Abstract
The experiences of diagnosis of congenital heart disease (CHD), cardiac surgery and hospitalisation(s) are distressing and represent a significant stressor for a child and family, which may impact psychosocial development. This systematic review provides a synthesis of psychosocial outcomes of infants and young children with congenital heart disease who had cardiac surgery early in life. Twenty-eight studies related to infant and young children’s psychosocial development, specifically emotional, social and behavioural functioning were identified. Variability was related to methodological factors including differences in study design, varying measurement tools and heterogeneous samples. Despite these limitations, the majority of studies were of high quality. The most common finding was a high prevalence of low-severity emotional and behavioural dysregulation. Young children with severe CHD or comorbid conditions experienced greater impairment, with higher rates of externalising behaviour problems, although internalising behaviour problems were also evident. This review integrates findings from literature in the past 28 years on the psychosocial well-being of infants and young children with CHD and demonstrates a risk for emotional, social and behavioural development difficulty, and, importantly, that symptoms of psychosocial impairment are detectable very early in infancy. We advocate for assessment and monitoring of emotional and behavioural regulation and social development to be routinely conducted from infancy to enable prevention and early intervention.

Similar content being viewed by others
References
References marked with an asterisk * indicate studies included in the review
Achenbach, T. M., & Rescorla, L. A. (2000). Child behavior checklist for ages 11/2–5. Burlington: University of Vermont.
*Alton, G. Y., Rempel, G. R., Robertson, C. M. T., Newburn-Cook, C. V., & Norris, C. M. (2010). Functional outcomes after neonatal open cardiac surgery: Comparison of survivors of the Norwood staged procedure and the arterial switch operation. Cardiology in the Young, 20, 668–675.
*Alton, G. Y., Taghados, S., Joffe, A. R., Robertson, C. M. T., Dinu, I., & the Western Canadian Pediatric Therapies Follow-up Group. (2015). Prediction of preschool functional abilities after early complex cardiac surgery. Cardiology in the Young, 25, 655–662.
Australian Institute of Health and Welfare. (2017). Heart, stroke and vascular diseases. Retrieved June 2018, from https://www.aihw.gov.au/reports-data/health-conditions-disability-deaths/heart-stroke-vascular-diseases/overview.
Bayer, J., Hiscock, H., Scalzo, K., Mathers, M., McDonald, M., Morris, A., … Wake, M. (2009). Systematic review of preventive interventions for children’s mental health: What would work in Australian contexts? Australian and New Zealand Journal of Psychiatry, 43, 695–710.
*Bellinger, D. C., Rappaport, L. A., Wypij, D., Wernovsky, G., & Newburger, J. W. (1997). Patterns of developmental dysfunction after surgery during infancy to correct transposition of the great arteries. Developmental and Behavioral Pediatrics, 18, 75–83.
Bellinger, D. C., Wypij, D., duPlessis, A. J., Rappaport, L. A., Jonas, R. A., Wernovsky, G., & Newburger, J. W. (2003). Neurodevelopmental status at 8 years in children with dextro-transposition of the great arteries: The Boston Circulatory Arrest Trial. Journal of Thoracic and Cardiovascular Surgery, 126, 1385–1396.
Brandlistuen, R. E., Stene-Larsen, K., Holmstrom, H., Landolt, M. A., Eskedal, L. T., & Vollrath, M. E. (2010). Symptoms of communication and social impairment in toddlers with congenital heart defects. Child: Care, Health and Development, 37, 37–43.
*Brandlistuen, R. E., Stene-Larsen, K., Holmstrøm, H., Landolt, M. A., Eskedal, L. T., & Vollrath, M. E. (2011). Occurrence and predictors of developmental impairments in 3-year-old children with congenital heart defects. Journal of Developmental and Behavioral Pediatrics, 32, 526–532.
*Brosig, C. L., Mussatto, K. A., Kuhn, E. M., & Tweddell, J. S. (2007). Neurodevelopmental outcome in preschool survivors of complex congenital heart disease: Implications for clinical practice. Journal of Pediatric Health Care, 21, 3–12.
Calkins, S. D., & Hill, A. L. (2007). Caregiver influences on emerging emotion regulation: Biological and environmental transactions in early development. In J. Gross (Ed.), Handbook of emotion regulation (pp. 229–248). New York: The Guilford Press.
Casey, F. A., Sykes, D. H., Craig, B. G., Power, R., & Mulholland, H. C. (1996). Behavioral adjustment of children with surgically palliated complex congenital heart disease. Journal of Pediatric Psychology, 21, 335–352.
Celermajer, D., Strange, G., Cordina, R., Selbie, L., Sholler, G., Winlaw, D., … d’Udekem, Y. (2016). Congenital Heart Disease requires a lifetime continuum of care: A call for a regional registry. Heart, Lung and Circulation, 25, 750–754.
*Claessens, N. H. P., Algra, S. O., Ouwehand, T. L., Jansen, N. J. G., Schappin, R., Haas, F., … Benders, M. J. N. L. (2018). Perioperative neonatal brain injury is associated with worse school-age neurodevelopment in children with critical congenital heart disease. Developmental Medicine and Child Neurology, 60, 1052–1058.
Corno, A. F., & Utens, E. M. W. J. (2018). Editorial: Neuro-development and psychological issues in congenital heart defects. Frontiers in Pediatrics, 5, 1–2.
DeMaso, D. R., Calderon, J., Taylor, G. A., Holland, J. E., Stopp, C., White, M. T., … Newburger, J. W. (2017). Psychiatric disorders in adolescents with single ventricle congenital heart disease. Pediatrics, 139, e20162241.
Dopfner, M., Berner, W., Fleischmann, T., & Schmidt, M. (1993). Verhaltensbeurteilungsbogen fur Vorschulkinder (VBV 3-6). Weinheim: Beltz.
De Young, A. C., Kenardy, J. A., & Cobham, V. E. (2011). Diagnosis of posttraumatic stress disorder in preschool children. Journal of Clinical Child and Adolescent Psychology, 40, 375–384.
*Eagleson, K. J., Justo, R. N., Ware, R. S., Johnson, S. G., & Boyle, F. M. (2013). Health-related quality of life and congenital heart disease in Australia. Journal of Paediatrics and Child Health, 49I, 856–864.
Ernst, M., Marino, B., Cassedy, A., Piazza-Waggoner, C., Franklin, R., Brown, K., & Wray, J. (2018). Biopsychosocial predictors of Quality of Life outcomes in pediatric congenital heart disease. Pediatric Cardiology, 39, 79–88.
Fekkes, M., Theunissen, N. C. M., Brugman, E., Veen, S., Verrips, E. G. H., Koopman, H. M., … Verloove-Vanhorick, S. P. (2000). Development and psychometric evaluation of the TAPQOL: A health-related quality of life instrument for 1- to 5-year-old children. Quality of Life Research, 9, 961–972.
Gardner, F. V., Freeman, N. H., Black, A. M. S., & Angelini, G. D. (1996). Disturbed mother–infant interaction in association with congenital heart disease. Heart, 76, 56–59.
*Gaynor, J. W., Nord, A. S., Wernovsky, G., Bernbaum, J., Solot, C. B., Burnham, N., … Gerdes, M. (2009). Apolipoprotein E genotype modifies the risk of behavior problems after infant cardiac surgery. Pediatrics, 124, 241–250.
Girard, J. M., & Cohen, J. F. (2016). A primer on observational measurement. Assessment, 23, 404–413.
Goldberg, S., Janus, M., Washington, J., Simmons, R. J., MacLusky, I., & Fowler, R. S. (1997). Prediction of preschool behavioral problems in healthy and pediatric samples. Developmental and Behavioral Pediatrics, 18, 304–313.
*Goldsworthy, M., Franich-Ray, C., Kinney, S., Shekerdemian, L., Beca, J., & Gunne, J. (2016). Development in 2-year-olds with congenital heart disease. Congenital Heart Disease, 11, 378–385.
Green, J. L., Knight, S., McCarthy, M. C., & DeLuca, C. D. (2013). Motor functioning during and following chemotherapy treatment for pediatric acute lymphoblastic leukemia. Pediatric Blood & Cancer, 60, 1261–1266.
Guedeney, A., & Fermanian, J. (2001). A validity and reliability study of assessment and screening for sustained withdrawal reaction in infancy: The Alarm Distress Baby Scale. Infant Mental Health Journal, 22, 559–575.
*Guerra, G. G., Robertson, C. M. T., Alton, G. Y., Joffe, A. R., Dinu, I. A., Nicholas, D., … Rebeyka, I. M. (2013). Quality of life 4 years after complex heart surgery in infancy. The Journal of Thoracic and Cardiovascular Surgery, 145, 482–488.
*Guerra, G. G., Joffe, A. R., Robertson, C. M. T., Atallah, J., Alton, G., Sauve, R. S., … Rebeya, I. M. (2014). Health-related quality of life experienced by children with chromosomal abnormalities and congenital heart defects. Pediatric Cardiology, 35, 536–541.
Harrison, P. L., & Oakland, T. (2003). Manual for the adaptive behavior assessment system II. PsychCorp. San Antonia: Harcourt Assessment Inc.
*Harrison, T. (2013). Autonomic nervous system function, child behavior, and maternal sensitivity in three-year-old children with surgically corrected transposition. Heart and Lung, 42, 414–421.
*Hulser, K., Dubowy, K., Knobl, H., Meyer, H., & Scholmerich, A. (2007). Developmental outcomes and psychosocial adjustment in children after surgery for congenital heart disease during infancy. Journal of Reproductive and Infant Psychology, 25, 139–151.
*Ikle, L., Hale, K., Fashaw, L., Boucek, M., & Rosenberg, A. A. (2003). Developmental outcome of patients with hypoplastic left heart syndrome treated with heart transplantation. The Journal of Pediatrics, 142, 20–25.
Ingerski, L. M., Shaw, K., Gray, W. N., & Janicke, D. M. (2010). A pilot study comparing traumatic stress symptoms by child and parent report across pediatric chronic illness groups. Developmental and Behavioral Pediatrics, 31, 713–719.
Jackson, C., Cheater, F. M., & Reid, I. (2008). A systematic review of decision support needs of parents making child health decisions. Health Expectations, 11, 232–251.
Jordan, B., Franich-Ray, C., Albert, N., Anderson, V., Northam, E., Cochrane, A., & Menahem, S. (2014). Early mother–infant relationships after cardiac surgery in infancy. Archives of Disease in Childhood, 99, 641–645.
Jordan, B., Franich-Ray, C., Anderson, V., Northam, E., Albert, N., Cochrane, A., & Menahem, S. (2013). Maternal report of infant emotional well-being following their infant’s hospitalization for neonatal cardiac surgery. Infant Mental Health Journal, 34, 259–266.
Karsdorp, P. A., Everaerd, W., Kindt, M., & Mulder, B. J. M. (2007). Psychological and cognitive functioning in children and adolescents with congenital heart disease: A Meta-Analysis. Journal of Pediatric Psychology, 32, 527–541.
Kern, J. H., Hinton, V. J., Nereo, N. E., Hayes, C. J., & Gersony, W. M. (1998). Early developmental outcome after the Norwood procedure for hypoplastic left heart syndrome. Pediatrics, 102, 1148–1152.
Kim, D. S., Yatong, K. L., Kim, J. H., Bergquist, C. S., Gerdes, M., Bernbaum, J. C., … Gaynor, J. W. (2018). Autosomal dominant mannose-binding lectin deficiency is associated with worse neurodevelopmental outcomes after cardiac surgery in infants. The Journal of Thoracic and Cardiovascular Surgery, 155, 1139–1147.
Landgraf, J. M., Abetz, L., & Ware, J. E. (1996). The CHQ user’s manual (1st ed.). Boston: The Health Institute, New England Medical Center.
Latal, B., Helfricht, S., Fischer, J. E., Bauersfeld, U., & Landolt, M. A. (2009). Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: A systematic review. BMC Pediatrics, 9, 6.
Long, A. F., & Godfrey, M. (2004). An evaluation tool to assess the quality of qualitative research studies. International Journal of Social Research Methodology, 7, 181–196.
Macha, T., & Petermann, F. (2008). The ET 6-6: A method for development assessment for German-speaking countries. Journal of Psychology, 216, 154–160.
*Majnemer, A., Limperopoulos, C., Shevell, M., Rohlicek, C., Rosenblatt, B., & Tchervenkov, C. (2006). Health and well-being of children with congenital cardiac malformations, and their families, following open-heart surgery. Cardiology in the Young, 16, 157–164.
*Majnemer, A., Limperopoulos, C., Shevell, M., Rohucek, C., Rosenblatt, B., & Tchervenkov, C. (2008). Developmental and functional outcomes at school entry in children with congenital heart defects. The Journal of Pediatrics, 153, 55–60.
Majnemer, A., Limperopoulos, C., Shevell, M. I., Rohlicek, C., Rosenblatt, B., & Tchervenkov, C. (2009). A new look at outcomes of infants with congenital heart disease. Pediatric Neurology, 40, 197–204.
Marino, B. S., Lipkin, P. H., Newburger, J. W., Peacock, G., Gerdes, M., Gaynor, J. W., … Mahle, W. T. (2012). Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: A scientific statement from the American Heart Association. Circulation, 126, 1143–1172.
*McCusker, C. G., Doherty, N. N., Molloy, B., Casey, F., Rooney, N., Mulholland, C., … Stewart, M. (2007). Determinants of neuropsychological and behavioural outcomes in early childhood survivors of congenital heart disease. Archives of Disease in Childhood, 92, 137–141.
Meiser-Stedman, R., Smith, P., Glucksman, W., Yule, W., & Dalgleish, T. (2008). The posttraumatic stress disorder diagnosis in preschool and elementary school-age children exposed to motor vehicle accidents. The American Journal of Psychiatry, 165, 1326–1337.
Miatton, M., De Wolf, D., Francois, K., Thiery, E., & Vingerhoets, G. (2007). Behavior and self-perception in children with a surgically corrected congenital heart disease. Developmental and Behavioral Pediatrics, 28, 294–301.
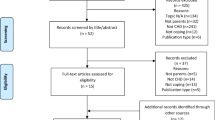
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting systems for systematic reviews and meta-analyses: The PRISMA statement. Open Medicine, 3, e123–e130.
Mussatto, K., Hollenbeck-Pringle, D., Trachtenberg, F., Sood, E., Sananes, R., Pike, N. A., … Pemberton, V. L. (2018). Utilisation of early intervention services in young children with hypoplastic left heart syndrome. Cardiology in the Young, 28, 126–133.
Mussatto, K. A., Hoffmann, R. G., Hoffman, G., Tweddell, J. S., Bear, L., Cao, Y., & Brosig, C. L. (2014). Risk and prevalence of developmental delay in young children with congenital heart disease. Pediatrics, 133, 570–577.
Papousek, M. (2011). Resilience, strengths, and regulatory capacities: Hidden resources in developmental disorders of infant mental health. Infant Mental Health Journal, 32, 29–46.
Pinquart, M., & Shen, Y. (2011). Behavior problems in children and adolescents with chronic physical illness: A meta-analysis. Journal of Pediatric Psychology, 36, 1003–1016.
*Re, J. M., Dean, S., Mullaert, J., Guedeney, A., & Menahem, S. (2018). Maternal distress and infant social withdrawal (ADBB) following infant cardiac surgery for congenital heart disease. World Journal for Pediatric and Congenital Heart Surgery, 9, 624–637.
Ringle, M. L., & Wernovsky, G. (2016). Functional, quality of life, and neurodevelopmental outcomes after congenital cardiac surgery. Seminars in Perinatology, 40, 556–570.
*Sadhwani, A., Asaro, L. A., Goldberg, C., Ware, J., Butcher, J., Gaies, M., … Agus, M. S. D. (2016). Impact of tight glycaemic control on neurodevelopmental outcomes at 1 year of age for children with congenital heart disease: A randomized controlled trial. The Journal of Pediatrics, 174, 193–198.
*Sarajuuri, A., Jokinen, E., Mildh, L., Tujulin, A., Mattila, I., Valanne, L., & Lonnqvist, T. (2012). Neurodevelopmental burden at age 5 years in patients with univentricular heart. Pediatrics, 130, e1636–e1646.
Schore, A. N. (2001). Effects of a secure attachment relationship on right brain development, affect regulation and infant mental health. Infant Mental Health Journal, 22, 7–66.
*Seltzer, L., Swartz, M. F., Kwon, J., Burchfiel, J., Cholette, J. M., Wang, H., … Alfieris, G. M. (2016). Neurodevelopmental outcomes after neonatal cardiac surgery: Roles of cortical isoelectric activity. The Journal of Thoracic and Cardiovascular Surgery, 151, 1137–1144.
Shonkoff, J., & Phillips, D. (Eds.). (2000). From neurons to neighbourhoods: The science of early childhood development. Washington, DC: National Academy Press.
Snookes, S. H., Gunn, J. K., Eldridge, B. J., Donath, S. M., Hunt, R. W., Galea, M. P., & Shekerdemian, L. (2010). A systematic review of motor and cognitive outcomes after early surgery for congenital heart disease. Pediatrics, 125, e818–e827.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). Vineland-II adaptive behavior scales: Survey forms manual. Circle Pines: AGS Publishing.
Stene-Larsen, K., Brandlistuen, R. E., Holmstrøm, H., Landolt, M. A., Eskedal, L. T., Engdahl, B., & Vollrath, M. E. (2011). Longitudinal findings from a Norwegian case-cohort study on internalizing problems in children with congenital heart defects. Acta Paediatrica, 100, 236–241.
*Sterken, C., Lemiere, J., Van der Berghe, G., & Mesotten, D. (2016). Neurocognitive development after pediatric heart surgery. Pediatrics, 137, e20154675.
*Tahirovic, E., Begic, H., Tahirovic, J., & Varni, J. W. (2011). Quality of life in children after cardiac surgery for congenital heart disease. Collegium Antropologicum, 35, 1285–1290.
Torowicz, D., Irving, S., Hanlon, A., Sumpter, D., & Medoff-Cooper, B. (2010). Infant temperament and parental stress in 3-month-old infants after surgery for complex congenital heart disease. Journal of Developmental and Behavioral Pediatrics, 31, 202–208.
van der Linde, D., Konings, E. E. M., Slager, M. A., Witsenburg, M., Helbing, W. A., Takkenberg, J. J. M., & Roos-Hesselink, J. W. (2011). Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. Journal of the American College of Cardiology, 58, 2241–2247.
Varni, J. W., & Limbers, C. A. (2009). The Pediatric Quality of Life Inventory: Measuring pediatric health-related quality of life from the perspective of children and their parents. Pediatric Clinics of North America, 56, 843–863.
*Vedovelli, L., Padalino, M., Suppiej, A., Sartori, S., Falasco, G., Simonato, M., … Cogo, P. (2018). Cardiopulmonary-bypass glial fibrillary acidic protein correlates with neurocognitive skills. The Annals of Thoracic Surgery, 106, 792–798.
*Visconti, K. J., Saudino, K. J., Rappaport, L. A., Newburger, J. W., & Bellinger, D. C. (2002). Influence of parental stress and social support on the behavioral adjustment of children with transposition of the great arteries. Developmental and Behavioral Pediatrics, 23, 314–321.
Viswanathan, M., Ansari, M. T., Berkman, N. D., Chang, S., Hartling, L., McPheeters, L. M., … Treadwell, J. R. (2012). Assessing the risk of bias of individual studies in systematic reviews of health care interventions. In: Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews. March 2012. AHRQ Publication No. 12-EHC047-EF. Retrieved July 11, 2019, from www.effectivehealthcare.ahrq.gov/.
*Werner, H., Latal, B., Buechel, E. V., Beck, I., & Landolt, M. (2014). Health-related quality of life after open-heart surgery. The Journal of Pediatrics, 164, 254–258.
Wernovsky, G. (2006). Current insights regarding neurological and developmental abnormalities in children and young adults with complex congenital cardiac disease. Cardiology in the Young, 16, 92–104.
Woolf, C., Muscara, F., Anderson, V. A., & McCarthy, M. C. (2015). Early traumatic stress responses in parents following a serious illness in their child: A systematic review. Journal of Clinical Psychology in Medical Settings, 22, 53–66.
Acknowledgements
The research project reported in this published work was conducted by the authors as part of their Doctorate in Pediatrics at the University of Melbourne, or employment with the Murdoch Children’s Research Institute, or The Royal Children’s Hospital, Melbourne, Australia. No funding support was received for this project. The authors have full control of all primary data and agree to allow the journal of publication to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tamera Clancy, Frank Muscara, Carolina de Weerth and Brigid Jordan all declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
No animal or human studies were carried out by the authors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clancy, T., Jordan, B., de Weerth, C. et al. Early Emotional, Behavioural and Social Development of Infants and Young Children with Congenital Heart Disease: A Systematic Review. J Clin Psychol Med Settings 27, 686–703 (2020). https://doi.org/10.1007/s10880-019-09651-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-019-09651-1