Abstract
Parents with infants in the neonatal intensive care unit (NICU) experience high levels of stress, anxiety, and depression. Mindfulness and relaxation-based interventions are effective in reducing distress in the general postpartum population. The aim of this systematic review was to evaluate whether mindfulness and/or relaxation-based interventions reduce stress, anxiety, and depression in NICU parents. A total of five studies met the inclusion criteria and were assessed for quality using the Downs & Black Checklist. The most consistent results in this review suggest that mindfulness and/or relaxation-based interventions may be effective at reducing anxiety symptoms in NICU parents, with moderate to large effect sizes, and show promise in reducing depressive symptoms. The findings show limited potential benefits on parental stress. Methodological weaknesses, heterogeneous intervention factors (including format and length), and varying participant adherence hinder the ability to make strong conclusions. Directions for future research are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, approximately 15 million infants are born preterm each year (Liu et al., 2016), and an estimated 50% or more may require care in a neonatal intensive care unit (NICU), a specialist service that is designed and equipped to care for very small or very unwell infants (Phaloprakarn et al., 2015). Parents of infants in the NICU experience increased stress due to a range of factors, including the NICU environment (Turner et al., 2015), disruptions in the parental role, feelings of powerlessness (Lean et al., 2018), witnessing distressing medical procedures performed on their infant (Obeidat et al., 2009), and logistical challenges around finances, childcare for older siblings, and time management (Turner et al., 2015).
Subsequently, parents of infants in the NICU experience higher rates of anxiety, depression, acute stress disorder, and post-traumatic stress disorder (PTSD) than the general postpartum population (Lean et al., 2018; Shaw et al., 2014; Turner et al., 2015). Prevalence studies in the NICU have found striking differences in these rates: 24.7% of NICU mothers experienced anxiety compared to 7.4 to 8.7% in the general maternal population (Lotterman et al., 2019); 39% of NICU parents had postpartum depression compared to 10 to 15% of non-NICU parents (Lefkowitz et al., 2010); and 18.5% of NICU parents met criteria for PTSD compared with 4% in the broader adult population (Yildiz et al., 2017). There are also longer-term adverse effects of the NICU experience after discharge, including impaired parenting and parent–child dyad disruptions in bonding and attachment (Lean et al., 2018).
Interventions for NICU Parents
A diverse range of psychological interventions have been developed to improve mental health outcomes for NICU parents. A 2019 systematic review and meta-analysis sought to assess the effectiveness of a wide range of interventions, from psychotherapy to acupuncture, among parents with infants in NICU (Sabnis et al., 2019). This review found that family-centered care was associated with the most significant reduction in parental distress in the NICU, and it also noted that alternative/complementary interventions, including relaxation and meditation, showed early promise (Sabnis et al., 2019). This conclusion was similar to a previous review that focused on maternal mental health in the NICU, which noted that mindfulness-based strategies may be useful for reducing depression and anxiety symptoms (Mendelson et al., 2017).
The Mind–Body Medicine Framework
Mindfulness-based interventions (MBIs) and relaxation-based interventions are considered similar but different components of mind–body medicine (Kabat-Zinn, 2005), an evidence-based framework focused on the interactions between the mind, body, and behavior (Luberto et al., 2020). However, the terms mindfulness and relaxation have been used interchangeably in clinical intervention research in the last four decades in part because the two approaches use a combination of overlapping skills, such as deep breathing and visualization, in their often multi-modal interventions (Luberto et al., 2020). Both approaches have been found to be effective at reducing symptoms of anxiety and depression, among other mental health conditions (Jain et al., 2007; Luberto et al., 2020).
Despite the similarities, MBIs and relaxation-based interventions differ in notable theoretical ways. MBIs seek to increase distress tolerance and teach acceptance (not change) of emotions and physical sensations (Kabat-Zinn, 2005). Relaxation techniques, however, actively attempt to reduce distress (Rausch et al., 2006). Achieving both of these goals can be useful in highly stressed populations, and that may be why mindfulness and relaxation-based skills are often combined into multi-modality intervention programs in medical settings (Luberto et al., 2020). Given the changing definition of these terms over time, both MBIs and relaxation-based interventions were included in this systematic review.
Mindfulness-Based Interventions (MBIs)
MBIs use the core tenets of mindfulness, which seek to intentionally increase awareness of the present moment, non-judgmentally, and sustain this attention over time (Kabat-Zinn, 2005). Stemming from Buddhist meditative practices, MBIs have been implemented in many clinical settings due in significant part to the success of the multi-week Mindfulness-Based Stress Reduction (MBSR) program, which utilizes a combination of meditation, breathing, and gentle movement components. Developed by Jon Kabat-Zinn and colleagues at the University of Massachusetts Medical School, MBSR is now delivered at more than 200 medical centers around the world (Niazi & Niazi, 2011) and has been shown to be effective in reducing symptoms of stress, PTSD, anxiety, depression, and chronic pain in adolescent and adult populations (Grossman et al., 2004).
Relaxation-Based Interventions
Relaxation-based interventions are used to reduce the activation of the sympathetic nervous system (e.g., the “fight or flight” response) and increase the response of the parasympathetic nervous system (e.g., the “rest and digest” response) (Ma et al., 2017). Practices focus on decreasing arousal and increasing a sense of calm, often through slowing the breath, tensing and relaxing the muscles, or focusing the mind on positive mental experiences (Luberto et al., 2020).
Research into MBIs and relaxation-based interventions has grown exponentially in the last two decades, due in part to their relatively low-cost and ease of delivery (Perrier et al., 2020). Some of the most common techniques, which are often paired together in multi-modal intervention programmes, are detailed in brief below.
Deep Breathing
Diaphragmatic breathing, also referred to as deep breathing, focuses on contracting the diaphragm, deepening and slowing the rate of inhalation and exhalation, and expanding the abdomen (Ma et al., 2017). This type of breathing has been found to lead to reductions in anxiety, stress, and symptoms of PTSD (Colgan et al., 2016). Deep breathing can also be effective at improving cognitive functioning during stressful situations, such as university exams (Paul et al., 2007).
Progressive Muscle Relaxation (PMR)
PMR involves taking deep breaths while tightening, holding, and relaxing different muscle groups throughout the body in a progressive order, often beginning at the head and working down to the feet (Liu et al., 2020). Originally developed by Edmund Jacobson in 1938 to stimulate a relaxation response in the body (Hughes et al., 2013), PMR has been found to be effective at reducing anxiety symptoms and improving sleep in a wide range of studies and populations, including pregnant women (Rajeswari & Sanjeeva, 2019), cancer patients (Gok et al., 2019), and hospitalized COVID-19 patients (Liu et al., 2020).
Guided Imagery
Guided imagery uses external guidance to prompt internal visualization of images intended to improve positive affect (Hart, 2008; Rossman, 2000). Research has tested guided imagery with a broad range of populations, including adults diagnosed with a generalized anxiety disorder (Nguyen & Brymer, 2018), women with breast cancer (Kolcaba & Fox, 1999), and hospitalized psychiatric patients (Apostolo & Kolcaba, 2009) and reported reductions in symptoms of anxiety, depression, and stress, among other conditions.
Rationale and Aim of Current Review
The effects of MBIs and/or relaxation-based interventions on NICU parents have not been broadly studied (Mendelson et al., 2017), and no systematic review has been published to date that focuses exclusively on this topic. However, there is a large body of evidence that supports these types of interventions to reduce symptoms of anxiety, depression, and stress in adult populations (Niazi & Niazi, 2011), and a small but growing group of literature showing support for NICU parents (Sabnis et al., 2019). Additionally, many existing intervention programs for NICU parents can be complex to deliver and costly to acquire (Sabnis et al., 2019). Mindfulness and relaxation-based interventions, however, may offer cost-effective alternatives (Saha et al., 2020), making them potentially more viable options in NICU settings with limited funding and staff resources.
Therefore, this systematic review assesses MBIs and relaxation-based interventions used in the NICU to reduce parental stress, anxiety, and depression. This review was undertaken to achieve the following aims: (1) to characterize the populations, interventions, delivery methods, and outcomes reported in peer-reviewed studies; (2) to estimate the overall effectiveness of interventions on parental stress, anxiety, and depression during NICU hospitalization and secondary outcomes such as breastfeeding measures; and (3) explore any differences in outcomes by delivery method (e.g., pre-recorded vs in-person).
Methods
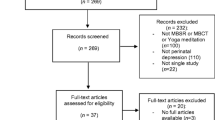
This review was performed per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021) and registered with the International Prospective Register of Systematic Reviews (PROSPERO registration number 2021 CRD42021247715).
Study Design
MedLine(OVID), PsycINFO, Embase, SCOPUS, Cochrane Library, and CINAHL Plus were searched using search terms (and synonyms) related to the intervention and setting including: mindfulness, relaxation therapy, guided imagery, meditation, Acceptance and Commitment Therapy (ACT), MBSR, NICU, intensive care, preterm, neonate. (See Appendix for the full search strategy). The search was restricted to studies published in English and in peer-reviewed journals, with no limits on the date of publication. No terms for the specified population or outcomes were included to ensure all possible studies were identified. Bibliographies of included studies, review papers, and conference abstracts were hand-searched to identify potential additional items. The database search was conducted between March 22 and March 31, 2021.
Study Selection and Eligibility Criteria
All published studies (randomized trials and observational cohort studies including pre-post study designs) were included that were conducted in a NICU in any country and (1) reported one or more of this review’s primary and/or secondary outcomes using standardized measurement tools and (2) compared parents who received mindfulness or relaxation-based intervention with parents who received either another intervention or standard care or (3) studies that delivered the experimental intervention and conducted pre- and post-intervention measurements on the same group of parents. Case series, conference abstracts, and qualitative studies were excluded.
Mindfulness or relaxation-based interventions were defined as those using a psychological approach in order to reduce psychological stress, increase awareness of the present moment, or as defined by the study authors. Examples included deep breathing/diaphragmatic breathing, guided imagery, and progressive muscle relaxation. Multi-modal intervention programs that included mindfulness or relaxation skills and other components such as parenting education or psychological therapy were excluded. Interventions that involved non-psychological specialized treatments such as music therapy or art therapy were also excluded.
Risk of Study Bias
Risk of bias and overall quality for each included study was assessed using the Downs and Black Checklist (D&B) (Downs & Black, 1998), designed for use with randomized and non-randomized intervention research. This checklist assesses the following domains for bias: reporting results, external validity, confounding factors, internal bias, and power analysis. Two researchers (KHG and MA) independently performed the risk of bias assessments. Conflicts were discussed and resolved by consensus. Scores were tallied to create a quality score with the ranges of excellent (26–28); good (20–25); fair (15–19); and poor (≤ 14) (Downs & Black, 1998).
Outcomes
The primary outcomes were parental stress, anxiety, and/or depression. These outcomes, as defined by the study authors, were assessed through the use of a wide range of standardized screening tools. The secondary outcomes were breastfeeding measures defined by the quantity of expressed breast milk, exclusive breastfeeding on discharge from the NICU, or as defined by authors.
Data Extraction
Search results were exported into Endnote V9 and duplicate articles were removed. The primary researcher (KHG) conducted the database search, and then records were screened by title, abstract, and full-text by two researchers (KHG and MA) for inclusion or exclusion using the software program Rayyan, a free, commonly used web-based tool recommended for the screening stage of systematic reviews (Kellermeyer et al., 2018). Disagreements about inclusion were resolved through a discussion between two researchers.
Data Synthesis
Owing to study heterogeneity and the small sample of included studies, formal meta-analyses were not attempted. A narrative synthesis was conducted with the information presented in text and tables to describe the characteristics and reported the effectiveness of included studies. The narrative synthesis explored findings within and among included studies.
Results
Study selection is illustrated in Fig. 1. Through database searches and hand searches, 334 records were identified. Of those, 213 duplicates were removed. Of the remaining 121 records, title and abstract reviews excluded 66 articles, and an additional 52 were excluded after full-text review. Thus, five studies were included in this review.
Characteristics of Included Studies
The five studies included in this review included 226 parents (Table 1), with individual study sample sizes that ranged from 20 to 71 parents. Overall, mothers made up the majority of the reported sample (more than 90%), with just one study including fathers (Marshall et al., 2019). Only three studies reported the race or ethnicity of participants (Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018), and of those, the majority (61%) were Caucasian. The mean age of participants across all studies was 28.65 years old (SD = 1.66). The majority of studies were published in the last decade, from 2013 to 2019 (Dabas et al., 2019; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018), while one study was published in the 1980s (Feher et al., 1989). Four were conducted in the U.S. (Feher et al., 1989; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018) and one in India (Dabas et al., 2019).
Half of these studies were labeled “pilot study” (Marshall et al., 2019; Mendelson et al., 2018) or “feasibility study” (Howland et al., 2017). Two of the studies were RCTs (Dabas et al., 2019; Feher et al., 1989).
Risk of Bias Quality Assessment
Across all studies, the mean risk of bias score was 18.4 (SD 1.95) out of a maximum score of 28, which is moderate in quality (Table 2). Only one study, an RCT, received a risk of bias score of “good” (Dabas et al., 2019), with the other four studies receiving scores of “fair” (Feher et al., 1989; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018). Most studies scored poorly on external validity (M = 1, out of a maximum score of 3, SD = .70) and the internal validity-confounding category (M = 3.4, out of a maximum score of 6, SD = 1.14). There was a notable absence across all studies in reporting a power analysis.
Intervention Characteristics
Program Descriptions
None of the studies followed a standardized program such as MBSR, and instead, each used researcher-created, custom programs of mindfulness and/or relaxation techniques (Table 3). Most studies combined multiple skills into their intervention programs, with two studies using only one technique (Howland et al., 2017; Mendelson et al., 2018). Breathing exercises, guided imagery, and meditation were most commonly used (Table 4).
Delivery Methods
Delivery methods of interventions ranged from a combination of in-person and pre-recorded materials to fully pre-recorded via video or audio recordings (Table 3). Four studies used pre-recorded intervention delivery exclusively.
Intervention Dose, Duration, and Frequency
Intervention dose, duration, and frequency varied widely across studies. Three studies employed intervention sessions of 20-min in length (Feher et al., 1989; Howland et al., 2017; Mendelson et al., 2018) and two ranged from 30- to 60-min (Dabas et al., 2019; Marshall et al., 2019). Participants were asked to use the intervention daily in all studies, and prescribed intervention time periods ranged from 7 days (Feher et al., 1989), to 8 weeks (Howland et al., 2017). One study asked participants to use the intervention throughout their infant’s hospital admission, with an average admission length of 72 days (SD = 42) (Marshall et al., 2019).
Four studies reported data on participants’ compliance with intervention usage recommendations (Feher et al., 1989; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018). Most reported low compliance, with one study reporting that 50% of participants used the intervention at least five times, out of a prescribed minimum of seven times (Feher et al., 1989). Another study reported similar compliance rates, with a mean intervention use of 4.46 times per week (SD = 1.1) instead of the recommended seven times per week (Howland et al., 2017).
Outcome Measures
There were 19 different measurement scales used across studies, including the Parental Stress Scale: Neonatal Intensive Care Unit (PSS:NICU) and the State–Trait Anxiety Inventory (STAI). The most frequently used scale was the PSS:NICU (Dabas et al., 2019; Marshall et al., 2019; Mendelson et al., 2018). Other measurement tools used across studies included salivary cortisol concentrations (Howland et al., 2017), and expressed breast milk volume (Dabas et al., 2019; Feher et al., 1989).
Outcome Results
Primary Outcomes
In total, three studies reported significant between groups findings on primary outcome measures (Dabas et al., 2019; Feher et al., 1989; Mendelson et al., 2018) (Table 5). Four studies measured stress (Dabas et al., 2019; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018), three measured anxiety (Dabas et al., 2019; Howland et al., 2017; Mendelson et al., 2018), and two measured depression (Howland et al., 2017; Mendelson et al., 2018).
Of the four studies that measured stress as a primary outcome, two studies, one RCT (Dabas et al., 2019) and one non-RCT (Mendelson et al., 2018), reported significant reductions between groups, with moderate (d = 0.60) (Mendelson et al., 2018) and large effect sizes (d = 1.27) (Dabas et al., 2019).
Three studies measured anxiety, and one RCT (Dabas et al., 2019) and one non-RCT (Mendelson et al., 2018) reported significant reductions in anxiety symptoms with effect sizes ranging from moderate (d = 0.55) (Mendelson et al., 2018) to large (d = 0.88) (Dabas et al., 2019). Additionally, two studies measured depression, and one non-RCT (Mendelson et al., 2018) reported significant reductions in depressive symptoms with a moderate effect size (d = 0.55).
Secondary Outcomes
Two RCTs assessed breastfeeding measures (Dabas et al., 2019; Feher et al., 1989), and both found significant increases in expressed breast milk quantity after the relaxation-based intervention with moderate effect sizes (d = 0.64 and 0.72, respectively). Some studies assessed other outcomes beyond the focus of this review, including trauma symptoms (Mendelson et al., 2018) and mother-infant bonding (Howland et al., 2017).
Outcomes by Intervention Delivery Method
Four studies used fully pre-recorded intervention delivery methods (Dabas et al., 2019; Feher et al., 1989; Howland et al., 2017; Mendelson et al., 2018). Of these, three had statistically significant results between groups, with two (Dabas et al., 2019; Mendelson et al., 2018) reporting meaningful results in four outcome measures (stress, anxiety, depression, and expressed breast milk output). Both of these studies used pre-recorded materials to deliver an introductory session to participants; after that, one provided MP3 recordings for participants to use daily (Mendelson et al., 2018) while the other played pre-recorded audio every evening at a scheduled time in the NICU (Dabas et al., 2019). The third study provided a pre-recorded audio tape to participants and reported significant improvements in expressed breast milk output (Feher et al., 1989).
Discussion
This review systematically assessed whether mindfulness and/or relaxation-based interventions are effective for reducing stress, anxiety, and/or depressive symptoms in parents with infants in the NICU. The evidence presented is mixed, with a diverse range of study designs, intervention programs, and measurement tools used across studies.
The most consistent evidence in this review suggests that mindfulness and/or relaxation-based interventions may be effective at reducing anxiety symptoms in NICU parents, with moderate to large effect sizes. This is similar to previous research, which found MBIs led to moderate to large reductions in anxiety symptoms in perinatal women (Shi & MacBeth, 2017).
The evidence is weaker for the effect on parental stress in the NICU, with one RCT (Dabas et al., 2019) and one non-RCT (Mendelson et al., 2018) out of four studies (Dabas et al., 2019; Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018) reporting significant reductions. A variety of factors may have influenced these results, including the use of the PSS:NICU scale in three out of four of these studies (Dabas et al., 2019; Marshall et al., 2019; Mendelson et al., 2018), which measures stress specific to the NICU-environment and does not measure potential effects of the intervention on sources of stress outside of the hospital.
The results of mindfulness and/or relaxation-based interventions on depression are also mixed. Out of two studies that included depression as a primary outcome (Howland et al., 2017; Mendelson et al., 2018), one non-RCT (Mendelson et al., 2018) reported significant reductions in depressive symptoms with moderate effect sizes. Previous studies in other settings have supported the use of MBIs to treat depression, finding MBI programs to be effective at reducing depressive symptoms in postpartum mothers (Pan et al., 2019) and the general adult population (Hofmann et al., 2010). Therefore, further study is merited to assess the effectiveness of mindfulness and/or relaxation-based interventions on parental depressive symptoms in the NICU.
This review shows initial support for the use of relaxation-based interventions to increase expressed breast milk output. The two RCTs that assessed this secondary outcome (Dabas et al., 2019; Feher et al., 1989) reported significant increases in expressed breast milk quantity after intervention use with moderate effect sizes. This finding aligns with previous research that has suggested psychological distress hinders the body’s breast milk “let-down” reflex, and reductions in maternal distress may improve breastfeeding outcomes (Mohd Shukri et al., 2018). This is of importance as premature infants who receive human milk have lower risks of short- and long-term adverse outcomes, including developmental and neurocognitive delays, chronic lung disease, and rehospitalization after NICU discharge (Meier et al., 2010).
Mindfulness and relaxation-based interventions were of interest in this review in part because they are relatively simple to learn, can take as little as 10-min per day to perform, and may not require extensive training to deliver. These are important considerations in the NICU, where parents and staff are often time-constrained and under significant stress (Mendelson et al., 2017). In this review, four studies used a pre-recorded delivery method exclusively, with no intervention dose lasting longer than 30 min (Dabas et al., 2019; Feher et al., 1989; Howland et al., 2017; Mendelson et al., 2018). Notably, three of these studies reported significant results across four outcome categories (stress, anxiety, depression, and expressed breast milk output) (Dabas et al., 2019; Feher et al., 1989; Mendelson et al., 2018). These findings are consistent with previous research showing electronic MBIs had a small but significant effect on reducing depressive and anxiety symptoms and a moderate effect on lowering stress in adult populations (Spijkerman et al., 2016).
Implications for Clinical Psychology
This review highlights the need to support parents with infants in the NICU, who are significantly stressed and at higher risk of developing anxiety, depression, and acute stress disorders than other parents (Sabnis et al., 2019). The findings of this review suggest mindfulness and relaxation-based interventions show promise in reducing some forms of NICU parent distress, particularly anxiety. It also suggests that relaxation-based interventions may help improve breastfeeding outcomes in NICU mothers.
Importantly, these findings highlight that these types of interventions are feasible to deliver in the NICU setting and acceptable to parents. Brief, pre-recorded interventions, requiring low staff involvement, were found to deliver clinically significant reductions in symptoms. Therefore, this review provides preliminary support for incorporating mindfulness and/or relaxation-based interventions, including pre-recorded versions, into NICU programs to support parents.
Limitations and Future Research
While promising, this review’s findings should be interpreted with caution in light of a few limitations. Every study in this review used a unique, author-developed intervention program, often incorporating a range of skills, and these factors make them difficult to compare. In the future, the repeated study of manualized interventions is needed to clearly demonstrate that mindfulness and/or relaxation-based interventions are effective with NICU parents. It is also important for researchers to more clearly define the differences between MBIs and relaxation-based interventions to assess the individual effectiveness of each. Additionally, attrition rates in NICU parent studies are typically high, with average rates of 15% or more attrition (Mendelson et al., 2017), and this review found similar results (5% to 29%, M = 16%). Reporting of participants’ frequency of use of interventions across studies was also inconsistent, making it difficult to assess dosage effect.
More broadly, most studies in this review were conducted among mothers, limiting the generalizability across the parent population. This is a wider problem across studies on NICU parents, with the majority of research conducted with mothers (Sabnis et al., 2019). However, the limited research on fathers has shown that they experience similar levels of distress as mothers in the NICU (Noergaard et al., 2018; Prouhet et al., 2018), and it is promising that the study that included fathers in this review reported significant reductions in anxiety symptoms and stress levels (Dabas et al., 2019). Future mindfulness and relaxation-based studies should aim to recruit more fathers to evaluate differences in responsiveness and effectiveness.
Similarly, race or ethnicity was only reported in three of these studies (Howland et al., 2017; Marshall et al., 2019; Mendelson et al., 2018), and within those, the majority of participants were Caucasian. Because of significant gaps in data about race and ethnicity in this study group, it is difficult to generalize these findings across diverse cultures. It is also important to note that these studies relied overwhelmingly on self-report screening tools to measure outcomes, and research has found these types of tools can have problematic variations between cultures (Owais et al., 2020).
Study design was also variable in quality. While two studies were RCTs, considered the gold standard of experimental design (Armour et al., 2018), three studies included in this review used a pre-post design with the same group of parents. Using only one group of parents, few conclusions about the effect of the intervention can be drawn as stress levels are expected to reduce with time (Cavaleri et al., 2018). Additionally, the sample size was generally small across these studies, and none reported using a power calculation.
While the literature is growing on the topic of mindfulness and relaxation-based interventions in the NICU, it is still a small body of mostly pilot research. Therefore, it is recommended that future research (1) tests standardized and replicable interventions of this type on parental outcomes (such as stress, anxiety, and depression) in the NICU, (2) evaluate mindfulness and relaxation-based interventions with diverse parent populations, including fathers and those from a range of cultural backgrounds (3) improve study quality with more rigorous study design (e.g., RCTs, the use of consistent and validated measures, and adequately powered sample sizes), and (4) provide standardized outcome measurements during NICU admission as well as after discharge (e.g. three months, six months) to assess long-term effects.
To summarize, the evidence presented in this review is mixed, but shows promise in the effectiveness of mindfulness and/or relaxation-based interventions to reduce some measures of parental distress in the NICU, particularly anxiety, and to improve breastfeeding outcomes for mothers with infants in the NICU. Further studies are needed to explore whether these types of interventions are effective in reducing depressive symptoms and parental stress. Additionally, more rigorous research is needed to determine what delivery methods (e.g., in-person vs. pre-recorded) and specific modalities of mindfulness or relaxation techniques (e.g., PMR, meditation, deep breathing) are most effective to reduce distress for NICU parents.
Data Availability
Downs & Black Checklist assessments for each study are available as supplementary materials.
Code Availability
Not applicable.
References
Apostolo, J. L., & Kolcaba, K. (2009). The effects of guided imagery on comfort, depression, anxiety, and stress of psychiatric inpatients with depressive disorders. Archives of Psychiatric Nursing, 23, 403–411. https://doi.org/10.1016/j.apnu.2008.12.003
Armour, M., Ee, C., & Steiner, G. Z. (2018). Randomized controlled trials. In P. Liamputtong (Ed.), Handbook of research methods in health social sciences. Springer. https://doi.org/10.1007/978-981-10-2779-6_94-1
Cavaleri, R., Bhole, S., & Arora, A. (2018). Critical appraisal of quantitative research. In P. Liamputtong (Ed.), Handbook of research methods in health social sciences. Springer. https://doi.org/10.1007/978-981-10-2779-6_120-2
Colgan, D. D., Christopher, M., Michael, P., & Wahbeh, H. (2016). The body scan and mindful breathing among veterans with PTSD: Type of intervention moderates the relationship between changes in mindfulness and post-treatment depression. Mindfulness, 7, 372–383. https://doi.org/10.1007/s12671-015-0453-0
Dabas, S., Joshi, P., Agarwal, R., Yadav, R. K., & Kachhawa, G. (2019). Impact of audio assisted relaxation technique on stress, anxiety and milk output among postpartum mothers of hospitalized neonates: A randomized controlled trial. Journal of Neonatal Nursing, 25, 200–204.
Downs, S., & Black, N. (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions. Journal of Epidemiology Community Health, 52, 377–384.
Feher, S. D., Berger, L. R., Johnson, J. D., & Wilde, J. B. (1989). Increasing breast milk production for premature infants with a relaxation/imagery audiotape. Pediatrics, 83, 57–60.
Gok, M. Z., Karadas, C., & Izgu, N. (2019). Effects of progressive muscle relaxation and mindfulness meditation on fatigue, coping styles, and quality of life in early breast cancer patients: An assessor blinded, three-arm, randomized controlled trial. European Journal of Oncology Nurses, 42, 116–125. https://doi.org/10.1016/j.ejon.2019.09.003
Grossman, P., Niemannb, L., Schmidtc, S., & Walach, H. (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57, 35–43.
Hart, J. (2008). Guided imagery. Alternative & Complementary Therapies, 14, 295–299. https://doi.org/10.1089/act.2008.14604
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. https://doi.org/10.1037/a0018555
Howland, C. L., Jallo, N., Connelly, C. D., & Pickler, R. H. (2017). Feasibility of a relaxation guided imagery intervention to reduce maternal stress in the NICU. Journal of Obstetric, Gynecologic & Neonatal Nursing, 46, 532–543. https://doi.org/10.1016/j.jogn.2017.03.004
Hughes, J. W., Fresco, D. M., Myerscough, R., van Dulmen, M. H., Carlson, L. E., & Josephson, R. (2013). Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosomatic Medicine, 75, 721–728. https://doi.org/10.1097/PSY.0b013e3182a3e4e5
Jain, S., Shapiro, S. L., & Swanick, S. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33, 11–21.
Kabat-Zinn, J. (2005). Coming to our senses: Healing ourselves and the world through mindfulness. Hachette.
Kellermeyer, L., Harnke, B., & Knight, S. (2018). Covidence and Rayyan. Journal of the Medical Library Association, 106, 580. https://doi.org/10.5195/jmla.2018.513
Kolcaba, K. Y., & Fox, C. (1999). The effects of guided imagery on comfort of women with early-stage breast cancer undergoing radiation therapy. Oncology Nursing Forum, 26, 67–72.
Lean, R. E., Rogers, C. E., Paul, R. A., & Gerstein, E. D. (2018). NICU hospitalization: Long-term implications on parenting and child behaviors. Current Treatment Options in Pediatrics, 4, 49–69.
Lefkowitz, D. S., Baxt, C., & Evans, J. R. (2010). Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). Journal of Clinical Psychology in Medical Settings, 17, 230–237. https://doi.org/10.1007/s10880-010-9202-7
Liu, K., Chen, Y., Wu, D., Lin, R., Wang, Z., & Pan, L. (2020). Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complementary Therapies in Clinical Practice. https://doi.org/10.1016/j.ctcp.2020.101132
Liu, L., Oza, S., Hogan, D., Chu, Y., Perin, J., Zhu, J., et al. (2016). Global, regional, and national causes of under−5 mortality in 2000–15: An updated systematic analysis with implications for the sustainable development goals. Lancet, 388, 3027–3035.
Lotterman, J. H., Lorenz, J. M., & Bonanno, G. A. (2019). You can’t take your baby home yet: A longitudinal study of psychological symptoms in mothers of infants hospitalized in the NICU. Journal of Clinical Psychology in Medical Settings, 26, 116–122. https://doi.org/10.1007/s10880-018-9570-y
Luberto, C. M., Hall, D. L., Park, E. R., Haramati, A., & Cotton, S. (2020). A perspective on the similarities and differences between mindfulness and relaxation. Global Advances in Health and Medicine. https://doi.org/10.1177/2164956120905597
Ma, X., Yue, Z. Q., Gong, Z. Q., Zhang, H., Duan, N. Y., Shi, Y. T., Wei, G. X., & Li, Y. F. (2017). The effect of diaphragmatic breathing on attention, negative affect, and stress in healthy adults. Frontiers in Psychology, 8, 874. https://doi.org/10.3389/fpsyg.2017.00874
Marshall, A., Guillen, U., MacKley, A., & Sturtz, W. (2019). Mindfulness training among parents with preterm neonates in the Neonatal Intensive Care Unit: A pilot study. American Journal of Perinatology, 36, 1514–1520. https://doi.org/10.1055/s-0039-1678557
Meier, P. P., Engstrom, J. L., Patel, A. L., Jegier, B. J., & Bruns, N. E. (2010). Improving the use of human milk during and after the NICU stay. Clinics in Perinatology, 37, 217–245. https://doi.org/10.1016/j.clp.2010.01.013
Mendelson, T., Cluxton-Keller, F., Vullo, G. C., Tandon, D., & Noazin, S. (2017). NICU-based interventions to reduce maternal depressive and anxiety symptoms: A meta-analysis. Pediatrics, 139, e20161870. https://doi.org/10.1542/peds.2016-1870
Mendelson, T., McAfee, C., Damian, A. J., Brar, A., Donohue, P., & Sibinga, E. (2018). A mindfulness intervention to reduce maternal distress in neonatal intensive care: A mixed methods pilot study. Archives of Women’s Mental Health, 21, 791–799. https://doi.org/10.1007/s00737-018-0862-x
Mohd Shukri, N. H., Wells, J., & Fewtrell, M. (2018). The effectiveness of interventions using relaxation therapy to improve breastfeeding outcomes: A systematic review. Maternal & Child Nutrition, 14, e12563. https://doi.org/10.1111/mcn.12563
Nguyen, J., & Brymer, E. (2018). Nature-based guided imagery as an intervention for state anxiety. Frontiers in Psychology, 9, 1858. https://doi.org/10.3389/fpsyg.2018.01858
Niazi, A. K., & Niazi, S. K. (2011). Mindfulness-based stress reduction: A non-pharmacological approach for chronic illnesses. North American Journal of Medical Sciences, 3, 20–23. https://doi.org/10.4297/najms.2011.320
Noergaard, B., Ammentorp, J., Garne, E., Fenger-Gron, J., & Kofoed, P. E. (2018). Fathers’ stress in a Neonatal Intensive Care Unit. Advances in Neonatal Care, 18, 413–422. https://doi.org/10.1097/ANC.0000000000000503
Obeidat, H. M., Bond, E. A., & Callister, L. C. (2009). The parental experience of having an infant in the newborn intensive care unit. Journal of Perinatal Education, 18, 23–29. https://doi.org/10.1624/105812409X461199
Owais, S., Faltyn, M., Johnson, A. V. D., Gabel, C., Downey, B., Kates, N., & Van Lieshout, R. J. (2020). The perinatal mental health of indigenous women: A systematic review and meta-analysis. Canadian Journal of Psychiatry, 65, 149–163. https://doi.org/10.1177/0706743719877029
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Pan, W. L., Chang, C. W., Chen, S. W., & Gau, M. L. (2019). Assessing the effectiveness of mindfulness-based programmes on mental health during pregnancy and early motherhood: A randomized control trial. BMC Pregnancy and Childbirth, 19, 346. https://doi.org/10.1186/s12884-019-2503-4
Paul, G., Elam, B., & Verhulst, S. J. (2007). A longitudinal study of students’ perceptions of using deep breathing meditation to reduce testing stresses. Teaching and Learning in Medicine, 19, 287–292.
Perrier, M. F., Gurgel-Juarez, N., Flowers, H. L., McCormick, A., & Short, J. (2020). Mindfulness-based interventions for children and adolescents across all settings: A scoping review protocol. Systematic Reviews, 9, 286. https://doi.org/10.1186/s13643-020-01548-7
Phaloprakarn, C., Manusirivithaya, S., & Boonyarittipong, P. (2015). Risk score comprising maternal and obstetric factors to identify late preterm infants at risk for neonatal intensive care unit admission. Journal of Obstetric Gynaecology Research, 41, 680–688. https://doi.org/10.1111/jog.12610
Prouhet, P. M., Gregory, M. R., Russell, C. L., & Yaeger, L. H. (2018). Fathers’ stress in the Neonatal Intensive Care Unit: A systematic review. Advances in Neonatal Care, 18, 105–120. https://doi.org/10.1097/ANC.0000000000000472
Rajeswari, S., & Sanjeeva, R. N. (2019). Efficacy of progressive muscle relaxation on pregnancy outcome among anxious Indian primi mothers. Iranian Journal of Nursing Midwifery Research, 25, 23–30. https://doi.org/10.4103/ijnmr.IJNMR_207_18
Rausch, S. M., Gramling, S. E., & Auerbach, S. M. (2006). Effects of a single session of large-group meditation and progressive muscle relaxation training on stress reduction, reactivity, and recovery. International Journal of Stress Management, 13, 273–290. https://doi.org/10.1037/1072-5245.13.3.273
Rossman, M. (2000). Guided imagery for self-healing. An essential resource for anyone seeking wellness (2nd ed.). H.J. Kramer.
Sabnis, A., Fojo, S., Nayak, S. S., Lopez, E., Tarn, D. M., & Zeltzer, L. (2019). Reducing parental trauma and stress in neonatal intensive care: Systematic review and meta-analysis of hospital interventions. Journal of Perinatology, 39, 375–386. https://doi.org/10.1038/s41372-018-0310-9
Saha, S., Jarl, J., Gerdtham, U., Sundquist, K., & Sundquist, J. (2020). Economic evaluation of mindfulness group therapy for patients with depression, anxiety, stress and adjustment disorders compared with treatment as usual. The British Journal of Psychiatry, 216, 197–203. https://doi.org/10.1192/bjp.2018.247
Shaw, R. J., St John, N., Lilo, E., Jo, B., Benitz, W., Stevenson, D. K., & Horwitz, S. M. (2014). Prevention of traumatic stress in mothers of preterms: 6-month outcomes. Pediatrics, 134, e481–e488. https://doi.org/10.1542/peds.2014-0529
Shi, Z., & MacBeth, A. (2017). The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: A systematic review. Mindfulness, 8, 823–847. https://doi.org/10.1007/s12671-016-0673-y
Spijkerman, M. J., Pots, W., & Bohlmeijer, B. J. (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 45, 102–114. https://doi.org/10.1016/j.cpr.2016.03.009
Turner, M., Chur-Hansen, A., Winefield, H., & Stanners, M. (2015). The assessment of parental stress and support in the neonatal intensive care unit using the Parent Stress Scale–Neonatal Intensive Care Unit. Women Birth, 28, 252–258. https://doi.org/10.1016/j.wombi.2015.04.001
Yildiz, P. D., Ayers, S., & Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affect Disorders, 208, 634–645. https://doi.org/10.1016/j.jad.2016.10.009
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Not applicable.
Author information
Authors and Affiliations
Contributions
KHG, AS, and JA came up with the conception and structure of the review. Material preparation, data collection, and analysis were performed by KHG and MA. KHG wrote the manuscript, with the assistance of AS and JA. All authors reviewed, edited, and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors Kristin Harrison Ginsberg, Jane Alsweiler, Mohsen Alyami, and Anna Serlachius declare that they have no conflict of interest.
Ethical Approval
Not applicable.
Human and Animal Rights
No animal or human studies were carried out by the authors for this article.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
Full Search Strategy
Ovid MEDLINE(R) Epub Ahead of Print, In Process & Other Non-Indexed Citations, Ovid MEDLINE (R) Daily, and Ovid MEDLINE (R) 1946-Present.
-
1
Mindfulness/
-
2
mindful*.ti,ab,kw,kf.
-
3
(mbsr or mbct).ti,ab,kw,kf.
-
4
Relaxation Therapy/
-
5
(relax* adj2 (technique* or therap*)).ti,ab,kw,kf.
-
6
Meditation/
-
7
meditation.ti,ab,kw,kf.
-
8
“Acceptance and Commitment Therapy”/
-
9
(acceptance adj2 commitment therap*).ti,ab,kw,kf.
-
10
Imagery, Psychotherapy/
-
11
((guided or reverie or psychotherap*) adj2 (imag* or therap*)).ti,ab,kw,kf.
-
12
Autogenic Training/
-
13
progressive muscle relax*.ti,ab,kw,kf.
-
14
autogenic training.ti,ab,kw,kf.
-
15
or/1–14
-
16
Intensive Care Units, Neonatal/
-
17
((neonatal or newborn or neo-natal or preterm or neonate) adj1 (intensive care or ICU?)).ti,ab,kw,kf.
-
18
NICU.ti,ab,kw,kf.
-
19
Intensive Care, Neonatal/
-
20
or/16–19
-
21
15 and 20
APA PsycInfo < 1806 to March Week 4 2021 >
-
1
Mindfulness/
-
2
mindful*.ti,ab.
-
3
(mbsr or mbct).ti,ab.
-
4
Relaxation Therapy/
-
5
(relax* adj2 (technique* or therap*)).ti,ab.
-
6
Meditation/
-
7
meditation.ti,ab.
-
8
“Acceptance and Commitment Therapy”/
-
9
(acceptance adj2 commitment therap*).ti,ab.
-
10
Imagery, Psychotherapy/
-
11
((guided or reverie or psychotherap*) adj2 (imag* or therap*)).ti,ab.
-
12
Autogenic Training/
-
13
progressive muscle relax*.ti,ab.
-
14
autogenic training.ti,ab.
-
15
or/1–14
-
16
Intensive Care Units, Neonatal/
-
17
((neonatal or newborn or neo-natal or preterm or neonate) adj1 (intensive care or ICU?)).ti,ab.
-
18
NICU.ti,ab.
-
19
neonatal intensive care/
-
20
or/16–19
-
21
15 and 20
Embase < 1980 to 2021 March Week 4 2021 >
-
1
Mindfulness/
-
2
mindful*.ti,ab,kw.
-
3
(mbsr or mbct).ti,ab,kw.
-
4
Relaxation Therapy/
-
5
(relax* adj2 (technique* or therap*)).ti,ab,kw.
-
6
Meditation/
-
7
meditation.ti,ab,kw.
-
8
“Acceptance and Commitment Therapy”/
-
9
(acceptance adj2 commitment therap*).ti,ab,kw.
-
10
Imagery, Psychotherapy/
-
11
((guided or reverie or psychotherap*) adj2 (imag* or therap*)).ti,ab,kw.
-
12
Autogenic Training/
-
13
progressive muscle relax*.ti,ab,kw.
-
14
autogenic training.ti,ab,kw.
-
15
or/1–14
-
16
Intensive Care Units, Neonatal/
-
17
((neonatal or neonate or newborn or preterm or neo-natal) adj1 (intensive care or ICU?)).ti,ab,kw.
-
18
NICU.ti,ab,kw.
-
19
Intensive Care, Neonatal/
-
20
or/16–19
-
21
15 and 20
SCOPUS
(TITLE-ABS-KEY (mindfulness OR “mbsr” OR “mbct” OR “Relaxation Therapy” OR meditation OR “Acceptance and Commitment Therapy” OR “Autogenic Training” OR “progressive muscle relaxation”) AND TITLE-ABS-KEY (“neonatal intensive care unit” OR “NICU” OR “neonatal intensive care units” OR “newborn intensive care” OR neonate OR preterm)).
Cochrane Library
-
MeSH descriptor: [Intensive Care, Neonatal] explode all trees.
-
MeSH descriptor: [Mindfulness] explode all trees.
-
MeSH descriptor: [Mind–Body Therapies] explode all trees.
-
Mindfulness based stress reduction*
-
Mindfulness based*
-
mbsr* or mbct*
-
MeSH descriptor: [Meditation] explode all trees.
-
meditation*
-
MeSH descriptor: [Relaxation Therapy] explode all trees.
-
(relaxation* near/2 (technique* or therap*)).
-
MeSH descriptor: [Intensive Care Units, Neonatal] explode all trees.
CINAHL Plus
(Mindfulness or mindful* or (mbsr) or (mbct) or (Relaxation Therapy) or ((relax* adj2 (technique* or therap*)) or meditation or (“Acceptance and Commitment Therapy”) or (Imagery, Psychotherapy) or ((guided or reverie or psychotherap*) adj2 (imag* or therap*)) or (Autogenic Training) or (progressive muscle relax*)) AND ((neonatal intensive care unit) or (NICU) or (Intensive Care Units, Neonatal) or ((neonatal or newborn or neo-natal) adj1 (intensive care or ICU?)) or (Intensive Care, Neonatal)).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ginsberg, K.H., Alsweiler, J., Alyami, M. et al. Mindfulness and Relaxation-Based Interventions to Reduce Parental Stress, Anxiety and/or Depressive Symptoms in the Neonatal Intensive Care Unit: A Systematic Review. J Clin Psychol Med Settings 30, 387–402 (2023). https://doi.org/10.1007/s10880-022-09902-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-022-09902-8