Abstract
Research suggests that best-practice psychotherapies only have moderate effects on reducing anxiety in youths. Such limitations in outcomes prompt consideration of alternative conceptualisations of anxiety and its treatment. Based upon the metacognitive model, we propose a novel therapy targeting metacognitive knowledge (beliefs about emotions and emotion regulation) for the treatment of anxiety in adolescents. The current case series study aimed to provide a proof of concept for the effectiveness of Meta-Emotion Therapy for adolescents (MET-A) for the treatment of adolescent anxiety. Four adolescents with elevated anxiety participated in this case series study. All participants received 10 individual sessions of MET-A. Participants and a parent completed the Revised Children’s Anxiety and Depression Scale at baseline, weekly and at one-month follow-up. The participants also completed the Beliefs About Emotions Questionnaire and the Difficulties with Emotion Regulation Scale at baseline, post-therapy and one-month follow-up. The results showed that all participants improved or recovered from symptoms of anxiety and depression from pre- to post-treatment, when taking into consideration both self- and parent-reported ratings (however, these ratings were often non-concordant). Gains were maintained at one-month follow-up. Further, participants who self-reported reductions in anxiety and depression also cited reductions in several maladaptive beliefs about emotions and improvements in aspects of emotion regulation. The participants endorsed the therapy as highly acceptable, appropriate, and feasible. Overall, the results of this study provide preliminary proof of concept for MET-A as a promising intervention for the treatment of adolescent anxiety Further investigation of MET-A is warranted to optimise treatment outcomes and measurement of change.
Clinical Trial Registration: Registered with the Australian and New Zealand Clinical Trial Registry number 382327.
Similar content being viewed by others
Introduction
Adolescence is a key risk phase for the development of anxiety with 52% with an anxiety disorder experiencing the onset before the age of 18 (Solmi et al., 2022). This is concerning as anxiety disorders are associated with substantial adolescent impairment in schooling, family, and peer relationships (de Lijster, et al., 2018). While most research has focused on the prevalence and consequences of anxiety disorders in youth, evidence suggests that high levels of anxiety at a subclinical level are also linked to similarly unfavourable outcomes (Balázs et al., 2013; Burstein et al., 2014). Thus, targeting the high levels of anxiety in adolescence, irrespective of whether they meet criteria for an anxiety disorder, is an important goal for treatment. However, a recent meta-analysis revealed that psychological therapies have only a moderate effect on reducing the severity of anxiety symptoms in 11 to 18 year olds with a primary diagnosis of an anxiety disorder, and only 36% of adolescents with an anxiety disorder no longer met the criteria following psychotherapy (Baker et al., 2021). Interestingly, the authors found these modest outcomes consistently across a range of potential moderators such as treatment type, treatment modality, anxiety disorder type, age, gender, parental involvement, treatment hours, ethnicity, and community versus clinical sample. Overall, the current state of research suggests that there are limitations in current best practice psychotherapies for adolescent anxiety, and therefore there is a need to consider therapies based upon other conceptualisations of anxiety.
One potentially helpful theoretical framework to guide the conceptualisation of anxiety psychopathology and psychotherapy is the metacognitive model. The original metacognitive model was developed by John Flavell (1979). Since then, the model has experienced further enhancements to guide the cognitive developmental field (Norman et al., 2019), as well as being used to guide the understanding of psychopathology and the design of psychotherapy (Moritz & Lysaker, 2018). While there is evidence that a metacognitive based therapy targeting metacognitive beliefs about cognitions can be effective in treating anxiety in adults (Solem et al., 2021) and children/adolescents (Thorslund, et al., 2020), there is increasing evidence that metacognitive beliefs about emotions (BEs) are also important in the development and maintenance of psychopathology (Schäfer et al., 2017; Strodl & Wylie, 2020). Indeed, recent evidence indicates that BEs are more strongly associated with some maladaptive coping strategies, such disordered eating, than metacognitive beliefs about thoughts (Strodl & Sorensen, 2023).
In addition to being linked with disordered eating, maladaptive beliefs about emotions have also been implicated in the experience of anxiety and depression (Koç & Uzun, 2022).
Certain BEs are considered maladaptive because they interfere with emotions serving their core function, which is to prepare one to take action to meet underlying needs (Greenberg, 2002). Examples of maladaptive beliefs about emotions include beliefs that emotions are overwhelming and uncontrollable, shameful and irrational, useless, invalid and meaningless, dangerous or contagious (Strodl et al., 2023). Ford and Gross (2018) propose a useful model explaining how beliefs about emotions might influence different stages of the emotion-regulation process. Synthesising these ideas, our metacognitive conceptualisation of anxiety, that guides the treatment plan utilised in this study, proposes that individuals appraise situations in terms of the degree to which their circumstances meet their underlying emotional needs. Emotions are seen to be signals of an underlying emotional need being met or not met. For example, an individual may experience joy or contentment if an emotional need is met. Conversely, they might experience anxiety if their need for safety is not met, or anger if their need for justice is not met. The intensity of the emotion therefore represents the degree to which the underlying emotional need is perceived to be met or not be met. If the individual believes that emotions are important signals to attend to, then the information signalled by the emotion is useful in directing the person to either a problem solving or acceptance stance. However, if the individual holds a maladaptive metacognitive belief that emotions are overwhelming or uncontrollable, or shameful or useless (for example), then they will be motivated to reduce the emotion using a coping strategy (e.g., avoidance or distraction). The metacognitive beliefs an individual holds about emotions and coping strategies therefore are critical to guiding a person’s response to experiencing emotions, such as anxiety, in an adaptive or maladaptive way. It is the combination of heightened emotion and maladaptive coping strategies affecting the individual’s functioning that characterise the presenting psychopathology.
Given the research supporting the relationships between maladaptive beliefs about emotions, coping strategies and mental health outcomes in adolescents, and recent evidence that beliefs about emotions are malleable in psychotherapy (Glisenti et al., 2022), there is a need to examine the effectiveness of a psychotherapy that targets maladaptive beliefs about emotions and coping strategies for the treatment of anxiety in adolescence. Thus, this study aimed to address a treatment gap by testing a proof of concept that a novel psychotherapy targeting maladaptive beliefs about emotions and coping strategies in adolescents, called Meta-Emotion Therapy for Adolescents (MET-A), will result in a reduction in self-reported and parent-reported anxiety and depression. Similarly, the study aimed to gather preliminary evidence as to whether MET is an effective intervention in reducing negative BEs and improving emotion regulation strategies. Finally, the study also aimed to gather initial observations as to the feasibility and participant acceptability of the intervention to guide future refinements of the intervention prior to larger pilot studies. It was hypothesised that MET-A will significantly improve scores on the primary measures of self-reported and parent-reported anxiety, as well as upon the secondary measures of self-reported and parent-reported depression, beliefs about emotions, and emotion regulation strategies. It was also hypothesised that the intervention will be reported as acceptable and feasible by the adolescent participants.
Methods
Design
This study utilised a case series design. This project was approved by Queensland University of Technology University Human Research Ethics Committee (QUT UHREC; 2022-4450-9571).
Participants
Four participants were recruited via advertisement in local school newsletters. Participants were four adolescent females aged either 15 or 16 years, with self-reported clinical levels of anxiety based upon a score of 65 or more on the Revised Children’s Anxiety and Depression Scale (Table 1). Exclusionary criteria included parent-reported high suicide risk, high-risk self-harming behaviour, recent bereavement or other recent critical event (e.g., separating families), intellectual disability, autism spectrum disorder, current psychosis, and current psychological treatment.
Measures
Adolescent Anxiety and Depression
The participants’ symptoms of anxiety and depression were measured using the Revised Children’s Anxiety and Depression Scale-25 (RCADS-25; Klaufus et al., 2020). The RCADS-25 consists of 25 items and two subscales: (a) Broad Anxiety [15 items; e.g. “I worry what other people think of me”] and (b) Depression [10 items; e.g. “I feel sad or empty”]. Responses are rated using a four-point Likert scale, ranging from 1 (never) to 4 (always), whereby higher scores indicate higher levels of anxiety and depression. The scale has demonstrated good to excellent internal consistency for both subscales in school-based (0.79–0.86) and clinical (0.80–0.91) samples of children and adolescents aged 8 to 18 years (Ebesutani et al., 2016), alongside good construct and criterion validity as well as test–retest reliability (0.70–0.73; Klaufus et al., 2020).
Parent-Reported Anxiety and Depression
Parent-reported levels of adolescent anxiety and depression were measured using the Revised Children’s Anxiety and Depression Scale-25-Parent (RCADS-25-P; Ebesutani et al., 2016). The RCADS-25-P consists of 25 items and two subscales, including (a) Broad Anxiety (15 items; e.g., “My child feels restless”); and (b) Depression (10 items; e.g. “My child is tired a lot”). Responses were measured on a four-point Likert scale, ranging from 1 (never) to 4 (always), whereby higher scores indicate higher levels of parent-reported adolescent anxiety and depression. The scale has good construct and criterion validity, good test–retest reliability (a = 0.80–0.90) and good to excellent internal consistency for total scores (a = 0.86–0.90) and subscales (a = 0.80–0.86) in both school-based and clinical samples of children and adolescents aged 8 to 18 years (Ebesutani et al., 2016).
Adolescent Emotion Regulation Strategies
Emotion regulation was assessed using the Difficulties in Emotion Regulation Scale – Short Form (DERS-SF; Kaufman et al., 2016). The DERS-SF consists of 18 items and six subscales:
-
(a)
Strategies (e.g., “When I’m upset, I believe that I will end up feeling very depressed”);
-
(b)
Non-acceptance (e.g., “When I’m upset, I feel guilty for feeling that way”);
-
(c)
Impulse (e.g., “When I’m upset, I become out of control”);
-
(d)
Goals (e.g., “When I’m upset, I have difficulty concentrating”);
-
(e)
Awareness (e.g., “When I’m upset, I acknowledge my emotions), and;
-
(f)
Clarity (e.g., “I have difficulty making sense out of my feelings”).
The DERS-SF is measured on a five-point Likert-type scale, ranging from 1 (almost never) to 5 (almost always), whereby higher scores correspond with increased emotion regulation difficulties. Scores are calculated by averaging items from each subscale. The scale demonstrates good construct and concurrent validity, acceptable to excellent internal consistency for total scores (0.91) and subscales (0.79–91) in adolescent samples (Kaufman et al., 2016).
Adolescent’s Beliefs About Emotions
The Beliefs about Emotions Questionnaire (BAEQ) measures an individual’s belief about the unacceptability of experiencing or expressing negative emotions (Manser et al., 2012). The BAEQ consists of 43 items, and six subscales. These include believing emotions are: (a) Overwhelming and Uncontrollable; (b) Shameful and Irrational; (c) Invalid and Meaningless; (d) Useless; (f) Damaging; and (g) Contagious. The BAEQ is measured on a five-point Likert scale, ranging from 1 (totally agree) to 5 (totally disagree), where high scores indicate more restrictive beliefs about experiencing or expressing negative emotions. The subscales have good convergent and divergent validity as well as acceptable to good internal consistency (a = 0.69-0.88; Manser et al., 2012).
Adolescent’s Feasibility Measures
Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM) and Feasibility of Intervention Measure (FIM)
The AIM, IAM and FIM are designed to measure three specific implementation outcomes: (a) Acceptability, the perception that the intervention is satisfactory or agreeable; (b) Appropriateness, the perceived fit or relevance of a given intervention for the consumer for the particular problem; and (c) Feasibility, the degree to which an intervention can be successfully implemented in a given setting (Weiner et al., 2017). The AIM, IAM and FIM are each four-item questionnaires, measured on a five-point Likert scale, from 1 (completely disagree) to 5 (completely agree), whereby higher scores indicate greater acceptability, appropriateness, or feasibility, respectively. Each scale has demonstrated good construct and discriminate validity, good to excellent internal consistency (AIM, a = 0.85; IAM, a = 0.91; FIM, a = 0.89; Weiner et al., 2017) and test–retest reliability (ranging from 0.78-0.88; Weiner et al., 2017).
Therapy Retention
Data regarding number of cancellations and dropouts was collected. Participants who completely stopped attending were considered dropouts.
Fidelity Measures
A detailed treatment manual was developed to ensure treatment fidelity, which outlined goals of each session, specific activities, important points of discussion, and consistent resources across participants. To assess fidelity and adherence to the treatment manual, the research team developed a short fidelity measure, according to individual session goals, which asked raters to rate, from 0 to 2, whether each goal was not achieved, partially achieved or fully achieved by the clinician. The video recordings of a random sample of 10% of all sessions were reviewed by the third author (GH). The fidelity of the program was deemed acceptable if results indicated that 90% of session content was completed.
Procedure
Screening
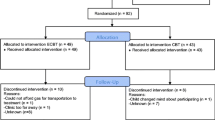
Participants were screened via two telephone calls. The first telephone call was with a parent. Youth meeting the inclusion criteria and not meeting the exclusionary criteria on discussion with the parent, were then contacted via a phone call. The adolescents who also reported meeting the inclusion criteria and not meeting the exclusion criteria, and who scored 65 or more on the RCADS-25 were included in the study. Eighteen participants expressed interest in the study, twelve parents and nine participants were telephone-screened and five met criteria for the study. The remainder were not included in the study for the following reasons: one was ineligible on the parent RCADS-25, two were ineligible on the child RCADS-25, three adolescents were not interested, and seven were lost to contact. Of the five eligible participants, one declined to participate due to scheduling issues, resulting in four participants taking part in the study. All participants and their parents provided written informed consent.
Participants completed the RCADS-25 each week during baseline (Weeks -3, -2, -1 to demonstrate stability at baseline) and treatment periods (Weeks 1 to 10) to assess self-reported anxiety and depression. The participants also completed the BAEQ to assess beliefs about emotions, and DERS-SF to assess emotion regulation at pre-treatment (Week -3) and post-treatment (Week 10), as well as at one-month follow-up (Week 14). Acceptability, appropriateness, and feasibility were also measured via the AIM, IAM and FIM at post-treatment (Week 10). The participants’ nominated parent completed the RCADS-25-P, to assess parent-reported anxiety and depression, at pre-treatment (Week-3) and post-treatment (Week 10), as well as at one-month follow-up (Week 14). The same parent completed the pre-treatment and post-treatment questionnaires. At post-treatment, the first author also contacted each parent via phone call to gather qualitative data about their views about MET (This involved asking the questions: “What did you like about the therapy?”, “What did you not like about the therapy?”, “What aspects of the therapy do you think we should change in the future?”.
Meta-Emotion Therapy Intervention
Treatment included ten weekly one-hour sessions of Meta-Emotion Therapy (MET-A). Ten weeks was chosen as a feasible dosage to fit in with the length of a school term. The treatment manual was adapted from a manual developed for a previous case series study that implemented Meta-Emotion Therapy for Binge Eating Disorder (Robertson & Strodl, 2020). MET-A is based on the metacognitive model (Efklides, 2008) and includes strategies incorporated in metacognitive therapy (Wells, 2009). It differs from Adrian Well’s version of metacognitive therapy by focusing on metacognitive knowledge of emotions rather than metacognitive knowledge of thoughts. The modules and key interventions included:
-
1.
Psychoeducation on anxiety, including antecedents and consequences.
-
2.
Creation of a shared formulation of anxiety based upon meta-emotion framework.
-
3.
Socialisation to the language of emotional needs and functions of emotions.
-
4.
Identification of specific negative beliefs about emotions and Socratic questioning to explore and challenge these beliefs.
-
5.
Introduction to mindfulness to facilitate experiential learning about emotions.
-
6.
Identification of maladaptive beliefs about the utility of coping strategies for anxiety.
-
7.
Introduction to behavioural experiments for challenging maladaptive beliefs about emotions and maladaptive beliefs about emotion-focused coping strategies.
-
8.
Continuation of behavioural experiments between sessions. Parents provided with handouts which included psychoeducation about the MET-A model and strategies to support their child.
-
9.
Discussion of the importance of understanding and tolerating emotions as useful signals for unmet emotional needs and problem solving how to meet these needs rather than using unhelpful coping strategies to suppress emotions.
-
10.
Review of MET-A content, progress and strategies learnt and identify a plan for relapse prevention.
Therapists
The therapists included two post-graduate clinical psychology students, one of which being the first author and co-author of the treatment manual (LC). Supervision was provided by the second author and co-author of the treatment manual (ES) who has 28 years’ experience as a clinical psychologist. Adherence to the MET manual was reviewed and corrected, where necessary, during weekly supervision for both therapists. Clinical observations by therapists were also recorded.
Data Analysis
Clinically significant change was calculated using Jacobson and Truax's (1991) Reliable Change Index, based upon Christensen and Mendoza's (1986) formula. The RCI for the RCADS-25 was calculated using mean pre-treatment baseline (Weeks -3, -2 and -1) scores, post-treatment score (Week 10), and follow-up score (Week 14). The RCI for the RCADS-P-25, BAEQ and DERS-SF was calculated using pre-treatment, post-treatment, and follow-up scores (Week -3, 12, and 16, respectively). Fisher and Durham (1999) proposed four treatment outcomes from this approach: (a) recovery, that is, reliable improvement from the clinical to normal population; (b) reliable improvement within the clinical population (in the current study, reliable improvement within the normal population will also be included in this category); (c) no change, and; (d) reliable deterioration. Clinical cut-off points were calculated for RCADS-25 and RCADS-P-25, using the M and SD information from the normal population, as follows:
where M1 = normal population M, and s1 = normal population SD. Cut-off scores were not used for the BAEQ and DERS-SF. Appendix A provides M, SD, and test–retest reliability of normal population references for each outcome. Cronbach’s alpha coefficients were used for the BAEQ and DERS-SF as test-rest reliability coefficients were not available (Raykov & Marcoulides, 2017).
Results
Therapy Retention
Four out of four cases completed the ten-session treatment, and there were no dropouts. Three cancellations occurred during the study and were rescheduled within the following week.
Fidelity
The third author (GH) who has 28 years’ experience as an Educational and Developmental Psychologist rated therapist adherence to the manual as 94.4%, suggesting that the fidelity of the program was acceptable.
Anxiety
Tables 2 and 3 outlines baseline, post-treatment and follow-up scores for the RCADS-25 and RCADS-P-25 broad anxiety subscales and show clinically significant change.
For self-reported anxiety, two of four participants experienced changes from pre- to post-treatment, and pre-treatment to follow-up. Case A and Case D experienced no changes in self-reported anxiety from pre- to post-treatment and pre-treatment to follow-up. In addition to experiencing reliable change, Case B and Case C moved from the clinical to the normal range and so were considered recovered from pre- to post-treatment, which was maintained at follow-up.
For parent-reported anxiety, one of four participants experienced reliable changes from pre- to post-treatment and two experienced reliable changes from pre-treatment to follow-up. Case A recovered from pre- to post-treatment, which was maintained at follow-up. Case B and C experienced changes in parent-reported anxiety from pre- to post-treatment and pre-treatment to follow-up did not meet the threshold for a reliable change. Case D narrowly missed statistical improvement from pre- to post-treatment but was recovered at follow-up.
Depression
Tables 2 and 3 outline baseline, post-treatment and follow-up scores for the RCADS-25 and RCADS-P-25 depression subscales and shows clinically significant change.
For self-reported depression, one of four participants experienced reliable changes from pre- to post-treatment, and pre-treatment to follow-up. Cases A, B and D experienced no reliable changes in self-reported depression from pre- to post-treatment. Case B, however, showed improvement from pre to follow-up, while Cases A and D did not. Case C recovered from pre- to post-treatment, which was maintained at follow-up.
For parent-reported depression, three of four participants experienced changes from pre- to post-treatment, and pre-treatment to follow-up. Cases A, B and D recovered from pre- to post-treatment, which was maintained at follow-up. Case C worsened on the parent rating from pre- to post-treatment; however, this was not maintained at follow-up.
Beliefs About Emotions
Table 2 outlines baseline, post-treatment, and follow-up scores for the BAEQ subscales and shows clinically significant change. Three of four participants experienced changes in beliefs about emotions from pre- to post-treatment. Case A experienced no change in any subscales from pre- to post-treatment and pre-treatment to follow-up. Case B improved in two subscales (Shameful and Irrational and Useless) from pre- to post-treatment, which was maintained at follow-up. Case C improved in four subscales (Overwhelming and uncontrollable, Shameful and Irrational, Useless, and Damaging) from pre- to post-treatment, and narrowly missed a statistically significant change in the Contagious subscale. These improvements were maintained for all at follow-up. Case D experienced no change in any beliefs about emotions subscales from pre- to post-treatment. However, from pre-treatment to follow-up, Case D improved in two subscales (Overwhelming and uncontrollable, Shameful and irrational) and narrowly missed a reliable change in the Contagious subscale.
Emotion Regulation
Table 2 outlines the Difficulties in Emotion Regulation Scale-Short Form (DERS-SF) total and subscale baseline, post-treatment, and follow-up scores and shows clinically reliable change. Two of the four participants experienced changes in DERS-SF subscales from pre- to post-treatment and pre-treatment to follow-up. Case A experienced no changes in DERS-SF subscales from pre- to post-treatment and pre-treatment to follow-up. Case B improved in one subscale (Clarity) from pre- to post-treatment, which was maintained at follow-up. Case C improved in two subscales (Awareness and Impulse) from pre- to post-treatment, and narrowly missed the cut-off for a reliable change in Strategies. These improvements were maintained for all but one subscale, Awareness, at follow-up. However, Case C did also experience a reliable change on Goals from pre- to follow-up. Case D came close to experiencing a reliable change in Strategies from pre- to follow-up.
Acceptability, Appropriateness, and Feasibility
Participants rated Meta-Emotion Therapy as highly appropriate (M = 4.94 out of 5), acceptable (M = 4.94 out of 5), and feasible (M = 4.56 out of 5). All participants agreed or strongly agreed to every item on the AIM, IAM and FIM. Overall, participants rated on average the acceptability, appropriateness, and feasibility of MET-A as 57.75 out of 60. Similarly, qualitative comments by participants and their parents indicated that, at least at face value, MET-A was viewed as credible, appropriate, and relevant to adolescent’s emotional experiences.
Discussion
The current case series study provides preliminary evidence that focusing on maladaptive beliefs about emotions and coping strategies, via an adapted version of Meta-Emotion Therapy (MET-A), may result in a reduction of either self-reported or parent-reported anxiety and depression in adolescents. The study also offered preliminary insights into the hypothesised mechanisms of change of maladaptive beliefs about emotions and emotion regulation strategies. Finally, the study provided initial evidence that MET-A may be feasible, acceptable, and agreeable to anxious adolescents.
The hypothesis that there would be a decrease in the primary outcome measure of anxiety and secondary outcome measure of depression from baseline to post-treatment and maintained at follow-up, was partially supported when taking into consideration both self- and parent-reported ratings. The combined results showed that the participants improved or recovered in symptoms of anxiety and depression. Although one parent did report a worsening of depressive symptoms. Further, for participants who experienced reliable improvement or recovery at post-treatment, these gains were consistently maintained at one-month follow-up. Interestingly, however, there was a lack of concordance between child- and parent-reported measures of anxiety and depression; that is, when the participant’s scores reflected improvement or recovery on anxiety or depression, the parent scores reflected no change, and vice versa.
While making sense of this non-concordance is outside of the scope of the study, it reflects a common trend of low parent–child agreement in outcome measures of in the existing literature (Makol et al., 2020). Indeed, meta-analytic evidence indicates a low-to-moderate correspondence between multiple informant ratings of child and adolescent internalising problems (r = 0.25; De Los Reyes et al., 2015). It has been suggested that modest parent–child agreement may be parents generally being more accurate in assessing behavioural signs of internalising symptoms (e.g., crying) as compared to subjective internal states (e.g., worrying; Karver, 2006). While it is unclear in the literature whether self- or parent-report is the more valid measure of adolescent anxiety or depression, it can be inferred that the discrepancy between parent and child reports of anxiety and depression may be due to reports from different informants tapping into slightly different aspects or saliency of the adolescent’s symptoms. Another explanation may be due to floor effects in parent-reported anxiety and depression. Generally, parents who endorsed high levels of anxious and depressive symptoms at pre-treatment, which was consistent with self-reports by the adolescent, cited improvements in symptoms at post-treatment. However, parents who endorsed low levels of anxious and depressive symptoms at pre-treatment generally cited no change, or an increase, in symptoms at post-treatment. It is plausible that low parent-reported scores at pre-treatment restricted the ability for treatment to show marked symptom improvements; thus, resulting in non-concordance with child-reported symptomatology.
The hypothesis that MET-A would result in significant decreases in beliefs about emotions and maladaptive emotion regulation strategies was partially supported. The results suggested that the adolescents who self-reported reductions in anxiety and depression also cited decreases in several maladaptive beliefs about emotions and improvements in some aspects of emotion regulation. This is in line with previous findings that beliefs about emotions can be successfully changed through psychotherapy (Glisenti et al., 2022) and that reducing beliefs about emotions results in reduced distress and internalising symptoms (Morvaridi et al., 2019). While conclusions cannot be made about causation at present, the results indicate that beliefs about emotions and emotion regulation may be key correlates of outcome and potentially important targets of intervention in the treatment of adolescent anxiety. As such, the preliminary evidence from this study warrants the inclusion of these measures in future intervention studies.
Lastly, the results show that MET-A was viewed by adolescent participants as a highly feasible, appropriate, and acceptable intervention for anxiety. Participants appeared to be highly motivated to participate in the intervention, given the lack of dropouts, low number of cancellations, and 100% completion rate. While these results may be a feature of the four participants in the current study, the results are promising, especially given that adolescents adherence is a predictor of psychotherapy outcome for anxiety (Lee et al., 2019).
Limitations and Recommendations
Although the results from the current study are promising, several limitations require consideration. First, as the program ended during the school assessment period it is possible that post-therapy anxiety and depression symptoms may have been elevated by the impact of external stressors on symptomatology. Second, as the BAEQ was originally developed for adults, its psychometric properties and sensitivity to change for an adolescent population are unknown. Third, the small sample size limits the generalisability of the findings of this study, especially as it is unknown how representative the four participants are of the broader anxious adolescent population. Associated with this, the female-only sample restricts the ability to generalise findings to males, which is particularly notable as some research has suggested differential beliefs about emotions in males as compared to females (Schleider & Weisz, 2016). Similarly, the limited age range of participants raises the question whether the outcomes can be generalised to younger or older adolescents, especially as metacognitive abilities have been found to develop with age throughout the adolescent period (Weil et al., 2013).
As for recommendations, direct participant and parent feedback, as well as global observations by clinicians, revealed several important considerations for the future development of MET-A. Firstly, all participants requested more than ten sessions to continue to solidify learnings. Thus, a key area for future development of MET-A is exploring the optimum dosage to create sustained change in pathology. At ten sessions, MET-A is on the lower end of most empirically-supported cognitive-behavioural manualised therapies, which indicate that up to 16 weekly therapy sessions may be required to achieve clinically significant and reliable change (Kagan et al., 2021). As such, future studies are needed to investigate the effectiveness of MET-A with extra sessions.
A second observation included frequent requests by parents for more information and resources to support their adolescent at home, as well as comments by adolescent participants that implementing certain learnings was difficult due to conflicting family or social beliefs about emotions. This suggests that systemic factors may need to be incorporated into future revisions of MET-A. This is supported by similar research which has found that parental expression of emotions and their reaction to their children’s emotions influence children’s emotion socialisation and emotion regulation (Hajal & Paley, 2020). As such, future research and development should explore the integration of family members into the MET-A treatment protocol. Finally, Makol et al. (2020) present evidence supporting a methodology utilising reports from a parent, adolescent and unfamiliar peer confederate to calculate a trait anxiety score that may be useful in managing poor concordance of multi-informant ratings of outcome in future intervention studies.
Conclusion
In summary, results of the current case series study indicate that focusing on altering maladaptive beliefs about emotions and coping strategies in psychotherapy may produce changes in self- or parent-reported anxiety and depression. The study also provided initial evidence of treatment feasibility, acceptability and appropriateness. Overall, the current study supported a preliminary proof of concept of MET-A for the treatment of anxiety in adolescence with indicators for future refinement. The study provides evidence to warrant larger trials targeting beliefs about emotions and beliefs about emotional coping strategies in adolescents experiencing clinical and subclinical levels of anxiety.
Data Availability
The data that support the findings of this study are available on request from the corresponding author, LC. The data are not publicly available due to protecting the privacy of the participants as a result of the small sample size.
Change history
18 February 2024
Missing Open Access funding information has been added in the Funding Note.
References
Baker, H. J., Lawrence, P. J., Karalus, J., Creswell, C., & Waite, P. (2021). The effectiveness of psychological therapies for anxiety disorders in adolescents: A meta-analysis. Clinical Child and Family Psychology Review, 24(4), 765–782. https://doi.org/10.1007/s10567-021-00364-2
Balázs, J., Miklósi, M., Keresztény, Á., Hoven, C. W., Carli, V., Wasserman, C., Apter, A., Bobes, J., Brunner, R., Cosman, D., Cotter, P., Haring, C., Iosue, M., Kaess, M., Kahn, J.-P., Keeley, H., Marusic, D., Postuvan, V., Resch, F., … Wasserman, D. (2013). Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. Journal of Child Psychology and Psychiatry, 54(6), 670–677. https://doi.org/10.1111/jcpp.12016
Burstein, M., Beesdo-Baum, K., He, J.-P., & Merikangas, K. R. (2014). Threshold and subthreshold generalized anxiety disorder among US adolescents: prevalence, sociodemographic, and clinical characteristics. Psychological Medicine, 44(11), 2351–2362. https://doi.org/10.1017/S0033291713002997
Christensen, L. B., & Mendoza, J. (1986). A method of assessing change in a single subject: An alteration of the RC index. Behavior Therapy, 17, 305–308. https://doi.org/10.1097/01.chi.0000125092.35109.c5
de Lijster, J. M., Dieleman, G. C., Utens, E. M. W. J., Dierckx, B., Wierenga, M., Verhulst, F. C., & Legerstee, J. S. (2018). Social and academic functioning in adolescents with anxiety disorders: A systematic review. Journal of Affective Disorders, 230(June 2017), 108–117. https://doi.org/10.1016/j.jad.2018.01.008
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858. https://doi.org/10.1037/a0038498
Ebesutani, C., Korathu-Larson, P., Nakamura, B. J., Higa-McMillan, C., & Chorpita, B. (2016). The revised child anxiety and depression scale 25–parent version: Scale development and validation in a school-based and clinical sample. Assessment, 24(6), 712–728. https://doi.org/10.1177/1073191115627012
Efklides, A. (2008). Metacognition: Defining its facets and levels of functioning in relation to self-regulation and co-regulation. European Psychologist, 13(4), 277–287. https://doi.org/10.1027/1016-9040.13.4.277
Fisher, P. L., & Durham, R. C. (1999). Recovery rates in generalized anxiety disorder following psychological therapy: An analysis of clinically significant change in the STAI-T across outcome studies since 1990. Psychological Medicine, 29(6), 1425–1434. https://doi.org/10.1017/S0033291799001336
Flavell, J. H. (1979). Metacognition and cognitive monitoring: A new area of cognitive developmental inquiry. American Psychologist, 34(10), 906-911. https://doi.org/10.1037/0003-066x.34.10.906
Ford, B. Q., & Gross, J. J. (2018). Why beliefs about emotion matter: An emotion-regulation perspective. Current Directions in Psychological Science, 28(1), 74–81. https://doi.org/10.1177/0963721418806697
Glisenti, K., Strodl, E., & King, R. (2022). The role of beliefs about emotions in emotion-focused therapy for binge-eating disorder. Journal of Contemporary Psychotherapy. https://doi.org/10.1007/s10879-022-09555-6
Greenberg, L. S. (2002). Emotion-focused therapy: Coaching clients to work through their feelings. In Emotion-focused therapy: Coaching clients to work through their feelings (pp. xvi, 337–xvi, 337). American Psychological Association. https://doi.org/10.1037/10447-000
Hajal, N. J., & Paley, B. (2020). Parental emotion and emotion regulation: A critical target of study for research and intervention to promote child emotion socialization. Developmental Psychology, 56(3), 403. https://doi.org/10.1037/dev0000864
Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. In Journal of Consulting and Clinical Psychology (Vol. 59, pp. 12–19). American Psychological Association. https://doi.org/10.1037/0022-006X.59.1.12
Kagan, E. R., Frank, H. E., Knepley, M. J., & Kendall, P. C. (2021). Beyond 16 sessions: Extending manualized treatment of anxious youth. Journal of Child and Family Studies, 30(2), 493–501. https://doi.org/10.1007/s10826-020-01872-5
Karver, M. (2006). Determinants of multiple informant agreement on child and adolescent behavior. Journal of Abnormal Child Psychology, 34, 251–262. https://doi.org/10.1007/s10802-005-9015-6
Kaufman, E. A., Xia, M., Fosco, G., Yaptangco, M., Skidmore, C. R., & Crowell, S. E. (2016). The Difficulties in emotion regulation scale short form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment, 38(3), 443–455. https://doi.org/10.1007/s10862-015-9529-3
Klaufus, L., Verlinden, E., van der Wal, M., Kösters, M., Cuijpers, P., & Chinapaw, M. (2020). Psychometric evaluation of two short versions of the Revised Child Anxiety and Depression Scale. BMC Psychiatry, 20(1), 47. https://doi.org/10.1186/s12888-020-2444-5
Koç, M. S., & Uzun, B. (2022). Psychometric properties of the Turkish version of the Beliefs About Emotions Questionnaire (BAEQ) and a preliminary investigation in relation to emotion regulation. Cognition, Brain, Behavior, 26(1), 67–88. https://doi.org/10.24193/cbb.2022.26.04
Lee, P., Zehgeer, A., Ginsburg, G. S., McCracken, J., Keeton, C., Kendall, P. C., et al. (2019). Child and adolescent adherence with cognitive behavioral therapy for anxiety: Predictors and associations with outcomes. Journal of Clinical Child & Adolescent Psychology, 48(sup1), S215–S226. https://doi.org/10.1080/15374416.2017.1310046
Makol, B. A., Youngstrom, E. A., Racz, S. J., Qasmieh, N., Glenn, L. E., & De Los Reyes, A. (2020). Integrating multiple informants’ reports: How conceptual and measurement models may address long-standing problems in clinical decision-making. Clinical Psychological Science, 8(6), 953–970. https://doi.org/10.1177/2167702620924439
Manser, R., Cooper, M., & Trefusis, J. (2012). Beliefs about emotions as a metacognitive construct: Initial development of a self-report questionnaire measure and preliminary investigation in relation to emotion regulation. Clinical Psychology and Psychotherapy, 19(3), 235–246. https://doi.org/10.1002/cpp.745
Moritz, S., & Lysaker, P. H. (2018). Metacognition–what did James H. Flavell really say and the implications for the conceptualization and design of metacognitive interventions. Schizophrenia Research, 201, 20–26. https://doi.org/10.1016/j.schres.2018.06.001
Morvaridi, M., Mashhadi, A., Shamloo, Z. S., & Leahy, R. L. (2019). The effectiveness of group emotional schema therapy on emotional regulation and social anxiety symptoms. International Journal of Cognitive Therapy, 12(1), 16–24. https://doi.org/10.1007/s41811-018-0037-6
Norman, E., Pfuhl, G., Sæle, R. G., Svartdal, F., Låg, T., & Dahl, T. I. (2019). Metacognition in psychology. Review of General Psychology, 23(4), 403–424. https://doi.org/10.1177/1089268019883821
Raykov, T., & Marcoulides, G. A. (2017). Thanks coefficient alpha, we still need you! Educational and Psychological Measurement, 79(1), 200–210. https://doi.org/10.1177/0013164417725127
Robertson, S., & Strodl, E. (2020). Treatment manual for meta-emotion therapy for binge eating disorder [Unpublished Manuscript]. School of Psychology and Counselling, Queensland University of Technology.
Schäfer, J. Ö., Naumann, E., Holmes, E. A., Tuschen-Caffier, B., & Samson, A. C. (2017). Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. Journal of Youth and Adolescence, 46(2), 261–276. https://doi.org/10.1007/s10964-016-0585-0
Schleider, J. L., & Weisz, J. R. (2016). Implicit theories relate to youth psychopathology, but how? A longitudinal test of two predictive models. Child Psychiatry & Human Development, 47(4), 603–617. https://doi.org/10.1007/s10578-015-0595-2
Solem, S., Wells, A., Kennair, L. E. O., Hagen, R., Nordahl, H., & Hjemdal, O. (2021). Metacognitive therapy versus cognitive–behavioral therapy in adults with generalized anxiety disorder: A 9-year follow-up study. Brain and Behavior, 11(10), 3–9. https://doi.org/10.1002/brb3.2358
Solmi, M., Radua, J., Olivola, M., Croce, E., Soardo, L., Salazar de Pablo, G., et al. (2022). Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Molecular Psychiatry, 27(1), 281–295. https://doi.org/10.1038/s41380-021-01161-7
Strodl, E., Hubert, M., & Cooper, M. (2023). Psychometric properties and factor structure of the Revised Beliefs About Emotions Questionnaire. Clinical Psychology & Psychotherapy. https://doi.org/10.1002/cpp.2889
Strodl, E., & Sorensen, P. (2023). The role of metacognitive beliefs versus meta-emotion beliefs in disordered eating. Australian Psychologist. https://doi.org/10.1080/00050067.2023.2181685
Strodl, E., & Wylie, L. (2020). Childhood trauma and disordered eating: Exploring the role of alexithymia and beliefs about emotions. Appetite, 154, 104802. https://doi.org/10.1016/j.appet.2020.104802
Thorslund, J., McEvoy, P. M., & Anderson, R. A. (2020). Group metacognitive therapy for adolescents with anxiety and depressive disorders: A pilot study. Journal of Clinical Psychology, 76(4), 625–645. https://doi.org/10.1002/jclp.22914
Weil, L. G., Fleming, S. M., Dumontheil, I., Kilford, E. J., Weil, R. S., Rees, G., Dolan, R. J., & Blakemore, S.-J. (2013). The development of metacognitive ability in adolescence. Consciousness and Cognition, 22(1), 264–271. https://doi.org/10.1016/j.concog.2013.01.004
Weiner, B. J., Lewis, C. C., Stanick, C., Powell, B. J., Dorsey, C. N., Clary, A. S., Boynton, M. H., & Halko, H. (2017). Psychometric assessment of three newly developed implementation outcome measures. Implementation Science, 12(1), 1–12. https://doi.org/10.1186/s13012-017-0635-3
Wells, A. (2009). Metacognitive therapy for anxiety and depression. In Metacognitive therapy for anxiety and depression. (pp. xvii, 316–xvii, 316). Guilford Press.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics Approval Statement
This study was approved by QUT Human Research Ethics Committee (HREA 2022–4450-9571).
Consent to Participate
Written informed consent was obtained from the participants and their parents.
Consent to Publish
The participants and parents have provided consent to publish non-identifiable data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cain, L., Strodl, E. & Howard, G. Targeting Beliefs About Emotions via Meta-Emotion Therapy for Adolescents with Anxiety: A Case Series Study. J Contemp Psychother (2024). https://doi.org/10.1007/s10879-023-09605-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s10879-023-09605-7