Abstract
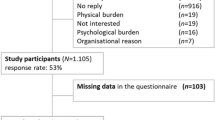
Sexual health concerns are one of the most common late effects facing hematopoietic stem cell transplant (HSCT) survivors. The current study tested whether self-reported depression and anxiety symptoms before transplant were associated with embedded items assessing two specific areas of sexual health—sexual interest and sexual satisfaction—one year post-HSCT. Of the 158 study participants, 41% were diagnosed with a plasma cell disorder (n = 60) and most received autologous transplantation (n = 128; 81%). At post-HSCT, 21% of participants reported they were not at all satisfied with their sex life, and 22% were not at all interested in sex. Greater pre-HSCT depressive symptomology was significantly predictive of lower sexual interest (β = −.27, p < .001) and satisfaction (β = −.39, p < .001) at post-HSCT. Similarly, greater pre-HSCT trait anxiety was significantly predictive of lower sexual interest (β = −.19, p = .02) whereas higher levels of state and trait anxiety were both predictive of lower satisfaction (β = −.22, p = .02 and β = −.29, p = .001, respectively). Participant sex significantly moderated the relationship between state anxiety and sexual satisfaction (b = −.05, t = −2.03, p = .04). Additional research examining the factors that contribute to sexual health post-HCST is needed to inform and implement clinical interventions to address these commonly overlooked survivorship concerns.

Similar content being viewed by others
Data Availability
Data may be available upon request to the corresponding author.
Notes
Of note, these are presumed to be cisgender samples. Cisgender men are individuals who were assigned male sex at birth and identify as men, whereas cisgender women were assigned female sex at birth and identify their gender as women. We have elected to retain language used by the original publications being cited, while recognizing that many such studies do not actually assess gender, rather infer gender based on sex assigned at birth. The inappropriate conflation of anatomical sex and gender is a major limitation of the existing literature and state of the science. Johnson and colleagues provide an excellent discussion of this longstanding barrier in health-focused research.17 (Johnson, Greaves, & Repta, 2009).
Relevant professional organizations include: the American Association of Sexuality Educators, Counselors and Therapists (AASECT), The International Society for Sexual Medicine (ISSM), The International Society for the Study of Women's Sexual Health (ISSWSH), and The Scientific Network on Female Sexual Health and Cancer.
References
American College of Surgeons. (2020). Optimal Resources for Cancer Care: 2020 Standards. In. Chicago, IL.
Amonoo, H. L., Massey, C. N., Freedman, M. E., El-Jawahri, A., Vitagliano, H. L., Pirl, W. F., & Huffman, J. C. (2019). Psychological considerations in hematopoietic stem cell transplantation. Psychosomatics, 60(4), 331–342. https://doi.org/10.1016/j.psym.2019.02.004
Auner, H., Szydlo, R., Hoek, J., Goldschmidt, H., Stoppa, A., Morgan, G., & Russell, N. (2015). Trends in autologous hematopoietic cell transplantation for multiple myeloma in Europe: Increased use and improved outcomes in elderly patients in recent years. Bone Marrow Transplantation, 50(2), 209–215.
Beck, A., Steer, R., & Brown, G. (1996). Manual for the Beck Depression Inventory, (BDI-II) San Antonio. The Psychological Association.
Bevans, M., El-Jawahri, A., Tierney, D. K., Wiener, L., Wood, W. A., Hoodin, F., & Syrjala, K. L. (2017). National Institutes of health hematopoietic cell transplantation late effects initiative: The patient-centered outcomes working group report. Biology of Blood Marrow Transplantation, 23(4), 538–551. https://doi.org/10.1016/j.bbmt.2016.09.011
Bossio, J. A., Miller, F., O’Loughlin, J. I., & Brotto, L. A. (2019). Sexual health recovery for prostate cancer survivors: The proposed role of acceptance and mindfulness-based interventions. Sexual Medicine Reviews, 7(4), 627–635.
Burns, L. J., Abbetti, B., Arnold, S. D., Bender, J., Doughtie, S., El-Jawahiri, A., & Denzen, E. M. (2018). Engaging patients in setting a patient-centered outcomes research agenda in hematopoietic cell transplantation. Biology of Blood Marrow Transplantation, 24(6), 1111–1118. https://doi.org/10.1016/j.bbmt.2018.01.029
Carcedo, R. J., Fernández-Rouco, N., Fernández-Fuertes, A. A., & Martínez-Álvarez, J. L. (2020). Association between sexual satisfaction and depression and anxiety in adolescents and young adults. International Journal of Environmental Research and Public Health, 17(3), 841.
Costanzo, E. S., Juckett, M. B., & Coe, C. L. (2013). Biobehavioral influences on recovery following hematopoietic stem cell transplantation. Brain, Behavior and Immunity, 30(Suppl), S68-74. https://doi.org/10.1016/j.bbi.2012.07.005
Coyle, R. M., Lampe, F. C., Miltz, A. R., Sewell, J., Anderson, J., Apea, V., & Lascar, M. (2019). Associations of depression and anxiety symptoms with sexual behaviour in women and heterosexual men attending sexual health clinics: A cross-sectional study. Sexually Transmitted Infections, 95(4), 254–261.
Crean-Tate, K. K., Faubion, S. S., Pederson, H. J., Vencill, J. A., & Batur, P. (2020). Management of genitourinary syndrome of menopause in female cancer patients: A focus on vaginal hormonal therapy. American Journal of Obstetrics and Gynecology, 222(2), 103–113. https://doi.org/10.1016/j.ajog.2019.08.043
D’Souza, A., Fretham, C., Lee, S. J., Arora, M., Brunner, J., Chhabra, S., & Hari, P. (2020). Current use of and trends in hematopoietic cell transplantation in the United States. Biology of Blood and Marrow Transplantation, 26(8), e177–e182.
El-Jawahri, A., Chen, Y. B., Brazauskas, R., He, N., Lee, S. J., Knight, J. M., & Wirk, B. M. (2017). Impact of pre-transplant depression on outcomes of allogeneic and autologous hematopoietic stem cell transplantation. Cancer, 123(10), 1828–1838.
Field, N., Prah, P., Mercer, C. H., Rait, G., King, M., Cassell, J. A., & Clifton, S. (2016). Are depression and poor sexual health neglected comorbidities? Evidence from a population sample. BMJ Open, 6(3), e010521.
Gilbert, E., Perz, J., & Ussher, J. M. (2016). Talking about sex with health professionals: The experience of people with cancer and their partners. European Journal of Cancer Care, 25(2), 280–293.
Gorman, J. R., Drizin, J. H., Al-Ghadban, F. A., & Rendle, K. A. (2021). Adaptation and feasibility of a multimodal mindfulness-based intervention to promote sexual health in cancer survivorship. Translational Behavioral Medicine, 11(10), 1885–1895.
Hartmann, U. (2007). Depression and sexual dysfunction. Journal of Men’s Health and Gender, 4(1), 18–25.
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications.
Humphreys, C., Tallman, B., Altmaier, E., & Barnette, V. (2007). Sexual functioning in patients undergoing bone marrow transplantation: A longitudinal study. Bone Marrow Transplantation, 39(8), 491–496.
Johnson, J. L., Greaves, L., & Repta, R. (2009). Better science with sex and gender: Facilitating the use of a sex and gender-based analysis in health research. International Journal for Equity in Health, 8, 14. https://doi.org/10.1186/1475-9276-8-14
Kalmbach, D. A., Pillai, V., Kingsberg, S. A., & Ciesla, J. A. (2015). The transaction between depression and anxiety symptoms and sexual functioning: A prospective study of premenopausal, healthy women. Archives of Sexual Behavior, 44, 1635–1649.
Kelly, D. L., Syrjala, K., Taylor, M., Rentscher, K. E., Hashmi, S., Wood, W. A., & Burns, L. J. (2021). Biobehavioral research and hematopoietic stem cell transplantation: Expert review from the biobehavioral research special interest group of the American society for transplantation and cellular therapy. Transplantation and cellular therapy, 27(9), 747–757.
Lazenby, M., Ercolano, E., Grant, M., Holland, J. C., Jacobsen, P. B., & McCorkle, R. (2015). Supporting commission on cancer-mandated psychosocial distress screening with implementation strategies. Journal of Oncology Practice/ American Society of Clinical Oncology, 11(3), e413-420. https://doi.org/10.1200/jop.2014.002816
Li, Z., Mewawalla, P., Stratton, P., Yong, A. S., Shaw, B. E., Hashmi, S., & Savani, B. N. (2015). Sexual health in hematopoietic stem cell transplant recipients. Cancer, 121(23), 4124–4131.
Loberiza, F. R., Jr., Rizzo, J. D., Bredeson, C. N., Antin, J. H., Horowitz, M. M., Weeks, J. C., & Lee, S. J. (2002). Association of depressive syndrome and early deaths among patients after stem-cell transplantation for malignant diseases. Journal of Clinical Oncology, 20(8), 2118–2126. https://doi.org/10.1200/jco.2002.08.757
McQuellon, R. P., Russell, G. B., Cella, D. F., Craven, B. L., Brady, M., Bonomi, A., & Hurd, D. D. (1997). Quality of life measurement in bone marrow transplantation: Development of the functional assessment of cancer therapy-bone marrow transplant (FACT-BMT) scale. Bone Marrow Transplantation, 19(4), 357–368. https://doi.org/10.1038/sj.bmt.1700672
Molassiotis, A. (1997). Psychosocial transitions in the long-term survivors of bone marrow transplantation. European Journal of Cancer Care, 6(2), 100–107.
Mosher, C. E., Redd, W. H., Rini, C. M., Burkhalter, J. E., & DuHamel, K. N. (2009). Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: A review of the literature. Psycho-Oncology, 18(2), 113–127. https://doi.org/10.1002/pon.1399
Nørskov, K. H., Schmidt, M., & Jarden, M. (2015). Patients’ experience of sexuality 1-year after allogeneic haematopoietic stem cell transplantation. European Journal of Oncology Nursing, 19(4), 419–426.
Oken, M. M., Creech, R. H., Tormey, D. C., Horton, J., Davis, T. E., McFadden, E. T., & Carbone, P. P. (1982). Toxicity and response criteria of the Eastern cooperative oncology group. American Journal of Clinical Oncology, 5(6), 649–655.
Perz, J., Ussher, J. M., & Gilbert, E. (2014). Feeling well and talking about sex: Psycho-social predictors of sexual functioning after cancer. BMC Cancer, 14(1), 1–19.
Phelan, R., Im, A., Hunter, R. L., Inamoto, Y., Lupo-Stanghellini, M. T., Rovo, A., & Murthy, H. S. (2022). Male-specific late effects in adult hematopoietic cell transplantation recipients: A systematic review from the late effects and quality of life working committee of the center for international blood and marrow transplant research and transplant complications working party of the European society of blood and marrow transplantation. Bone Marrow Transplantation, 57, 1150–1163.
Prieto, J. M., Atala, J., Blanch, J., Carreras, E., Rovira, M., Cirera, E., & Gastó, C. (2005). Patient-rated emotional and physical functioning among hematologic cancer patients during hospitalization for stem-cell transplantation. Bone Marrow Transplantation, 35(3), 307–314. https://doi.org/10.1038/sj.bmt.1704788
Schover, L. R., van der Kaaij, M., van Dorst, E., Creutzberg, C., Huyghe, E., & Kiserud, C. E. (2014). Sexual dysfunction and infertility as late effects of cancer treatment. European Journal of Cancer Supplements, 12(1), 41–53.
Shen, H., Chen, M., & Cui, D. (2020). Biological mechanism study of meditation and its application in mental disorders. General Psychiatry, 33(4), e100214.
Smith, S. K., Loscalzo, M., Mayer, C., & Rosenstein, D. L. (2018). Best practices in oncology distress management: Beyond the screen. American Society of Clinical Oncology Educational Book, 38, 813–821. https://doi.org/10.1200/edbk_201307
Smith, T., Kingsberg, S. A., & Faubion, S. (2022). Sexual dysfunction in female cancer survivors: Addressing the problems and the remedies. Maturitas, 165, 52–57. https://doi.org/10.1016/j.maturitas.2022.07.010
Sopfe, J., Pettigrew, J., Afghahi, A., Appiah, L. C., & Coons, H. L. (2021). Interventions to improve sexual health in women living with and surviving cancer: Review and recommendations. Cancers, 13(13), 3153.
Spielberger, C. D. (1983). State-trait anxiety inventory for adults.
Spielberger, C. D., & Reheiser, E. C. (2003). Measuring anxiety, anger, depression, and curiosity as emotional states and personality traits with the STAI. Comprehensive Handbook of Psychological Assessment, 2, 70.
Syrjala, K. L., Kurland, B. F., Abrams, J. R., Sanders, J. E., & Heiman, J. R. (2008). Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood, the Journal of the American Society of Hematology, 111(3), 989–996.
Syrjala, K. L., Schoemans, H., Yi, J. C., Langer, S. L., Mukherjee, A., Onstad, L., & Lee, S. J. (2021). Sexual functioning in long-term survivors of hematopoietic cell transplantation. Transplantation and Cellular Therapy, 27(1), 80.e81-80.e12. https://doi.org/10.1016/j.bbmt.2020.09.027
Thygesen, K., Schjødt, I., & Jarden, M. (2012). The impact of hematopoietic stem cell transplantation on sexuality: A systematic review of the literature. Bone Marrow Transplantation, 47(5), 716–724.
Tierney, D. K. (2004). Sexuality following hematopoietic cell transplantation. Clinical Journal of Oncology Nursing, 8(1), 43–47.
Ussher, J. M., Perz, J., & Gilbert, E. (2015). Perceived causes and consequences of sexual changes after cancer for women and men: A mixed method study. BMC Cancer, 15(1), 1–18.
Utz, A. L., & Jagasia, S. (2013). Sexual dysfunction in long-term survivors: Monitoring and management. Blood and marrow transplantation long-term management: Prevention and complications (pp. 183–192). Wiley.
Varela, V. S., Zhou, E. S., & Bober, S. L. (2013). Management of sexual problems in cancer patients and survivors. Current Problems in Cancer, 37(6), 319–352.
Wang, Y. P., & Gorenstein, C. (2013). Psychometric properties of the beck depression inventory-II: A comprehensive review. Brazilian Journal of Psychiatry, 35(4), 416–431. https://doi.org/10.1590/1516-4446-2012-1048
Yi, J. C., & Syrjala, K. L. (2009). Sexuality after hematopoietic stem cell transplantation. Cancer Journal, 15(1), 57–64. https://doi.org/10.1097/PPO.0b013e318198c758
Funding
This work was made possible by Grant KL2 RR 02415 (PI: Ehlers), CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Contributions
SE, CP, and DG designed the study. SE, TB, and CH contributed to the acquisition of data. JK and KM analyzed the data. JV, JK, SE, KM, CP, ES, and KC interpreted the data. JV, JK, SE, and KM drafted the manuscript. All authors critically revised the manuscript. All authors have read the manuscript and have agreed with its submission.
Corresponding author
Ethics declarations
Conflict of interests
Jennifer A. Vencill, Janae L. Kirsch, Keagan McPherson, Eric Sprankle, Christi A. Patten, Kristie Campana, Tabetha Brockman, Carrie Bronars, Christine Hughes, Dennis Gastineau, and Shawna L. Ehlers have no conflicts of interest to report.
Ethical Approval
This study was conducted in accordance with institutional review board policies and all participants provided informed consent (IRB: 08-006915).
Consent to Participate
Participants provided written, informed consent.
Consent to Publish
Participants signed informed consent and data is presented in aggregate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vencill, J.A., Kirsch, J.L., McPherson, K. et al. Prospective Association of Psychological Distress and Sexual Quality of Life Among Hematopoietic Stem Cell Transplant Survivors. J Clin Psychol Med Settings (2024). https://doi.org/10.1007/s10880-024-10013-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10880-024-10013-9