Abstract
There is widespread concern that elder abuse and neglect (EAN) incidents increased during the onset of the COVID-19 pandemic due in part to increases in risk factors. Initial reports relying on administrative systems such as adult protective services records produced mixed results regarding whether or not there was a change in EAN incidents. Using data from an ongoing longitudinal study on EAN in dementia family caregiving that started before the pandemic, we assessed the hypothesis that the pandemic is related to a change in probability of EAN and EAN protective factors. Family caregivers to persons with dementia completed two waves of 21 daily diaries, 6-months apart, assessing their daily use of EAN behaviors. The first group (n = 32) completed their first wave before the pandemic and their second wave during the pandemic. The second group (n = 32) completed both waves during the pandemic. For this cohort, the generalized linear mixed logistic model results showed inconsistent associations between the onset of COVID-19 and the probability of a caregiver engaging in elder abuse or neglect behaviors. In terms of protective factors, the use of formal services was not significantly impacted by COVID-19; however, the likelihood of receiving informal support from family and friends increased significantly during the pandemic period. Dementia family caregivers were not likely impacted negatively by initial pandemic restrictions, such as shelter-in-place orders, as anticipated. These findings contribute to our understanding of how distal, disruptive processes may influence more proximal caregiver stresses and the likelihood of EAN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Before COVID-19’s onset, some have described abuse and neglect (EAN) as an epidemic (Dong, 2005; Lachs & Pillemer, 2015) because EAN affects about 10% of community-dwelling older adults and over half of the persons with Alzheimer’s disease and related dementias (Acierno et al., 2010; Pickering et al., 2020; Wiglesworth et al., 2010). Media reports (Birnstengel, 2020; Byrne, 2020) and concerns from clinicians (Elman et al., 2020; Han & Mosqueda, 2020; Makaroun et al., 2020), speak to even higher rates of EAN during the COVID-19 pandemic. However, there is a lack of longitudinal data testing whether the COVID-19 pandemic impacted risk of EAN.
While there is a paucity of research on the causes of EAN within family caregiving, several risk factors in family caregiving have been identified, including caregiver stress related to behavioral symptom management and the lack of formal and informal social support for the caregiver (Fang & Yan, 2018; Pickering et al., 2020). The COVID-19 pandemic is thought to impact these known risk factors on a population level (Chang & Levy, 2021; Kent et al., 2020; Makaroun et al., 2020). Some have argued that shelter-in-place orders, in particular, have impacted risk/protective factors for EAN, particularly for those with dementia, by removing sources of social support such as formal services and increasing reliance on family caregivers. (Han & Mosqueda, 2020). Therefore, the logic that follows is that adverse changes in social support and other risk/protective factors may have increased the overall rate of EAN.
To date, there has been one study on changes in known EAN risk factors completed with family caregivers to older adults during the pandemic. This cross-sectional study reported that 64% of respondents felt they had somewhat or greatly increased feelings of social isolation and loneliness compared to pre-pandemic times (Makaroun et al., 2021). Though the sample was not exclusive to dementia family caregivers, these data support that risk factors for EAN may have changed during the pandemic. Thus, the empirical evidence is limited regarding the effects of the pandemic on EAN risk and related risk/protective factors within dementia family caregiving. Knowledge of how the pandemic impacted EAN is important in order to understand the need for post-pandemic services to suppress the adverse effects of the pandemic on EAN in dementia caregiving.
Some evidence has linked disasters and public health crises (Gearhart et al., 2018; Schumacher et al., 2010), including the COVID-19 and shelter-in-place orders (Nix & Richards, 2021; Piquero et al., 2020, 2021), with increased prevalence and severity of intimate partner violence. However, similar data on EAN and dementia family caregiving are lacking to guide the interpretation of current reports from service agencies and inform intervention efforts during this public health crisis (Gutman & Yon, 2014). Therefore, the purpose of this study is to examine the impact of the COVID-19 pandemic on EAN within family caregiving for dementia. Using self-reports from an ongoing longitudinal study of daily experiences of dementia family caregivers, we tested the hypotheses that the COVID-19 pandemic was associated with (1) a significant increase in daily risk of EAN as compared to the pre-pandemic period and (2) significant changes in levels of risk among known risk/protective factors (i.e., receipt of formal services, receipt of informal support, caregiver stress).
Methods
We selected a subset of cases from participants in an ongoing longitudinal study that opened before the COVID-19 pandemic. The parent study examines the impact of stressors on caregiving outcomes, such as EAN. It uses a multilevel longitudinal design in which participants complete traditional surveys at enrollment and then twice more, each one separated by six months. After completing each of the three traditional surveys, participants complete a 21-day micro-longitudinal “burst” of daily surveys. Each daily survey assesses their environmental, social, and caregiving experiences in near real-time. This protocol yields data about 21 serial days that are nested within three periods that span 18 months. These three periods are then nested within each respondent. Participants receive all daily surveys by e-mail or interactive-voice-response by phone (IVR) via a data broker to ensure participant anonymity. Since all study activities occur online or by phone (i.e., recruitment, enrollment, data collection, compensation), data collection was not disrupted because of the onset of the COVID-19 pandemic across the United States. Study procedures are designed so that participation is confidential, but research data are anonymous. We use this design to limit the threat of bias related to mandatory reporting. The University of Alabama at Birmingham’s IRB approved this study as exempt.
Participants in the ongoing study were recruited nationally from various sources, including community agencies, newsletters, newspapers, bus ads, and social media. The study uses a three-step authentication process for enrollment to ensure valid and legitimate participants (King et al., 2014; Kramer et al., 2014; Teitcher et al., 2015). Eligibility criteria include serving as a caregiver who is 18 years or older who provides unpaid care to a spouse/common-law partner, parent, or grandparent (or in-law, age 60 + years) with mild cognitive impairment or dementia as indicated by the AD8 (Galvin et al., 2005). Care consists of help with at least two Instrumental Activities of Daily Living or one Activity of Daily Living, and the caregiver lives with or shares cooking facilities with the care recipient. Participants must live in the U.S. and read/speak English or Spanish.
Enrollment for the parent study began in fall 2019. This just-in-time analysis uses selected cases from two groups: 1) a “pre-COVID” group of 32 participants who completed their first wave of measurement before the pandemic (i.e., before January 26th, 2020), and their second wave of measurement during the pandemic (i.e., after March 28th, 2020), and 2) a “during COVID” group of 32 participants who completed their first and second waves of measurement during the pandemic (i.e., both waves after March 20th, 2020). The “during COVID” group is included for comparison purposes to aide in interpretation as there are no existing data on the longitudinal trajectory of EAN prevalence or risk in dementia family caregivers.
The pre-COVID group initially was composed of 38 participants. However, six participants were excluded from analyses because they had not provided at least ten daily diaries in each wave of measurement. The during-COVID group was also selected sequentially based on the same missing daily survey exclusion criteria until a matched sample size of 32 participants was reached.
Measures
Demographic and background characteristics were measured on the traditional surveys at the person level, including race, gender, age, and relationship of the caregiver to the care recipient. All daily survey items ask respondents to report about experiences that occurred from “7 am yesterday morning to 7 am this morning.”
Self-reported EAN by caregivers was previously demonstrated as valid compared to expert judgment (Wiglesworth et al., 2010). EAN items assessed on the daily diaries were informed by prior work (Pickering et al., 2020; Sullivan et al., 2012), and based on the Conflict Tactics Scale-Revised and Modified Conflict Tactics Scale (Beach et al., 2005; Straus et al., 1996). The neglect measure is a dichotomous composite that indicates whether any of the following four actions occurred within the past 24 h: (1) skipped care or not helping with personal hygiene or going to the bathroom even though the care recipient needed help; (2) skipped care or not helping at mealtime even though the care recipient needed help; (3) ignoring a care recipient’s reasonable request for help; and (4) leaving the care recipient alone for any period of time even though you thought someone should be there to supervise or help. The psychological abuse measure is a dichotomous composite indicating if either of two psychologically aggressive actions occurred on the diary day: (1) cursing, yelling, shouting at, or speaking to the care recipient in a way you know is not fair or appropriate; (2) threatening to abandon or put the care recipient in a nursing home. The physical abuse measure is a dichotomous composite indicating if any of the three physically aggressive actions occurred on the diary day: (1) pinching, pushing, shoving, or grabbing the care recipient, twisting their arm or hair, or throwing something at them that could have injured them; (2) biting, hitting, kicking, punching, choking, or burning the care recipient; or (3) bruising, scratching, or otherwise physically injuring the care recipient in any way. An EAN composite measure that combined these three forms of EAN was created then was dichotomized for the primary analyses.
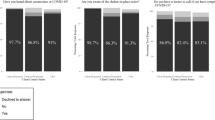
Single items assessing formal and informal support also were collected at the day level. Participants were asked about receipt of formal services (“Did you get help from a paid provider in caring for your relative with dementia, such as a nurse’s aide or companion?”), and informal support (“Did you get help from a family member or friend in providing care to your relative with dementia?”) with yes/no response options for each.
Caregiver stress reactions to behavioral symptoms of dementia (BSD) exhibited by the care recipient were also collected at the day level. Participants were asked to rate how bothered they were by several behavioral symptoms throughout the day, including restlessness, mood symptoms, care resistance, property destruction, disinhibition, verbal aggression, physical aggression, and any other behavioral symptoms they found bothersome. Participants responded on a 5-point Likert scale with higher scores indicating higher levels of bother. Responses were then summed across the eight items to create a total daily BSD stress reaction score.
Analysis
Due to the nested structure of these data (days within persons), a multilevel model (MLM) approach was taken to account for the residual variance at both the person (between) and the day (within) components (Hayes, 2006; Peugh, 2010). By allowing individual intercepts to vary (random effects in a mixed model), we can consider individual influences on an outcome variable as compared to traditional ordinary least squared regressions. Specifically, a generalized linear mixed logistic model was used to estimate the daily probability of various outcome measures in our current sample (Hayes, 2006; Peugh, 2010). BSD stress reactions were estimated with a linear effects mixed model as the response measure is continuous. The linear mixed-effects models using 'Eigen' and S4 (LME4; ver 1.1–26) function was specified in RStudio (ver 1.4) to model outcomes (Bates, 2010; Team, 2015). Post-hoc pairwise comparisons and predicted probabilities were generated by the emmeans package (Lenth, 2021) in Rstudio.
A dummy variable was computed to represent each of the 4-levels in which groups and measurement waves are represented in the analysis. Level 1 represents the pre-COVID group at their first measurement wave (before COVID), Level 2 represents the pre-COVID group at their second measurement wave (during COVID), Level 3 represents the during-COVID group at their first measurement wave (during COVID), and Level 4 represents the during-COVID group at their second measurement wave (during COVID). By specifying dichotomous measures for each combination of group and period, we created a fixed-effects component with 4-levels (Time). By treating Level 1 (pre-COVID group at the first measurement wave) as the reference level/baseline, we can determine if there are any significant changes in the outcome scores (EAN, formal services, informal support, BSD stress reactions) against Level 2 (pre-COVID group at period 2), Level 3 (during-COVID group at period 1) and Level 4 (during-COVID group at period 2). In doing so, we are comparing outcomes of the pre-COVID group at their first measurement wave – which occurred pre-pandemic – to all other measurement points, which happened after the pandemic. Additional models were run with the individual composite measures for physical abuse, psychological abuse, and neglect.
Results
The sample included N = 64 caregivers across the two groups (N = 32 pre-COVID, N = 32 during-COVID) reporting on n = 2,370 diary days. The average daily diary compliance rate is 88% calculated as the number of daily diaries completed out of the number of diaries that could have been completed. Participants were predominantly female, white, and caring for a spouse. Over half of care recipients were male, and the most common diagnosis was Alzheimer’s disease. No significant differences between groups were observed on demographics (Table 1). No notable differences were observed between the final sample and those excluded for missing data other than that those excluded were a slightly higher proportion of non-White participants, though this is out of a sample size of 6 (Supplementary Table 1). Supplementary Table 2 presents the day-level descriptives for all outcome measures. The values represent the mean number of days out of 21 sampled that the outcome was reported. Supplementary Table 3 reports the person-level descriptives for all outcome measures. The values represent the proportion of participants who reported the outcome.
Tables 2 and 3 report the results produced by the generalized linear mixed logistic and generalized linear mixed-effect models. For ease of interpretation, figures were created to graphically represent the predicted probabilities produced by the models for the binomial outcomes (back-transformed from the logit scale). These predicted probabilities represent the average probability that the participant endorsed the outcome during that wave of measurement by each group.
Regarding the first hypothesis, no significant differences in the probability of EAN were found for the pre-COVID group at their first measurement wave compared to the pre-COVID group at their second measurement wave, or the during-COVID group at either wave 1 or wave 2. In other words, no significant changes in the probabilities of EAN were observed during the pandemic when compared to pre-pandemic time-period. While non-significant, the likelihood of EAN trended downward as the pandemic started compared to the pre-pandemic time-point, but then returned to the baseline probability within 6 months. Post-hoc comparisons showed a significant increase in the probability of EAN for the during-COVID group from their first measurement wave to their second (Table 4), approximately equaling the level of risk for the pre-COVID group at their first measurement wave (6% vs. 7% probability) (Fig. 1).
Predicted Probabilities of Group and Period for Elder Abuse and Neglect. Note: Predicted probabilities are based on the response variable (0 or 1). The probabilities are derived from the odds ratios produced by the final model. The comparison line represents a significant pairwise comparison (p < 0.001); the three other pairwise comparisons are non-significant
When neglect, psychological abuse and physical abuse were analyzed separately, no significant difference in likelihood was detected (Table 3). However, in post-hoc pairwise comparisons, we found the same effect as the combined EAN variable, with the likelihood of neglect significantly increasing for the during-COVID group at their second measurement wave compared to their first, rising slightly above the probability of the pre-COVID group at their first measurement wave (3% vs 1.7% probability) (Fig. 2). Psychological abuse also followed this trend in its post-hoc pairwise comparisons, but only approached significance (p = 0.0597) (Fig. 3). We did not see any significant pairwise comparisons for psychological abuse (Fig. 3) or physical abuse (Fig. 4).
Predicted Probabilities of Group and Period for Neglect. Note: Predicted probabilities are based on the response variable (0 or 1). The probabilities are derived from the odds ratios produced by the final model. The comparison line represents a significant pairwise comparison (p < 0.001); the three other pairwise comparisons are non-significant
Regarding the second hypothesis related to risk/protective factors, no significant difference was observed for receipt of formal services over time (Fig. 5). In contrast, there was a significant difference in the probability of receiving informal support, with those in the pre-COVID group significantly more likely to receive informal support at their second measurement (during the initial pandemic period) wave compared to their first measurement wave taken before the pandemic (1.94 OR, CI 1.33 – 2.84, p < 0.001). While not significant, those in the during-COVID group also had a higher probability of receiving informal support during the initial pandemic period at their first measurement wave as compared to the pre-COVID group at their first measurement wave. In post-hoc pairwise comparisons, there were no significant differences in formal services, while informal support saw a significant decrease for the during-COVID group from their first measurement wave to their second (25% vs. 16% probability) (Fig. 6). In terms of caregiver stress reactions to BSD, we did not observe a significant change between the pre-COVID group at their first measurement wave compared to the three other measurement points (Fig. 7). There were also no significant pairwise comparisons in our post-hoc analysis.
Predicted Probabilities of Group and Period for Informal Support. Note: Predicted probabilities are based on the response variable (0 or 1). The probabilities are derived from the odds ratios produced by the final model. The comparison lines represent significant pairwise comparisons (p < 0.001); the other pairwise comparison is non-significant
Discussion
For this cohort of family caregivers to persons with dementia, no clear associations emerged between the onset of COVID-19 and the probability of EAN. While not temporally significant, the trends suggested that, contrary to early reports, EAN decreased during the initial pandemic period. For the during-COVID group, there was a significant increase in EAN from their first to second measurement, but the second measurement was not significantly different from the pre-COVID group’s first measurement. This comparison suggests that while EAN decreased during the initial pandemic period, it returned to the baseline level as time continued. This u-shaped trend is in contrast to reports of how COVID-19 impacted intimate partner violence rates which described the IPV trend as initially spiking in police calls for service during the initial pandemic shelter-in-place periods followed by a decrease as time progressed (Nix & Richards, 2021). Our results also showed that there was not a significant increase in the probability of EAN related to COVID-19 demonstrating that not all forms of interpersonal stress lead to greater EAN in dementia family caregiving, consistent with prior studies (Pickering et al., 2020). The mean number of days for which EAN behaviors occurred in the overall sample is also consistent with prior studies (Pickering et al., 2020). This continuity across samples highlights that while there are no EAN behaviors on the majority of days, it remains too frequent in dementia family caregiving.
Given the shelter-in-place and social distancing mandates, it was thought both formal services and informal support would decrease in the initial pandemic period (Han & Mosqueda, 2020; Makaroun et al., 2020, 2021), and caregiver perceived stress would increase due to exaggerated behavioral symptoms of dementia that are related to changes in care (Cagnin et al., 2020). However, we observed no significant changes in the probability of receiving formal support. This was likely because healthcare workers are considered essential workers and were not restricted from working, so those who already had care in place were not affected. Additionally, we observed a significant increase in the probability of receiving informal support from family and friends at the pandemic onset compared to the pre-pandemic period for the pre-COVID group, and a significant decline in probability from pandemic onset compared to 6-months later for the during-COVID group. Shelter-in-place mandates, such as the closures of businesses and telework, may have increased the availability of family and friends to help with caregiving. While it appears in contrast to cross-sectional reports of the impact of pandemic restrictions on family caregivers (Makaroun et al., 2021), this finding is consistent with increased perceptions of social support during the initial pandemic shelter-in-place period among national samples of U.S. adults reported in other longitudinal work (Luchetti et al., 2020). Notably, the previous study reported on caregivers’ perceptions of social isolation and loneliness (Makaroun et al., 2021), which is not the same concept as receipt of formal and informal support. Meta-analyses have demonstrated for family caregivers that perceptions of social support and actual receipt of social support are not redundant concepts (Del-Pino-Casado et al., 2018). Equally, perceptions of social support are not the inverse of perceptions of social isolation and loneliness. Perceptions of social isolation and loneliness have not been examined as risk factors for EAN within dementia family caregiving prior to the pandemic (Fang & Yan, 2018), which limits our ability to draw conclusions as to why there may be a difference in findings.
Furthermore, results from this study suggest that caregivers’ stress reactions to behavioral symptoms of dementia did not significantly change over time. There were non-significant trends indicating stress reactions were higher at the initial pandemic time for both groups. While this trend equates to a ~ 0.45% increase in the predicted probability, the change is not clinically significant. This near regularity is in contrast to cross-sectional studies, which indicate caregivers reported increased psychological distress related to increases in behavioral symptoms of dementia during the initial pandemic period (Cagnin et al., 2020; Cohen et al., 2020). The contrast may be because these prior studies lacked a baseline measurement for comparison; asking participants to estimate changes from the pre-pandemic period is subject to bias from state-congruent recall, which can overestimate negative moods compared to real-time assessments (Sato & Kawahara, 2011). State-congruent recall bias may also be why there are discrepancies between these findings and those from other studies on EAN risk factors during COVID.
This increase in the availability of informal support from family and friends for caregivers may explain why the probability of engaging in elder abuse or neglect trended down during the initial pandemic period. As COVID-19 represent an unplanned natural experiment, this study was not powered to test possible mediation effects of informal support. Nevertheless, we did find support for this hypothesis in the extant literature, with a systematic review reporting seven studies have demonstrated that either the lack of informal support increases EAN while increases in receipt of informal support decrease EAN risk among dementia family caregivers (Fang & Yan, 2018). These findings suggest interventions to increase informal support for dementia family caregivers may successfully reduce EAN risk.
A strength of this study is the daily diary method which enhances ecological validity and reduces recall bias and measurement error for the outcome measures (Schneider & Stone, 2015). For example, by counting each day whether or not a caregiver received actual formal/informal support, we can observe the changes in the amount of support received. Furthermore, we have previously reported higher rates of EAN among dementia family caregivers measured through anonymous daily diary methods than found among traditional retrospective surveys (Pickering et al., 2020). Others have reported high congruent validity between self-reported diary surveys and objective assessments of other stigmatizing health behaviors (Linas et al., 2016; Simons et al., 2015). Another strength of this study is its use of a longitudinal design that included measurements completed before the pandemic started for comparison. In doing this, we could estimate changes over time in the level of risk of an outcome among a cohort of dementia family caregivers.
Findings should be considered in the context of the study’s limitations. Analyses were not powered to detect small changes in EAN risk. However, this study's main focus was detecting a large change consistent with early reports of dramatic increases in EAN. Power is based on the sample size in each level in a multilevel model design (Snijders, 2005). Although we are looking at between-group differences, by utilizing a multilevel model, we believe that our primary outcome is a person-driven process. Therefore, our power is generated by our daily diaries (n = 2370) and is not from our person-level data (N = 64). In this team’s previous work, we saw significant effects at the day-level with a 50-person to 21-day ratio (Pickering et al., 2020), and this paper reports a 64:42 ratio. Simulation studies have also suggested a 20:30 ratio for fixed effects models, 50:20 for cross-level interactions, and 100:10 when the interest is in the variance and covariance components (Hox & McNeish, 2020).
Furthermore, a comparison group that completed both measurement points before COVID that could demonstrate the trajectory of EAN would have been ideal for determining if COVID impacted the natural trajectory. However, as this is an unplanned natural experiment, we had to rely on a comparison group that completed both measurements during COVID to evaluate the immediate impacts of COVID restrictions on EAN risk. While we used calendar dates to create the groups, some participants did their first measurement period 4–5 months after the pandemic. As there was variation in state and local restrictions across time (including when they were reduced), these participants were likely subject to different stressors. Due to anonymity, we could not assess impact of local restrictions. Nevertheless, the findings demonstrate a lack of a significant increase in EAN risk over time compared to the pre-pandemic period. Given the lack of studies reporting the characteristics of a nationally representative sample of dementia family caregivers, it is unclear how generalizable the study sample is. However, others have found that Facebook can produce more generalizable samples than other convenience methods (Whitaker et al., 2017).
In terms of policy and public health responses, restrictions such as shelter-in-place orders may not have impacted dementia family caregivers only in negative ways. Our results suggest that earlier initial reports of decreases in EAN reports were likely because EAN was not increasing uniformly across all older adults. The lack of a significant impact of COVID-19 on the probability of EAN in dementia family caregiving suggests that administratively collected service data require careful consideration of their representativeness prior to interpretation of the EAN community and national trends. While we did not find an increase in EAN risk among co-residing dementia family caregivers, other populations, such as older adults without dementia who lost access to resources or family caregivers who became caregivers due to the pandemic, may have experienced increases in EAN. More research differentiating between caregiving situations is needed to understand better the impact of COVID-19 and pandemic restrictions on EAN. Furthermore, given that this is a novel pandemic, the risk/protective factors selected for analyses for this study were chosen because there was prior empirical support to aid in interpreting findings. It is possible that other factors, such as caregiver mental health, may have significantly changed due to the pandemic. However, this possibility does not change the finding of a lack of a significant increase in EAN probability during the initial pandemic period in this sample.
References
Acierno, R., Hernandez, M. A., Amstadter, A. B., Resnick, H. S., Steve, K., Muzzy, W., & Kilpatrick, D. G. (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100(2), 292–297. https://doi.org/10.2105/AJPH.2009.163089
Bates, D. M. (2010). lme4: Mixed-effects modeling with R. Springer.
Beach, S. R., Schulz, R., Williamson, G. M., Miller, L. S., Weiner, M. F., & Lance, C. E. (2005). Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society, 53(2), 255–261. https://doi.org/10.1111/j.1532-5415.2005.53111.x
Birnstengel, G. (2020). Elder abuse appears to be climbing during the pandemic, experts say. https://www.pbs.org/newshour/nation/elder-abuse-appears-to-be-climbing-during-the-pandemic-experts-say
Byrne, K. (2020). 'It shouldn't be happening:' Elder abuse, neglect on the rise in Milwaukee County during COVID-19. https://www.tmj4.com/rebound/it-shouldnt-be-happening-elder-abuse-neglect-on-the-rise-in-milwaukee-county-during-covid-19
Cagnin, A., Di Lorenzo, R., Marra, C., Bonanni, L., Cupidi, C., Laganà, V., Rubino, E., Vacca, A., Provero, P., Isella, V., Vanacore, N., Agosta, F., Appollonio, I., Caffarra, P., Pettenuzzo, I., Sambati, R., Quaranta, D., Guglielmi, V., Logroscino, G., Filippi, M., Tedeschi, G., Ferrarese, C., Rainero, I., & Bruni, A. C. (2020). Behavioral and Psychological Effects of Coronavirus Disease-19 Quarantine in Patients With Dementia. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.578015
Chang, E. S., & Levy, B. R. (2021). High Prevalence of Elder Abuse During the COVID-19 Pandemic: Risk and Resilience Factors. The American Journal of Geriatric Psychiatry. https://doi.org/10.1016/j.jagp.2021.01.007
Cohen, G., Russo, M. J., Campos, J. A., & Allegri, R. F. (2020). Living with dementia: Increased level of caregiver stress in times of COVID-19. International Psychogeriatrics, 32(11), 1377–1381. https://doi.org/10.1017/s1041610220001593
Del-Pino-Casado, R., Frias-Osuna, A., Palomino-Moral, P. A., Ruzafa-Martinez, M., & Ramos-Morcillo, A. J. (2018). Social support and subjective burden in caregivers of adults and older adults: A meta-analysis. PLoS ONE, 13(1), e0189874. https://doi.org/10.1371/journal.pone.0189874
Dong, X. (2005). Medical Implications of Elder Abuse and Neglect. Clinics in Geriatric Medicine, 21(2), 293–313. https://doi.org/10.1016/j.cger.2004.10.006
Elman, A., Breckman, R., Clark, S., Gottesman, E., Rachmuth, L., Reiff, M., Callahan, J., Russell, L. A., Curtis, M., Solomon, J., Lok, D., Sirey, J. A., Lachs, M. S., Czaja, S., Pillemer, K., & Rosen, T. (2020). Effects of the COVID-19 Outbreak on Elder Mistreatment and Response in New York City: Initial Lessons. Journal of Applied Gerontology, 39(7), 690–699. https://doi.org/10.1177/0733464820924853
Fang, B., & Yan, E. (2018). Abuse of Older Persons With Dementia: A Review of the Literature. Trauma, Violence, & Abuse, 19(2), 127–147. https://doi.org/10.1177/1524838016650185
Galvin, J. E., Roe, C. M., Powlishta, K. K., Coats, M. A., Muich, S. J., Grant, E., Miller, J. P., Storandt, M., & Morris, J. C. (2005). The AD8: A brief informant interview to detect dementia. Neurology, 65(4), 559–564. https://doi.org/10.1212/01.wnl.0000172958.95282.2a
Gearhart, S., Perez-Patron, M., Hammond, T. A., Goldberg, D. W., Klein, A., & Horney, J. A. (2018). The Impact of Natural Disasters on Domestic Violence: An Analysis of Reports of Simple Assault in Florida (1999–2007). Violence and Gender, 5(2), 87–92. https://doi.org/10.1089/vio.2017.0077
Gutman, G. M., & Yon, Y. (2014). Elder abuse and neglect in disasters: Types, prevalence and research gaps. International Journal of Disaster Risk Reduction, 10, 38–47. https://doi.org/10.1016/j.ijdrr.2014.06.002
Han, S. D., & Mosqueda, L. (2020). Elder Abuse in the COVID -19 Era. Journal of the American Geriatrics Society, 68(7), 1386–1387. https://doi.org/10.1111/jgs.16496
Hayes, A. F. (2006). A primer on multilevel modeling. Human Communication Research, 32(4), 385–410.
Hox, J., & McNeish, D. (2020). Small Samples in Multilevel Modeling. In Small Sample Size Solutions (pp. 215–225). https://doi.org/10.4324/9780429273872-18
Kent, E. E., Ornstein, K. A., & Dionne-Odom, J. N. (2020). The Family Caregiving Crisis Meets an Actual Pandemic. Journal of Pain and Symptom Management, 60(1), e66–e69. https://doi.org/10.1016/j.jpainsymman.2020.04.006
King, D. B., O’Rourke, N., & DeLongis, A. (2014). Social media recruitment and online data collection: A beginner’s guide and best practices for accessing low-prevalence and hard-to-reach populations. Canadian Psychology/psychologie Canadienne, 55(4), 240–249. https://doi.org/10.1037/a0038087
Kramer, J., Rubin, A., Coster, W., Helmuth, E., Hermos, J., Rosenbloom, D., Moed, R., Dooley, M., Kao, Y.-C., Liljenquist, K., Brief, D., Enggasser, J., Keane, T., Roy, M., & Lachowicz, M. (2014). Strategies to address participant misrepresentation for eligibility in Web-based research. International Journal of Methods in Psychiatric Research, 23(1), 120–129. https://doi.org/10.1002/mpr.1415
Lachs, M. S., & Pillemer, K. A. (2015). Elder Abuse [Review]. The New England Journal of Medicine, 373(20), 1947–1956. https://doi.org/10.1056/NEJMra1404688
Lenth, R. V. (2021). emmeans: Estimated Marginal Means, aka Least-Squares Means. In (Version R package version 1.6.2–1) https://CRAN.R-project.org/package=emmeans
Linas, B. S., Genz, A., Westergaard, R. P., Chang, L. W., Bollinger, R. C., Latkin, C., & Kirk, G. D. (2016). Ecological Momentary Assessment of Illicit Drug Use Compared to Biological and Self-Reported Methods. JMIR mHealth and uHealth, 4(1), e27. https://doi.org/10.2196/mhealth.4470
Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID-19. American Psychologist. https://doi.org/10.1037/amp0000690
Makaroun, L. K., Bachrach, R. L., & Rosland, A.-M. (2020). Elder Abuse in the Time of COVID-19 - Increased Risks for Older Adults and Their Caregivers. The American Journal of Geriatric Psychiatry, 28(8), 876–880. https://doi.org/10.1016/j.jagp.2020.05.017
Makaroun, L. K., Beach, S., Rosen, T., & Rosland, A. M. (2021). Changes in Elder Abuse Risk Factors Reported by Caregivers of Older Adults during the COVID-19 Pandemic. Journal of the American Geriatrics Society. https://doi.org/10.1111/jgs.17009
Nix, J., & Richards, T. N. (2021). The immediate and long-term effects of COVID-19 stay-at-home orders on domestic violence calls for service across six U.S. jurisdictions. Police Practice and Research, 1–9. https://doi.org/10.1080/15614263.2021.1883018
Peugh, J. L. (2010). A practical guide to multilevel modeling. Journal of School Psychology, 48(1), 85–112.
Pickering, C. E. Z., Yefimova, M., Maxwell, C., Puga, F., & Sullivan, T. (2020). Daily Context for Abusive and Neglectful Behavior in Family Caregiving for Dementia. The Gerontologist, 60(3), 483–493. https://doi.org/10.1093/geront/gnz110
Piquero, A. R., Riddell, J. R., Bishopp, S. A., Narvey, C., Reid, J. A., & Piquero, N. L. (2020). Staying Home, Staying Safe? A Short-Term Analysis of COVID-19 on Dallas Domestic Violence. American Journal of Criminal Justice, 45(4), 601–635. https://doi.org/10.1007/s12103-020-09531-7
Piquero, A. R., Jennings, W. G., Jemison, E., Kaukinen, C., & Knaul, F. M. (2021). Evidence from a systematic review and meta-analysis. Journal of Criminal Justice. https://doi.org/10.1016/j.jcrimjus.2021.101806
Sato, H., & Kawahara, J.-I. (2011). Selective bias in retrospective self-reports of negative mood states. Anxiety, Stress & Coping, 24(4), 359–367. https://doi.org/10.1080/10615806.2010.543132
Schneider, S., & Stone, A. A. (2015). Ambulatory and diary methods can facilitate the measurement of patient-reported outcomes. Quality of Life Research, 25(3), 497–506. https://doi.org/10.1007/s11136-015-1054-z
Schumacher, J. A., Coffey, S. F., Norris, F. H., Tracy, M., Clements, K., & Galea, S. (2010). Intimate Partner Violence and Hurricane Katrina: Predictors and Associated Mental Health Outcomes. Violence and Victims, 25(5), 588–603. https://doi.org/10.1891/0886-6708.25.5.588
Simons, J. S., Wills, T. A., Emery, N. N., & Marks, R. M. (2015). Nov). Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors, 50, 205–212. https://doi.org/10.1016/j.addbeh.2015.06.042
Snijders, T. A. (2005). Power and sample size in multilevel linear models. Encyclopedia of statistics in behavioral science.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. Journal of Family Issues, 17(3), 283–316. https://doi.org/10.1177/019251396017003001
Sullivan, T. P., McPartland, T. S., Armeli, S., Jaquier, V., & Tennen, H. (2012). Is it the exception or the rule? Daily co-occurrence of physical, sexual, and psychological partner violence in a 90-day study of substance-using, community women. Psychology of Violence, 2(2), 154–164. https://doi.org/10.1037/a0027106
Team, R. (2015). RStudio: integrated development for R. RStudio. Inc., Boston, MA, 700.
Teitcher, J. E. F., Bockting, W. O., Bauermeister, J. A., Hoefer, C. J., Miner, M. H., & Klitzman, R. L. (2015). Detecting, Preventing, and Responding to “Fraudsters” in Internet Research: Ethics and Tradeoffs. The Journal of Law, Medicine & Ethics, 43(1), 116–133. https://doi.org/10.1111/jlme.12200
Whitaker, C., Stevelink, S., & Fear, N. (2017). The Use of Facebook in Recruiting Participants for Health Research Purposes: A Systematic Review. Journal of Medical Internet Research, 19(8). https://doi.org/10.2196/jmir.7071
Wiglesworth, A., Mosqueda, L., Mulnard, R., Liao, S., Gibbs, L., & Fitzgerald, W. (2010). Screening for abuse and neglect of people with dementia. Journal of the American Geriatrics Society, 58(3), 493–500. https://doi.org/10.1111/j.1532-5415.2010.02737.x
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pickering, C.E.Z., Maxwell, C.D., Yefimova, M. et al. Early Stages of COVID-19 Pandemic Had No Discernable Impact on Risk of Elder Abuse and Neglect Among Dementia Family Caregivers: A Daily Diary Study. J Fam Viol 38, 965–975 (2023). https://doi.org/10.1007/s10896-022-00392-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-022-00392-8