Abstract
Purpose
Family violence (FV) is defined as any situation where an individual employs abusive behaviour to control and/or harm a former or current spouse, non-marital partner, or a member of their family. The health consequences of FV are vast, including a wide range of physical and mental health conditions for individuals experiencing violence or survivors, perpetrators, and their children. Primary health care (PHC) is recognized as a setting uniquely positioned to identify the risk and protective factors for FV, being an entry point into the health care system and a first, or only, point of contact for families with professionals who can facilitate access to specialist care and support.
Methods
A rapid evidence assessment of empirical studies on FV interventions in PHC was conducted to examine outcomes of effective FV interventions that promote identification, assessment, and care delivery within diverse PHC settings, factors shaping PHC provider and system readiness, and key intervention components that are important for sustaining PHC responses to FV. After completing data extraction, quality appraisal, and a hand search, a total of 49 articles were included in data synthesis and analysis.
Results
Several FV interventions that include multiple components such as, screening and identification of FV, training of PHC providers, advocacy, and referrals to supports, have been rigorously tested and evaluated in diverse PHC settings in rural and urban areas including primary care/family medicine practice clinics and community PHC centers. These interventions have demonstrated to be effective in identifying and responding to violence primarily experienced by women. There is a dearth of FV interventions or programs from empirical studies focused on men, children, and perpetrators. Additionally, provider and system readiness measurement tools and models have been implemented and evaluated in PHC specifically to assess physician or the health care team’s readiness to manage FV in terms of knowledge and awareness of FV. The findings highlight that there is no clear or standardized definition of provider or system “readiness” in the literature related to FV responses in PHC. Further, the findings revealed four key intervention components to facilitate PHC provider and organization readiness to address FV: (1) multidisciplinary teamwork and collaboration, (2) improving provider knowledge on the social and cultural determinants impacting FV, and (3) embedding system-level supports within PHC.
Conclusions
FV is a serious public health concern and PHC providers have a vital role in early detection of FV and the poor health outcomes associated with violence A focus on comprehensive or multi-component FV interventions are more likely to change provider behavior, and would allow for safe, confident, and professional identification and assessment of FV within PHC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Family violence (FV) has been defined as behaviour directed towards a family member, or someone with whom they have an intimate relationship such as former or current spouse or non-marital partner that is physically, sexually, emotionally, psychologically, or economically abusive or coercive (Benbow et al., 2018). It can include intimate partner abuse (Zahl-Olsen et al., 2019), child physical abuse, child sexual abuse, and elder abuse (Guedes et al., 2016; Libal & Parekh, 2009).
The health consequences of FV include a wide range of physical and mental health conditions in individuals experiencing violence or survivors, perpetrators, and their children (Hooker et al., 2020; Sharma & Borah, 2022; Taylor, 2016; van Gelder et al., 2020). Research evidence suggests that IPV-related physical and mental health outcomes differ between men and women (Hayes & Kopp, 2019). Men who were exposed to intimate partner violence (IPV) were most likely to report externalized mental health issues such as behavioral disorders and substance use disorder (Afifi et al., 2009), whereas women who experience IPV report physical, physiological, and psychological impacts (Benbow et al., 2018). Psychological impacts range from experiences with stress, frustration, anger, decreased social function to severe depression, anxiety, post-traumatic stress disorder and suicidality (Benbow et al., 2018; Gear et al., 2016). Exposure to FV in children can result in social, behavioral, emotional, and cognitive problems (Hooker et al., 2020; Rossman, 2001; Ullman et al., 2013). These outcomes often persist into adulthood and increase the potential for their own later experience with or perpetration of violence (Letourneau et al., 2007; Wolfe et al., 2003). Individual studies show that Indigenous peoples experience FV at much higher rates than non-Indigenous people (Breiding et al., 2014; Brownridge, 2008; Burczycka & Conroy, 2018; Fiolet et al., 2021; Sinha et al., 2013), leading to disproportionately high rates of physical injury and mental health issues, as well as increased numbers of familial homicides (Burczycka & Conroy, 2018; Lievore, 2005; Mouzos, 2001; Mouzos & Rushforth, 2003). The high prevalence of FV impacting Indigenous peoples reflects the lasting impacts of colonialism and cultural suppression that perpetuates intergenerational trauma and cycles of violence (Heidinger, 2018; National Inquiry into Missing and Murdered Indigenous Women and Girls, 2019).
Prior studies of individuals with a history of FV have documented increased health care utilization (Arias & Corso, 2005). This has been found for inpatient hospitalization, primary and specialty care, and mental health care (Bonomi et al., 2009). Women exposed to physical and sexual violence are shown to have higher mental health care utilization compared to women who never had experienced such violence (Bonomi et al., 2009; Rivara et al., 2007). Additionally, women who are sexually assaulted may experience re-occurring reproductive, gastrointestinal, cardiovascular, and sexual health problems (Basile et al., 2022). However, much of the current literature has been based on clinic (Miller et al., 2010) or convenience samples (Hoelle et al., 2015), relying exclusively on self-reports about utilization (Rivara et al., 2007), with research conducted mostly in the United States (Bonomi et al., 2009; Miller et al., 2010). No studies have examined whether health care utilization varies in relationship to the time of abuse, both during and after the period of FV.
Primary health care (PHC) is recognized as a setting uniquely positioned to identify the risk and protective factors for FV, being an entry point into the health care system and a first, or only, point of contact for families with professionals who can facilitate access to specialist care and support (Bradley et al., 2020; Gear et al., 2012). Family physicians and registered nurses have more contact with individuals affected by violence and abuse than other health services (Beynon et al., 2012; Richardson et al., 2002). Literature on barriers to screening and assessment for FV in PHC predominantly focus on individual issues such as, a lack of confidence among general practitioners in both recognizing violence and knowing how to directly raise the topic with patients (Ramsay et al., 2012), shortage of time with the patient, and absence of FV training or skills (Goicolea et al., 2017; Hudspeth et al., 2022; Ramsay et al., 2012), rather than system and organizational factors that impede directly on a provider’s ability to respond to FV. Additionally, the barriers experienced by PHC providers with screening and assessing for FV in virtual environments during the COVID-19 pandemic has also been studied, which include impacts on provider-patient relationships, quality and safety of care, and confidentiality (Montesanti et al., 2022).
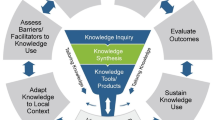
Moreover, previous research has demonstrated which intervention components are essential for facilitating FV screening and assessment within health care settings. Comprehensive FV interventions that incorporate multiple components, including institutional or system-level supports, referral supports, and provider education have demonstrated greater success in increasing FV screening and identification rates and improved care delivery than ‘‘screening-only’’ interventions (O'Campo et al., 2011). However, there is limited knowledge on how to successfully implement and sustain multi-component interventions in PHC practices (Larkins et al., 2015). Additionally, the degree to which providers and organizations are ready for change to adopt new health services or programs can be important predictors of whether an intervention is successfully implemented. The concept of ‘readiness’ can be applied to understand PHC providers preparedness through increasing knowledge and skills to adopt or implement FV interventions within their routine practice, as well as their motivation and attitudes towards addressing FV (Hegarty et al., 2020). Health care provider readiness also goes beyond increasing the knowledge and skills of providers, to assessing how physically and emotionally ready providers are for the work. Furthermore, assessing organizational readiness for change involves identifying organizational dynamics, climate, and culture, change processes and individual organizational member characteristics such as the team environment (Kelly et al., 2017). This paper describes the findings from a rapid evidence assessment of comprehensive FV interventions in PHC, which were used to guide the development of a FV PHC readiness tool in a Canadian province.
Methods
A rapid evidence assessment of empirical studies on FV interventions in PHC was conducted within a five-month timeframe. The aims of this rapid evidence assessment were: 1) to evaluate outcomes of comprehensive FV interventions that promote identification, assessment, and care delivery within diverse PHC settings (i.e., interventions that incorporate approaches beyond screening only); 2) to examine provider and system characteristics that determine readiness for implementing FV interventions in PHC practices; and 3) identify underlying intervention components that are important for sustaining PHC responses to FV. Rapid evidence assessments are a rigorous and explicit method that utilize a wide range of evidence to provide a timely, valid, and balanced assessment of available empirical evidence related to a particular policy or practice issue in a short timeframe (Thomas et al., 2013). The process is characterized by developing a focused research question, a less developed search strategy, literature searches, and then more simplified data extraction and quality appraisal of the identified literature when compared to traditional systematic reviews (Watt et al., 2008).
Search Strategy
A search was executed by an expert searcher/health librarian (SC) on the following databases: PROSPERO, OVID Medline, EBSCO CINAHL, and SCOPUS using controlled vocabulary (e.g., MeSH) and key words representing the concepts “domestic violence” and “primary care” and “organizational structure” and “intersectoral cooperation” and “readiness.” Searches were limited to articles published in English between 2005–2022. Results (n = 371) were exported to Covidence software for review management where 38 duplicates were removed. Detailed search strategies are available in supplementary information A. We imported citations from our search results to EndNote reference management software (v. X9, Clarivate Analytics). The primary electronic database search was complemented by a secondary search, including non-systematic searching of Google Scholar, hand searching of selected journal articles, reference and citation tracking of all included studies.
Study Screening and Selection
Two reviewers (DG and KB) independently screened all potential articles. In the case of disagreement, both reviewers read and discussed the article until consensus was reached. Articles were included only if they satisfied all four inclusion criteria (Supplementary Information C): (1) focused on PHC settings; (2) described the development and/or implementation of multi-component FV interventions or programs within PHC; (3) described the factors that shape provider or organization readiness to adopt or implement FV interventions; and (4) if the article was published in the English language.
The search strategy identified 333 articles for potential inclusion. Following a review of the titles and abstracts, 226 articles were included for full-text review. The full text was retrieved for all articles, and an additional 70 articles were excluded because they did not meet full-text extraction criteria (for example, if the intervention did not use a comprehensive approach to the identification, assessment, and care delivery for FV or report on outcomes). Following full-text review, 46 studies met all inclusion criteria. The PRISMA flow diagram for the literature search is shown in Fig. 1 and the PRISMA-S checklist is included in the supplementary information B. Additionally, we identified four articles through a hand search that met our inclusion criteria and were included in the data synthesis and analysis.
Data Extraction and Analysis
Two reviewers (DG and KB) independently extracted the following information from included studies into a standard extraction form (Supplementary Information D): article citation, publication type, population studied, country, study setting, description of the FV intervention, description of intervention components (e.g., provider training, referral to supports, screening tool, institutional supports, collaboration and coordination with community agencies/organizations, training and education of PHC providers), role of interdisciplinary PHC team, and challenges or barriers to implementing and sustaining FV interventions or programs within PHC settings described by the authors. To evaluate outcomes from FV interventions implemented in PHC practices quantitative and qualitative data was extracted by the first author (SM) using the Reach, Effectiveness, Adoption, Implementation fidelity, and Maintenance (RE-AIM) framework (Glasgow et al., 1999) and Proctor’s dimensions of implementation effectiveness (Proctor et al., 2011). Both frameworks are widely used in the implementation literature for their inclusion of constructs relevant to implementation success in multiple settings. The authors focused on Proctor’s dimensions of acceptability and cost, as the other dimensions (Adoption, Fidelity, Penetration/Reach, and Sustainability/Maintenance) are captured under the RE-AIM framework. Independent extraction by DG and KB ensured the accuracy of included data and that any relevant information was not missed. Data synthesis and analysis of the findings was conducted by the first author (SM), and final results were reviewed with DG. (Finfgeld-Connett, 2013).
Quality Assessment
The quality of the studies was assessed using the Critical Appraisal Skills Program (CASP) and the Joanna Briggs Institute Critical Appraisal tool (JBI). Specifically, the CASP Systematic Review Checklist, CASP Qualitative Checklist, CASP Randomized Controlled Trial Checklist, JBI case study checklist, JBI cross sectional checklist, and JBI cohort study checklist, and JBI quantitative study checklist were used. Since the developers of either appraisal tool did not recommend using a scoring system, included studies were assessed based on clarity of the research objectives, appropriateness of the data collection strategy, and quality of the research methodology. Quality assessments were independently completed by two reviewers (DG and KB); any conflicts were resolved through consensus. No studies were excluded from the review based on the quality assessment.
Results
Description of Study Characteristics
In total, 50 articles were included in this review (Supplementary Information E). The types of studies included systematic reviews (2), randomized control trials (1), cohort studies (3), cross-sectional studies (6), case studies (5), qualitative studies (19), case control studies (1), and mixed methods studies (11). The included articles were based in Australia (1), Canada (4), China (1), Denmark (1), Egypt (1), Greece (2), India (1), Malaysia (2), Mexico (1), Netherlands (2), New Zealand (5), Palestine (1), Saudi Arabia (1), South Africa (1), Spain (5), Tanzania (1), Turkey (1), UK (8), USA (12), or had a global focus (3). The PHC settings mainly included general practice/family medicine clinics and community health centers which were based (or described programs) in urban (21), rural/remote (2), or a mix of both (26) settings. One study implemented a FV intervention within a pediatric clinic that serves only children (Eismann et al., 2019). Seven articles described the implementation of interventions or programs in mixed health care settings that included general practitioner clinics and other settings such as the hospital emergency department and an outpatient academic primary care clinic (Ambuel et al., 2013; Briones-Vozmediano et al., 2022; Clark et al., 2020; Colombini et al., 2020; García-Quinto et al., 2022; Goicolea et al., 2015; Goicolea et al., 2019). One study described the implementation of an IPV intervention within a PHC setting but involved outreach by a registered nurse outside the clinic setting (Ford-Gilboe et al., 2011). It is important to note that the terms primary health care (PHC) or primary care were both used across the included studies. The authors of these studies do not provide an explanation for the use of either term. Upon observation there appears to be geographical differences in the use of the term across the literature—for example, ‘primary care’ is more commonly used in the UK compared to ‘primary health care’ in New Zealand. The conceptual differences between the terms ‘primary health care’ and ‘primary care’ have been explored in the academic literature. The term PHC has been used to denote a shift from solo family doctor practices delivering selective, treatment-focused models that focus on the health of individuals, to a more comprehensive model that encompasses a wider population health focus that includes population-based screening programs, a deliberate focus on the social determinants of health, and integration with community and social services (Baum et al., 2017). While both terms denote different models of health service delivery, they are often used interchangeable in the literature.
The target study populations involved in the research studies included members of the health care teams and allied health workers (clinicians/general practitioners, nurse practitioners or registered nurses, midwives, psychologists, social workers, nutritionists, paramedics, community health workers, ancillary professional staff (e.g., laboratory technicians), as well as survivors, their caregivers, children, and perpetrators. One Canadian study examined PHC providers’ preparedness to support Indigenous women who experience IPV (Rizkalla et al., 2020).
The findings are organized into three main categories: 1) implementation outcomes from FV interventions implemented in PHC settings, 2) PHC provider, system/service readiness measurement tools and models; and 3) intervention components for sustaining PHC responses to FV.
Implementation Outcomes from FV Interventions in PHC Settings
Clinical effectiveness and implementation outcomes from FV interventions implemented in PHC were evaluated (Table 1). Four specific FV interventions implemented within PHC settings were identified (Ambuel et al., 2013; Bradbury-Jones et al., 2017; Dowrick et al., 2020; Eismann et al., 2019; Feder et al., 2011; Joyner & Mash, 2012; Ramsay et al., 2012; Szilassy et al., 2021; Wuest et al., 2015). The Identification and Referral Program to Improve Safety (IRIS) was assessed in five of the included studies (Bradbury-Jones et al., 2017; Dowrick et al., 2020; Feder et al., 2011; Ramsay et al., 2012; Szilassy et al., 2021). This is a cost-effective training, support, and referral program within general practice across the UK that aims to improve the response of clinicians to women experiencing abuse. The IRIS program was tested in randomized controlled trials in different general practice settings which reported positive outcomes after implementing the program, including increased overall referrals from general practice to specialist care (Feder et al., 2011), women feeling empowered by the referral process (Bradbury-Jones et al., 2017), and feeling safe to talk to their providers about their experience with domestic violence (Bradbury-Jones et al., 2017; Szilassy et al., 2021). Feder et al. (2011) implemented the IRIS program across 24 general practice sites across two primary care trusts in the UK and recorded 223 referrals of patients to advocacy resources and 641 disclosures of domestic violence in the intervention group. Dowrick et al. (2020) examined how the IRIS program changed professional practice within UK general practices in two urban primary care trusts. They described the work involved in restructuring the relationship between primary care and specialist domestic violence and abuse (DVA) services, which enabled flexible referral and feedback processes, and encouraged movement of patients to specialist service from PHC settings (Dowrick et al., 2020). The authors described how the collaboration between both professional groups with different histories, systems of bureaucracy, professional skills, spaces of work, identities, and jurisdictions was a positive outcome of the IRIS program (Dowrick et al., 2020). Some challenges with the IRIS program described by authors included time constraints with patient consultations (Ramsay et al., 2012; Szilassy et al., 2021), lack of clarity about expectations and responsibility for action when information about domestic violence and abuse was shared (Dowrick et al., 2020; Ramsay et al., 2012; Szilassy et al., 2021), limited availability of resources (Bradbury-Jones et al., 2017; Dowrick et al., 2020; Feder et al., 2011; Ramsay et al., 2012; Szilassy et al., 2021), challenges modifying the behaviour and attitude of clinicians (Ramsay et al., 2012), and difficulties ensuring women’s agency in disclosing abuse (Bradbury-Jones et al., 2017).
The article by Szilassy et al. (2021) expanded the IRIS program to develop IRIS + (Enhanced Identification and Referral to Improve Safety), which extends to address the needs of men (survivors and perpetrators) and children, in addition to women survivors. The study highlighted challenges with the adoption of the IRIS model (which was originally designed to support female survivors) to the identification and referral of supports for men and children. Pre/post intervention questionnaires with clinicians and patients and semi-structured interviews with clinicians, service providers and referred adults and children demonstrated specific barriers to referring men to IRIS + . These included relatively low prevalence of male survivors compared to female survivors in the general population; less contact with men due to infrequent general practitioner visits compared to women; assumption that men are unwilling to disclose due to concerns about confidentiality; and clinicians’ anxiety about having difficult conversations with individuals who might be violent (Szilassy et al., 2021). There was also a fear among clinicians that children would be removed from their home. The study findings concur that general practice clinicians lack substantial child safeguarding training, which poses challenges in supporting survivors and their children (Szilassy et al., 2021). This highlights the need for identification and appropriate referral of all family members exposed to domestic violence, especially children, whose needs are often neglected (Szilassy et al., 2021).
The Safe Environment for Every Kid (SEEK) model was described in one study, which aims to identify and help address prevalent psychosocial risk factors for child maltreatment in PHC settings in the USA (Eismann et al., 2019). This is the only intervention identified in the review that focused on the prevention of adverse childhood experiences (ACEs), such as abuse, IPV, parental separation or divorce, substance abuse, and mental illness. The model was studied in university-based resident clinics and pediatric practices and consists of four components: (1) training for child health care professionals on addressing targeted psychosocial risk factors; (2) screening caregivers for psychosocial risk factors at well-child visits age 0 to 5 years; (3) brief intervention incorporating principles of motivational interviewing to engage caregivers; and (4) referral to treatment. In Eismann et al.’s (2019) feasibility study of the SEEK model, screening completion rates at the resident clinics and pediatric practices ranged from 75 to 93% (Eismann et al., 2019).
One advocacy intervention identified in the literature was a theory-based intervention tested in two Canadian provinces called the Intervention for Health Enhancement After Leaving (iHEAL) (Ford-Gilboe et al., 2011). The goal of iHEAL is to improve women’s health and quality of life after leaving an abusive partner (Ford-Gilboe et al., 2011). The iHEAL is a short-term (6-month), complex, intervention for women who are past the initial crisis of leaving, and who are working through the transition of creating a life separate from their abusive partners. It is delivered in 12–14 visits in women’s homes or safe locations by a registered nurse and domestic violence advocate with specialized expertise in violence and trauma, such as a domestic violence outreach worker or social worker, working in partnership in the context of a larger team and in collaboration with the woman (Ford-Gilboe et al., 2011; Wuest et al., 2015). Ford-Gilboe et al (2011) describes the early phases and testing of the iHEAL intervention published in 2011. Empirical studies evaluating the outcomes of iHEAL, including adaptations of the intervention for specific populations (including Indigenous women) have since been published (Varcoe et al., 2021; Wuest et al., 2015) and were identified through a hand search.
Joyner and Mash (2012) described the feasibility and acceptability of implementing a comprehensive model for recognizing, assessing, and assisting women survivors of IPV in South African PHC settings located in urban and rural areas. A three-tier model of care for women who experienced IPV emerged from a co-operative inquiry group process that involved four nurses, one doctor and a qualitative researcher. The first tier relies on the PHC provider, usually a nurse, to recognize cues suggestive of IPV (Joyner & Mash, 2012). The model promoted selective case finding of women with a higher risk of IPV following feedback from clinicians who expressed concerns with high workloads. If IPV is disclosed as an underlying issue, then the clinician will deliver important clinical aspects of care and refer to a local IPV champion (Joyner & Mash, 2012). The IPV champion is someone with capacity to provide more comprehensive assessment and counselling, a desire to work with patients experiencing IPV; empathy and good listening skills; respect for client confidentiality and autonomy; an efficient case manager; employs a collaborative approach to problem-solving; and effective multi-disciplinary teamwork (Joyner & Mash, 2012). The IPV champion could be a social worker who would work in collaboration with the PHC team (Joyner & Mash, 2012). The second tier relies on an IPV champion. Here patients are assessed and assisted comprehensively by the IPV champion and then invited to participate in a five-week empowerment group. The third tier relies on the establishment of community-based support groups that would support women in the longer-term. These groups could be established with the help of the IPV champions (Joyner & Mash, 2012).
PHC Provider, System/Service Readiness Measurement Tools, and Models
Eleven studies reported on the implementation of readiness tools or guiding models to measure clinician or health care teams’ readiness to manage IPV. The Physician Readiness to Manage IPV Survey (PREMIS) was described in nine articles included in this review (Alsalman et al., 2023; Ambikile et al., 2020; Clark et al., 2020; Goicolea et al., 2015, 2019; Martin-Engel et al., 2021; Papadakaki et al., 2012, 2013; Ramsay et al., 2012). PREMIS is a 67-item questionnaire developed and validated in the USA to assess the preparedness of physicians to manage IPV and to evaluate the effectiveness of physician IPV education and training. The PREMIS tool psychometrically evaluates: (1) perceived knowledge, (2) actual knowledge, (3) preparedness, and (4) practice issues surrounding IPV (Ambikile et al., 2020; Clark et al., 2020; Goicolea et al., 2015, 2019; Martin-Engel et al., 2021; Papadakaki et al., 2012, 2013; Ramsay et al., 2012). It measures readiness using multidimensional scales and subscales. The PREMIS tool was evaluated in PHC settings in other countries including Spain (Goicolea et al., 2015), Greece (Papadakaki et al., 2013) and Saudi Arabia (Alsalman et al., 2023). Papadakaki et al. (2013) used a pre/post design with a control group to measure changes in IPV knowledge, perceived knowledge, perceived preparedness, and detection ability of general practitioners and general practice residents serving rural health centers in Crete, Greece following an intensive two-day IPV training program. Test–retest reliability was evaluated with good correlation values within a time interval of 2–4 weeks (Papadakaki et al., 2013). The training was highly accepted, and the results showed increased preparedness, perceived knowledge, and actual knowledge post intervention and after 12 months by both general practitioners and medical residents (with residents scoring better on actual knowledge). In this study, PREMIS was a useful tool to ascertain physician readiness to support IPV survivors (Papadakaki et al., 2013). Another study by Clark et al. (2020) conducted interviews and administered PREMIS to identify practices, policies, barriers, and opportunities to improve IPV response in an outpatient primary care clinic. The providers who participated understood IPV screening to be within the scope of their work; however, they highlighted challenges with lack of staff training and education resources (Clark et al., 2020). Alongside the interviews, the findings from the PREMIS helped the study team to identify provider needs, whether it be through further IPV training or the creation of an established referral network (Clark et al., 2020). Alsalman et al. (2023) administered a modified version of the PREMIS tool to reflect Saudi culture and primarily addresses women’s abuse. Among the 169 physicians working in PHC centers in Saudi Arabia who completed the self-administered questionnaire, the results showed an inadequate level of perceived preparedness among physicians. Approximately one-third of the participants perceived themselves as well-prepared to ask appropriate questions about IPV, respond to abuse disclosure, and identify as well as assist patients. Moreover, only 18.3% of them perceived themselves to have good knowledge regarding IPV.
Another study by Leung et al. (2017) described the development of the 30-item GRIPS scale to assess the perceived readiness of general practitioners to identify and respond to IPV. The readiness scale was created to further measure training outcomes and to identify practitioners’ training needs, which is beyond the scope of the existing and widely used PREMIS tool (Leung et al., 2017). Only requiring 15 mins to complete, the results of this research study indicated that GRIPS is an easily administrable scale, particularly effective in measuring health practitioners’ self-efficacy, motivational and emotional readiness to address IPV (Leung et al., 2017). Achieving face-, content- and construct-validity, as well as internal consistency reliability, GRIPS is a promising tool that can help facilitate IPV disclosure and identification within general practice (Leung et al., 2017).
Hegarty et al. (2020) conducted a qualitative meta-synthesis on health practitioners’ perceptions of what enhances their readiness to address IPV. The authors identified five themes for facilitating readiness of health providers to address DVA: (1) having a personal commitment to addressing DVA, (2) adopting an advocacy approach by working with their patients on pathway to safety and wellness, (3) trusting the relationship between the provider and patient, (4) collaborating with a team, and (5) being supported by the health system through training to address DVA, making asking about DVA routine, and allowing time to do the sensitive work with patients (Hegarty et al., 2020). Their findings led them to develop the CATCH (Commitment, Advocacy, Trust, Collaboration, Health System Support) model, which can enable clinicians to tailor IPV strategies in the health setting and support their readiness in addressing IPV (Hegarty et al., 2020).
The review also identified 3 tools for assessing health system/service readiness to respond to FV. One qualitative study described the Health System Readiness Assessment Tool implemented on occupied Palestinian Territory, that identified health system obstacles to successfully implementing PHC interventions to address domestic violence (Colombini et al., 2020). This study found partial readiness for health systems and services to adopt domestic violence interventions related to governance (no DV legislation), financial resources (limited or no public funding and limited staff and infrastructure), information systems, service coordination (disjointed referral network), and to some extent around the values system (tension between patriarchal views on domestic violence and more gender equal norms). Gear and colleagues (Gear et al., 2016) developed the Primary Health Care FV Responsiveness Evaluation Tool which encompasses key system elements to guide an effective response to FV and quality improvement benchmark in PHC. Lastly, the Health care Can Change from Within (HCCW) model described by Ambuel et al. (2013) aims to shift multiple levels of the health care system, including clinical staff, clinical environment, and clinical culture. Sustained improvements at two-year follow-up were reported at the individual level, with increased provider knowledge of referral resources and self-efficacy supporting patients experiencing IPV, as well as at the systems level, through strengthening of relationships with non-profit domestic violence-focused agencies (Ambuel et al., 2013). The HCCW model was tested in four family medicine outpatient clinics and one pediatric outpatient clinic. Similarly, Hamberger et al. (2014) conducted a longitudinal cohort study of the HCCW model and noted similar findings with respects to increased provider knowledge as Ambuel et al. (2013). Furthermore, research findings on the HCCW model show significant positive changes in clinic environment and clinical practice. However, the model was tested with a small sample size in clinic settings and involved a single group, pre-post quasi-experimental study design, affecting generalizability of the results to other health care clinics and systems.
Despite the development of tools or models to measure PHC provider and system/service readiness, there remain knowledge gaps on evaluating readiness based on structural capabilities beyond providers’ knowledge, to include policy, organizational structure, and organizational leadership (Gear et al., 2018). Only five articles had described specific organizational readiness activities (e.g., infrastructure, management support) to further sustain changes on providers’ capacity to manage violence and abuse (Chappell et al., 2021; Colombini et al., 2020; Gear et al., 2021; Hegarty et al., 2020; Miller & Jaye, 2007) (Table 2).
Intervention Components for Sustaining PHC Responses to FV
The findings highlighted three key intervention components for sustaining PHC responses to FV. These intervention components include: (1) strengthening multidisciplinary teamwork and collaboration, (2) improving provider knowledge on the social and cultural determinants impacting FV, and (3) embedding system-level supports for providers in PHC. Each of these components are described in detail below.
Multidisciplinary Teamwork and Collaboration
A factor enhancing clinician readiness and sustainment of FV responses in PHC involves collaboration with a team including specialist professionals (Ambuel et al., 2013; Briones-Vozmediano et al., 2022; Dowrick et al., 2020; Eismann et al., 2019; Ford-Gilboe et al., 2011; Hegarty et al., 2020; Lam et al., 2020; Martin-Engel et al., 2021; Mohd Mydin et al., 2022; Nicolaidis & Touhouliotis, 2006; Szilassy et al., 2017, 2021; Turner et al., 2017). Several providers comprise the PHC workforce supporting survivors and families of FV, including general practitioners, nurses, midwives, psychologists, and social workers. Social workers can provide both psychosocial and legal support to survivors (Eismann et al., 2019; Gear et al., 2016; Lam et al., 2020), which can enhance broader care experiences for survivors. Nurses are often viewed as the most trusted and closest to the patient and their community and can support greatly with identification and management of FV (Miller & Jaye, 2007; Mohd Mydin et al., 2022).
Interventions to improve PHC teams’ response to FV should focus on strengthening a team’s self-efficacy and perceived preparation. Goicolea et al. (2015) conduced a multiple case study analysis involving 15 PHC teams located in four different Spanish regions and found that providers achieved a sense of self-confidence and self-efficacy through their daily engagement with a team of professionals who were highly committed to addressing domestic violence and abuse. In this study, monthly group meetings where providers would debrief about their experiences of addressing domestic violence and abuse in the workplace, including discussion of their feelings about dealing with domestic violence and abuse, increased the team’s self-confidence to identify and assess for violence and abuse among patients (Goicolea et al., 2015). Furthermore, the authors of this study explain that safe spaces for reflection and case discussion and the presence of experienced providers facilitate team learning and contribute to increased self-confidence in less-experienced providers (Goicolea et al., 2015).
Readiness to address FV was enhanced not only through having a supportive team environment, but from collaborating with specialist FV professionals. This was particularly true for clinicians in general practice settings in the UK who had access to a specialist domestic violence and abuse advocate through the IRIS program (Bradbury-Jones et al., 2017; Dowrick et al., 2020; Feder et al., 2011). Several studies highlighted the expansive benefits from having formalized collaborations with community agencies, as this can raise awareness of community resources (Ambuel et al., 2013; Chappell et al., 2021; Nicolaidis & Touhouliotis, 2006), build relationships for further referrals and enable patient advocacy (Martin-Engel et al., 2021). Staff at community agencies (e.g., social workers, community health workers, peer support staff) can help address a survivor or their families’ psychosocial concerns and connect them to resources, including local support groups (Eismann et al., 2019; Ford-Gilboe et al., 2011). Engaging FV specialists, natural helpers (e.g., knowledge holders and Elders within the communities) (Rizkalla et al., 2020), community advocates and champions with provider teams (Ambuel et al., 2013; Bradbury-Jones et al., 2017; Dowrick et al., 2020), and case managers (Nicolaidis & Touhouliotis, 2006) can also help reduce anxiety for general practitioners and nurses about broaching topics of violence and abuse, especially with the limited time, resources, and training they have to address FV concerns within their practice.
Several articles described how clinicians feel incapable of responding to FV due to work overload, which is further exacerbated by insufficient staffing and staff turnover (Briones-Vozmediano et al., 2022; Giraldo-Rodríguez & Agudelo-Botero, 2022). Time constraints were also mentioned as another barrier to broaching topics of violence and further addressing FV (Ambikile et al., 2020; Eismann et al., 2019; Goicolea et al., 2015; Ibrahim et al., 2021; Klause et al., 2020; Miller & Jaye, 2007; Mohd Mydin & Othman, 2020; Mohd Mydin et al., 2022; Mork et al., 2014; Nicolaidis & Touhouliotis, 2006; Ruiz-Perez et al., 2018; Soglin et al., 2009). It was noted that reporting abuse concerns remains time-consuming and inefficient, which limits the time available to support survivors more directly (Chappell et al., 2021). Thus, having a social worker or advocate worker embedded in the PHC team opens new opportunity for more comprehensive services as physician appointments may be too short to address many social issues (Goicolea et al., 2019; Rizkalla et al., 2020).
Nicolaidis and Touhouliotis (2006) explored how the Chronic Care Model, a widely known framework for improving chronic illness management, can guide comprehensive approaches to health care delivery for intimate partner survivors, which emphasize coordinated interdisciplinary team practice within primary care. Moreover, Goicolea et al. (2015) explained that the core components of a PHC model – holistic care, continuity of care, coordination with other health care services and other sectors (i.e., education, social services), a family approach and community orientation – encourages multidisciplinary teamwork and thus, better prepares professionals in PHC practices to respond to FV.
Improving Provider Knowledge on the Social and Cultural Determinants Impacting FV
Findings across studies described how a clinician’s response to cases of FV seen within their practice is shaped by their knowledge, attitudes, and perceived preparedness. Taskiran et al. (2019) conducted a cross-sectional study of 129 family physicians and 137 midwives/nurses in Turkey to examine their perceptions about their responses to women disclosing physical, verbal, or sexual violence. The authors found that the disclosure of IPV in PHC is very high, but more than one-third of physicians and half of midwives/nurses respond inappropriately (Taskiran et al., 2019). The reasons for their inappropriate responses varied from 36% of respondents believing that the woman would continue to live with their abuser, 18% felt they had limited knowledge in detecting violence, 6.8% reported a lack of knowledge in referral process, and 2.2% did not think clinicians recording or reporting violence would make a difference (Taskiran et al., 2019). The authors of this study explain that the reasoning behind this behavior may be a result of societal and cultural norms on gender roles. As this study explored the actions of PHC workers in the case of a disclosure, not screening practices, the authors conclude that the patriarchal and traditionalist structure in Turkey may influence women’s motivations to disclose (Taskiran et al., 2019). Similarly, research by Ibrahim et al. (2021) expressed how women within middle eastern cultures are expected to not disclose IPV to others, including their health care providers. As a result, it is also rare for providers to intervene in cases of IPV, with two thirds of providers who participated in this study believing it to not be part of their medical responsibility (Ibrahim et al., 2021). The article by Colombini et al. (Colombini et al., 2020) also argued that there is a “culture of silence” surrounding domestic violence within the community, with survivors being blamed for the abuse.
Within different cultural contexts, scholars have promoted the adoption of culturally safe FV interventions that support clinicians’ understanding of the social and cultural determinants impacting FV (Colombini et al., 2020; Ibrahim et al., 2021). Scholars also stressed the importance of health care professionals having a neutral and non-judgmental attitude when responding to survivors of family or domestic violence (Briones-Vozmediano et al., 2022; Lam et al., 2020; Mork et al., 2014; Ramsay et al., 2012). In one study involving focus group interviews with PHC providers in Hong Kong, China, the authors reported that long-term trust established with the patient and the family and taking the time to listen to patients express their feelings, could facilitate the process of recognizing and managing suspected cases of domestic violence (Lam et al., 2020). Ruiz-Perez et al. (2018) described how provider’s having an “active attitude” in case detection and referral helped women feel safe and supported to disclose. Moreover, Gear et al. (2019) conducted interviews with 17 PHC professionals, including clinicians and practice managers, in New Zealand PHC settings and highlighted that many participants had inadequate understanding of the relationship between health care and the socioecological contexts in which violence occurs, preventing an understanding of IPV as a key determinant of ill-health, and thus resisting the PHC system’s response to address the health effects of IPV.
Study findings also demonstrated variation in beliefs and attitudes towards FV within a PHC team and across the broader PHC sector (Hegarty et al., 2020; Ramsay et al., 2012). Ramsay et al. (2012) administered the PREMIS survey to 82 general practices located in two urban primary care trust areas in the UK who were participating in the IRIS program trial, to examine perceived preparation and perceived knowledge of domestic violence among general practitioners and nurses. These general practices all used electronic records and were serving culturally and ethnically diverse patient populations. Prior to implementing the IRIS program, the PREMIS survey was completed by 183 general practitioners and 89 practice nurses (Ramsay et al., 2012). The survey results showed that general practitioners had a greater understanding of the woman’s social circumstances than nurses (Ramsay et al., 2012). Other studies described that social workers and nurses had more favourable attitudes to support survivors, compared to physicians (Goicolea et al., 2019; Ibrahim et al., 2021). Qualitative interviews with PHC physicians in Malaysia found that physicians were worried that asking their patients about elder abuse and neglect would affect the doctor-patient relationship and that such issues should be passed to social workers (Mohd Mydin & Othman, 2020). Briones-Vozmediano et al. (2022) conducted qualitative interviews with nurses from 27 PHC centres in Spain and found that nurses felt their primary role in responding to IPV is detecting and attending to cases, which could include physical examinations, treating injuries and bruises if necessary, giving information on available resources, offering emotional support, referring patients to the most appropriate professional according to the case, and empowering patients. Conversely, findings from a self-administered questionnaire to nurses and midwives in Tanzania showed they had insufficient knowledge and poor attitudes to provide culturally competent care to IPV survivors in the country, which was largely impacted by lack of opportunity to complete IPV training (Ambikile et al., 2020). Additionally, a qualitative study conducted in Ontario, Canada reported on the obstacles conveyed by PHC providers when supporting Indigenous women who experience IPV, which are shaped by their awareness of First Nations culture and history of colonization, and fear of being perceived as culturally inappropriate or judgmental when asking Indigenous women about their experience with FV (Rizkalla et al., 2020).
Studies that offered intensive training programs to PHC providers found significant changes in both knowledge and attitudes towards violence and abuse post-intervention (Ambuel et al., 2013; Miller & Jaye, 2007; Mohd Mydin & Othman, 2020; Mohd Mydin et al., 2022; Mork et al., 2014; Papadakaki et al., 2013; Turner et al., 2017), enabling them to become emotionally equipped to identify and respond to FV. Twenty-three articles focused on enhancing provider training and education to increase identification of FV and referral pathways for survivors (Chappell et al., 2021; Eismann et al., 2019; Gear et al., 2021; Goicolea et al., 2015; Joyner & Mash, 2012; Klause et al., 2020; Lam et al., 2020; Lo Fo Wong et al., 2007; Martin-Engel et al., 2021; Miller & Jaye, 2007; Mohd Mydin & Othman, 2020; Mohd Mydin et al., 2022; Mork et al., 2014; Mydin et al., 2021; Papadakaki et al., 2013; Pokharel et al., 2021; Rizkalla et al., 2020; Ruiz-Perez et al., 2018; Soglin et al., 2009; Szilassy et al., 2017; Taskiran et al., 2019; Taylor et al., 2006; Turner et al., 2017). The findings from the studies show variation in the outcomes from training and education. In the studies that focused on the implementation of the IRIS program, the training sessions showed increased identification of domestic violence and increased referrals to local domestic violence agencies (Bradbury-Jones et al., 2017; Feder et al., 2011). One study examining a physician-oriented educational intervention involving two 1-h didactic sessions on IPV and regular emails with IPV information did not result in increased IPV identification from the baseline assessments (Soglin et al., 2009). Building on the previous theme, scholars have argued that training for FV needs to be considered within comprehensive approaches to FV response within PHC that not only include training, but incorporate information resources for patient education, screening tools for the identification of FV, referral pathways to services and supports, and links to community agencies with specialized knowledge on FV for adequate support for patients and their families experiencing violence, including survivors (Chappell et al., 2021).
While some training interventions have been implemented in health care settings globally, the quality and reach of training opportunities for different providers working within PHC is variable. Several articles highlighted that the professional scope of training interventions or programs should expand to include broader health care teams and allied health care professionals (Feder et al., 2011; Klause et al., 2020; Mohd Mydin & Othman, 2020; Mydin et al., 2021; Soglin et al., 2009). While some articles focused on delivering training to PHC providers and/or medical residents (Eismann et al., 2019; Feder et al., 2011; Lam et al., 2020; Wong et al., 2007; Miller & Jaye, 2007; Mohd Mydin & Othman, 2020; Mork et al., 2014; Papadakaki et al., 2013; Soglin et al., 2009), others focused on delivering training to registered nurses and nurse practitioners working in PHC settings (Klause et al., 2020) and some offered training intended for a mix of health care providers (Martin-Engel et al., 2021; Mohd Mydin et al., 2022; Szilassy et al., 2021; Turner et al., 2017). However, findings from the implementation of the IRIS + training program demonstrated that the training was helpful for physicians but not relevant for practice nurses and nurse practitioners, and also failed to reach allied health professionals working within PHC (Szilassy et al., 2021). Three articles shared the need for tailored, ongoing FV training to continuously improve knowledge, education, and awareness of FV risk factors for all health care providers (Lam et al., 2020; Wong et al., 2007). Furthermore, ensuring FV training programs address cultural competency and are linked to specialized knowledge and resources within community agencies or advocacy organizations are key to facilitating providers’ approaches to care with survivors (Chibber et al., 2011; Ford-Gilboe et al., 2011; Gear et al., 2019; Ibrahim et al., 2021; Pokharel et al., 2021; Rizkalla et al., 2020).
Embedding System-Level Supports for Providers in PHC
Several studies included in this review described system-level gaps affecting FV identification and response (Ambikile et al., 2020; Ambuel et al., 2013; Briones-Vozmediano et al., 2022; García-Quinto et al., 2022; Gear et al., 2021; Gear et al., 2016; Goicolea et al., 2019; Nicolaidis & Touhouliotis, 2006; Papadakaki et al., 2013; Taskiran et al., 2019). PHC providers in these studies shared that their health care facilities lacked strategic policies and protocols on when to screen their patients for FV (including elder and child abuse) and how to effectively respond (Ambikile et al., 2020; Briones-Vozmediano et al., 2022; Clark et al., 2020; Colombini et al., 2020; Gear et al., 2019; Lam et al., 2020; Mohd Mydin & Othman, 2020; Mohd Mydin et al., 2022; Ramsay et al., 2012). This results in uncertainty and doubt among providers in knowing what to do if a patient is experiencing or at-risk of violence and abuse (Gear et al., 2019). One article highlighted that while clinicians desire to support survivors, it would be helpful for them to know what questions to ask and have guidelines to follow for screening and referral processes (Colombini et al., 2020). Research by Martin-Engel et al. (2021) described how the health centers in their study emphasized specific, actionable clinic policies for FV identification and referral to community agencies, which contributed towards clinicians having greater confidence when supporting survivors in their practice.
The use of a protocol was perceived by PHC providers to influence their motivation to respond to FV (Ambuel et al., 2013; Joyner & Mash, 2012; Lam et al., 2020; Mohd Mydin & Othman, 2020; Mohd Mydin et al., 2022). Goicolea et al. (2015) found that among PHC teams that used a protocol this provided a guide for “essential” actions on responding to domestic violence to be carried out and the roles of different team members. The use of a protocol was described to reduce uncertainty and increased self-confidence and self-efficacy among PHC providers. Thus, the authors highlighted that where self-efficacy was high among PHC teams this contributed to a positive response to domestic violence, while professionals or teams who felt ill prepared, responses were poorer (Goicolea et al., 2015). In Ramsay et al.’s (2012) article, 43.8% of clinicians who responded to the survey reported that there was no protocol for dealing with domestic violence in their practice, which may have improved the management of women experiencing abuse. The authors conclude that the absence of protocols in most of the general practice settings may have contributed to the low identification rate and number of cases being referred to local domestic violence advocacy services. Two studies mentioned that while international guidelines for addressing FV have been established, they are not always embedded in clinic policies (Ambuel et al., 2013; Gear et al., 2021). Joyner and Mash (2012) established a co-operative inquiry group to support implementation of an IPV screening and management protocol in both rural and urban settings. The group drew on the four-step action research cycle: planning, action, observation, and reflection to work collectively on identifying the barriers associated with IPV screening and management within their practice, creating new knowledge from their experience, and conceptualizing their learning (Joyner & Mash, 2012). Over a fourteen-month period, the team adapted the protocol to develop a comprehensive model of care, including connections to community-based support groups (Joyner & Mash, 2012).
Research has demonstrated the importance of embedding system-level supports in FV interventions (Ambuel et al., 2013; Dowrick et al., 2020; Eismann et al., 2019; Feder et al., 2011). The well-established evidence on the IRIS training and support intervention has demonstrated the effectiveness of integrated, system-level interventions that include an on-site domestic violence advocacy worker and referral pathway (Bradbury-Jones et al., 2017; Feder et al., 2011; Szilassy et al., 2021). The success of the SEEK model for addressing psychosocial risk factors for maltreatment across multiple primary care settings in the USA, has been attributed to embedded on-site support staff to assist with communication and referrals to services for caregivers and training for child health care professionals on addressing targeted psychosocial risk factors. Ambuel et al. (2013) also describes that changes need to occur at the system level before individual providers can effectively implement their knowledge and skills related to IPV detection, prevention, and intervention. They developed the Health care Can Change from Within (HCCW) intervention model to bring about change at multiple levels of the health care system including individual clinicians and clinical staff, clinical environment (policies, procedures, patient education), and clinical culture (Ambuel et al., 2013).
Discussion
This rapid evidence assessment identified effective FV interventions using a multi-component comprehensive approach within PHC settings and the factors that shape PHC readiness to integrate FV interventions into routine care. The review identified rigorous research studies examining the implementation outcomes of different FV interventions or programs within varied PHC settings (e.g., rural, urban, or inner-city centres) and serving diverse patient population groups. These interventions were implemented in Canada, USA, UK and South Africa, and involve multiple components including multidisciplinary teamwork; improving provider knowledge and understanding of the social and cultural determinants of FV; provider education and training; system supports including domestic violence or IPV champions or advocates, FV protocols and guidelines; and advocacy strategies for survivors. Also, the FV interventions included in the review focused primarily on supporting female patients experiencing violence and/or female survivors. There is a dearth of empirically tested FV interventions that focus on men, children, and perpetrators. Clinicians often do not recognize men to be affected by violence (Huntley et al., 2019), and there is little research evidence on effective FV interventions for men in health care settings at large (Akoensi et al., 2013; Gondolf, 2012). There is also uncertainty about the health care response to FV when children are affected (Drinkwater et al., 2017; Larkins et al., 2015), and about the effectiveness and cost-effectiveness of interventions to improve health care responses to children experiencing violence and abuse in the home (Howarth et al., 2016). There is also a lack of evidence to support the effectiveness of interventions to support healing and recovery following sexual violence, particularly over time.
FV interventions in health care settings that have emphasized training clinicians on how to recognize signs and respond to FV, have shown limited effect on identification of patients experiencing FV and on referral for further support (Minsky-Kelly et al., 2005). Research that suggests training may improve PHC providers FV knowledge and their self‐perceived readiness to respond to those affected by violence (Kalra et al., 2021). Findings from this review also show inconsistent evidence that FV training alone may improve PHC providers’ knowledge and attitudes towards FV. Moreover, the sustained effect of training on these outcomes are also unclear from this review. For longer-term interventions, the most promising results have been from interventions with a systems-based approach to FV that incorporate advocacy supports, focus on empowerment, and referral to services and resources, alongside provider training and education (Miller et al., 2015). Research supports the potential benefits of advocacy support for family members who have experienced violence and validates the knowledge and expertise that lay advocates and FV specialists provide within a larger system of services. For instance, the IRIS program in the UK is a well-studied domestic violence intervention that focuses on integrated training among physicians with system-level supports in a PHC setting. A central component of this intervention is the incorporation of the specialist domestic violence and abuse (DVA) advocate within PHC clinics who deliver training and support to general practitioners and provide advocacy to patients experiencing violence or abuse who are referred by general practitioners. The program also established a structured connection between family physicians and DVA advocates.
Several readiness tools or guiding models to assess PHC provider or health care teams’ readiness to respond to violence and abuse were identified from the review. The PREMIS tool is the most cross-culturally adapted instrument across various countries and is promising for assessing PHC providers’ readiness to respond to IPV. It is the most frequently examined instrument originally developed in the USA by Short et al. (2006). The tool quantitatively measures readiness in terms of preparedness, knowledge, opinions, and practices regarding IPV. Moreover, the tool has also been tested among different health care professionals aside from clinicians, including pharmacists (Barnard et al., 2018), nurses (Blumling et al., 2018), perinatal care providers (Guiguet-Auclair et al., 2021), as well as in health care settings other than PHC. The articles that were identified from this review had evaluated the tool in PHC settings in Spain and Greece and demonstrated internal consistency, content validity and reliability of the tool. Other readiness assessment tools identified from the review not only assesses health care providers’ readiness to respond to IPV in terms of their knowledge and awareness, but also by determining the training needs of providers (Alsalman et al., 2023) and enabling factors such as the collaborative team environment (Renner et al., 2021). Differences were reported across studies on the attitudes of PHC providers towards responding to FV. For instance, Ramsay et al. (2012) found that physicians reported a positive attitude towards responding to FV compared to practice nurses, whereas Goicolea et al., 2019 reported that social workers and nurses had more favourable attitudes to support survivors. A recent systematic review has been conducted on the measurement tools for assessing health care providers’ readiness to respond to IPV in a variety of health care settings, similarly concluded that the PREMIS tool is the most widely used measure for assessing health care providers’ readiness to respond to IPV (Ying Ying et al., 2023). The search results from this review did not identify studies incorporating virtual or remote-based FV interventions within PHC that encompass multiple components beyond identification and assessment. Given the prevalence of virtual PHC delivery post-pandemic, future research is needed to study how virtual or remote-based delivery within PHC practices impacts provider and organization readiness to identify and support patients affected by FV; as well as test for feasibility and acceptability of evidence-based interventions identified from this review in the virtual environment. Furthermore, the findings from this rapid evidence assessment highlight a paucity of research on readiness measurement tools that evaluate ‘system-level’ factors related to the PHC context that shape provider and organization readiness to respond to FV.
Efforts to improve the FV response in PHC have largely focused on individual-level change. What is required to guide PHC practice is a closer examination of existing organizational practices and the broader PHC system that shape providers’ increased feelings of preparedness and self-confidence, as well as decreased feelings of anxiety when responding to FV. Rather than solely focusing on increasing individual provider knowledge, organizations, as well as the greater system, should ensure the fundamental conditions that allow providers to confidently respond to FV (Loncar & Scott, 2023). For instance, having clear guidelines or protocols, regular training, embedded domestic violence advocates or peer support workers to bridge connections to community resources, and an overall prioritization of FV as a key healthcare issue. This is in line with the World Health Organization’s current guidelines for the health sectors’ response to violence against women that suggest that training of individual providers needs to be supported by wider systemic changes (WHO, 2019).
The findings also revealed system considerations for sustaining FV interventions in PHC. PHC providers have a crucial role to play in addressing FV but are often lacking the resources, support, or confidence to identify and respond to families affected by violence. Research has demonstrated that organizational change in health care is challenging, but that certain types of activities are more likely to result in longer-term change. Organizational change that focuses on collective action (the work that people do with each other, clarification of roles and resources) and reflexive monitoring (appraisal/feedback of the activities that are carried out) have been found to be most effective (Babiker et al., 2014) compared to change that focus solely on individuals. According to Weiner et al. (2008), an organization’s readiness relies on organization members’ motivation to change (change commitment) and belief in their own capacity to change (change efficacy). Studies that emphasized collaboration and engagement with a multidisciplinary team (e.g., regular group meetings and reflections) reported to facilitate the team’s learning and improve providers’ self-efficacy and self-confidence to respond to FV. Furthermore, predisposing factors such as provider attitude towards survivors of FV (Hegarty et al., 2020; Ruiz-Perez et al., 2018) and enabling contextual factors such as the organization and team environment also ensure support for the identification and assessment of FV within clinical practice. Other contextual consideration shaping provider and organization readiness that were seldom discussed in the literature is the location of the PHC clinic and patient population being served.
Moreover, the findings from this review highlighted the importance of a social determinant of health and equity perspective, which is central to a strong PHC approach, in designing FV interventions that incorporate an understanding of diversity among patients, and that foster continuity of relationships across service sectors to help families navigate complex systems (Ford-Gilboe et al., 2011). Findings from empirical studies included in this review also demonstrated how an understanding of a person’s varied social locations and cultural background can impact provider behavior on FV (Ibrahim et al., 2021; Rizkalla et al., 2020). There is more to professional ‘competency’ in tackling complex social problems than simply acknowledging diversity and holding a non-judgmental attitude (although these are undoubtedly important, see Hegarty et al., 2020). Instead, an awareness of the structural factors which enable and perpetuate inequalities is integral to being able to address them. Only one study examined PHC providers’ preparedness to support Indigenous women who experience IPV (Rizkalla et al., 2020). The paucity of Indigenous-focused FV intervention in PHC was an identified gap in this review.
Strengths and Limitations
The rapid evidence assessment has several strengths and limitations. We attempted to include all relevant articles through multiple literature search strategies: database searches, manual reference list searches, and searching references identified in included sources. We minimized bias with at least two reviewers independently conducting all stages of this review. However, this review is language-restricted and only included studies published in English language. Also, this review was based solely upon peer-reviewed literature. A strength of this review was an examination of comprehensive FV interventions within PHC, and identification of effective system-based strategies in enhancing PHC provider and organization readiness, and under which circumstances.
Conclusion
FV is a serious public health concern and PHC providers have a vital role in early detection of FV and the poor health outcomes associated with violence. A systems-based approach to service delivery alongside interventions that incorporated training and education, on-site FV resources including the role of advocates or champions, practice guidelines and protocols, and referral to supports has been advocated to support sustainable FV responses within PHC settings. Echoing previously published findings, we found that several factors shape PHC providers readiness to respond to FV, including provider knowledge, attitudes and beliefs, embedded support workers in the PHC team, and availability of training opportunities. A focus on comprehensive or multi-component FV interventions would allow for safe, confident, and professional identification and assessment of FV within PHC.
Data Availability
All data created during this research is available upon request.
References
Afifi, T. O., MacMillan, H., Cox, B. J., Asmundson, G. J., Stein, M. B., & Sareen, J. (2009). Mental health correlates of intimate partner violence in marital relationships in a nationally representative sample of males and females. Journal of Interpersonal Violence, 24(8), 1398–1417. https://doi.org/10.1177/0886260508322192
Akoensi, T. D., Koehler, J. A., Lösel, F., & Humphreys, D. K. (2013). Domestic violence perpetrator programs in Europe, Part II: A systematic review of the state of evidence. International Journal of Offender Therapy and Comparative Criminology, 57(10), 1206–1225. https://doi.org/10.1177/0306624x12468110
*Alsalman, Z., Shafey, M., & Al Ali, L. (2023). Intimate Partner Violence; Are Saudi Physicians in Primary Health Care Setting Ready to Identify, Screening, and Respond? International Journal of Women's Health, 15, 623-633. https://doi.org/10.2147/ijwh.S401926
*Ambikile, J. S., Leshabari, S., & Ohnishi, M. (2020). Knowledge, attitude, and preparedness toward IPV care provision among nurses and midwives in Tanzania. Human Resources for Health, 18(1), 56.https://doi.org/10.1186/s12960-020-00499-3
*Ambuel, B., Hamberger, L., Guse, C., Melzer-Lange, M., Phelan, M., & Kistner, A. (2013). Health care Can Change from Within: Sustained Improvement in the Health care Response to Intimate Partner Violence. Journal of Family Violence, 28(8), 833-847.https://doi.org/10.1007/s10896-013-9550-9
Arias, I., & Corso, P. (2005). Average cost per person victimized by an intimate partner of the opposite gender: A comparison of men and women. Violence and Victims, 20(4), 379–391.
Babiker, A., El Husseini, M., Al Nemri, A., Al Frayh, A., Al Juryyan, N., Faki, M. O., Assiri, A., Al Saadi, M., Shaikh, F., & Al Zamil, F. (2014). Health care professional development: Working as a team to improve patient care. Sudanese Journal of Paediatrics, 14(2), 9–16.
Barnard, M., West-Strum, D., Yang, Y., & Holmes, E. (2018). Evaluation of a Tool to Measure Pharmacists' Readiness to Manage Intimate Partner Violence. Pharmacy (Basel), 6(3). https://doi.org/10.3390/pharmacy6030066
Baum, F., Freeman, T., Lawless, A., Labonte, R., & Sanders, D. (2017). What is the difference between comprehensive and selective primary health care? Evidence from a five-year longitudinal realist case study in South Australia. British Medical Journal Open, 7(4), e015271. https://doi.org/10.1136/bmjopen-2016-015271
Benbow, S. M., Bhattacharyya, S., & Kingston, P. (2018). What’s in a name? Family violence involving older adults. Journal of Adult Protection, 20(5), 187–192. https://doi.org/10.1108/JAP-08-2018-0016
Beynon, C. E., Gutmanis, I. A., Tutty, L. M., Wathen, C. N., & MacMillan, H. L. (2012). Why physicians and nurses ask (or don’t) about partner violence: A qualitative analysis. BMC Public Health, 12(1), 473. https://doi.org/10.1186/1471-2458-12-473
Blumling, A., Kameg, K., Cline, T., Szpak, J., & Koller, C. (2018). Evaluation of a Standardized Patient Simulation on Undergraduate Nursing Students’ Knowledge and Confidence Pertaining to Intimate Partner Violence. Journal of Forensic Nursing, 14(3), 174–179. https://doi.org/10.1097/jfn.0000000000000212
Bonomi, A. E., Anderson, M. L., Rivara, F. P., & Thompson, R. S. (2009). Health care utilization and costs associated with physical and nonphysical-only intimate partner violence. Health Services Research, 44(3), 1052–1067. https://doi.org/10.1111/j.1475-6773.2009.00955.x
*Bradbury-Jones, C., Clark, M., & Taylor, J. (2017). Abused women's experiences of a primary care identification and referral intervention: a case study analysis. Journal of advanced nursing, 73(12), 3189-319https://doi.org/10.1111/jan.13250
Bradley, N. L., DiPasquale, A. M., Dillabough, K., & Schneider, P. S. (2020). Health care practitioners’ responsibility to address intimate partner violence related to the COVID-19 pandemic. CMAJ, 192(22), E609-e610. https://doi.org/10.1503/cmaj.200634
Breiding, M. J., Chen, J., & Black, M. C. (2014). Intimate Partner Violence in the United States - 2010. https://www.cdc.gov/violenceprevention/pdf/cdc_nisvs_ipv_report_2013_v17_single_a.pdf. Accessed 8 May 2023.
*Briones-Vozmediano, E., Otero-Garcia, L., Gea-Sanchez, M., De Fuentes, S., Garcia-Quinto, M., Vives-Cases, C., & Maquibar, A. (2022). A qualitative content analysis of nurses' perceptions about readiness to manage intimate partner violence. Journal of advanced nursing, 78(5), 1448-1460.https://doi.org/10.1111/jan.15119
Brownridge, D. A. (2008). Understanding the Elevated Risk of Partner Violence Against Aboriginal Women: A Comparison of Two Nationally Representative Surveys of Canada. Journal of Family Violence, 23(5), 353–367. https://doi.org/10.1007/s10896-008-9160-0
Burczycka, M., & Conroy, S. (2018). Family violence in Canada: A statistical profile, 2016. https://www150.statcan.gc.ca/n1/en/pub/85-002-x/2018001/article/54893-eng.pdf?st=2L7zV0K0
Basile, K. C., Smith, S. G., Kresnow, M., Khatiwada, S, & Leemis, RW. (2022). The national intimate partner and sexual violence survey: 2016/2017 report on sexual violence. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
*Chappell, K. K., Hein, L. C., & Andrews, J. O. (2021). Can We Ask Everyone? Addressing Sexual Abuse in Primary Care. Journal for Nurse Practitioners, 17(5), 594-599. https://doi.org/10.1016/j.nurpra.2021.01.017
*Chibber, K. S., Krishnan, S., & Minkler, M. (2011). Physician practices in response to intimate partner violence in southern India: insights from a qualitative study. Women & health, 51(2), 168-185. https://doi.org/10.1080/03630242.2010.550993
*Clark, C. J., Renner, L. M., & Logeais, M. E. (2020). Intimate Partner Violence Screening and Referral Practices in an Outpatient Care Setting. Journal of Interpersonal Violence, 35(23-24), 5877-5888. https://doi.org/10.1177/0886260517724253
*Colombini, M., Alkaiyat, A., Shaheen, A., Moreno, C. G., Feder, G., Bacchus, L., & Garcia Moreno, C. (2020). Exploring health system readiness for adopting interventions to address intimate partner violence: a case study from the occupied Palestinian Territory. Health Policy & Planning, 35(3), 245-256. https://doi.org/10.1093/heapol/czz151
*Dowrick, A., Kelly, M., & Feder, G. (2020). Boundary spanners: Negotiating connections across primary care and domestic violence and abuse services. Social science & medicine (1982), 245(ut9, 8303205), 112687. https://doi.org/10.1016/j.socscimed.2019.112687
Drinkwater, J., Stanley, N., Szilassy, E., Larkins, C., Hester, M., & Feder, G. (2017). Juggling confidentiality and safety: A qualitative study of how general practice clinicians document domestic violence in families with children. British Journal of General Practice, 67(659), e437–e444. https://doi.org/10.3399/bjgp17X689353
*Eismann, E. A., Theuerling, J., Maguire, S., Hente, E. A., & Shapiro, R. A. (2019). Integration of the Safe Environment for Every Kid (SEEK) Model Across Primary Care Settings. Clinical pediatrics, 58(2), 166-176. https://doi.org/10.1177/0009922818809481
*Feder, G., Davies, R. A., Baird, K., Dunne, D., Eldridge, S., Griffiths, C., Gregory, A., Howell, A., Johnson, M., Ramsay, J., Rutterford, C., & Sharp, D. (2011). Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: a cluster randomised controlled trial. Lancet, 378(9805), 1788-1795https://doi.org/10.1016/s0140-6736(11)61179-3
Finfgeld-Connett, D. (2013). Use of content analysis to conduct knowledge-building and theory-generating qualitative systematic reviews. Qualitative Research, 14(3), 341–352. https://doi.org/10.1177/1468794113481790
Fiolet, R., Tarzia, L., Hameed, M., & Hegarty, K. (2021). Indigenous Peoples’ Help-Seeking Behaviors for Family Violence: A Scoping Review. Trauma, Violence & Abuse, 22(2), 370–380. https://doi.org/10.1177/1524838019852638
*Ford-Gilboe, M., Merritt-Gray, M., Varcoe, C., & Wuest, J. (2011). A theory-based primary health care intervention for women who have left abusive partners. Advances in Nursing Science, 34(3), 198-214. https://doi.org/10.1097/ANS.0b013e3182228cdc
*García‐Quinto, M., Briones‐Vozmediano, E., Otero‐García, L., Goicolea, I., & Vives‐Cases, C. (2022). Social workers' perspectives on barriers and facilitators in responding to intimate partner violence in primary health care in Spain. Health & Social Care in the Community, 30(1), 102-113. https://doi.org/10.1111/hsc.13377
Gear, C., Koziol-McLain, J., Wilson, D., Rae, N., Samuel, H., Clark, F., & McNeill, E. (2012). Primary health care response to family violence: A Delphi evaluation tool. Quality in Primary Care, 20(1), 15–30.
*Gear, C., Koziol-McLain, J., Wilson, D., & Clark, F. (2016). Developing a response to family violence in primary health care: the New Zealand experience. BMC Fam Pract, 17(1), 115https://doi.org/10.1186/s12875-016-0508-x
*Gear, C., Eppel, E., & Koziol-Mclain, J. (2018). Exploring the complex pathway of the primary health care response to intimate partner violence in New Zealand. Health research policy and systems, 16(1), 99.https://doi.org/10.1186/s12961-018-0373-2
*Gear, C., Koziol-Mclain, J., & Eppel, E. (2019). Exploring sustainable primary care responses to intimate partner violence in New Zealand: Qualitative use of complexity theory. BMJ open, 9(11), e031827 https://doi.org/10.1136/bmjopen-2019-031827
*Gear, C., Koziol-McLain, J., & Eppel, E. (2021). Engaging with Uncertainty and Complexity: A Secondary Analysis of Primary Care Responses to Intimate Partner Violence. Global qualitative nursing research, 8(101666563), 2333393621995164https://doi.org/10.1177/2333393621995164
*Giraldo-Rodríguez, L., & Agudelo-Botero, M. (2022). Barriers to managing elder abuse in primary care services: experiences of health care providers in Mexico City. Journal of Elder Abuse & Neglect, 34(1), 38-55.https://doi.org/10.1080/08946566.2021.2016534
Glasgow, R. E., Vogt, T. M., & Boles, S. M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health., 89(9), 1322–1327.
*Goicolea, I., Hurtig, A.-K., San Sebastian, M., Vives-Cases, C., & Marchal, B. (2015). Developing a programme theory to explain how primary health care teams learn to respond to intimate partner violence: a realist case-study. BMC Health Services Research, 15(101088677), 228.https://doi.org/10.1186/s12913-015-0899-8
Goicolea, I., Mosquera, P., Briones-Vozmediano, E., Otero-García, L., García-Quinto, M., & Vives-Cases, C. (2017). Primary health care attributes and responses to intimate partner violence in Spain. Gaceta sanitaria, 31, 187–193.
*Goicolea, I., Marchal, B., Hurtig, A.-K., Vives-Cases, C., Briones-Vozmediano, E., & San Sebastian, M. (2019). Why do certain primary health care teams respond better to intimate partner violence than others? A multiple case study. Gaceta sanitaria, 33(2), 169-176https://doi.org/10.1016/j.gaceta.2017.10.005
Gondolf, E. W. (2012). The future of batterer programs: Reassessing evidence-based practice. Northeastern University Press. pp 1–317.
Guedes, A., Bott, S., Garcia-Moreno, C., & Colombini, M. (2016). Bridging the gaps: A global review of intersections of violence against women and violence against children. Global Health Action, 9, 31516. https://doi.org/10.3402/gha.v9.31516
Guiguet-Auclair, C., Debost-Legrand, A., Lémery, D., Barasinski, C., Mulin, B., & Vendittelli, F. (2021). Measuring the readiness to screen and manage intimate partner violence: Cross-cultural adaptation and psychometric evaluation of the PREMIS tool for perinatal care providers. PLoS ONE, 16(11), e0258943. https://doi.org/10.1371/journal.pone.0258943
*Hamberger, L., Ambuel, B., Guse, C., Phelan, M., Melzer-Lange, M., & Kistner, A. (2014). Effects of a Systems Change Model to Respond to Patients Experiencing Partner Violence in Primary Care Medical Settings. Journal of Family Violence, 29(6), 581-594.https://doi.org/10.1007/s10896-014-9616-3
Hayes, B., & Kopp, P. (2019). Gender Differences in the Effect of Past Year Victimization on Self-Reported Physical and Mental Health: Findings from the 2010 National Intimate Partner and Sexual Violence Survey. American Journal of Criminal Justice, 45. https://doi.org/10.1007/s12103-019-09510-7
*Hegarty, K. , McKibbin, G., Hameed, M., Koziol-McLain, J., Feder, G., Tarzia, L., & Hooker, L. (2020). Health practitioners' readiness to address domestic violence and abuse: A qualitative meta-synthesis. PLoS One, 15(6), e0234067. https://doi.org/10.1371/journal.pone.0234067
Heidinger, L. (2018). Intimate partner violence: Experiences of First Nations, Métis and Inuit women in Canada, 2018. https://www150.statcan.gc.ca/n1/pub/85-002-x/2022001/article/00004-eng.htm. Accessed 8 May 2023.
Hoelle, R. M., Elie, M. C., Weeks, E., Hardt, N., Hou, W., Yan, H., & Carden, D. (2015). Evaluation of health care use trends of high-risk female intimate partner violence victims. The Western Journal of Emergency Medicine, 16(1), 107–113. https://doi.org/10.5811/westjem.2014.12.22866
Hooker, L., Versteegh, L., Lindgren, H., & Taft, A. (2020). Differences in help-seeking behaviours and perceived helpfulness of services between abused and non-abused women: A cross-sectional survey of Australian postpartum women. Health and Social Care in the Community, 28(3), 958–968. https://doi.org/10.1111/hsc.12927
Howarth, E., Moore, T. H., Welton, N. J., Lewis, N., Stanley, N., MacMillan, H., Shaw, A., Hester, M., Bryden, P., & Feder, G. (2016). IMPRoving Outcomes for children exposed to domestic ViolencE (IMPROVE): An evidence synthesis. Public Health Research, 4, 10. https://doi.org/10.3310/phr04100
Huntley, A. L., Potter, L., Williamson, E., Malpass, A., Szilassy, E., & Feder, G. (2019). Help-seeking by male victims of domestic violence and abuse (DVA): A systematic review and qualitative evidence synthesis. British Medical Journal Open, 9(6), e021960. https://doi.org/10.1136/bmjopen-2018-021960
Hudspeth, N., Cameron, J., Baloch, S., Tarzia, L., & Hegarty, K. (2022). Health practitioners’ perceptions of structural barriers to the identification of intimate partner abuse: a qualitative meta-synthesis. BMC Health Services Research, 22(1), 1–20.
*Ibrahim, E., Hamed, N., & Ahmed, L. (2021). Views of primary health care providers of the challenges to screening for intimate partner violence. Eastern Mediterranean Health Journal, 27(3), 233–241. https://doi.org/10.26719/emhj.20.125
*Joyner, K., & Mash, B. (2012). A comprehensive model for intimate partner violence in South African primary care: action research. BMC Health Services Research, 12(1), 399-399.https://doi.org/10.1186/1472-6963-12-399
Kalra, N., Hooker, L., Reisenhofer, S., Di Tanna, G. L., & García-Moreno, C. (2021). Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev., 5(5), CD012423. https://doi.org/10.1002/14651858.CD012423.pub2
Kelly, P., Hegarty, J., Barry, J., Dyer, K. R., & Horgan, A. (2017). A systematic review of the relationship between staff perceptions of organizational readiness to change and the process of innovation adoption in substance misuse treatment programs. Journal of Substance Abuse Treatment., 80, 6–25.
*Klause, K. T., Dodds, V. A., Selleck, C., & Deupree, J. P. (2020). Addressing Intimate Partner Violence at a Safety-Net Clinic for Adults. Journal for Nurse Practitioners, 16(2), 154-157.https://doi.org/10.1016/j.nurpra.2019.08.019
*Lam, T. P., Chan, H. Y., Piterman, L., Wong, M. W., Sun, K. S., Lam, K. F., Chan, T. H., Dan, W., & Tiwari, A. (2020). Factors that facilitate recognition and management of domestic violence by primary care physicians in a Chinese context - a mixed methods study in Hong Kong. BMC Family Practice, 21(1), 1-12.https://doi.org/10.1186/s12875-020-01228-4
Larkins, C., Drinkwater, J., Hester, M., Stanley, N., Szilassy, E., & Feder, G. (2015). General practice clinicians’ perspectives on involving and supporting children and adult perpetrators in families experiencing domestic violence and abuse. Family Practice, 32(6), 701–705. https://doi.org/10.1093/fampra/cmv070
Letourneau, N. L., Fedick, C. B., & Willms, J. D. (2007). Mothering and Domestic Violence: A Longitudinal Analysis [article]. Journal of Family Violence, 22(8), 649–660. https://login.ezproxy.library.ualberta.ca/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=edshol&AN=edshol.hein.journals.jfamv22.72&site=eds-live&scope=site.
*Leung, T. P., Bryant, C., Phillips, L., & Hegarty, K. (2017). GPs' perceived readiness to identify and respond to intimate partner abuse: development and preliminary validation of a multidimensional scale. Australian and New Zealand Journal of Public Health, 41(5), 512-517. https://doi.org/10.1111/1753-6405.12683
Libal, K., & Parekh, S. (2009). Reframing violence against women as a human rights violation: Evan Stark’s Coercive Control. Violence against Women, 15(12), 1477–1489. https://doi.org/10.1177/1077801209346958
Lievore, D. (2005). No longer silent: A study of women's help-seeking decisions and service responses to sexual assault. https://www.aic.gov.au/publications/archive/archive-134. Accessed 8 May 2023.
Loncar, N., & Scott, K. L. (2023). “The Average Counsellor Wouldn’t Know”: Exploring How General Health Practitioners Understand and Respond to Domestic Violence. Canadian journal of nursing research, 55(2), 153–164.
*Martin-Engel, L., Allen, J., Alencar, A., Levin, S., Udezi, V. O., Pagels, P., & Eary, R. L. (2021). Improving Readiness to Manage Intimate Partner Violence in Family Medicine Clinics by Collaboration With a Community Organization. PRiMER (Leawood, Kan.), 5(101726396), 20. https://doi.org/10.22454/PRiMER.2021.717020
Miller, E., Decker, M. R., Raj, A., Reed, E., Marable, D., & Silverman, J. G. (2010). Intimate partner violence and health care-seeking patterns among female users of urban adolescent clinics. Maternal and Child Health Journal, 14(6), 910–917. https://doi.org/10.1007/s10995-009-0520-z
Miller, E., McCaw, B., Humphreys, B. L., & Mitchell, C. (2015). Integrating intimate partner violence assessment and intervention into healthcare in the United States: A systems approach. Journal of Womens Health (larchmt)., 24(1), 92–99. https://doi.org/10.1089/jwh.2014.4870
*Miller, D., & Jaye, C. (2007). GPs' perception of their role in the identification and management of family violence. Family practice, 24(2), 95-101
Minsky-Kelly, D., Hamberger, L. K., Pape, D. A., & Wolff, M. (2005). We’ve had training, now what? Qualitative analysis of barriers to domestic violence screening and referral in a health care setting. Journal of Interpersonal Violence, 20(10), 1288–1309. https://doi.org/10.1177/0886260505278861
*Mohd Mydin, F. H., & Othman, S. (2020). Elder Abuse and Neglect Intervention in the Clinical Setting: Perceptions and Barriers Faced by Primary Care Physicians in Malaysia. Journal of Interpersonal Violence, 35(23/24), 6041-6066.https://doi.org/10.1177/0886260517726411
*Mohd Mydin, F. H., Othman, S., Choo, W. Y., Mohd Hairi, N. N., Mohd Hairi, F., Ali, Z., & Abdul Aziz, S. (2022). Primary care nurses' challenges, opportunities, and facilitators of elder abuse intervention in Malaysia. Public Health Nursing, 39(1), 3-14.https://doi.org/10.1111/phn.12961
Montesanti, S., Ghidei, W., Silverstone, P., Wells, L., Squires, S., & Bailey, A. (2022). Examining organization and provider challenges with the adoption of virtual domestic violence and sexual assault interventions in Alberta, Canada, during the COVID-19 pandemic. Journal of Health Services Research & Policy, 27(3), 169–179. https://doi.org/10.1177/13558196221078796
*Mork, T., Andersen, P. T., & Taket, A. (2014). Barriers among Danish women and general practitioners to raising the issue of intimate partner violence in general practice: a qualitative study. BMC women's health, 14(101088690), 74.https://doi.org/10.1186/1472-6874-14-74
Mouzos, J., & Rushforth, C. (2003). Family Homicide in Australia. Trends & issues in crime and criminal justice no. 255. Canberra: Australian Institute of Criminology. https://www.aic.gov.au/publications/tandi/tandi255. Accessed 8 May 2023.
Mouzos, J. (2001). Indigenous and Non-Indigenous Homicides in Australia: A Comparative Analysis. Trends & Issues in Crime & Criminal Justice(210), 1–6. https://login.ezproxy.library.ualberta.ca/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=cja&AN=57213787&site=eds-live&scope=site
*Mydin, F. H. M., Yuen, C. W., & Othman, S. (2021). The Effectiveness of Educational Intervention in Improving Primary Health-Care Service Providers' Knowledge, Identification, and Management of Elder Abuse and Neglect: A Systematic Review. Trauma, Violence & Abuse, 22(4), 944-960https://doi.org/10.1177/1524838019889359
National Inquiry Into Missing and Murdered Indigenous Women and Girls. (2019). Reclaiming Power and Place: The Final Report of the National Inquiry into Missing and Murdered Indigenous Women and Girls. https://www.mmiwg-ffada.ca/final-report/. Accessed 8 May 2023.
*Nicolaidis, C., & Touhouliotis, V. (2006). Addressing intimate partner violence in primary care: lessons from chronic illness management. Violence and victims, 21(1), 101-115.
O’Campo, P., Kirst, M., Tsamis, C., Chambers, C., & Ahmad, F. (2011). Implementing successful intimate partner violence screening programs in health care settings: Evidence generated from a realist-informed systematic review. Social Science and Medicine, 72(6), 855–866. https://doi.org/10.1016/j.socscimed.2010.12.019
*Papadakaki, M., Prokopiadou, D., Petridou, E., Kogevinas, M., & Lionis, C. (2012). Defining physicians' readiness to screen and manage intimate partner violence in Greek primary care settings. Evaluation & the health professions, 35(2), 199-220https://doi.org/10.1177/0163278711423937
*Papadakaki, M., Petridou, E., Kogevinas, M., & Lionis, C. (2013). Measuring the effectiveness of an intensive IPV training program offered to Greek general practitioners and residents of general practice. BMC medical education, 13(101088679), 46.https://doi.org/10.1186/1472-6920-13-46
*Pokharel, B., Yelland, J., Hooker, L., & Taft, A. (2021). A Systematic Review of Culturally Competent Family Violence Responses to Women in Primary Care. Trauma, Violence & Abuse(100890578), 15248380211046968. https://doi.org/10.1177/15248380211046968
Proctor, E., Silmere, H., Raghavan, R., Hovmand, P., Aarons, G., Bunger, A., Griffey, R., & Hensley, M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research., 38, 65–76.
*Ramsay, J., Rutterford, C., Gregory, A., Dunne, D., Eldridge, S., Sharp, D., & Feder, G. (2012). Domestic violence: knowledge, attitudes, and clinical practice of selected UK primary health care clinicians. The British journal of general practice : the journal of the Royal College of General Practitioners, 62(602), e647-655.https://doi.org/10.3399/bjgp12X654623
Renner, L. M., Wang, Q., Logeais, M. E., & Clark, C. J. (2021). Health Care Providers’ Readiness to Identify and Respond to Intimate Partner Violence. Journal of Interpersonal Violence, 36(19–20), 9507–9534. https://doi.org/10.1177/0886260519867705
Richardson, J., Coid, J., Petruckevitch, A., Chung, W. S., Moorey, S., & Feder, G. (2002). Identifying domestic violence: Cross sectional study in primary care. BMJ, 324(7332), 274. https://doi.org/10.1136/bmj.324.7332.274
Rivara, F. P., Anderson, M. L., Fishman, P., Bonomi, A. E., Reid, R. J., Carrell, D., & Thompson, R. S. (2007). Health care utilization and costs for women with a history of intimate partner violence. American Journal of Preventive Medicine, 32(2), 89–96. https://doi.org/10.1016/j.amepre.2006.10.001
*Rizkalla, K., Maar, M., Pilon, R., McGregor, L., & Reade, M. (2020). Improving the response of primary care providers to rural First Nation women who experience intimate partner violence: a qualitative study. BMC women's health, 20(1), 209.https://doi.org/10.1186/s12905-020-01053-y
Rossman, B. B. R. (2001). Longer term effects of children's exposure to domestic violence. In: S. A. Graham-Bermann & J. L. Edleson (Eds.), Domestic violence in the lives of children: The future of research, intervention, and social policy. (pp. 35–65). American Psychological Association. https://doi.org/10.1037/10408-003
*Ruiz-Perez, I., Pastor-Moreno, G., Escriba-Aguir, V., & Maroto-Navarro, G. (2018). Intimate partner violence in women with disabilities: perception of health care and attitudes of health professionals. Disability and rehabilitation, 40(9), 1059-1065.https://doi.org/10.1080/09638288.2017.1288273
Sharma, A., & Borah, S. B. (2022). Covid-19 and Domestic Violence: an Indirect Path to Social and Economic Crisis [Article]. Journal of Family Violence, 37(5), 759–765-765. https://doi.org/10.1007/s10896-020-00188-8
Short, L. M., Alpert, E., Harris Jr, J. M., & Surprenant, Z. J. (2006). PREMIS: a comprehensive and reliable tool for measuring physician readiness to manage IPV. American Journal of Preventive Medicine, 30(2), 173.
Sinha, V., Trocmé, N., Fallon, B., & MacLaurin, B. (2013). Understanding the investigation-stage overrepresentation of First Nations children in the child welfare system: An analysis of the First Nations component of the Canadian Incidence Study of Reported Child Abuse and Neglect 2008. Child Abuse and Neglect, 37(10), 821–831. https://doi.org/10.1016/j.chiabu.2012.11.010
*Soglin, L. F., Bauchat, J., Soglin, D. F., & Martin, G. J. (2009). Detection of intimate partner violence in a general medicine practice. Journal of Interpersonal Violence, 24(2), 338-348. https://doi.org/10.1177/0886260508316481
*Szilassy, E., Drinkwater, J., Hester, M., Larkins, C., Stanley, N., Turner, W., & Feder, G. (2017). Making the links between domestic violence and child safeguarding: an evidence-based pilot training for general practice. Health & Social Care in the Community, 25(6), 1722-1732.https://doi.org/10.1111/hsc.12401
*Szilassy, E., Roy, J., Williamson, E., Pitt, K., Man, M.-S., & Feder, G. (2021). Reaching everyone in general practice? Feasibility of an integrated domestic violence training and support intervention in primary care. BMC Family Practice, 22(1), 19.https://doi.org/10.1186/s12875-020-01297-5
*Taskiran, A. C., Ozsahin, A., & Edirne, T. (2019). Intimate partner violence management and referral practices of primary care workers in a selected population in Turkey. Primary health care research & development, 20(100897390), e96. https://doi.org/10.1017/S1463423619000288
*Taylor, D. K., Bachuwa, G., Evans, J., & Jackson-Johnson, V. (2006). Assessing barriers to the identification of elder abuse and neglect: a communitywide survey of primary care physicians. Journal of the National Medical Association, 98(3), 403-404.
Taylor, G. (2016). A Focus on Family Violence in Canada : the Chief Public Health Officer's Report on the State of Public Health in Canada 2016. Public Health Agency of Canada. http://www.deslibris.ca/ID/10090057. Accessed 8 May 2023.
Thomas, J., Newman, M., & Oliver, S. (2013). Rapid evidence assessments of research to inform social policy: Taking stock and moving forward. Evidence and Policy, 9(1), 5–27. https://doi.org/10.1332/174426413x662572
*Turner, W., Hester, M., Broad, J., Szilassy, E., Feder, G., Drinkwater, J., Firth, A., & Stanley, N. (2017). Interventions to Improve the Response of Professionals to Children Exposed to Domestic Violence and Abuse: A Systematic Review. Child abuse review (Chichester, England : 1992), 26(1), 19–39. https://doi.org/10.1002/car.2385
Ullman, S. E., Relyea, M., Peter-Hagene, L., & Vasquez, A. L. (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive Behaviors, 38(6), 2219–2223.
van Gelder, N., Peterman, A., Potts, A., O’Donnell, M., Thompson, K., Shah, N., & Oertelt-Prigione, S. (2020). COVID-19: Reducing the risk of infection might increase the risk of intimate partner violence. eClinicalMedicine, 21, 100348. https://doi.org/10.1016/j.eclinm.2020.100348
*Varcoe, C., Ford-Gilboe, M., Browne, A. J., Perrin, N., Bungay, V., McKenzie, H., Smye, V., Price Elder, R., Inyallie, J., Khan, K., & Dion Stout, M. (2021). The Efficacy of a Health Promotion Intervention for Indigenous Women: Reclaiming Our Spirits. J Interpers Violence, 36(13–14). https://doi.org/10.1177/0886260518820818
Watt, A., Cameron, A., Sturm, L., Lathlean, T., Babidge, W., Blamey, S., Facey, K., Hailey, D., Norderhaug, I., & Maddern, G. (2008). Rapid versus full systematic reviews: Validity in clinical practice? ANZ Journal of Surgery, 78(11), 1037–1040. https://doi.org/10.1111/j.1445-2197.2008.04730.x
Weiner, B. J., Amick, H., & Lee, S. Y. (2008). Conceptualization and measurement of organizational readiness for change: A review of the literature in health services research and other fields. Medical Care Research and Review., 65, 4.
Wolfe, D. A., Crooks, C. V., Lee, V., McIntyre-Smith, A., & Jaffe, P. G. (2003). The Effects of Children’s Exposure to Domestic Violence: A Meta-Analysis and Critique. Clinical Child and Family Psychology Review, 6(3), 171–187. https://doi.org/10.1023/A:1024910416164
*Lo Fo Wong, S., Wester, F., Mol, S., & Lagro-Janssen, T. (2007). 'I am not frustrated anymore' Family doctors' evaluation of a comprehensive training on partner abuse. Patient Education & Counseling, 66(2), 129-137.https://doi.org/10.1016/j.pec.2006.12.013
World Health Organization. Caring for women subjected to violence: a WHO curriculum for training health-care providers; 2019. Available at http://www.who.int/reproductivehealth/publications/caring-for-women-subject-to-violence/en/. Accessed 8 May 2023.
*Wuest, J., Merritt-Gray, M., Dubé, N., Hodgins, M. J., Malcolm, J., Majerovich, J. A., Scott-Storey, K., Ford-Gilboe, M., & Varcoe, C. (2015). The process, outcomes, and challenges of feasibility studies conducted in partnership with stakeholders: a health intervention for women survivors of intimate partner violence. Res Nurs Health, 38(1), 82-96.https://doi.org/10.1002/nur.21636
Ying Ying, C., Hairi, N. N., & Othman, S. (2023). Tools for Assessing Health care Providers’ Readiness to Respond to Intimate Partner Violence: A Systematic Review. Journal of Family Violence, 1–24. https://doi.org/10.1007/s10896-023-00491-0
Zahl-Olsen, R., Bertelsen, T. B., Haaland, A. T., Gausel, N., Zahl-Olsen, A., & Tilden, T. (2019). Physical Couple and Family Violence Among Clients Seeking Therapy: Identifiers and Predictors. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.02847
Acknowledgements
The authors would like to acknowledge Women and Children’s Health Research Institute (WCHRI) situated at the University of Alberta for their funding of the project titled ‘Strengthening Health System Responses to Family Violence.’ The authors are also grateful for the support provided by the study team, specifically Krista Milford for her support with project coordination and mentorship of the graduate research assistant and research coordinator who supported this review. Stephanie Montesanti receives financial support by the Canada Research Chair program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
No competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Montesanti, S., Goveas, D., Bali, K. et al. Exploring Factors Shaping Primary Health Care Readiness to Respond to Family Violence: Findings from a Rapid Evidence Assessment. J Fam Viol (2023). https://doi.org/10.1007/s10896-023-00677-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s10896-023-00677-6