Abstract
This study aimed to explore relationships between being an ‘affected other’ (AO) and an individual’s own gambling, health risk behaviours, financial problems, poor general health, and low mental wellbeing. A cross-sectional survey using representative and supplementary convenience samples was undertaken with 1234 residents of a British Island aged 16 + years. Being an AO was measured as having a partner or relative who has been gambling regularly in the past 12 months. PGSI was used to assess gambling severity. Health risk behaviours included: poor diet, low physical activity, daily smoking, and binge drinking. Other measures included experiencing financial problems, poor general health, and low mental wellbeing. Analyses were performed using χ2 and binary logistic regressions. 11.0% of participants were AOs. AOs were more likely to gamble at at-risk/problem-gambling levels and experience financial problems compared to those who were not affected others. The significant relationship between being an AO and low mental wellbeing was mediated by experiencing financial problems. The relationship between being an AO and engaging in two or more health risk behaviours was no longer significant after controlling for sociodemographics and an individual’s own gambling. The relationship between being an AO and poor general health was no longer significant after controlling for sociodemographics, health risk behaviours and an individual’s own gambling. AOs experienced risks to health and wellbeing, with findings not limited to AOs specifically with a relationship to an individual with problem-gambling. Therefore, support for AOs should be more widely available, aiming to address AOs’ needs holistically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, gambling is increasingly recognised as a public health concern with different countries putting different levels of regulations in place to prevent and respond to gambling harms. Work has also taken place in different countries to understand the proportion of the population experiencing gambling harms. In 2022/23, the prevalence of problem gambling in the United Kingdom’s (UK) adult population was estimated to be 0.3%, with a further 3.0% at low or moderate risk (The Gambling Commission, 2023). Other data has found such rates to be higher in the UK, with Gunstone et al. (2021) finding the prevalence of problem gambling to be 2.8%, with a further 9.9% at low or moderate risk. Differences between prevalence rates across studies are heavily impacted by the methods and measures used. The study by Gunstone et al. (2021) is considered more reliable due to the larger sample size (n = 18,038), and the full Problem Gambling Severity Index (PGSI) tool being utilised, compared to The Gambling Commission (2023) data which had a smaller sample size (n = 4002) and used the short form PGSI (Newall et al., 2022; Sturgis, 2020; Sulkunen et al., 2019; Wardle, 2015). Nonetheless, while such figures may be relatively small percentages, this would amount to a large problem across the population, with over 1.4 million people considered to have problem gambling in the UK (Gunstone et al., 2021). While harms at the problem gambling level are significant, the burden of harm is not solely isolated to this group. Research has demonstrated that the majority of gambling harms fall on those below the threshold for problem gambling, indicating that gambling is a public health issue impacting a greater number than those with problem gambling alone (Browne, 2020; Browne et al., 2017; Canale et al., 2016).
Globally, research has demonstrated a number of gambling-related harms spanning individual, relationship, community and societal levels (Langham et al., 2015; Orford, 2020). Harms to the individual have been demonstrated, ranging from lower-level harms such as lost time and smaller financial problems to serious harms with long-term implications including debt, crime, homelessness, and suicide (Langham et al., 2015; Orford, 2020; Wardle et al., 2020). Furthermore, a representative survey study from a British Island (n = 2303) showed that compared to those with non-problem gambling, those gambling at low- and moderate-risk and problem gambling levels were more likely to have a poor diet, smoke tobacco, and have harmful alcohol use, as well as having increased likelihood of experiencing poorer general health and low mental wellbeing (Butler et al. 2019).
A less well-researched area of gambling-related harm is the impacts that gambling has on individuals who have a significant relationship with a person with problem gambling (e.g., children, partners etc.) termed as ‘affected others’ (AOs). Research has tried to estimate the prevalence of AOs in the general population and has shown that problem gambling impacts a greater proportion of the population than the gambling individual alone (Tulloch et al., 2021). In the UK, Gunstone et al. (2021) found that 6.5% of the UK population were individuals who ‘knew someone with a gambling problem (either currently, or in the past) and feel that they have personally experienced negative effects from this person’s gambling behaviour’. Further, research from Australia has estimated that for each individual with problem gambling, their gambling affects between four and six other individuals, while those with moderate-risk and low-risk gambling affect one and three others respectively (Goodwin et al., 2017).
Research has shown that there is a large degree of cross-over in the experiences of gambling-related harms by the gambling individual and by AOs (Li et al., 2017). Harms to AOs impact in numerous ways, including financial problems, reduced emotional and psychological wellbeing, harm to physical health, and significant breakdowns in the relationship with the individual who gambles, characterised by a lack of trust and interpersonal conflicts, which can include violence (Banks et al., 2018; Castren et al., 2021; Dowling et al., 2021; Gunstone et al., 2021; Holdsworth et al., 2013; Langham et al., 2015; Lind et al., 2022; Riley et al., 2018; Subramaniam et al., 2017; Tulloch et al., 2021; Velleman et al., 2015). Research has also illustrated that AOs were more likely to engage in health risk behaviours including harmful alcohol use, daily tobacco smoking, over-eating, as well as risky gambling behaviours themselves (Dowling et al., 2021; Lind et al., 2022; Riley et al., 2018).
When examining harms to AOs there has been limited use of validated measures or scales across factors such as mental wellbeing (Dowling et al., 2021; Tulloch et al., 2021). Studies examining gambling-related harms to AOs have utilised different measures for defining AOs, with some studies covering family members only, others including friends and colleagues. Some studies have included only those who are currently AOs, while other studies include those who have ever been an AO. However, one factor most studies of AOs have in common is that they tend to include AOs on the basis that they have a relationship with somebody specifically with problem gambling. While there is a validated measure for identifying individuals who may have problem gambling, or experience sub-problem gambling level harms, no such measure exists for identifying AOs. Therefore, a range of experiences of gambling-related harms may be missed in AOs with a relationship to somebody who gambles at sub-problem gambling levels (Dowling et al., 2021; Tulloch et al., 2021).
Most research on AOs has not examined harms occurring at the sub-problem gambling level. Further, only a small number of studies have examined harms to AOs in general population samples. Across both of these areas the evidence base is particularly scarce from a British perspective. The current study aims to address this gap, in a general population sample from a British Island, by utilising a measure for identifying AOs which did not depend solely on the AO having a relationship with someone who gambles at the problem gambling level. Specifically, the current study aims to explore relationships between an individual’s own gambling behaviours, health risk behaviours, financial problems, poor general health, low mental wellbeing, and having a relative or partner who has been gambling regularly in the past 12 months.
Methods
The sample included individuals residing on a British Island with a population of 53,627 residents aged 16 + years (86.1% of all residents). 24.7% of all residents were aged 16–34 years, 28.0% were aged 35–54, and 33.4% of residents were aged 55 + . There was a relatively even split of males (49.2%) and females (50.8%) aged 16 + living on the British Island.
There are a number of online and offline gambling environments and opportunities available on the British Island, residents can participate in gambling activities including lotteries, raffles, fixed-odds betting terminals, online gambling (such as for sports gambling and online bingo), and scratch cards, there are also several betting shops and bookmakers available.
Study Design and Participants
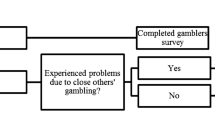
A cross-sectional survey of residents aged 16 + was undertaken between October and November 2019. The survey was conducted in two phases. Phase 1 was an invited representative sample of the British Island’s population, with 7000 addresses selected. A random sample was then selected, stratified by parish and social or non-social housing (due to a low expected response rate amongst individuals in social housing). Following phase 1, phase 2 was implemented, consisting of a convenience sample, making the survey open-access to all members of the public, promoted through media channels.
The total sample size was n = 1234, equating to 2.4% of the population (aged 16 + years).
Measures
Affected Others
A self-report item was included asking participants: ‘In the last 12 months, has your partner or one of your relatives been gambling regularly?’ Response options included: Yes; No; or, Don’t know. AOs were coded as those who responded yes; zero participants responded don’t know. Those who answered ‘Yes’ to this question were also asked whether they experienced several harms directly as a result of their partner or relative’s gambling.
Gambling Behaviours and Problem Gambling
Problem and at-risk gambling was measured using the PGSI. The PGSI is a self-report, validated instrument for use in general populations (Ferris & Wynne, 2001; Holtgraves, 2008). The PGSI tool consists of nine questions, each measured on a four-point scale (0 = never, 1 = sometimes, 2 = most of the time, 3 = almost always). Scores for each question are summed, giving a total overall score ranging from 0 to 27, with higher scores indicating a greater severity of gambling risk. PGSI score can be divided into the following categories: 0 = non-problem gambling; 1–2 = low-risk gambling; 3–7 = moderate-risk gambling; 8 + = problem gambling. Due to small sample sizes, the low- and moderate-risk and problem gambling categories were combined to create a dichotomous variable of non-problem gambling and at-risk/problem gambling. Other gambling behaviours such as the frequency of participation in different gambling activities, and whether individuals gambled online were also measured.
Health Risk Behaviours
Four measures of health risk behaviours were included for analyses: poor diet, low physical activity, daily smoking, and binge drinking. Poor diet was defined as eating less than 2 portions of fruit and vegetables (excluding potatoes) per day. Low physical activity was defined as taking part in less than 150 min of physical activity that was ‘enough to raise your breathing rate’ in the previous week. Daily smoking was defined as the current smoking of tobacco on a daily basis. Consumption of alcohol was measured using AUDIT-C questions. AUDIT-C is a commonly used validated screening tool for identifying harmful alcohol use (Bush et al., 1998). Binge drinking was defined as having 6 or more standard drinks (one standard drink in the UK is equal to one UK unit of alcohol (10mls of pure alcohol)) on one occasion, at least once per week. Engaging in two or more health risk behaviours was defined as engaging in two or more of having a poor diet, low physical activity, daily smoking, and binge drinking.
Financial Problems
Experiencing financial problems was defined as those who answered Yes to the question ‘In the past 12 months, have you been behind (e.g., paid late, had to borrow money, or have gone without) with payments for expenses such as rent, utilities, mortgage repayments, taxes etc.?’
Poor General Health
General health was measured using a self-reported question on ‘health today’, this question asked individuals to rate their health on a visual scale from 0–10 (0 indicating ‘the worst health you can imagine’ and 10 indicating ‘the best health you can imagine’). Poor general health was defined as scores of 5 or less.
Low Mental Wellbeing
Mental wellbeing was measured using the Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS; Stewart-Brown et al., 2009). This is a validated scale including seven items about an individual’s current mental wellbeing, scored on a 5-point scale (1 = none of the time; 2 = rarely; 3 = some of the time; 4 = often; 5 = all of the time). Total scores on the SWEMWBS range from 7 to 35, with higher scores indicating higher levels of mental wellbeing. Raw scores are then converted to metric scores using a standard conversion table (Stewart-Brown et al., 2009). Scores were dichotomised to indicate low mental wellbeing as more than one standard deviation (4.397) below the mean (24.378), thus low mental wellbeing was operationalised as scores of < 19.981.
Sociodemographic Factors
Measured sociodemographic factors included: sex, age (16–34; 35–54; 55 + years), and income level (< £20,000; £20,000–£79,999; £80,000 +).
Analyses
Analyses were undertaken in SPSS (v.28). Bivariate analyses using χ2 tests were used to illustrate significant associations between AO status and sociodemographics, an individual’s own gambling behaviours, health risk behaviours, financial problems, poor general health, and low mental wellbeing. Binary logistic regression (enter method) models were used to estimate the size and significance of associations between AO status and each measure of interest, after controlling for sociodemographics. In regressions for health risk behaviours and financial problems, the individual’s own gambling behaviours were additionally controlled for within the same model. In the regressions for both poor general health and low mental wellbeing, the individual’s own gambling behaviours and all health risk behaviours were additionally controlled for in a separate model. In the regressions for low mental wellbeing experiencing financial problems was additionally controlled for in another separate model. Financial problems were not included in models examining the relationship between AO status and poor general health, as this relationship was no longer significant once health risk behaviours and the individual’s own gambling were controlled for.
Results
Affected Others’ Sociodemographics
Just over one in ten (11.0%; n = 126) study participants reported that they had a partner or relative who had been gambling regularly in the past 12 months (i.e. AO). 33.6% (n = 41) of AOs indicated that it was their spouse or partner who was gambling regularly, 13.9% (n = 17) their sibling, 9.0% (n = 11) their parent, 36.9% (n = 45) another relative, 6.6% (n = 8) had multiple relatives who were gambling regularly in the past year. Table 1 shows the sociodemographic characteristics of AOs. In bivariate analyses, there were significant associations between AO status and age (16–34, 17.6%; 35–54, 11.9%; 55 + , 7.9%; p < 0.001). There were no significant relationships between AO status and sex or income level.
Affected Others’ Experience of Gambling-Related Harms
AOs reported experiencing several harms as a direct result of their relative or partner’s gambling. Overall, 19.5% of AOs experienced one or more harms directly related to their relative or partner’s gambling. 12.9% reported that they had a serious argument not including violence, or had been emotionally hurt or neglected by the individual who had been gambling. 8.9% of AOs reported that they missed out on money that would have improved their quality of life, as it was spent on gambling activities. 8.9% also reported being let down by the gambling individual who failed to do something they were counting on them to do because of their gambling. 5.6% of AOs had something broken, damaged, or stolen by the gambling individual. 4.8% of AOs had to stop seeing or being in contact with the other individual due to their gambling. 2.4% felt physically threatened, physically hurt due to assault or violence, or concerned that the individual who had been gambling regularly may cause harm to their children. There were no significant associations between experiencing these gambling-related harms and sociodemographics.
Affected Others’ Gambling Behaviours
AOs gambled on a range of activities within the past 12 months (lotteries 81.0%; scratch cards 59.5%; horse and dog race betting 28.6%; sports betting 22.4%; private betting 21.1%; bingo 13.5%; fruit or slot machines 7.1%; online fruit machines/instant win games 5.6%; roulette, cards or dice 4.0%; poker 2.4%). AOs were significantly more likely to have gambled on any gambling activity and to have gambled online in the past 12 months than NAOs (Table 2). There was also a significant association between AO status and gambling frequency, with a higher proportion of AOs gambling at least once a week compared to NAOs (Table 2).
There was a significant association between AO status and at-risk/problem gambling. After controlling for sex, age, and income level, AOs were 2.2 times (AOR = 2.17 (1.08–4.38); p < 0.05) more likely to gamble at at-risk/problem gambling levels themselves, compared to NAOs.
Affected Others’ Health Risk Behaviours
Table 3 describes the relationships between being an AO and health risk behaviours. In bivariate analyses, the prevalence of all health risk behaviours was higher amongst AOs when compared to NAOs. Further, associations with poor diet and low physical activity were significant, however, associations with binge drinking, and daily smoking were not. There was also a significant relationship between AO status and engaging in two or more health risk behaviours. After controlling for sex, age, income level, and an individual’s at-risk/problem gambling the associations between AO status and poor diet, low physical activity, and engaging in two or more health risk behaviours were no longer significant (Table 4; Supplementary Tables 1, 2 and 5).
Affected Others’ Financial Problems
In bivariate analyses, the prevalence of experiencing financial problems was higher amongst AOs when compared to NAOs (Table 3). The relationship between experiencing financial problems and AO status was significant. After controlling for sex, age, income level, and an individual’s at-risk/problem gambling AOs were 2.1 times (AOR = 2.12 (1.10–4.07); p < 0.05) more likely to experience financial problems than NAOs (Table 4; Supplementary Table 6).
Affected Others’ General Health and Mental Wellbeing
In bivariate analysis, the prevalence of both poor general health and low mental wellbeing was significantly higher in AOs, compared to NAOs (Table 3). In multivariate analyses, after controlling for sex, age, and income level, AOs were 1.8 times more likely (AOR = 1.82 (1.06–3.13); p < 0.05) to have poor general health, and 1.7 times more likely (AOR = 1.70 (1.04–2.77); p < 0.05) to have low mental wellbeing, compared to NAOs (Supplementary Tables 7 and 8). After additionally controlling for an individual’s own at-risk/problem gambling, and all health risk behaviours, AOs remained 1.7 times more likely to have low mental wellbeing than NAOs, however, the relationship between AO status and poor general health was no longer significant (Table 4; Supplementary Tables 7 and 8). After additionally controlling for financial problems, the relationship between AO status and low mental wellbeing was no longer significant (AOR = 1.65; CIs = 0.95–2.87; Supplementary Table 8).
Discussion
Findings in this study demonstrate links between being an AO and increased engagement in riskier gambling behaviours and experiencing financial problems. This study found that an individual’s own gambling behaviours mediated relationships between being an AO and increased engagement in health risk behaviours. The relationship between AO status and poor general health was mediated by an individual’s own gambling behaviours and engagement in health risk behaviours. The significant relationship between AO status and low mental wellbeing was not initially mediated by an individual’s own gambling behaviours or engagement in health risk behaviours. However, after additionally controlling for experiencing financial problems this relationship was no longer significant. Crucially, this study indicated that such outcomes are not limited to individuals with relationships specifically with someone with problem gambling, but incorporated relationships with someone who gambles at any level (but at least regularly).
Relationships with Own Gambling
The finding in the current study that at-risk/problem gambling was over twice as likely among AOs compared to NAOs mirrors results seen in a Finnish population study (Lind et al., 2022). This relationship is likely seen due to social and environmental factors, which promote gambling as an increasingly normalised and shared activity between family members and peers, with gambling marketing playing a key role in this (Guillou-Landreat et al., 2021; King et al., 2010; Subramaniam et al., 2017). This relationship is further supported by research from Australia, which has demonstrated that within the social circles of those with at-risk/problem gambling there is an increased prevalence of gambling participation and harms (Russell et al., 2018). Such social circles were found to be deeply interconnected, and both influenced and normalised gambling behaviours (Russell et al., 2018). Family gambling attitudes and behaviours are a key factor that shape an individual’s gambling behaviours, both in youth and as an individual progresses through the life-course, with parental gambling heavily linked to the gambling behaviours of adolescents, including early initiation (Reith and Dobbie 2011; Emond & Griffiths, 2020). Certain family norms and practices may promote gambling as a normalised and shared family activity, however, also promote risks of experiencing future gambling harm. For example, in the UK, family members may purchase scratch cards for children, or family holidays at seaside resorts may involve children using ‘legal youth gambling products’ such as coin pusher machines, however, use of such products is also associated with future adult gambling participation and harm (Emond & Griffiths, 2020; Newall et al., 2021). Such interactions between family and youth gambling may play a role in shaping an individual’s future gambling activities, and reinforce relationships between individuals who gamble, which may help to explain at least a part of the relationship seen in the current study between being an AO and at-risk/problem gambling (Reith & Dobbie, 2011). This is particularly interesting in the context of the finding in the current study showing that for nearly one in ten AOs it was their parent who had been gambling regularly.
The links between being an AO and an individual’s own experiences of at-risk and problem gambling are concerning, as the relationships between these individuals may exacerbate difficulties in reducing gambling consumption, socially reinforcing experiences of gambling harm (Russell et al., 2018). Further, this relationship is likely to make situations whereby both individuals are proximal to each other in their daily lives increasingly difficult, as there will be a dual burden of experiencing harm not only from an individual’s own gambling behaviours but also the gambling behaviours of the other individual.
Relationships with Health Risk Behaviours
In contrast to other studies of AOs, there were no significant associations between AO status and any individual health risk behaviour. Methodological differences may partly explain this, in that the measure for being an AO in the current study was not exclusive to those with a relationship to someone with problem gambling. Therefore, for a higher proportion of individuals in the current study, the other individual’s gambling may not yet be significant enough of a problem to influence individual health risk behaviours, particularly not as a coping mechanism (Banks et al., 2018). However, an individual’s own gambling mediated the relationship between AO status and engagement in two or more health risk behaviours, so that this relationship was no longer significant. It is possible that through increased participation in gambling, AOs may be increasingly exposed to a range of health risk behaviours more generally, thus increasing engagement with health risk behaviours overall. This is supported by prior research by Butler et al. (2019) which demonstrated that individuals were more likely to engage in a range of health risk behaviours across the spectrum of gambling risk levels. Further Butler et al. (2019) suggested that health risk behaviours may be linked through environments and social norms, which provide opportunities to engage in multiple health risk behaviours in one setting. Any relationship which shows increased engagement in two or more health risk behaviours (even if mediated by an individual’s own gambling behaviours) warrants concern, as the cumulative effects of engaging in more than one health risk behaviour are greater than heightened engagement in one health risk behaviour alone, increasing the risks of morbidity (Bellis et al., 2016).
Findings also demonstrated direct harms from the other individual’s gambling, with one in five AOs experiencing at least one harm as a direct result of their relative or partner’s gambling. Conflicts in the relationship were the most prevalent harms shown, with these types of harms present for over one in ten AOs. A small number of AOs reported that they had experienced violence (or the threat thereof) or were concerned that the individual who had been gambling may harm their children. Previous literature has documented the impacts of gambling on violent outcomes in domestic settings, both in terms of intimate partner violence and child maltreatment (Hing et al., 2022; Roberts et al., 2016). However, such outcomes have not been well explored at the sub-problem gambling level, or outside of a domestic setting. It is beyond the scope of the current study to discern whether these outcomes were limited to those with a relationship to an individual with problem gambling or not. Future research may wish to prioritise exploring violent outcomes related to gambling, both at the sub-problem gambling level and for AOs outside of the same household.
Relationships with Experiencing Financial Problems
The current study found significant associations between AO status and experiencing financial problems. Further, it was also found in the current study that nearly one in ten AOs experience financial harm as a direct result of their partner or relative spending money on gambling activities. These findings are consistent with previous research showing the significant burden of financial problems on people experiencing problem gambling and AOs, which often reach crisis points (Banks et al., 2018; Dowling et al., 2021; Langham et al., 2015). Research has shown that financial problems are one of the first presenting gambling-related harms that AOs become aware of, with financial problems often preceding further second-hand harms such as emotional stressors, conflicts, and breakdown of relationships (Dowling et al., 2021; Holdsworth et al., 2013; Subramaniam et al., 2017). Prior research has demonstrated the direct detrimental impact of financial problems, such as unsecured debt, on mental health and wellbeing (Brown et al., 2005; Kiely et al., 2015; Richardson et al., 2013). The processes of dealing with financial problems can also be detrimental to health and wellbeing through, for example, having to work extra hours, having to substitute healthier choices (e.g., food) for cheaper less healthy alternatives, or go without things which are beneficial to health (e.g., a gym membership) (Banks et al., 2018). Financial problems also have significant implications for longer-term harms from gambling, even after an individual may cease gambling behaviours, with ongoing financial hardships, poverty, and reliance on welfare having notable impacts on health and wellbeing, with such harms also having intergenerational impacts (Dowling et al., 2021; Langham et al., 2015).
Relationships with Poor General Health and Low Mental Wellbeing
Associations between AO status and poor general health and low mental wellbeing were found in the current study. However, controlling for health risk behaviours and an individual’s own gambling behaviour mediated the relationship between being an AO and poor general health, with this association no longer significant. It is possible that through increased engagement with riskier gambling and other health risk behaviours (linked through gambling environments and social processes which promote engagement in multiple health risk behaviours), being an AO may increase risks of experiencing poor general health.
When an individual’s own gambling behaviour and health risk behaviours were controlled for, the relationship between AO status and low mental wellbeing remained significant, however, once financial problems were additionally controlled for this relationship was no longer significant. This indicates that for AOs, increased experiences of financial problems may be a driving cause of low mental wellbeing in this group. This is interesting considering the measure for being an AO in this study may include a wider group of AOs than those with a relationship to someone with problem gambling only. As such experiencing financial problems may potentially be an early driver of low mental wellbeing among AOs, before further gambling harms progress, with financial problems often a key driver of more psychosocial harms which may then take precedence (Dowling et al., 2021; Holdsworth et al., 2013; Subramaniam et al., 2017).
Implications for Policies and Support
The current study adds to the understanding that gambling-related harms impact a far larger proportion of the population than only an individual who gambles at the problem gambling level. Therefore, this study’s findings give support to public health policies that aim to prevent gambling harms across the spectrum of gambling risk levels—which may in turn prevent harms at individual, relationship, and societal levels. Policies that limit susceptibility to financial problems from gambling (such as affordability checks) may prove promising in protecting the health and wellbeing of people who gamble and AOs. Further, policies which aim to reduce the impacts of environmental factors which encourage engagement in multiple health risk behaviours are likely to have health benefits at the population level.
Previous research has found that AOs utilise a range of coping strategies before seeking other forms of support and that this is likely due to barriers, such as stigma and not being aware of what support is on offer, to seeking help from services, including those which offer informal support (Banks et al., 2018; Dowling et al., 2021). Therefore, improving public health messaging to increase awareness of gambling-related harms, what support is available, and encouraging AOs to seek support is essential to meeting the health and wellbeing needs of AOs. Support for AOs should be easily accessible regardless of the risk level of the other individual’s gambling, or the AO’s relationship to them, and when presenting to services the needs of AOs need to be assessed and managed holistically, including their own gambling and other health risk behaviours.
While gambling-related harms are generally significant before AOs will seek support, they may present earlier at services for other associated problems, such as financial problems or low mental wellbeing, this may then provide opportunities to screen for gambling-related harms and identify any relevant support needs (Butler et al., 2019). To address gambling-related harms it is critical that such opportunities are not missed, therefore routine enquiry into gambling harms (originating from both the individual’s own gambling behaviours and their relationships with others) in the context of presentations for factors such as financial problems or low mental wellbeing, may improve identification of those impacted by gambling harms.
Limitations
The findings in the current study must be considered in light of the following limitations:
The cross-sectional nature of this study means that any assessment of causality of the associations shown is not possible. It cannot be determined whether being an AO precedes an individual’s own risky gambling behaviours and low wellbeing or vice versa.
Harms may vary between different groups of AOs, however, no sub-group analyses were possible due to the relatively small sample size of AOs. Future exploration of experiences of harm and health risk behaviours in different groups of AOs at the sub-problem gambling level remains of importance.
The frequency of the partner or relative’s gambling was not assessed, and while it is hoped that our measure of ‘gambling regularly in the past 12 months’ will have included a range of partner or relative gambling behaviours (particularly including those at a sub-problem gambling level), it may be that only partners or relatives with a problem gambling were included. However, the higher prevalence of AOs in the current study (11.0%) compared to a previous UK-based study (6.5%; Gunstone et al., 2021), suggests that a wider group may have been included. In future research, if a partner or relative’s PGSI score were to be available this would be advantageous.
Conclusion
While gambling-related harms are increasingly being considered as a public health issue, health and social harms to AOs remain poorly understood and addressed. Most research on AOs has not taken into account harms that can occur at the sub-problem gambling level, and such evidence is particularly limited from a British perspective. This study aimed to address this gap by utilising a measure for identifying AOs in a general population which did not depend solely on the AO having a relationship with someone who gambles at the problem gambling level. This study indicated that there are associations between being an AO, their own risky gambling behaviours, financial problems, and poorer wellbeing. Support for AOs should therefore be more widely available, and not limited to those with a relationship with someone who gambles at the problem gambling level. Further, support for AOs should aim to address their needs holistically to have the greatest impact on wellbeing.
References
Banks, J., Andersson, C., Best, D., Edwards, M., & Waters J. (2018). Families living with problem gambling: Impacts, coping strategies and help-seeking. Sheffield Hallam University.
Bellis, M., Hughes, K., Nicholls, J., Sheron, N., Gilmore, I., & Jones, L. (2016). The alcohol harm paradox: Using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health, 16. https://doi.org/10.1186/s12889-016-2766-x
Brown, S., Taylor, K., & Wheatley, P. S. (2005). Debt and distress: Evaluating the psychological cost of credit. Journal of Economic Psychology, 26(5), 642–663. https://doi.org/10.1016/j,joep.2005.01.002
Browne M. (2020) Measuring harm from gambling and estimating its distribution in the population. In Bowden-Jones, H., C. Dickson, C. Dunand, & O. Simon, (Eds.) Harm reduction for gambling a public health approach, 1st ed. Routledge, pp.14–22
Browne, M., Greer, N., Rawat, V., & Rockloff, M. (2017). A population-level metric for gambling-related harm. International Gambling Studies, 17(2), 163–175. https://doi.org/10.1080/14459795.2017.1304973
Bush, K., Kivlahan, D., McDonell, M., Fihn, S., & Bradley, K. (1998). The audit alcohol consumption questions (audit-c): An effective brief screening test for problem drinking. Archives of Internal Medicine, 1(58), 1789–1795. https://doi.org/10.1001/archinte.158.16.1789
Butler, N., Quigg, Z., Bates, R., Sayle, M., & Ewart, H. (2019). Gambling with your health: Associations between gambling problem severity and health risk behaviours, health and wellbeing. Journal of Gambling Studies, 36(2), 527–538. https://doi.org/10.1007/s10899-019-09902-8
Canale, N., Vieno, A., & Griffiths, M. (2016). The extent and distribution of gambling-related harms and the prevention paradox in a British population survey. Journal of Behavioral Addictions, 5(2), 204–212. https://doi.org/10.1556/2006.5.2016.023
Castren, S., Lind, K., Hagfors, H., & Salonen, A. (2021). Gambling-related harms for affected others: A Finnish population-based survey. International Journal of Environmental Research and Public Health, 18(18). https://doi.org/10.3390/ijerph18189564
Dowling, N., Hawker, C., Merkouris, S., Rodda, S., & Hodgins, D. (2021). Addressing gambling harm to affected others: A scoping review. Victorian Responsible Gambling Foundation. Melbourne. https://www.drugsandalcohol.ie/38077/1/VRGF_RR_Gambling_AffectedOthersScopingReview.pdf
Emond, A., & Griffiths, M. (2020). Gambling in children and adolescents. British Medical Bulletin, 136(1), 21–29. https://doi.org/10.1093/bmb/ldaa027
Ferris, J., & Wynne, H. (2001). The Canadian problem gambling index: Final report. Ottawa.
Goodwin, B., Browne, M., Rockloff, M., & Rose, J. (2017). A typical problem gambler affects six others. International Gambling Studies, 17(2), 276–289. https://doi.org/10.1080/14459795.2017.1331252
Guillou-Landreat, M., Gallopel-Morvan, L., Lever, D., Le Goff, D., & Le Reste, J. (2021). Gambling marketing strategies and the internet: What do we know? A systematic review. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.583817
Gunstone, B., Gosschalk, K., Zabicka, E., & Sullivan-Drage, C. (2021) Annual GB treatment and support survey 2021. Gamble Aware. https://www.begambleaware.org/sites/default/files/2022-03/Annual%20GB%20Treatment%20and%20Support%20Survey%20Report%202021%20%28FINAL%29_0.pdf.
Hing, N., O’Mullan, C., Mainey, L., Greer, N., & Breen, H. (2022) An integrative review of research on gambling and domestic and family violence: Fresh perspectives to guide future research. Frontiers in Psychology, 13. https://doi.org/10.3389/fpsyg.2022.987379
Holdsworth, L., Nuske, E., Tiyce, M., & Hing, N. (2013) Impacts of gambling problems on partners: Partners’ interpretations. Asian Journal of Gambling Issues and Public Health, 3(11). https://doi.org/10.1186/2195-3007-3-11
Holtgraves, T. (2008). Evaluating the problem gambling severity index. Journal of Gambling Studies, 25(1), 105–120. https://doi.org/10.1007/s10899-008-9107-7
Kiely, K., Leach, L., Olesen, S., & Butterworth, P. (2015). How financial hardship is associated with the onset of mental health problems over time. Social Psychiatry and Psychiatric Epidemiology, 50, 909–918. https://doi.org/10.1007/s00127-015-1027-0
King, D., Delfabbro, P., & Griffiths, M. (2010). The convergence of gambling and digital media: Implications for gambling in young people. Journal of Gambling Studies, 26, 175–187. https://doi.org/10.1007/s10899-009-9153-9
Langham, E., Thorne, H., Browne, M., Donaldson, P., Rose, J., & Rockloff, M. (2015). Understanding gambling related harm: A proposed definition, conceptual framework, and taxonomy of harms. BMC Public Health, 16(1). https://doi.org/10.1186/s12889-016-2747-0
Li, E., Browne, M., Rawat, V., Langham, E., & Rockloff, M. (2017). Breaking bad: Gambling harms among gamblers and affected others. Journal of Gambling Studies, 33, 223–248. https://doi.org/10.1007/s10899-016-9632-8
Lind, K., Castren, S., Hagfors, H., & Salonen, A. (2022). Harm as reported by affected others: A population-based cross-sectional Finnish gambling 2019 study. Addictive Behaviours, 129. https://doi.org/10.1016/j.addbeh.2022.107263
Newall, P., Russell, A., Sharman, S., & Walasek, L. (2021) Recollected usage of legal youth gambling products: Comparisons between adult gamblers and non-gamblers in the UK and Australia. Addictive Behaviors, 114. https://doi.org/10.1016/j.addbeh.2020.106685
Newall, P., Weiss-Cohen, L., Thoma, V., & Ayton, P. (2022). Differences amongst estimates of the UK problem gambling prevalence rate are partly due to a methodological artefact. International Journal of Mental Health and Addiction. https://doi.org/10.1007/s11469-022-00877-z
Orford, J. (2020). The gambling establishment challenging the power of the modern gambling industry and its allies. 1st edn. Routledge.
Reith, G., & Dobbie, F. (2011). Beginning gambling: The role of social networks and environment. Addiction Research & Theory, 19(6), 483–493. https://doi.org/10.3109/16066359.2011.558955
Richardson, T., Elliott, P., & Roberts, R. (2013). The relationship between personal unsecured debt and mental and physical health: A systematic review and meta-analysis. Clinical Psychology Review, 33(8), 1148–1162. https://doi.org/10.1016/j.cpr.2013.08.009
Riley, B., Harvey, P., Crisp, B., Battersby, M., & Lawn, S. (2018). Gambling-related harm as reported by concerned significant others: A systematic review and meta-synthesis of empirical studies. Journal of Family Studies, 27(1). https://doi.org/10.1080/13229400.2018.1513856
Roberts, A., Coid, J., King, R., Murphy, R., Turner, J., Bowden-Jones, H., Du Preez, K., & Landon, J. (2016). Gambling and violence in a nationally representative sample of UK men. Addiction, 111(12), 2196–2207. https://doi.org/10.1111/add.13522
Russell, A., Langham, E., & Hing, N. (2018). Social influences normalize gambling-related harm among higher risk gamblers. Journal of Behavioral Addictions, 7(4), 1100–1111. https://doi.org/10.1556/2006.7.2018.139
Stewart-Brown, S., Tennant, A., Tennant, R., Platt, S., Parkinson, J., & Weich, S. (2009) Internal construct validity of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS): A Rasch analysis using data from the Scottish Health Education Population Survey. Health and Quality of Life Outcomes, 7. https://doi.org/10.1186/1477-7525-7-15
Sturgis, P. (2020) An assessment of the accuracy of survey estimates of the prevalence of problem gambling in the United Kingdom. https://about.gambleaware.org/media/2179/an-assessment-of-the-accuracy-of-survey-estimates-of-the-prevalence-of-problem-gambling-in-the-united-kingdom.pdf
Subramaniam, M., Chong, S., Satghare, P., Browning, C., & Thomas, S. (2017). Gambling and family: A two-way relationship. Journal of Behavioral Addictions, 6(4), 689–698. https://doi.org/10.1556/2006.6.2017.082
Sulkunen, P., Babor, T., Ornberg, J., Egerer, M., Hellman, M., Livingstone, C., Marionneau, V., Nikkinen, J., Orford, J., Room, R., & Rossow, I. (2019). Setting limits gambling science and public policy (1st ed.). Oxford University Press.
The Gambling Commission (2023). Statistics on participation and problem gambling for the year to March 2023. Gambling Commission. https://www.gamblingcommission.gov.uk/statistics-and-research/publication/statistics-on-participation-and-problem-gambling-for-the-year-to-march-2023.
Tulloch, C., Browne, M., Hing, N., Rockloff, M., & Hilbrecht, M. (2021). How gambling harms the wellbeing of family and others: A review. International Gambling Studies, 22(3), 552–540. https://doi.org/10.1080/14459795.2021.2002384
Velleman, R., Cousins, J., & Orford, J. (2015) Effects of gambling on the family. In: H., Bowden-Jones, & S., George, (Eds.), A clinician's guide to working with problem gamblers, 1st ed. Routledge, pp.90–103.
Wardle, H. (2015) Gambling behaviour in Britain. In: H., Bowden-Jones, & S., George (Eds.), A clinician's guide to working with problem gamblers, 1st ed. Routledge, pp.2–14.
Wardle, H., John, A., Dymond, S., & McManus, S. (2020). Problem gambling and suicidality in England: Secondary analysis of a representative cross-sectional survey. Public Health, 184, 11–16. https://doi.org/10.1016/j.puhe.2020.03.024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest with regards to this article.
Data availability statement
The study materials and data are available from the corresponding author upon reasonable request.
Human and Animal Rights
This research study was approved by the Liverpool John Moores University Research Ethics Committee (reference number: 19/PHI/044). All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wilson, C., Butler, N. & Quigg, Z. Harms from Other People’s Gambling: Associations with an Individual’s Own Gambling Behaviours, Health Risk Behaviours, Financial Problems, General Health, and Mental Wellbeing. J Gambl Stud (2024). https://doi.org/10.1007/s10899-024-10291-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s10899-024-10291-w