Abstract
The effects of a recruitment manoeuvre (RM) with positive end-expiratory pressure (PEEP) on lung compliance (CLUNG) are not well characterised in robot-assisted laparoscopic radical prostatectomy (RARP). Patients were allocated to group R (n = 10; with an RM) or C (n = 9; without an RM). An RM involved sustained inflation of 30 cmH2O for 30 s. The lungs were ventilated with volume-controlled ventilation with tidal volume of 7 mL kg−1 of predicted body weight and fraction of inspired oxygen of 0.5. End-tidal carbon dioxide pressure was maintained at normocapnia. Patients were in the horizontal lithotomy position (pre-op). After pneumoperitoneum, patients underwent RARP in a steep Trendelenburg lithotomy position at a PEEP level of 0 cmH2O (RARP0). An RM was used in the R group but not in the C group. Patients were then ventilated with 5 cmH2O PEEP for 1 h after RARP0 (RARP5.1) and 2 h after RARP0 (RARP5.2). Oesophageal pressure and airway pressure were measured for calculating CLUNG and chest wall compliance. CLUNG significantly decreased from pre-op to RARP0 and did not significantly increase from RARP0 to RARP5.1 and RARP5.2 in either group. CLUNG differed significantly between groups at RARP5.1 and RARP5.2 (103 ± 30 vs. 68 ± 11 mL cm−1 H2O and 106 ± 35 vs. 72 ± 9 mL cm−1 H2O; P < 0.05). In patients undergoing RARP, with the addition of RM, the CLUNG was effectively increased from the horizontal lithotomy position to the steep Trendelenburg lithotomy position under pneumoperitoneum.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
1 Introduction
Using lung protective ventilation (LPV) strategies in patients at risk of postoperative pulmonary complications undergoing major abdominal procedures has become an area of interest in recent years. However, controversy persists around which features of LPV are beneficial in this group, as the largest study utilised low tidal volumes [1], a recruitment manoeuvre (RM), and positive end-expiratory pressure (PEEP). Although there has been much recent research in this area, key uncertainties in perioperative ventilation remain.
Since the introduction of computer-enhanced robotic surgi-cal systems in 2001, robot-assisted laparoscopic radical prostatectomy (RARP) has been commonly used in the surgical treatment of prostate cancer. RARP presents several advantages over conventional surgery, including nerve sparing, shorter hospitalization times, reduced blood loss, and less postoperative pain [2, 3]. However, to maximize the surgical visual field, RARP usually requires the patient to be placed in a steep Trendelenburg lithotomy position with a pneumoperitoneum.
Both the increase in abdominal pressure because of a pneumoperitoneum with CO2 insufflation and the steep Trendelenburg lithotomy position during RARP have been shown to impair respiratory function, mainly inducing atelectasis formation in the dependent lung regions [4].
Recent clinical data have demonstrated that a mechanical ventilatory strategy using lower tidal volumes and PEEP decreases the risk of pulmonary complications by minimising alveolar stretching at the end of inspiration and thus avoiding possible inflammation or alveolar collapse [5]. Using PEEP after recruitment can reportedly prevent re-collapse of the alveoli [6,7,8]. The distinct differences seen in compliance at identical pressure levels before and after recruitment support the idea of a gain in the number of open alveoli by the RM itself [9]. Recent clinical studies have also reported that mechanical ventilation using PEEP with or without an RM could help improve intraoperative arterial partial pressure of oxygen (PaO2) and lung compliance (CLUNG) and reduce pulmonary shunt fraction [10, 11]. However, the effects of an RM with PEEP on CLUNG are not well characterised in patients undergoing RARP. To the best of our knowledge, the effects of an RM with PEEP on CLUNG in patients undergoing RARP have not been thoroughly investigated.
Therefore, the aim of this study was to evaluate the effects of an RM on respiratory and ventilatory parameters and arterial blood gas analysis in patients undergoing RARP.
2 Methods
This single-centre, prospective, randomized, comparative clinical and observational study was approved by the Ethics Committee of Juntendo University Hospital. Written informed consent was obtained from all 19 adult male patients enrolled in the study. This registered clinical trial (UMIN000013888) included consecutive patients undergoing RARP from November 2013 to May 2014. We enrolled non-smoking patients aged 20–70 years with an American Society of Anesthesiologists (ASA) Physical Status Classification score of 1–2 who were scheduled for RARP using a computer-enhanced robotic operating system (da Vinci™ Surgical System, Intuitive Surgical, Inc., Sunnyvale, CA, USA). Patients with a known history of chronic obstructive pulmonary disease, renal or heart failure, or obesity [defined as a body mass index (BMI) ≥ 30 kg m−2] were excluded from the study. No premedication was given. Upon arriving in the operating theatre, patients were monitored by electrocardiography, pulse oximetry, capnography, non-invasive automated arterial pressure measurement, and temperature measurement using a patient monitor (BSM-5135; Nihon Kohden Corp., Tokyo, Japan). Patients were breathing a fraction of inspired oxygen (FIO2) of 1.0 during the induction of general anaesthesia using remifentanil at a rate of 0.4–0.8 μg kg−1 min−1 and propofol via target-controlled infusion to a plasma concentration of 4 μg mL−1. The lungs were ventilated manually via a face mask with an FIO2 of 1.0. Muscle paralysis was achieved with rocuronium 0.6 mg kg−1 to facilitate the orotracheal intubation. Patients were intubated via a cuffed tracheal tube reinforced with a stylet with an internal diameter of 8.0 mm (Mallinckrodt™ endotracheal tube; Covidien plc., Dublin, Ireland). The lungs were ventilated mechanically through a ventilator (AVEA™ Ventilator Systems; CareFusion Inc., San Diego, CA, USA) with volume-controlled ventilation with an inspiratory pause of 10%, an inspiratory to expiratory ratio of 1:2, and a tidal volume (VT) of 7 mL kg−1 of the predicted body weight. The predicted body weight was calculated as 49.9 + 0.91 × [height (cm) − 152.4]. The respiratory rate (RR) was 12 bpm and varied to maintain eucapnia (end-tidal carbon dioxide partial pressure [EtCO2] of 40–50 mmHg). Patients were ventilated using oxygen and air with an FIO2 of 0.5 as needed to maintain an oxygen saturation (SaO2) ≥ 95%. PEEP was not initially added. An arterial cannula was inserted percutaneously into the radial artery of the non-dominant hand after the induction of anaesthesia, in line with the standard practice of our institution for continuous arterial pressure monitoring and blood gas sampling. An arterial blood gas analysis was performed within 1 min of sampling using a blood gas analyser (RAPIDLab® 1200 Systems; Siemens Healthcare GmbH, Erlangen, Germany). Patients were placed in the horizontal lithotomy position. Anaesthesia was maintained with a continuous infusion of propofol, remifentanil, and rocuronium throughout the surgery. Adequate anaesthetic depth was maintained by bispectral index monitoring (Aspect A-2000™; Aspect Medical System, Inc., Newton, MA, USA). The infusion rate of propofol was varied to maintain the bispectral index in the range of 40–60. Maintenance of haemodynamic stability (arterial systolic pressure and heart rate 80–100% of the pre-anaesthetic value) included administration of remifentanil at a rate of 0.1–0.2 μg kg−1 min−1. The neuromuscular block was maintained with the administration of rocuronium at a rate of 0.4 mg kg−1 h−1. Standardised fluid management was performed in patients using a crystalloid solution (acetated Ringer’s solution; Terumo®, Tokyo, Japan) at a rate of 20 mL kg−1 h−1 immediately before the anaesthetic induction and until the patient was placed in a steep Trendelenburg lithotomy position, followed by 5 kg−1 h−1 until the end of the surgery. The occurrence of intraoperative hypotension (mean arterial pressure < 65 mmHg or a decrease in mean arterial pressure > 20% of baseline for more than 5 min) was managed with a bolus of a 10 mL kg−1 crystalloid solution with an incremental administration of intravenous vasoactive drugs (ephedrine 4 mg or phenylephrine 0.05 mg), as appropriate. To maintain normothermia, a heating blanket (Bair Hugger™; Augustine Medical Inc., Eden Prairie, MN, USA) and a blood and fluid warming system (Ranger™, Augustine Medical Inc.) were used, whereas no warmed infusions were used. Operating room temperatures were kept at approximately 23 °C (73.4 °F). During RARP, patients were in a steep Trendelenburg lithotomy position, a pneumoperitoneum was established with CO2 insufflation, and the intra-abdominal pressure (IAP) was maintained automatically at 10 mmHg. At the end of the surgery, the infusions of propofol and remifentanil were discontinued and the residual neuromuscular paralysis was reversed with sugammadex 0.2-0.4 mg kg−1.
2.1 Study protocol
To analyse the effects of an RM, patients were allocated to one of two groups; 10 with an RM (R group) and 9 without an RM (C group). The RM used in this study involved a sustained inflation of 30 cmH2O applied for 30 s. Patient allocation was performed by a researcher who was not involved in anaesthesia care or the outcome analysis. Random assignments were made using sealed envelopes. The attending anaesthesiologists and outcome assessors were aware of the allocated RM, but the patients, urologists, and data analysts were blinded to the interventional details.
About 30 min after pneumoperitoneum induction, if the patients were haemodynamically stable (i.e., mean arterial pressure ≥ 65 mmHg and heart rate ≥ 50 beats min−1), the protocol was started as follows.
Data were collected at the following time points:
-
(1)
30 min after anaesthesia induction in the horizontal lithotomy position before pneumoperitoneum induction (pre-op);
-
(2)
30 min after pneumoperitoneum induction (abdominal CO2 insufflation to obtain and IAP of 10 mmHg) (pneumo);
-
(3)
30 min after the establishment of a steep Trendelenburg lithotomy position (the patient positioned at 26° head down) (RARP0), the following occurs:
-
R group participants then received a single RM that involved sustained inflation of 30 cmH2O applied for 30 s. After the RM, the ventilator was immediately switched back to volume-controlled mode and was carefully added a PEEP level of 5 cmH2O.
-
C group participants did not receive the RM, and the ventilator was carefully added a PEEP level of 5 cmH2O.
-
-
(4)
1 h after achieving a PEEP level of 5 cmH2O (RARP5.1);
-
(5)
2 h after achieving a PEEP level of 5 cmH2O (RARP5.2); and
-
(6)
At the end of surgery, after abdominal deflation and in the horizontal lithotomy position with a PEEP level of 5 cmH2O (post-op).
The data collected or calculated continuously throughout this study included the following:
-
Respiratory and ventilatory parameters: exhaled VT (Vte), plateau pressure (PPLAT), PEEP, static compliance (CSTAT), chest wall compliance (CCW), CLUNG, RR, and EtCO2.
-
Arterial blood gas analysis: PaO2, arterial partial pressure of carbon dioxide (PaCO2), pH, and SaO2.
-
Haemodynamics: mean arterial pressure and heart rate.
-
Complications of pneumoperitoneum, positioning, or anaesthesia during surgery.
2.2 Monitoring
Here, we continuously monitored and recorded oesophageal pressure (POES). During mechanical ventilation, the distending force of the lung is the transpulmonary pressure [12], that is, the difference between airway pressure (PAW) and the pressure required to expand the chest wall [13, 14] that is clinically estimated by measuring POES as a surrogate of pleural pressure [15]. POES was used for CCW and CLUNG using a ventilator (comprehensive model of AVEA™ Ventilator Systems; CareFusion, Inc.). The patients were kept in the horizontal lithotomy position. Air flow was measured with pneumotachography. For measuring POES, an oesophageal balloon-tipped catheter (SmartCath™, Vyaire Medical Inc., Mettawa, IL, USA) was inserted transnasally and advanced into the oesophagus. To airway pressure (PAW) measurement accuracy, a tracheal catheter (P/N 110635™; Cardinal Health, Inc., Dublin, OH, USA) was placed in an endotracheal tube using a sealed sideport connector and not extended beyond the tip of the tube. A pressure sensor of the oesophageal and the tracheal catheter was attached to the ventilator at the connection on the front panel identified with the legend POES and Aux, respectively. All data were recorded and analysed using an optimal waveform in computer software. The waveform produced during insertion provided information to confirm proper placement. After the oesophageal balloon was filled with 0.5–1 mL of air and the pressure was monitored and measured, POES was waveform should be compared with PAW waveform. POES waveform correlates to PAW in that they become positive during a positive pressure breath and negative during a spontaneous breath. The oesophageal tracing showed small cardiac oscillations reflective of cardiac activity, indicating that the balloon was positioned in the lower third of the oesophagus directly behind the heart. Once placed using the above criteria, the appropriate balloon location confirmed using an occlusion technique. This required that the airway was occluded and POES and PAW were compared for similarity. Furthermore, we confirmed correct placement of the oesophageal and tracheal catheter on postoperative chest radiography.
2.3 Data analysis
Age, ASA Physical Status Classification, height, weight, and BMI were recorded. Physiological variables involved in this study were evaluated and recorded by an investigator who was blinded to the group allocation details. The magnitudes of PAW and POES were measured and obtained directly from the ventilator. CSTAT, CCW and CLUNG were calculated using the following equations:
-
CSTAT = Vt/(PPLAT − PEEP)
-
CCW = Vte/dPOES, where dPOES = PPEAK OES − PEEPOES
-
CLUNG = Vte/dPPLAT TP, where dPPLAT TP = (PPLAT AW − POES) − (PEEPAW − PEEPOES)
dPOES, delta POES; PPEAK OES, peak POES; PEEPOES, baseline POES (at the end of exhalation); dPPLAT TP, delta transpulmonary pressure; PPLAT AW, plateau PAW (during an inspiratory pause); POES (at the time airway plateau pressure is measured); PEEPAW, baseline PAW (at the end of an expiratory hold manoeuvre)
-
1/CSTAT = 1/CCW + 1/CLUNG
Vt ≈ Vte, PPEAK OES ≈ POES (at the time PPLAT AW is measured, during an inspiratory pause).
2.4 Statistical analysis
The statistical comparison was performed as follow. All data were tested for normal distribution by the Kolmogorov–Smirnov Goodness-of-Fit test and are presented as mean ± standard deviation (SD). The data analysis was performed using Welch’s t test and repeated-measures analysis of variance; if significant, Scheffe’s test was applied for a post hoc comparison between the different experimental conditions. P values < 0.05 were considered statistically significant.
We estimated that a maximal sample of 24 patients was required to detect CLUNG improvement by the RM from baseline to 145%. The α and β errors for the sample size with a 0.025 level of significance were 0.05 and 0.2, respectively.
All statistical calculations and data analysis were performed using StatView 5.0™ (SAS Institute Inc., Cary, NC).
3 Results
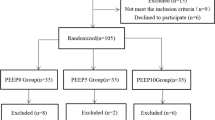
Of the 24 screened patients, 19 patients were finally recruited, 2 patients who were not finally recruited (A time period from RARP0 to RALP5.2 was within 2 h) and 3 patients who refused to participate were excluded. So, this study was a relatively underpowered study. No other patients developed any complications perioperatively related to pneumoperitoneum, positioning, or anaesthesia during surgery. All surgeries were performed successfully without conversion to the open technique. The clinical characteristics of the enrolled patients are shown in Table 1; there were no significant intergroup differences. Respiratory and arterial blood gas analysis data are shown in Table 2.
In the C group, CLUNG significantly decreased from pre-op to RARP0, RARP5.1 (P < 0.01), and RARP5.2 (P < 0.05) but did not significantly increase from RARP0 to RARP5.1 or RARP5.2. In the R group, CLUNG significantly decreased from pre-op to RARP0 (P < 0.05) but did not significantly increase from RARP0 to RARP5.1 or RARP5.2. CLUNG differed significantly between the two groups, at the same time point (RARP5.1 [P < 0.05] and RARP5.2 [P < 0.05]). PaO2 did not significantly change from pre-op to RARP0 but significantly increased from pre-op to RARP5.1, RARP5.2, and post-op in the C group (P < 0.01). PaO2 did not significantly change from pre-op to RARP0 and RARP5.1 but significantly increased from pre-op to RARP5.2 and post-op in the R group (P < 0.01). PaO2 significantly increased from pneumo or RARP0 to RARP5.2 and post-op in the R group (P < 0.01). There were no statistically significant intergroup differences in PaO2 during this procedure. PaCO2 increased in both groups, but there were no statistically significant intergroup differences in PaCO2 during this procedure.
Mean arterial pressure and heart rate remained stable through single RM that involved sustained inflation of 30 cmH2O applied for 30 s at steep Trendelenburg lithotomy position. Intravenous vasoactive drugs (ephedrine 4 mg or phenylephrine 0.05 mg) had been administered only few bolus.
4 Discussion
This small randomised clinical trial evaluated the effects of an RM of 30 cmH2O applied for 30 s on the systemic oxygenation and CLUNG of patients undergoing RARP. The main finding of our study was that an RM with PEEP during RARP was effective at improving CLUNG. After PEEP 5 cmH2O could be not sufficient to restore the atelectasis.
A pneumoperitoneum with CO2 insufflation and steep Trendelenburg lithotomy position are used in combination to optimise the surgical view during RARP. A pneumoperitoneum with CO2 insufflation can affect the cardiopulmonary system in several ways. Lung volumes decrease, mean arterial pressure increases, and CO2 absorption can be associated with acidosis. All of these changes can lead to a wide range of cardiopulmonary distresses [16, 17]. During RARP, use of a steep Trendelenburg position is routinely requested by the surgeons to facilitate exposure of the pelvis and the lower abdomen causes the abdominal contents to push the diaphragm cephalad along with all of the mediastinal structures [18]. The diaphragm cranial shift by the abdominal contents and pneumoperitoneum may lead to an increased PAW, reduce the lung’s functional residual capacity (FRC), decrease CLUNG, predispose the patient to atelectasis, and aggravate a ventilation/perfusion mismatch [4]. CLUNG is reduced, and this continues even after de-sufflation [19]. These pulmonary changes can have significant adverse consequences for patients with abnormal pulmonary mechanics. Maisch studied that the FRC revealed a plausible physiologic picture of the effects of PEEP or of PEEP in conjunction with an RM. At identical pressure levels, a larger FRC can be found after recruitment compared to the corresponding value before it. However, FRC seems unable to detect lung over-distension. Compared to the gain in PEEP before it, a gain in absolute lung volume (i.e., FRC) after recruitment cannot result from a pure distension of aerated alveoli or airways but must be the result of an increase in the number of functional alveolar units. Thus, this is proof of the intended “opening effects” of alveolar recruitment [9].
Several ventilation strategies aimed at improving arterial oxygenation and respiratory mechanics in patients undergoing laparoscopic surgery have been investigated in recent years. Studies have determined that the application of PEEP counterbalances the cranial shift of the diaphragm, thus increasing FRC and respiratory system compliance and reducing respiratory system elasticity [20]. Recent attempts have been made to translate the concept of LPV strategies from the context of adult respiratory distress syndrome [21]. The apparent success of mechanical ventilation based on a strategy of using the lowest PEEP results in acceptable oxygenation [22, 23]. The application of an “open lung” strategy consisting of an RM [24] followed by the subsequent application of PEEP has been suggested to effectively re-expand pneumoperitoneum-induced atelectasis and improve oxygenation in patients undergoing prolonged laparoscopic surgery [25]. In addition, given that the beneficial effects of a single RM is reportedly insufficient [26, 27], a recent clinical study suggested that the repetitive use of RM is a way to improve arterial oxygenation since it keeps the alveoli open and improves aeration [28]. A single application of 40 cmH2O for 7–8 s was reportedly sufficient to prevent postoperative atelectasis after anaesthetic induction in patients with a normal body weight [29], and that an RM with a PEEP of 10 cmH2O significantly improved their intraoperative pulmonary mechanics and oxygenation [9]. However, data on the use of an RM in surgical patients with healthy lungs, particularly those venti-lated with a protective ventilatory strategy, remain insufficient.
In patients who undergo laparoscopic surgery in the Trendelenburg position, an open lung strategy (recruiting pressure of 40 cmH2O and PEEP 5 cmH2O) applied after pneumoperitoneum induction increased transpulmonary pressure and led to alveolar recruitment and improved chest wall elasticity and gas exchange [30]. In the R group, an open lung strategy (sustained inflation of 30 cmH2O for 30 s with a PEEP of 5 cmH2O; mean TV of 7 mL kg−1) applied after pneumoperitoneum in the Trendelenburg position improved CLUNG but did not change PaO2/FIO2 compared with patients in the C group. Compared with the practice of non-protective mechanical ventilation, the use of a lung-protective ventilation strategy (sustained inflation of 30 cmH2O for 30 s with a PEEP of 6–8 cmH2O; mean TV of 6.4 mL kg−1) in patients undergoing major abdominal surgery was associated with improved clinical outcomes and reduced health care utilisation (IMPROVE ClinicalTrials.gov number NCT01282996) [1].
Andersson and colleagues found that the previously seen improvement in arterial oxygenation despite an increase in atelectasis volume could be due to an improved ventilation–perfusion matching during pneumoperitoneum [31]. This may cause ventilation/perfusion matching and maintain the PaO2/FIO2 ratio. The Trendelenburg position decreased FRC, whereas 5 cmH2O PEEP slightly recovered the ventilation/perfusion mismatch in the Trendelenburg position and could result in an increasing PaO2/FIO2 ratio during surgery. A decremental PEEP trial identified a PEEP setting that sustained the oxygenation benefit of a 40 cmH2O, 40 s lung-recruitment manoeuvre for 4 h [32]. Futier used each RM by applying a continuous positive airway pressure of 30 cmH2O for 30 s [1]. With even larger inflation volumes, more than two repeated inflations to the same PAW added little to the recruitment of normal lung tissue [24]. Repeated RM use may be necessary to improve the sustained CLUNG [33].
Our investigation is under powered analysis to evaluate the effects of an RM in patients undergoing RARP and presents some limitations that require consideration. First, the latter value of PEEP could not be sufficient to restore the atelectasis in this study. Second, this study was limited by its small sample size. Therefore, although a single RM did not benefit the systemic oxygenation and CLUNG of surgical patients undergoing RARP in the steep Trendelenburg lithotomy position with a pneumoperitoneum in our trial, this result is difficult to generalise. Third, the study was not conducted in a blinded fashion. The anaesthesiologist was aware of the mode of ventilation. Fourth, enrolled patients had an ASA Physical Status Classification score of 1–2; therefore, our results apply only to healthy patients. Finally, this study did not enrol patients with respiratory diseases or obesity (BMI ≥ 30 kg m−2), as these patients could be more vulnerable to the deterioration of oxygenation and respiratory mechanics during a pneumoperitoneum with CO2 insufflation in a steep Trendelenburg lithotomy position.
5 Conclusion
In patients undergoing RARP, the addition of an RM effectively increased CLUNG from the horizontal lithotomy position to a steep Trendelenburg lithotomy position under pneumoperitoneum. We suggest that by measuring POES to estimate PPLAT TP and CLUNG, mechanical ventilator settings could be more appropriately customised to accommodate interindividual variations in lung and chest wall mechanical characteristics.
This study showed promise for improvements in lung function, a topic that warrants further investigation. Further studies such as a large-scale multicentre studies or well-powered randomised controlled trials are required to more clearly determine the effects of a single RM and validate the use of RM with a lung protective ventilation strategy in patients undergoing RARP.
Change history
13 March 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s10877-023-00993-8
References
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S, IMPROVE Study Group. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Zorn KC, Gofrit ON, Orvieto MA, Mikhail AA, Zagaja GP, Shalhav AL. Robotic-assisted laparoscopic prostatectomy: functional and pathologic outcomes with interfascial nerve preservation. Eur Urol. 2007;51:755–62.
Menon M, Tewari A, Peabody JO, Shrivastava A, Kaul S, Bhandari A, Hemal AK. Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin N Am. 2004;31:701–17.
Baltayian S. A brief review: anesthesia for robotic prostatectomy. J Robot Surg. 2008;2:59–66.
Seiberlich E, Santana JA, Chaves Rde A, Seiberlich RC. Protective mechanical ventilation, why use it? Rev Bras Anestesiol. 2011;61(659–67):361–5.
Tusman G, Böhm SH, Vazquez de Anda GF, do Campo JL, Lachmann B. “Alveolar recruitment strategy” improves arterial oxygenation during general anaesthesia. Br J Anaesth. 1999;82:8–13.
Bohm SH, Vazquez de Anda GF, Lachmann B. The open lung concept. In: Vincent JL, editor. Yearbook of intensive care and emergency medicine. 2nd ed. Berlin: Springer; 1998. p. 430–40.
Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;118:319–21.
Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G, Bohm SH. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106:175–81.
Hartland BL, Newell TJ, Damico N. Alveolar recruitment maneuvers under general anesthesia: a systematic review of the literature. Respir Care. 2015;60:609–20.
Spadaro S, Karbing DS, Mauri T, Marangoni E, Mojoli F, Valpiani G, Carrieri C, Ragazzi R, Verri M, Rees SE, Volta CA. Effects of positive end-expiratory pressure on pulmonary shunt and dynamic compliance during abdominal surgery. Br J Anaesth. 2016;116:855–61.
Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care. 2004;8:350–5.
Ranieri VM, Brienza N, Santostasi S, Puntillo F, Mascia L, Vitale N, Giuliani R, Memeo V, Bruno F, Fiore T, Brienza A, Slutsky AS. Impairment of lung and chest wall mechanics in patients with acute respiratory distress syndrome: role of abdominal disten-sion. Am J Respir Crit Care Med. 1997;156:1082–91.
Talmor D, Sarge T, O’Donnell CR, Ritz R, Malhotra A, Lisbon A, Loring SH. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med. 2006;34:1389–94.
Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982;126:788–91.
Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, Struys MM. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433–9.
Phong SV, Koh LK. Anaesthesia for robotic-assisted radical prostatectomy: considerations for laparoscopy in the Trendelenburg position. Anaesth Intensive Care. 2007;35:281–5.
Gainburg DM. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012;78:596–604.
Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110:810–5.
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, Tallarini F, Cozzi P, Cressoni M, Colombo A, Marini JJ, Gattinoni L. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–55.
Talmor D, Sarge T, Malhotra A, O’Donnell CR, Ritz R, Lisbon A, Novack V, Loring SH. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359:2095–104.
Albert RK. Least PEEP: primum non nocere. Chest. 1985;87:2–4.
Petty TL. The use, abuse, and mystique of positive end-expiratory pressure. Am Rev Respir Dis. 1988;138:475–8.
Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna G. Re-expansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth. 1993;71:788–95.
Meininger D, Byhahn C, Mierdl S, Westphal K, Zwissler B. Positive end-expiratory pressure improves arterial oxygenation during prolonged pneumoperitoneum. Acta Anaesthesiol Scand. 2005;49:778–83.
Grasso S, Mascia L, Del Turco M, Malacarne P, Giunta F, Brochard L, Slutsky AS, Marco Ranieri V. Effects of recruiting maneuvers in patients with acute respiratory distress syndrome ventilated with protective ventilatory strategy. Anesthesiology. 2002;96:795–802.
Futier E, Constantin JM, Pelosi P, Chanques G, Kwiatkoskwi F, Jaber S, Bazin JE. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;113:1310–9.
Trojik T, Shosholcheva M, Radulovska-Chabukovska J, Lovach-Chepujnoska M. Evaluation of effects of repetitive recruitment maneuvers. Acta Inform Med. 2012;20:85–9.
Rothen HU, Neumann P, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G. Dynamics of re-expansion of atelectasis during general anaesthesia. Br J Anaesth. 1999;82:551–6.
Cinnella G, Grasso S, Spadaro S, Rauseo M, Mirabella L, Salatto P, De Capraris A, Nappi L, Greco P, Dambrosio M. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2013;118:114–22.
Andersson LE, Bååth M, Thörne A, Aspelin P, Odeberg-Wernerman S. Effects of carbon dioxide pneumoperitoneum on development of atelectasis during anesthesia, examined by spiral computed tomography. Anesthesiology. 2005;102:293–9.
Girgis K, Hamed H, Khater Y, Kacmarek RM. A decremental PEEP trial identifies the PEEP level that maintains oxygenation after lung recruitment. Respir Care. 2006;51:1132–9.
Li M-Q, Han G-J, Li J-Q, Xu J-Y, Shi Z-X, Zhang Z, Lu F, Wang X-M, Xu Y-J, Mo X. Effect of repeated recruitment manoeuvres on patients with severe acute respiratory distress syndrome. West Indian Med J. 2015;64:362–6.
Acknowledgements
The authors thank all patients who participated in the study as well as the contributing medical, nursing, clinical, and research staff.
Funding
This work was not supported financially by any grants from private medical organization or our university.
Author information
Authors and Affiliations
Contributions
All authors take full responsibility for the work described in this article. K.O. and S.D. conceived and conducted the study, analysed the data, and wrote the manuscript. I.E. reviewed, criticised constructively, and revised the manuscript for important intellectual content. K.I. and H.N. helped design the study and contributed to the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declare any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1007/s10877-023-00993-8"
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kudoh, O., Satoh, D., Hori, N. et al. RETRACTED ARTICLE: The effects of a recruitment manoeuvre with positive end-expiratory pressure on lung compliance in patients undergoing robot-assisted laparoscopic radical prostatectomy. J Clin Monit Comput 34, 303–310 (2020). https://doi.org/10.1007/s10877-019-00306-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00306-y