. (2002). Heat-related mortality during the 1999 heat wave in Chicago. American Journal of Preventative Medicine, 22(4), 221–227.
Nelson, N. G., Collins, C. L., Comstock, R. D., & McKenzie, L. B. (2011). Exertional heat-related injuries treated in emergency departments in the U.S., 1997–2006. American Journal of Preventive Medicine, 40(1), 54–60.
Sheridan, S. C., & Kalkstein, L. S. (2004). Progress in heat watch-warning system technology. Bulletin of the American Meteorological Society, 85, 1931–1941.
Ebi, K. L., Teisberg, T. J., Kalkstein, L. S., Robinson, L., & Weiher, R. F. (2004). Heat watch/warning systems save lives: Estimate costs and benefits for Philadelphia 1995–98. Bulletin of the American Meteorological Society, 85, 1067–1073.
Kalkstein, L. S., Sheridan, S. C., & Kalkstein, A. J. (2009). Heat/health warning systems: Development, implementation, and intervention activities. In K. L. Ebi, I. Burton, & G. McGregor (Eds.), Biometeorology for adaptation to climate variability and change (pp. 33–48). Heidelberg: Springer.
Hajat, S., Sheridan, S. C., Allen, M. J., Pascal, M., Laaidi, K., Yagouti, A., et al. (2010). Heat-health warning systems: A comparison of the predictive capacity of different approaches to identifying dangerously hot days. American Journal of Public Health, 100(6), 1137–1144.
Smith, T. T., Zaitchik, B. F., & Gohlke, J. M. (2013). Heat waves in the United States: Definitions, patterns and trends. Climatic Change, 118(3–4), 811–825.
Jones, B., O’Neill, B. C., McDaniel, L., McGinnis, S., Mearns, L. O., & Tebaldi, C. (2015). Future population exposure to US heat extremes. Nature Climate Change,. doi:10.1038/nclimate2631.
Rhea, S., Ising, A., Fleischauer, A. T., Deyneka, L., Vaughan-Batten, H., & Waller, A. (2012). Using near real-time morbidity data to identify heat-related illness prevention strategies in North Carolina. Journal of Community Health, 37(2), 495–500.
Lippmann, S., Fuhrmann, C. M., Waller, A., & Richardson, D. (2013). Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ Res, 124, 35–42.
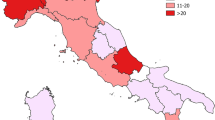
Kovach, M. M., Konrad, C. E., & Fuhrmann, C. M. (2015). Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Applied Geography, 60, 175–183.
Semenza, J. C., McCullough, J. E., Flanders, W. D., McGeehin, M. A., & Lumpkin, J. R. (1999). Excess hospital admissions during the July 1995 heat wave in Chicago. American Journal of Preventative Medicine, 16(4), 269–277.
Knowlton, K., Rotkin-Ellman, M., King, G., Margolis, H. G., Smith, D., Solomon, G., et al. (2009). The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environmental Health Perspectives, 117, 61–67.
Green, R. S., Basu, R., Malig, B., Broadwin, R., Kim, J. J., & Ostro, B. (2010). The effect of temperature on hospital admissions in nine California counties. International Journal of Public Health, 55, 113–121.
Ostro, B., Rauch, S., Green, R., Malig, B., & Basu, R. (2010). The effects of temperature and use of air conditioning on hospitalizations. American Journal of Epidemiology, 172(9), 1053–1061.
Nitschke, M., Tucker, G. R., Hansen, A. L., Williams, S., Zhang, Y., & Bi, P. (2011). Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: A case-series analysis. Environmental Health, 10, 42.
Basu, R., Pearson, D., Malig, B., Broadwin, R., & Green, R. (2012). The effect of high ambient temperature on emergency room visits. Epidemiology, 23(6), 813–820.
North Carolina Department of Public Health. (2012). Strategic plan for addressing health impacts of climate change in North Carolina. http://epi.publichealth.nc.gov/oee/climate/ClimateReadyStrategicPlan.pdf.
National Oceanic and Atmospheric Administration. (2015). National Weather Service Raleigh, products and services guide. http://www.erh.noaa.gov/rah/criteria.
Robinson, P. J. (2001). On the definition of a heat wave. Journal of Applied Meteorology, 40, 762–775.
Saha, M. V., Davis, R. E., & Hondula, D. M. (2014). Mortality displacement as a function of heat strength in 7 US cities. American Journal of Epidemiology, 179(4), 467–474.
Hess, J. J., Saha, S., & Luber, G. (2014). Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environmental Health Perspectives, 122, 1209–1215.
Xu, Z., Sheffield, P. E., Su, H., Wang, X., Bi, Y., & Tong, S. (2014). The impact of heat waves on children’s health: A systematic review. International Journal of Biometeorology, 58(2), 239–247.
Wheeler, K., Lane, K., Walters, S., & Matte, T. (2013). Heat-related deaths—New York City, 2000–2011. Morbidity and Mortality Weekly Report, 62(31), 617–621.
Gubernot, D. M., Anderson, G. B., & Hunting, K. L. (2014). The epidemiology of occupational heat exposure in the United States: A review of the literature and assessment of research needs in a changing climate. International Journal of Biometeorology, 58, 1779–1788.
Montz, B. E., Allen, T. R., & Monitz, G. I. (2011). Systemic trends in disaster vulnerability: Migrant and seasonal farmworkers in North Carolina. Risk, Hazards and Crisis in Public Policy, 2(1), 1–17.
Mirabelli, M. C., & Richardson, D. (2005). Heat-related fatalities in North Carolina. American Journal of Public Health, 95(4), 635–637.
Mirabelli, M. C., Quandt, S. A., Crain, R., Grzywacz, J. G., Robinson, E. N., Vallejos, Q. M., & Arcury, T. A. (2010). Symptoms of heat illness among Latino farm workers in North Carolina. American Journal of Preventative Medicine, 39(5), 468–471.
Fleischer, N. L., Tiesman, H. M., Sumitani, J., Mize, T., Amarnath, K. K., Bayakly, A. R., et al. (2013). Public health impact of heat-related illness among migrant farmworkers. American Journal of Preventative Medicine, 44(3), 199–206.
Quandt, S. A., Wiggins, M. F., Chen, H., Bischoff, W. E., & Arcury, T. A. (2013). Heat index in migrant farmworker housing: Implications for rest and recovery from work-related heat stress. American Journal of Public Health, 103(8), e24–e26.
Grundstein, A., Ramseyer, C., Zhao, F., Peses, J., Akers, P., Qureshi, A., et al. (2012). A retrospective analysis of American football hyperthermia deaths in the United States. International Journal of Biometeorology, 56, 11–20.
Kerr, Z. Y., Casa, M. J., Marshall, S. W., & Comstock, R. D. (2013). Epidemiology of exertional heat illness among U.S. high school athletes. American Journal of Preventive Medicine, 44(1), 8–14.
Casa, D. J., & Csillan, D. (2009). Preseason heat-acclimatization guidelines for secondary school athletics. Journal of Athletic Training, 44(3), 332–333.
Yip, F. Y., Flanders, W. D., Wolkin, A., Engelthaler, D., Humble, W., Neri, A., et al. (2008). The impact of excess heat events in Maricopa County, Arizona: 2000–2005. International Journal of Biometeorology, 52, 765–772.
Shendell, D. G., Alexander, M. S., Lorentzson, L., & McCarty, F. A. (2010). Knowledge and awareness of heat-related morbidity among adult recreational endurance athletes. International Journal of Biometeorology, 54, 441–448.
Guirguis, K., Gershunov, A., Tardy, A., & Basu, R. (2014). The impact of recent heat waves on human health in California. Journal of Applied Meteorology and Climatology, 53, 3–19.
Harlan, S. L., Chowell, G., Yang, S., Petitti, D. B., Morales Butler, E. J., Ruddell, B. L., & Ruddell, D. M. (2014). Heat-related deaths in hot cities: Estimates of human tolerance to high temperature thresholds. International Journal of Environmental Research and Public Health, 11(3), 3304–3326.
Kim, Y. M., Kim, S., Cheong, H. K., Ahn, B., & Choi, K. (2012). Effect of heat wave on body temperature and blood pressure in the poor and elderly. Environmental Health and Toxicology, 27, e2012013.
Muresanu, D. F., & Sharma, H. S. (2007). Chronic hypertension aggravates heat stress induced cognitive dysfunction and brain pathology: An experimental study in the rat, using growth hormone therapy and possible neuroprotection. Annals of the New York Academy of Sciences, 1122, 1–22.
Reid, C. E., Snowden, J. M., Kontgis, C., & Tager, I. B. (2012). The role of ambient ozone in epidemiologic studies of heat-related mortality. Environmental Health Perspectives, 120, 1627–1630.
Kent, S. T., McClure, L. A., Zaitchik, B. F., Smith, T. T., & Gohlke, J. M. (2014). Heat waves and health outcomes in Alabama (USA): The importance of heat wave definition. Environmental Health Perspectives, 122, 151–158.
Acknowledgments
We thank Nick Petro from the Raleigh, NC National Weather Service office for providing the archived heat products. This project was developed with support from the Regional Climate Center and Regional Integrated Sciences and Assessments Programs, through the National Oceanic and Atmospheric Administration, as well as the North Carolina Division of Public Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Disclaimer: NC DETECT is a statewide public health syndromic surveillance system, funded by the NC Division of Public Health (NC DPH) Federal Public Health Emergency Preparedness Grant and managed through collaboration between NC DPH and the UNC-Chapel Hill Department of Emergency Medicine’s Carolina Center for Health Informatics. The NC DETECT Data Oversight Committee does not take responsibility for the scientific validity or accuracy of the methods, statistical analyses, results, or conclusions presented.
Appendix
Rights and permissions
About this article
Cite this article
Fuhrmann, C.M., Sugg, M.M., Konrad, C.E. et al. Impact of Extreme Heat Events on Emergency Department Visits in North Carolina (2007–2011). J Community Health 41, 146–156 (2016). https://doi.org/10.1007/s10900-015-0080-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-015-0080-7