Abstract
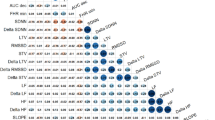
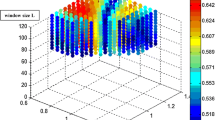
Fetal well-being during labor is usually assessed by visual analysis of a fetal heart rate (FHR) tracing. Our primary objective was to evaluate the ability of automated heart rate variability (HRV) analysis methods, including our new fetal stress index (FSI), to predict neonatal acidosis. 552 intrapartum recordings were analyzed. The analysis occurred in the last 90 min before birth and was conducted during two 5-min intervals: (i) a stable period of FHR and (ii) the period corresponding to the maximum FSI value. For each period, we computed the mean FHR, FSI, short-term variability (STV), and long-term variability (LTV). Visual FHR interpretation was performed using the FIGO classification. The population was separated into two groups: (i) an acidotic group with an arterial pH at birth ≤ 7.10 and a control group. Prediction of a neonatal pH ≤ 7.10 was assessed by computing the receiver-operating characteristic area under the curve (AUC). FHR, FSI, STV, and LTV did not differ significantly between groups during the stable period. During the FSI max peak period, LTV and STV correlated significantly in the acidotic group (– 5.85 ± 2.19, p = 0.010 and – 0.62 ± 0.29, p = 0.037, respectively). The AUC values were 0.569 for FIGO classification, 0.595 for STV, and 0.622 for LTV. The multivariate model (FIGO, FSI, FC, STV, LTV) had the greatest accuracy for predicting acidosis (AUC = 0.719). FSI was not predictive of neonatal acidosis probably because of the low quality of the FHR signal in cardiotocography. When used separately, HRV indexes and visual FHR analysis were poor predictors of neonatal acidosis. Including all indexes in a multivariate model increased the predictive ability.




Similar content being viewed by others
References
Rei M, Ayres-de-Campos D, Bernardes J. Neurological damage arising from intrapartum hypoxia/acidosis. Best Pr Res Clin Obstet Gynaecol. 2016;30:79–86.
Low JA, Galbraith RS, Muir DW, Killen HL, Pater EA, Karchmar EJ. Factors associated with motor and cognitive deficits in children after intrapartum fetal hypoxia. Am J Obstet Gynecol. 1984;148:533–9.
Paneth N, et al. Electronic fetal monitoring and later outcome. Clin Invest Med. 1993;162:159–65.
Spencer JA. Clinical overview of cardiotocography. BJOG Int J Obstet Gynaecol. 1993;100:4–7.
Blackwell SC, Grobman WA, Antoniewicz L, Hutchinson M, Bannerman CG. Interobserver and intraobserver reliability of the NICHD 3-Tier Fetal Heart Rate Interpretation System. Am J Obstet Gynecol. 2011;205:378.e1–.e5. https://doi.org/10.1016/j.ajog.2011.06.086.
Ayres-de-Campos D, Spong CY, Chandraharan E. FIGO intrapartum fetal monitoring expert consensus panel. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynecol Obstet. 2015;131:13–24. https://doi.org/10.1016/j.ijgo.2015.06.020.
Chandraharan E. Fetal scalp blood sampling during labour: is it a useful diagnostic test or a historical test that no longer has a place in modern clinical obstetrics? BJOG Int J Obstet Gynaecol. 2014;121:1056–62. https://doi.org/10.1111/1471-0528.12614.
Belfort MA, Saade GR, Thom E, Blackwell SC, Reddy UM, Thorp JM, et al. A randomized trial of intrapartum fetal ECG ST-segment analysis. N Engl J Med. 2015;373:632–41. https://doi.org/10.1056/NEJMoa1500600.
Pinas A, Chandraharan E. Continuous cardiotocography during labour: analysis, classification and management. Best Pract Res Clin Obstet Gynaecol. 2016;30:33–47. https://doi.org/10.1016/j.bpobgyn.2015.03.022.
Lear CA, Galinsky R, Wassink G, Yamaguchi K, Davidson JO, Westgate JA, et al. The myths and physiology surrounding intrapartum decelerations: the critical role of the peripheral chemoreflex. J Physiol. 2016;594:4711–25. https://doi.org/10.1113/JP271205.
Van Laar J, Peters C, Vullings R, Houterman S, Bergmans J, Oei S. Fetal autonomic response to severe acidaemia during labour: fetal autonomic stress response during labour. BJOG Int J Obstet Gynaecol. 2010;117:429–37. https://doi.org/10.1111/j.1471-0528.2009.02456.x.
Van Ravenswaaij-Arts CM, Kollée LA, Hopman JC, Stoelinga GB, van Geijn HP. Heart rate variability. Ann Intern Med. 1993;118:436–47.
Romano M, Iuppariello L, Ponsiglione AM, Improta G, Bifulco P, Cesarelli M. Frequency and time domain analysis of foetal heart rate variability with traditional indexes: a critical survey. Comput Math Methods Med. 2016;2016:9585431. https://doi.org/10.1155/2016/9585431.
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–81.
Chaffin DG, Goldberg CC, Reed KL. The dimension of chaos in the fetal heart rate. Am J Obstet Gynecol. 1991;165:1425–9.
Street P, Dawes GS, Moulden M, Redman CWG. Short-term variation in abnormal antenatal fetal heart rate records. Am J Obstet Gynecol. 1991;165:515–23. https://doi.org/10.1016/0002-9378(91)90277-X.
Lu K, Holzmann M, Abtahi F, Lindecrantz K, Lindqvist PG, Nordstrom L. Fetal heart rate short term variation during labor in relation to scalp blood lactate concentration. Acta Obstet Gynecol Scand. 2018;97:1274–80. https://doi.org/10.1111/aogs.13390.
Wretler S, Holzmann M, Graner S, Lindqvist P, Falck S, Nordström L. Fetal heart rate monitoring of short term variation (STV): a methodological observational study. BMC Pregnancy Childbirth. 2016;16:55. https://doi.org/10.1186/s12884-016-0845-8.
Lear CA, Galinsky R, Wassink G, Mitchell CJ, Davidson JO, Westgate JA, et al. Sympathetic neural activation does not mediate heart rate variability during repeated brief umbilical cord occlusions in near-term fetal sheep. J Physiol. 2016;594:1265–77. https://doi.org/10.1113/JP270125.
Garabedian C, Champion C, Servan-Schreiber E, Butruille L, Aubry E, Sharma D, et al. A new analysis of heart rate variability in the assessment of fetal parasympathetic activity: an experimental study in a fetal sheep model. PLoS ONE. 2017;12:e0180653. https://doi.org/10.1371/journal.pone.0180653.
Ghesquière L, De Jonckheere J, Drumez E, Sharma D, Aubry E, Deruelle P, et al. Parasympathetic nervous system response to acidosis: evaluation in an experimental fetal sheep model. Acta Obstet Gynecol Scand. 2018. https://doi.org/10.1111/aogs.13515.
Chudáček V, Spilka J, Burša M, Janků P, Hruban L, Huptych M, et al. Open access intrapartum CTG database. BMC Pregnancy Childbirth. 2014;14:16. https://doi.org/10.1186/1471-2393-14-16.
Garabedian C, Clermont-Hama Y, Sharma D, Aubry E, Butruille L, Deruelle P, et al. Correlation of a new index reflecting the fluctuation of parasympathetic tone and fetal acidosis in an experimental study in a sheep model. PLoS ONE. 2018;13:e0190463.
Butruille L, De Jonckheere J, Flocteil M, Garabedian C, Houfflin-Debarge V, Storme L, et al. Parasympathetic tone variations according to umbilical cord pH at birth: a computerized fetal heart rate variability analysis. J Clin Monit Comput. 2017;31:1197–202. https://doi.org/10.1007/s10877-016-9957-y.
Garabedian C, Butruille L, Servan-Schreiber E, Ficheur G, Storme L, Deruelle P, et al. Fetal heart-rate variability: validation of a new continuous. Noninvas Comput Anal Gynecol Obstet Invest. 2017;82:500–7. https://doi.org/10.1159/000452668.
Dawes GS, Moulden M, Redman CW. System 8000: computerized antenatal FHR analysis. J Perinat Med. 1991;19:47–51.
Cesarelli M, Romano M, Bifulco P. Comparison of short term variability indexes in cardiotocographic foetal monitoring. Comput Biol Med. 2009;39:106–18. https://doi.org/10.1016/j.compbiomed.2008.11.010.
Van Leeuwen P, Werner L, Hilal Z, Schiermeier S, Hatzmann W, Grönemeyer D. Fetal electrocardiographic measurements in the assessment of fetal heart rate variability in the antepartum period. Physiol Meas. 2014;35:441–54. https://doi.org/10.1088/0967-3334/35/3/441.
Grimm B, Haueisen J, Huotilainen M, Lange S, Van Leeuwen P, Menendez T, et al. Recommended standards for fetal magnetocardiography. Pacing Clin Electrophysiol PACE. 2003;26:2121–6.
Van Laar JOEH, Porath MM, Peters CHL, Oei SG. Spectral analysis of fetal heart rate variability for fetal surveillance: review of the literature. Acta Obstet Gynecol Scand. 2008;87:300–6. https://doi.org/10.1080/00016340801898950.
Schiermeier S, Reinhard J, Hatzmann H, Zimmermann RC, Westhof G. Fetal short time variation during labor: a non-invasive alternative to fetal scalp pH measurements? J Perinat Med. 2009;37:529–33. https://doi.org/10.1515/JPM.2009.089.
Signorini MG, Magenes G, Cerutti S, Arduini D. Linear and nonlinear parameters for the analysis of fetal heart rate signal from cardiotocographic recordings. IEEE Trans Biomed Eng. 2003;50:365–74. https://doi.org/10.1109/TBME.2003.808824.
Ayres-de-Campos D, Arteiro D, Costa-Santos C, Bernardes J. Knowledge of adverse neonatal outcome alters clinicians’ interpretation of the intrapartum cardiotocograph. BJOG Int J Obstet Gynaecol. 2011;118:978–84. https://doi.org/10.1111/j.1471-0528.2011.03003.x.
Jenniskens K, Janssen PA. Newborn outcomes in british columbia after caesarean section for non-reassuring fetal status. J Obstet Gynaecol Can JOGC. 2015;37:207–13. https://doi.org/10.1016/S1701-2163(15)30306-6.
Clifford G, Sameni R, Ward J, Robinson J, Wolfberg AJ. Clinically accurate fetal ECG parameters acquired from maternal abdominal sensors. Am J Obstet Gynecol. 2011;205(47):e1–5. https://doi.org/10.1016/j.ajog.2011.02.066.
Acknowledgement
This work was supported by the French National Research Agency (ANR) under grant number ANR-18-CE19-0015-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ethics statement is explained in the paper by Chudáček et al. [22]. The CTG recordings and clinical data were matched using anonymized unique identifiers generated by the hospital information system. The timings of the CTG records were matched to the stages of labor (first and second stage) and were made relative to the time of birth, and were also deidentified. This study was approved by the Institutional Review Board of University Hospital Brno, and all women signed an informed consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gatellier, MA., De Jonckheere, J., Storme, L. et al. Fetal heart rate variability analysis for neonatal acidosis prediction. J Clin Monit Comput 35, 771–777 (2021). https://doi.org/10.1007/s10877-020-00535-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00535-6