Abstract
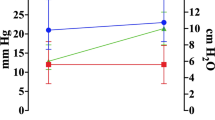
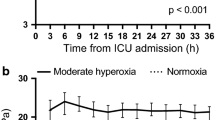
Patients with acute brain injury (ABI) often require the application of positive end-expiratory pressure (PEEP) to optimize mechanical ventilation and systemic oxygenation. However, the effect of PEEP on cerebral function and metabolism is unclear. The primary aim of this study was to evaluate the effects of PEEP augmentation test (from 5 to 15 cmH2O) on brain oxygenation, systemic oxygen cascade and metabolism in ABI patients. Secondary aims include to determine whether changes in regional cerebral oxygenation are reflected by changes in oxygenation cascade and metabolism, and to assess the correlation between brain oxygenation and mechanical ventilation settings. Single center, pilot cross-sectional observational study in an Academic Hospital. Inclusion criteria were: adult (> 18 y/o) patients with ABI and stable intracranial pressure, available gas exchange and indirect calorimetry (IC) monitoring. Cerebral oxygenation was monitored with near-infrared spectroscopy (NIRS) and different derived parameters were collected: variation (Δ) in oxy (O2)-hemoglobin (Hb) (ΔO2Hbi), deoxy-Hb(ΔHHbi), total-Hb(ΔcHbi), and total regional oxygenation (ΔrSO2). Oxygen cascade and metabolism were monitored with arterial/venous blood gas analysis [arterial partial pressure of oxygen (PaO2), arterial saturation of oxygen (SaO2), oxygen delivery (DO2), and lactate], and IC [energy expenditure (REE), respiratory quotient (RQ), oxygen consumption (VO2), and carbon dioxide production (VCO2)]. Data were measured at PEEP 5 cmH2O and 15 cmH2O and expressed as delta (Δ) values. Ten patients with ABI [median age 70 (IQR 62–75) years, 6 (60%) were male, median Glasgow Coma Scale at ICU admission 5.5 (IQR 3–8)] were included. PEEP augmentation from 5 to 15 cmH2O did not affect cerebral oxygenation, systemic oxygen cascade parameters, and metabolism. The arterial component of cerebral oxygenation was significantly correlated with DO2 (ΔO2HBi, rho = 0.717, p = 0.037). ΔrSO2 (rho = 0.727, p = 0.032), ΔcHbi (rho = 0.797, p = 0.013), and ΔHHBi (rho = 0.816, p = 0.009) were significantly correlated with SaO2, but not ΔO2Hbi. ΔrSO2 was significantly correlated with VCO2 (rho = 0.681, p = 0.049). No correlation between brain oxygenation and ventilatory parameters was found. PEEP augmentation test did not affect cerebral and systemic oxygenation or metabolism. Changes in cerebral oxygenation significantly correlated with DO2, SaO2, and VCO2. Cerebral oxygen monitoring could be considered for individualization of mechanical ventilation setting in ABI patients without high or instable intracranial pressure.


Similar content being viewed by others
References
Borsellino B, Schultz MJ, Gama de Abreu M, Robba C, Bilotta F. Mechanical ventilation in neurocritical care patients: a systematic literature review. Expert Rev Respir Med. 2016;10:1123–32.
Frisvold SK, Robba C, Guérin C. What respiratory targets should be recommended in patients with brain injury and respiratory failure? Intensive Care Med. 2019. https://doi.org/10.1007/s00134-019-05556-7.
Sutherasan Y, Vargas M, Pelosi P. Protective mechanical ventilation in the non-injured lung: review and meta-analysis. Crit Care. 2014;18:211. https://doi.org/10.1186/cc13778.
Serpa Neto A, Hemmes SNT, Barbas CSV, Beiderlinden M, Biehl M, Binnekade JM, Canet J, Fernandez-Bustamante A, Futier E, Gajic O, Hedenstierna G, Hollmann MW, Jaber S, Kozian A, Licker M, Lin WQ, Maslow AD, Memtsoudis SG, Reis Miranda D, Moine P, Ng T, Paparella D, Putensen C, Ranieri M, Scavonetto F, Schilling T, Schmid W, Selmo G, Severgnini P, Sprung J, Sundar S, Talmor D, Treschan T, Unzueta C, Weingarten TN, Wolthuis EK, Wrigge H, Gama De Abreu M, Pelosi P, Schultz MJ. Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology. 2015;123:66–78. https://doi.org/10.1097/ALN.0000000000000706.
Simonis FD, Serpa Neto A, Binnekade JM, Braber A, Bruin KCM, Determann RM, Goekoop G-J, Heidt J, Horn J, Innemee G, de Jonge E, Juffermans NP, Spronk PE, Steuten LM, Tuinman PR, de Wilde RBP, Vriends M, Gama de Abreu M, Pelosi P, Schultz MJ. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS. JAMA. 2018;320:1872. https://doi.org/10.1001/jama.2018.14280.
Pelosi P, Rocco PRM, Gama de Abreu M. Close down the lungs and keep them resting to minimize ventilator-induced lung injury. Crit Care. 2018;22:72. https://doi.org/10.1186/s13054-018-1991-3.
Nemer S, Santos R, Caldeira J, Reis P, Guimarães B, Loureiro T, Ramos R, Farias E, Prado D, Turon R. Positive end-expiratory pressure can increase brain tissue oxygen pressure in hypoxemic severe traumatic brain injury patients. Crit Care. 2011. https://doi.org/10.1186/cc10189.
Robba C, Ball L, Nogas S, Battaglini D, Messina A, Brunetti I, Minetti G, Castellan L, Rocco RMP, Pelosi P. Effects of positive end-expiratory pressure on lung recruitment respiratory mechanics and intracranial pressure in mechanically ventilated brain injured patients. Front Physiol. 2021;12:711273.
Picetti E, Pelosi P, Taccone FS, Citerio G, Mancebo J, Robba C. VENTILatOry strategies in patients with severe traumatic brain injury: the VENTILO Survey of the European Society of Intensive Care Medicine (ESICM). Crit Care. 2020;24:158. https://doi.org/10.1186/s13054-020-02875-w.
Castañón-González JA, Satué-Rodríguez J, Camacho-Juárez JS, Carrillo-Rosales F, León-Gutiérrez MA, Miranda-Ruiz R. Effects of different positive end expiratory pressure levels on resting energy expenditure measured by indirect calorimeter in patients with pressure-controlled ventilation. Gac Med Mex. 2004;140:583–8.
Robba C, Ball L, Battaglini D, Cardim D, Moncalvo E, Brunetti I, Bassetti M, Giacobbe DR, Vena A, Patroniti N, Rocco PRM, Matta BF, Pelosi P. Early effects of ventilatory rescue therapies on systemic and cerebral oxygenation in mechanically ventilated COVID-19 patients with acute respiratory distress syndrome: a prospective observational study. Crit Care. 2021;25:111. https://doi.org/10.1186/s13054-021-03537-1.
Mascia L, Grasso S, Fiore T, Bruno F, Berardino M, Ducati A. Cerebro-pulmonary interactions during the application of low levels of positive end-expiratory pressure. Intensive Care Med. 2005;31:373–9. https://doi.org/10.1007/s00134-004-2491-2.
Delsoglio M, Achamrah N, Berger MM, Pichard C. Indirect calorimetry in clinical practice. J Clin Med. 2019;8:1387. https://doi.org/10.3390/jcm8091387.
Mauri T, Eronia N, Turrini C, Battistini M, Grasselli G, Rona R, Volta CA, Bellani G, Pesenti A. Bedside assessment of the effects of positive end-expiratory pressure on lung inflation and recruitment by the helium dilution technique and electrical impedance tomography. Intensive Care Med. 2016;42:1576–87. https://doi.org/10.1007/s00134-016-4467-4.
Sugimoto H, Ohsashi N, Sawada Y, Yoshioka T, Sugimoto T. Effects of positive end-expiratory pressure on tissue gas tensions and oxygen transport. Crit Care Med. 1984;12:661–3. https://doi.org/10.1097/00003246-198408000-00012.
Cressoni M, Chiumello D, Algieri I, Brioni M, Chiurazzi C, Colombo A, Colombo A, Crimella F, Guanziroli M, Tomic I, Tonetti T, Luca Vergani G, Carlesso E, Gasparovic V, Gattinoni L. Opening pressures and atelectrauma in acute respiratory distress syndrome. Intensive Care Med. 2017;43:603–11. https://doi.org/10.1007/s00134-017-4754-8.
Robba C, Ball L, Battaglini D, Iannuzzi F, Brunetti I, Fiaschi P, Zona G, Taccone FS, Messina A, Mongodi S, Pelosi P. Effects of positive end-expiratory pressure on lung ultrasound patterns and their correlation with intracranial pressure in mechanically ventilated brain injured patients. Crit Care. 2022;26:31. https://doi.org/10.1186/s13054-022-03903-7.
Routsi C, Vincent JL, Bakker J, De Backer D, Lejeune P, d’Hollander A, Le Clerc JL, Kahn RJ. Relation between oxygen consumption and oxygen delivery in patients after cardiac surgery. Anesth Analg. 1993. https://doi.org/10.1213/00000539-199312000-00004.
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G. Lung recruitment in patients with the acute respiratory distress syndrome. N Eng J Med. 2006;354:1775–86.
Romagnoli S, Bevilacqua S, Lazzeri C, Ciappi F, Dini D, Pratesi C, Gensini GF, Romano SM. Most Care®: a minimally invasive system for hemodynamic monitoring powered by the Pressure Recording Analytical Method (PRAM). HSR Proc Intensive Care Cardiovasc Anesth. 2009;1:20–7.
Hirayama I, Asada T, Yamamoto M, Hayase N, Hiruma T, Doi K. Changes in carbon dioxide production and oxygen uptake evaluated using indirect calorimetry in mechanically ventilated patients with sepsis. Crit Care. 2021;25:416. https://doi.org/10.1186/s13054-021-03830-z.
Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, Chieregato A, Cinotti R, Duranteau J, Einav S, Ercole A, Ferguson N, Guerin C, Siempos II, Kurtz P, Juffermans NP, Mancebo J, Mascia L, McCredie V, Nin N, Oddo M, Pelosi P, Rabinstein AA, Neto AS, Seder DB, Skrifvars MB, Suarez JI, Taccone FS, van der Jagt M, Citerio G, Stevens RD. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46:2397–410. https://doi.org/10.1007/s00134-020-06283-0.
Hyder F, Rothman DL, Bennett MR. Cortical energy demands of signaling and nonsignaling components in brain are conserved across mammalian species and activity levels. Proc Natl Acad Sci USA. 2013;110:3549–54. https://doi.org/10.1073/pnas.1214912110.
Morbitzer KA, Wilson WS, Chaben AC, Darby A, Dehne KA, Brown ER, Rhoney DH, Jordan JD. Energy expenditure in critically Ill adult patients with acute brain injury: indirect calorimetry vs. Predictive Equations. Front Neurol. 2019;10:1426. https://doi.org/10.3389/fneur.2019.01426.
Watts ME, Pocock R, Claudianos C. Brain energy and oxygen metabolism: emerging role in normal function and disease. Front Mol Neurosci. 2018;11:216. https://doi.org/10.3389/fnmol.2018.00216.
Chen H, Zhou X-F, Zhou D-W, Zhou J-X, Yu R-G. Effect of increased positive end-expiratory pressure on intracranial pressure and cerebral oxygenation: impact of respiratory mechanics and hypovolemia. BMC Neurosci. 2021;22:72. https://doi.org/10.1186/s12868-021-00674-9.
Gattinoni L, Vassalli F, Romitti F. Benefits and risks of the P/F approach. Intensive Care Med. 2018;44:2245–7. https://doi.org/10.1007/s00134-018-5413-4.
Luecke T, Pelosi P. Clinical review: positive end-expiratory pressure and cardiac output. Crit Care. 2005;9:607–21. https://doi.org/10.1186/cc3877.
Clapis FCM, Auxiliadora-Martins M, Japur CC, Martins-Filho OA, Évora PRB, Basile-Filho A. Mechanical ventilation mode (volume × pressure) does not change the variables obtained by indirect calorimetry in critically ill patients. J Crit Care. 2010;25:659.e9-16. https://doi.org/10.1016/j.jcrc.2009.11.010.
Cecchini S, Schena E, Cuttone R, Carassiti M, Silvestri S (2011) Influence of ventilatory settings on indirect calorimetry in mechanically ventilated patients. In: 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE, pp 1245–8
Kagan I, Zusman O, Bendavid I, Theilla M, Cohen J, Singer P. Validation of carbon dioxide production (VCO2) as a tool to calculate resting energy expenditure (REE) in mechanically ventilated critically ill patients: a retrospective observational study. Crit Care. 2018;22:186. https://doi.org/10.1186/s13054-018-2108-8.
Vargas M, Sutherasan Y, Gregoretti C, Pelosi P. PEEP Role in ICU and operating room: from pathophysiology to clinical practice. Sci World J. 2014. https://doi.org/10.1155/2014/852356.
Levenbrown Y, Hossain MJ, Keith JP, Burr K, Hesek A, Shaffer T. The effect of positive end-expiratory pressure on cardiac output and oxygen delivery during cardiopulmonary resuscitation. Intensive Care Med Exp. 2020;8:36. https://doi.org/10.1186/s40635-020-00330-2.
Jellinek H, Krenn H, Oczenski W, Veit F, Schwarz S, Fitzgerald RD. Influence of positive airway pressure on the pressure gradient for venous return in humans. J Appl Physiol. 2000;88:926–32. https://doi.org/10.1152/jappl.2000.88.3.926.
Sakurai A, Ihara S, Tagami R, Yamaguchi J, Sugita A, Kuwana T, Sawada N, Hori S, Taniguch T, Kinoshita K. Parameters influencing brain oxygen measurement by regional oxygen saturation in postcardiac arrest patients with targeted temperature management. Ther Hypothermia Temp Manag. 2020;10:71–5. https://doi.org/10.1089/ther.2019.0032.
Yang X, Lei X, Zhang L, Zhang L, Dong W. The application of near-infrared spectroscopy in oxygen therapy for premature infants. J Matern Fetal Neonatal Med. 2020;33:283–8. https://doi.org/10.1080/14767058.2018.1489535.
Harper AM, Glass HI. Effect of alterations in the arterial carbon dioxide tension on the blood flow through the cerebral cortex at normal and low arterial blood pressures. J Neurol Neurosurg Psychiatry. 1965;28:449–52. https://doi.org/10.1136/jnnp.28.5.449.
Kety SS, Schmidt CF. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Investig. 1948;27:484–92. https://doi.org/10.1172/JCI101995.
Yamamoto M. Aging and cerebral vasodilator responses to hypercarbia. Arch Neurol. 1980;37:489. https://doi.org/10.1001/archneur.1980.00500570037005.
Stepanek J, Dunn RA, Pradhan GN, Cevette MJ. Supplemental CO2 improves oxygen saturation, oxygen tension, and cerebral oxygenation in acutely hypoxic healthy subjects. Physiol Rep. 2020. https://doi.org/10.14814/phy2.14513.
Beilman GJ, Groehler KE, Lazaron V, Ortner JP. Near-infrared spectroscopy measurement of regional tissue oxyhemoglobin saturation during hemorrhagic shoCK. Shock. 1999;12:196–200. https://doi.org/10.1097/00024382-199909000-00005.
Lubarsky DA, Griebel JA, Carnporesi EM, Piantadosi CA. Comparison of systemic oxygen delivery and uptake with NIR spectroscopy of brain during normovolemic hemodilution in the rabbit. Resuscitation. 1992;23:45–57. https://doi.org/10.1016/0300-9572(92)90161-5.
Robba C, Battaglini D, Rasulo F, Lobo FA, Matta B. The importance of monitoring cerebral oxygenation in non brain injured patients. J Clin Monit Comput. 2023. https://doi.org/10.1007/s10877-023-01002-8.
Suter PM, Fairley HB, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292:284–9. https://doi.org/10.1056/NEJM197502062920604.
Lange F, Tachtsidis I. Clinical brain monitoring with time domain NIRS: a review and future perspectives. Appl Sci. 2019;9:1612. https://doi.org/10.3390/app9081612.
Robba C, Taccone FS, Citerio G. Monitoring cerebral oxygenation in acute brain-injured patients. Intensive Care Med. 2022;48:1463–6. https://doi.org/10.1007/s00134-022-06788-w.
Brower R, Matthay M, Morris A, Schoenfeld D, Thompson B, Wheeler A. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N Engl J Med. 2000;342:1301–8. https://doi.org/10.1056/NEJM200005043421801.
Donati A, Damiani E, Domizi R, Pierantozzi S, Calcinaro S, Pelaia P. Near-infrared spectroscopy to assess tissue oxygenation in patients with polytrauma: relationship with outcome. Crit Care. 2015;19:P308. https://doi.org/10.1186/cc14388.
Jackson PA, Kennedy DO. The application of near infrared spectroscopy in nutritional intervention studies. Front Hum Neurosci. 2013;7:473. https://doi.org/10.3389/fnhum.2013.00473.
Wood MD, Boyd JG, Wood N, Frank J, Girard TD, Ross-White A, Chopra A, Foster D, Griesdale DE. The use of near-infrared spectroscopy and/or transcranial doppler as non-invasive markers of cerebral perfusion in adult sepsis patients with delirium: a systematic review. J Intensive Care Med. 2021. https://doi.org/10.1177/0885066621997090.
Taran S, Pelosi P, Robba C. Optimizing oxygen delivery to the injured brain. Curr Opin Crit Care. 2022;28:145–56. https://doi.org/10.1097/MCC.0000000000000913.
Robba C, Cardim D, Ball L, Battaglini D, Dabrowski W, Bassetti M, Giacobbe DR, Czosnyka M, Badenes R, Pelosi P, Matta B, GeCovid group. The use of different components of brain oxygenation for the assessment of cerebral haemodynamics: a prospective observational study on COVID-19 patients. Front Neurol. 2021;12:735469. https://doi.org/10.3389/fneur.2021.735469.
Collette SL, Rodgers MP, van Walderveen MAA, Compagne KCJ, Nederkoorn PJ, Hofmeijer J, Martens JM, de Borst GJ, Luijckx GJR, Majoie CBLM, van der Lugt A, Bokkers RPH, Uyttenboogaart M. Management of extracranial carotid artery stenosis during endovascular treatment for acute ischaemic stroke: results from the MR CLEAN registry. Stroke Vasc Neurol. 2022. https://doi.org/10.1136/svn-2022-001891.
Eleveld N, Esquivel-Franco DC, Drost G, Absalom AR, Zeebregts CJ, de Vries J-PPM, Elting JWJ, Maurits NM. The influence of extracerebral tissue on continuous wave near-infrared spectroscopy in adults: a systematic review of in vivo studies. J Clin Med. 2023;12:2776. https://doi.org/10.3390/jcm12082776.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception, design: DB, CR. Data collection: DB, LD, DM. Statistical analysis: DB. Data interpretation: DB, CR, PP. Writing first draft: DB. Editing, supervision: CR. Intellectual content, critical revision, editing: DB, CR, PRM, PL, BM, PP.
Corresponding author
Ethics declarations
Conflict of interest
BM is consultant for Masimo. CR gave lectures for Masimo, DB for Baxter (COSMED).
Ethical Approval
This is a single center, prospective physiological cross-sectional observational study approved by the Institutional Review Board Comitato Etico Regione Liguria (N°23/2020).
Informed consent
According to local regulations, informed consent was obtained from patients’ next of kin, as all patients were unconscious at the time of inclusion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Battaglini, D., Delpiano, L., Masuello, D. et al. Effects of positive end-expiratory pressure on brain oxygenation, systemic oxygen cascade and metabolism in acute brain injured patients: a pilot physiological cross-sectional study. J Clin Monit Comput 38, 165–175 (2024). https://doi.org/10.1007/s10877-023-01042-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01042-0