Abstract
Primary immunodeficiency disease (PIDD) comprises a group of disorders of immune function. Some of the most severe PIDD can be treated with hematopoietic cell transplant (HCT). Hizentra® is a 20% liquid IgG product approved for subcutaneous administration in adults and children greater than 2 years of age with PIDD-associated antibody deficiency. Limited information is available on the use of Hizentra® in children following HCT for PIDD. A multicenter retrospective chart review demonstrated 37 infants and children (median age 70.1 [range 12.0 to 176.4] months) with PIDD treated by HCT who received Hizentra® infusions over a median duration of 31 (range 4–96) months post-transplant. The most common indication for HCT was IL2RG SCID (n = 16). Thirty-two patients switched from IVIG to SCIG administration, due to one or more of the following reasons: patient/caregiver (n = 17) or physician (n = 12) preference, discontinuation of central venous catheter (n = 16), desire for home infusion (n = 12), improved IgG serum levels following lower levels on IVIG (n = 10), and loss of venous access (n = 8). Serious bacterial infections occurred at a rate of 0.041 per patient-year while on therapy. Weight percentile increased by a mean of 16% during the observation period, with females demonstrating the largest gains. Mild local reactions were observed in 24%; 76% had no local reactions. One serious adverse event (death from sepsis) was reported. Hizentra® was discontinued in 15 (41%) patients, most commonly due to recovery of B cell function (n = 11). These data demonstrate that Hizentra® is a safe and effective option in children who have received HCT for PIDD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary immunodeficiency diseases (PIDD), also known as inborn errors of immunity, are a group of disorders that result in an increased susceptibility to infections, autoinflammatory disease, and cancer [1,2,3,4,5]. Immunoglobulin G (IgG) replacement therapy is indicated for the treatment of patients with PIDD associated with defects in the ability to produce normal quantity and quality of endogenous immunoglobulin. Intravenously-administered IgG (IVIG) is commonly administered every 3–4 weeks but is associated with systemic side effects in up to 15% of infusions, relies on venous access, and must be administered by a healthcare provider [6,7,8,9,10,11]. Subcutaneously-administered IgG (SCIG) formulations are similarly efficacious to IVIG in prevention of infection, but result in fewer systemic side effects (< 1% of infusions), and can be infused at home [12,13,14,15,16,17,18].
Hematopoietic cell transplant (HCT) remains the treatment of choice for many PIDDs, such as severe combined immunodeficiency (SCID) and hemophagocytic lymphohistiocytosis (HLH). Recommended use of IgG pre and post-HCT has been described [19, 20] and included poor or incomplete immunity due to pre-HCT status or mixed T and/or B cell chimerism [21] and prevention and treatment of infections [22].
Reasons for requiring IVIG in the immediate peri-transplant setting may include the presence of a central venous catheter, frequent clinic follow-up visits necessitating blood draws, and frequent infusions of IV medications and blood products. The role of SCIG in the post-transplant setting is less clear. Limited information on the use of SCIG is available for patients who have received HCT for malignancy [23,24,25,26], or very young pediatric patients with PIDD [27]. The nationwide implementation of newborn screening for SCID, a PIDD treated with HCT, has led to increased identification of newborns with SCID [28]. In these infants, early HCT before 3.5 months of age and prior to development of infection is associated with the best survival. These newborns may benefit from supportive care with SCIG before and also after transplant while awaiting B cell function to recover [29, 30]. Unfortunately, some patients with PIDD do not recover B cell function following HCT, and these patients may also be candidates for longer term post-transplant SCIG [31].
Hizentra® is a 20% liquid SCIG formulation approved for use by adults and children greater than 2 years of age with PIDD [32,33,34] and has also been reported to be safe and effective in children less than 2 years of age [27, 35]. We assessed the safety and efficacy of Hizentra® in pediatric subjects pre- and post-HCT. Because HCT is frequently associated with central venous catheter use, we assessed the reasons for switch from IVIG to SCIG. Neutropenia during the HCT period is a major risk factor for infection including cellulitis [36]. Because subcutaneous administration of immunoglobulin could increase risk of infection due to local trauma, neutrophil counts were evaluated during the HCT period.
Methods
A multicenter retrospective chart review was performed to identify children who received HCT for an underlying PIDD diagnosis and were treated with Hizentra® replacement therapy for supportive care post-transplant. The study was approved by the Institutional Review Board at all participating institutions. Patients were included if they received more than one dose of Hizentra® after HCT (and prior to HCT in some patients), including those on other Ig replacement (IVIG or SCIG) for their initial therapy. A 1:1 conversion factor was used when converting patients receiving IVIG to SCIG. Infusions in patients older than 18 years of age were not examined. Exclusion criteria included patients with protein losing conditions such as lymphangiectasias, nephrosis, or protein losing enteropathies. Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at Carolinas Medical Center [37]. REDCap is a secure, web-based application designed to support data acquisition for research studies. Descriptive statistics only are reported. Primary outcomes including efficacy and safety of treatment were based on rates of serious bacterial infections (SBIs), non-SBIs, and adverse events (AEs). Rates of SBIs and non-SBIs were reported for study subjects prior to receiving Hizentra®. Reported SBIs included bacteremia/sepsis, bacterial meningitis, bacterial pneumonia, osteomyelitis/septic arthritis, and visceral abscesses (liver, lung, and brain) based on pre-defined criteria adjusted to pediatric patients (FDA Guidance for Industry 2008). Information about AEs was collected, including local reactions at the infusion site. Other study assessments included serum IgG levels, volume of infusion, number of infusion sites, duration of infusions, neutrophil counts, and height and weight measurements during treatment period.
Rate of infusions was assessed among patients receiving Hizentra® by pump or manual delivery, and a cut-off value of > 20 mL/h was used for rapid delivery based on previously published studies [16, 38, 39]. Characteristics around HCT, central venous catheter history, and complications post-HCT were collected. Reasons for switch from IVIG to SCIG were determined. Weight and body length, previously shown to be associated with improvement in growth percentiles during SCIG treatment [25], were recorded at the start and end of treatment. Only patients with values at both time points were included. Results were provided for all patients and difference in mean weight, and length percentile was calculated using a t-test.
Results
Study Population
Thirty-seven children with PIDD from 8 centers were available for review. Patient demographics and underlying PIDD diagnoses are shown in Table 1. Thirty-two (86%) were males, and the most common race was white (n = 24 patients, 65%). The most common indications for HCT included SCID (n = 28) in 76% of children, while the remainder (n = 9, 14%) received HCT for various indications including hemophagocytic lymphohistiocytosis, X-linked chronic granulomatous disease, cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) haploinsufficiency, hyperimmunoglobulin M syndrome, signal transducer and activator of transcription 1 (STAT1) gain-of-function (GOF), and 22q11 deletion syndrome.
The median age at transplant was 4 (range 0.5–111) months. The majority of the cohort received either no conditioning (49%) or serotherapy only (8%) prior to HCT. Myeloablative conditioning was used in 11%, while reduced intensity conditioning was administered to 32%. With regard to stem cell source, 62% received bone marrow, 22% received peripheral blood stem cells (PBSC), and 16% children received cord blood (Table 1). Graft versus host disease (GVHD) prophylaxis was used in 22 patients, and pharmacologic immunosuppression included one or more of the following: cyclosporine (n = 13), mycophenolate mofetil (n = 11), tacrolimus (n = 8), cyclophosphamide (n = 6), methotrexate (n = 5), corticosteroid (n = 2), and sirolimus (n = 1). Ten patients received no GVHD prophylaxis, and 5 patients received T cell-depleted donor bone marrow only. Acute GVHD post-HCT included grades 1–2 in 11 (30%) children and grades 3–4 in 7 (19%) children. Chronic GVHD was mild, moderate, or severe in 6, 2, and 1 child(ren), respectively. The most common site was skin in both acute GVHD (grades 1–2, n = 7, grades 3–4, n = 7) and chronic skin GVHD (n = 8) (Table 1). One patient died at 16 months post-transplant from bacterial sepsis.
Infusion Parameters
The median age at the start of Hizentra® was 15 months (range 0.5–114), with median start date post-transplant 11 months (range 0.5–87). Patients were observed from 4 to 96 months while receiving infusions every 7–14 days. Three patients started therapy prior to transplant, and an additional six patients started at ≤ 6 months post-HCT. Five patients naïve to immunoglobulin therapy were started on Hizentra® directly, without prior administration of other immunoglobulin products, including IVIG.
Median cumulative monthly dosage was lower for patients receiving SCIG than IVIG. The median SCIG dose was 776 mg/kg/4 weeks, and the median IgG level available in 34 patients was 871 (range 404–1780) mg/dL). Thirty-two patients received IVIG therapy prior to Hizentra® including a median dose of 807 (mg/kg/4 weeks and median trough IgG level of 696 (range 316–1170) mg/dL. Two patients received SCIG (Vivaglobin®, 16% liquid formulation, CSL Behring) prior to Hizentra®.
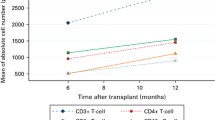
Hizentra® was administered subcutaneously using infusion pumps (n = 31) or manual delivery (n = 6). A total of 4107 infusions were administered. The median number of infusions per patient was 111 (range 8–316). Premedication prior to SCIG infusion was utilized in only 1 patient (lidocaine cream). Sites of administration included thigh (62%), thigh and abdomen (14%), buttocks (14%), abdomen (8%), and thigh and arm (2%). The median total treatment volume per patient was 10.4 mL (range 5–45), while median volume per site for all patients was 6.1 mL (range 2.5–22.5 mL). Manual delivery was most often accomplished using a 23-, 25-, or 27-gauge butterfly needle set, and the media volume per site was 3.1 mL (range 1.5–5 mL). Needle length was reported in 18 patients, and the most frequently used size was 6 mm (72%), followed by 4 mm (17%) and 9 mm (11%). In all patients, therapy was administered at home after instruction was completed. A parent or caregiver administered the infusions in 78% patients. The remaining 22% patients received administration by a home care or clinic infusion nurse. Median SCIG infusion time was 67.1 min (range 10–240) for pump entry and 5.2 min (range 3–10) for manual entry, and the average number of infusion sites was 1.7 (range 1 to 2). The median rate (mL/h) was 20.0 (range 5–135) for pump entry and 120 (range 100–200) for manual entry. Rapid infusion (> 20 mL/h) was achieved by 100% of patients in the manual entry group and in 6% of patients in the pump-administered group, with similar infusion volumes in both groups. Calculated infusion rates were 11.3 mL/h/site (range 0.63–67.5) for pump entry and 90 mL/h/site (range 50–200) for manual entry. Serum IgG levels were higher for patients receiving Hizentra® (871 [range 404–1780] mg/dL among 34 patients) compared to those who received IVIG or other SCIG prior to Hizentra® (696 [316–1170] mg/dL in 36 patients), likely related to higher steady-state level related to increased frequency of SCIG compared to IVIG dosing.
Efficacy and Tolerability
Infections including SBIs and non-SBIs during IVIG or Hizentra® are shown in Table 2. On therapy, SBIs included sepsis/bacteremia (n = 2) and pneumonia (n = 3); the incidence of SBIs was 0.041 infections per patient-year. Non-SBIs during the same time period included cellulitis in three patients (central venous catheter site [n = 2], gastrostomy tube site [n = 1]), central line-associated blood stream infection in two patients, parainfluenza bronchiolitis in two patients, and one patient each with cytomegalovirus viremia, Enterobacter gastroenteritis, Clostridium difficile gastroenteritis, or fever without a source. The incidence of non-SBIs was 0.082 infections per patient-year. In 32 patients who received IVIG prior to starting Hizentra®, the incidence of SBIs and non-SBIs were 0.247 and 0.71 infections per patient-year, respectively.
The median absolute neutrophil count (ANC) prior to transplant in 35 patients was 4214 (range 0–12,410) cells/µL. The median duration of neutropenia, defined as ANC < 1.5 × 103 cells/µL after HCT, was 7.25 months (range 0.25–36) with neutropenia lasting < 6 months (n = 16), ≥ 6–12 months (n = 9), and ≥ 12 months (n = 10). Two patients did not experience any neutropenia after HCT. Nine patients were neutropenic over the course of administration of Hizentra®, having a median ANC 918 (range 71–1,480) cells/µL, lasting up to 37 months after initiation. There were no episodes of cellulitis associated with infusion sites during this period, although concurrent administration of antibiotic prophylaxis was not examined. While platelet counts were not assessed, bleeding was not reported as a complication of SCIG therapy.
Most (76%) patients experienced no local AEs (Table 3). Local reactions were mostly mild and observed in 9 (24%) children. Excluding local reactions, other AEs included one patient each with pyrexia, headache, rash, or diarrhea. In patients with acute GVHD of the skin (grades 1–2, n = 7; grades 3–4, n = 7) and chronic skin GVHD (n = 8), no adverse events were associated with SCIG treatment. One SAE (death) occurred in a patient with sepsis who at the time of death had no indwelling catheter, was not neutropenic, normal mitogen studies, and had the following donor chimerism: T cells (99%), B cells (2%), and myeloid (2%).
Growth Parameters
Weight and length percentiles were assessed at the beginning and end of the treatment observation period. There was an increase in overall weight percentile with a mean increase of 16% [range 1–99%] from 36 to 52% over the observation period (mean 31 months). Females (n = 5) showed a trend towards higher increase in weight percentile with a mean of 35% [range − 41–89%] from 52% at start to 87% at end compared to males (n = 32) with a mean of 13% [range − 49–97%] from 33% at start to 47% at end (p = 0.18). Length parameters for 37 patients were unchanged for both males and females, with a median of 26% [range 1–96%], both at the start and end of the observation period.
Switch from IVIG to SCIG
For 32 patients who were on other Ig therapy initially, the indications for switching to Hizentra® are described in Table 4; multiple indications were reported for some patients. These include patient/caregiver (n = 17) or physician (n = 12) preference, discontinuation of central venous catheter (n = 16), desire for home infusion (n = 12), improved IgG serum levels following IVIG (n = 10), and loss of venous access (n = 8), and less common reasons included desire for caregiver administration (n = 3), adverse events from IVIG (n = 2), repeated central line infection (n = 1), and missed days of school (n = 1). Hizentra® was discontinued in 15 (41%) patients due to recovery of B cell function (n = 11). The average duration of therapy in these patients was 14.4 months [range 4–37]. Other reasons for discontinuation included switch to IVIG related to replacement (following a prior discontinuation) of central venous catheter (n = 2), behavioral complaints during SCIG (n = 1), and death related to sepsis (n = 1). Twenty-two (59%) children remained on Hizentra® due to continued need for replacement therapy related to ongoing B cell dysfunction.
Discussion
This report is the largest to evaluate the safety and efficacy of SCIG (Hizentra®) in 37 children with PIDD who underwent HCT. On therapy, the study population had an annualized rate of SBIs of 0.041 per patient-year compared to 0.247 per patient-year in 32 patients receiving IVIG prior to the observation period. This rate is similar to those observed in older children and adults on SCIG for PIDD [32,33,34, 40,41,42]. Infections occurring shortly after the initiation of IVIG therapy prior to obtaining steady-state IgG levels may have contributed to a higher rate of SBIs during this period, with sepsis/bacteremia responsible for the majority of infections. While the median age at transplant was 4 months, the median start date of Hizentra® was not until 15 months, and patients may have benefitted from being more clinically stable at this stage post-HCT, accounting for differences in SBI rates between IVIG and SCIG. Other factors that may have contributed to differences in SBI rates outside of immunoglobulin administration include differences in immunosuppressive medications, engraftment of T cells, and presence of indwelling catheters associated with risk of central line-associated blood stream infections. Local reactions occurred in 9/37 (24%) children and were mild and transient. This is similar to previously published studies on SCIG management and PIDD which report an overall incidence of adverse events of 7–96% [17, 32, 34, 42,43,44].
Neutropenia is a major risk factor for infection, including cellulitis, during the pre-engraftment period immediately following HCT [36]. Cellulitis is also a well-known complication from central venous catheter placement, particularly in the same pre-engraftment period [45,46,47]. Subcutaneous administration of medications during neutropenic periods could increase the risk for cellulitis related to local skin trauma following needle administration [48,49,50]. In this cohort, there were no episodes of cellulitis, in particular none during periods of neutropenia. Severe GVHD may hamper use of SCIG, as infusions in stiff, noncompliant tissues may not be possible or painful [50, 51]. In our cohort, no adverse events were associated with SCIG treatment in patients with acute GVHD of the skin. This suggests that in patients with mild forms of either cutaneous acute or chronic skin GVHD, SCIG may be well tolerated.
The median duration of IVIG prior to switch to Hizentra® was 10 (range 1–86) months. Among these 32 patients, 9 patients were on IVIG for 3 months or fewer prior to switch. Among the reasons for switch from IVIG to Hizentra®, preference for switch by the patient/caregiver and transition of infusions to a home setting were the most common reasons given. Indeed, it has been reported that families of children who underwent HCT favored infusion at home due to reduced need for clinic visits and increased participation in their child’s treatment [24]. In one study, patient satisfaction scores were higher with SCIG compared to IVIG in adults who underwent HCT [25], similar to published reports on SCIG and patient satisfaction/quality of life in PIDD children and adults [52,53,54,55]. In our cohort, there were no treatment discontinuations among SCIG patients, possibly related to low rate of adverse events and higher overall satisfaction with SCIG. Twenty-two (59%) children remained on long-term Hizentra® immunoglobulin replacement post-HCT due to ongoing B cell dysfunction, including 13 (59%) patients who received no conditioning, 8 (36%) patients who received reduced intensity conditioning, and 1 (5%) patient who received myeloablative conditioning.
Weight percentile increased by a mean of 16% during the observation period (average 31 months), with females demonstrating the largest gains (mean 35%). Similar observations have been reported in young children during catch-up growth after a period of high infectious disease burden or inadequate dietary intake [56,57,58,59,60], as well as a smaller cohort of HCT children published by our group [27]. There was no difference in length percentile in either male or female patients. Previous observations suggest stunted growth in children requires recovery in weight before resuming linear growth [56, 57, 60]. Perhaps a longer observation period in the current study would have seen differences in gains in length percentiles. Conversely, complications related to pre- and post-transplant infections and post-transplant complications such as GVHD may have adversely affected growth velocity [61], although observed differences may have been limited due to small sample size. Data from this study support the observation that poor growth seen among HCT patients, most likely related to prior frequent and severe infections and transplant complications, can possibly be reversed with optimal immunoglobulin replacement although other factors including genetics may play a role.
This study was limited by the number of study participants, duration of follow-up, and the retrospective nature of the study. The dosages used for both IVIG and SCIG were higher than normal in some patients, which was left up to the discretion of each investigator but could have been related to the clinical condition of the patient, initial loading dose, low IgG trough levels, or other factors. Conclusions were unable to be drawn regarding outcomes related to specific types of PIDD, conditioning regimens, cell sources, and GVHD prophylaxis due to the small study group. Growth changes observed in this study was limited by lack of a comparison cohort. Findings including low rate of local adverse reactions and improved growth parameter need to be confirmed with prospective studies including larger sample sizes and longer observation periods.
Hizentra® appears effective in preventing infections in children receiving HCT and was well tolerated for periods up to 96 months. These data support use of this therapy in pediatric patients with inborn errors of immunity even in the post-transplant period.
Data Availability
All data supporting the findings of this study are available within the paper.
References
Buckley RH. Primary immunodeficiency diseases due to defects in lymphocytes. N Engl J Med. 2000;343:1313–24.
Chapel H, Geha R, Rosen F. Primary immunodeficiency diseases: an update. Clin Exp Immunol. 2003;132:9–15.
Ochs HD, Smith CIE, Puck JM. Primary immunodeficiency diseases: a molecular and genetic approach. 3rd ed. New York: Oxford University Press Inc, USA; 2014.
Al-Herz W, Bousfiha A, Casanova JL, Chatila T, Conley ME, Cunningham-Rundles C, et al. Primary immunodeficiency diseases: an update on the classification from the international union of immunological societies expert committee for primary immunodeficiency. Front Immunol. 2014;5:162.
Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol. 1999;92:34–48.
Roifman CM. Intravenous immunoglobulin treatment of immunodeficiency. Preface Immunol Allergy Clin North Am. 2008;28(4):xv–xvi. https://doi.org/10.1016/j.iac.2008.08.002.
Quartier P, Debre M, De Blic J, de Sauvarzac R, Sayegh N, Jabado N, et al. Early and prolonged intravenous immunoglobulin replacement therapy in childhood agammaglobulinemia: a retrospective survey of 31 patients. J Pediatr. 1999;134:589–96.
Busse PJ, Razvi S, Cunningham-Rundles C. Efficacy of intravenous immunoglobulin in the prevention of pneumonia in patients with common variable immunodeficiency. J Allergy Clin Immunol. 2002;109:1001–4.
Church JA, Borte M, Taki H, Nelson RP, Sleasman JW, Knutsen AP, et al. Efficacy and safety of privigen in children and adolescents with primary immunodeficiency. Pediatr Asthma Allergy Immunol. 2009;22:53–62.
Eijkhout HW, van der Meer JW, Kallenberg CG, Weening RS, van Dissel JT, Sanders LA, et al. The effect of two different dosages of intravenous immunoglobulin on the incidence of recurrent infections in patients with primary hypogammaglobulinemia. A randomized, double-blind, multicenter crossover trial. Ann Intern Med. 2001;135:165–74.
Stein MR, Nelson RP, Church JA, Wasserman RL, Borte M, Vermyle C, et al. Safety and efficacy of Privigen®, a novel 10 % liquid immunoglobulin preparation for intravenous use, in patients with primary immunodeficiencies. J Clin Immunol. 2009;29:137–44.
Skoda-Smith S, Torgerson TR, Ochs HD. Subcutaneous immunoglobulin replacement therapy in the treatment of patients with primary immunodeficiency disease. Ther Clin Risk Manag. 2010;6:1–10. https://doi.org/10.1057/rm.2009.17.
Gustafson R, Gardulf A, Hansen S, Leibl H, Engl W, Lindén M, et al. Rapid subcutaneous immunoglobulin administration every second week results in high and stable serum immunoglobulin G levels in patients with primary antibody deficiencies. Clin Exp Immunol. 2008;152(2):274–9. https://doi.org/10.1111/j.1365-2249.2008.03620.x.
Abrahamsen TG, Sandersen H, Bustness A. Home therapy with subcutaneous immunoglobulin infusions in children with congenital immunodeficiencies. Pediatrics. 1996;98:1127–31.
Berger M. Principles of and advances in immunoglobulin replacement therapy for primary immunodeficiency. Immunol Allergy Clin N Am. 2008;28:413–37.
Gardulf A, Nicolay U, Asensio O, Bernatowska E, Bock A, Carvalho BC, et al. Rapid subcutaneous IgG replacement therapy is effective and safe in children and adults with primary immunodeficiencies – a prospective, multi-national study. J Clin Immunol. 2006;26:177–85.
Ochs HD, Gupta S, Kiessling P, Nicolay U, Berger M. Safety and efficacy of self-administered subcutaneous immunoglobulin in patients with primary immunodeficiency diseases. J Clin Immunol. 2006;26:265–73.
Berger M. Subcutaneous administration of IgG. Immunol Allergy Clin N Am. 2008;28:413–37.
Heimall J, Buckley RH, Puck J, Fleisher TA, Gennery AR, Haddad E, et al. Recommendations for screening and management of late effects in patients with severe combined immunodeficiency after allogenic hematopoietic cell transplantation: a consensus statement from the second pediatric blood and marrow transplant consortium international conference on late effects after pediatric HCT. Biol Blood Marrow Transplant. 2017;23(8):1229–40.
Otani IM, Lehman HK, Jongco AM, Tsao LR, Azar AE, Tarrant TK, Engel E Walter JE, Truong TQ, Khan DA, Ballow M, Cunningham-Rundles C, Lu H, Kwan M, Barmettler S. Practical guidance for the diagnosis and management of secondary hypogammaglobulinemia: a work group report of the AAAAI primary immunodeficiency and altered immune response committees. J Allergy Clin Immunol. 2022;149(5):1525–1560.
Haddad E, Leroy S, Buckley RH. B-cell reconstitution for SCID: should a conditioning regimen be used in SCID treatment? J Allergy and Clin Immunol. 2013;131(4):994–1000.
Krause I, Wu R, ShererPatanik YM, Peter JB, Shoenfeld Y. In vitro antiviral and antibacterial activity of commercial intravenous immunoglobulin preparations – a potential role for adjuvant intravenous immunoglobulin therapy in infectious diseases. Transfus Med. 2002;12(2):133–9.
Sundin M, Nordin K, Jostemyr Y, Winiarski J. Subcutaneous IgG replacement after pediatric SCT. Pediatr Transplantation. 2012;16:866–71.
Pasic I, Alanazia W, Dranitsarisb G, Liebermanc L, Viswabandyaa A, Kima D, et al. Subcutaneous immunoglobulin in allogeneic hematopoietic cell transplant patients: a prospective study of feasibility, safety, and healthcare resource use. Hematol Oncol Stem Cell Ther. 2021;14(4):302–10. https://doi.org/10.1016/j.hemonc.2021.01.001.
Karakulska-Prystupiuk E, Dwilewicz-Trojaczek J, Drozd-Sokołowska J, Kmin E, Chlebus M, Szczypińska K, et al. Prevalence of hypogammaglobulinemia and its management with subcutaneous immunoglobulin supplementation in patients after allogeneic hematopoietic stem cell transplantation-a single-center analysis. Ann Hematol. 2021;100(12):3007–16. https://doi.org/10.1007/s00277-021-04649-y.
Font S, López-Granados L, Sisinni L, Berna J, Martínez L, Gamarra-Martínez E, et al. Chronic hypogammaglobulinemia after allogeneic stem cell transplantation and their treatment with subcutaneous immunoglobulin in pediatric patients. An Pediatr (Engl Ed). 2022;97(2):103–11. https://doi.org/10.1016/j.anpede.2021.08.010.
Patel NC, Gallagher JL, Ochs HD, Atkinson TP, Wahlstrom J, Dorsey M, et al. Subcutaneous immunoglobulin replacement therapy with Hizentra® is safe and effective in children less than 5 years of age. J Clin Immunol. 2015;35(6):558–65.
Kwan A, Abraham RS, Currier R, Brower A, Andruszewski K, Abbott JK, et al. Newborn screening for severe combined immunodeficiency in 11 screening programs in the United States. JAMA. 2014;312:729–38.
Baker MW, Grossman WJ, Laessig RH, Hoffman GL, Brokopp CD, Kurtycz DF, et al. Development of a routine newborn screening protocol for severe combined immunodeficiency. J Allergy Clin Immunol. 2009;124:522–7.
Dorsey M, Wright NA, Chaimowitz S, Saldaña BJ, Miller H, Keller MD, et al. Infections in infants with SCID: isolation, infection screening, and prophylaxis in PIDTC centers. J Clin Immunol. 2021;41(1):38–50.
Hardin O, Lokhnygina Y, Buckley RH. Long-term clinical outcomes of severe combined immunodeficiency patients given nonablative marrow transplants. J Allergy Clin Immunol Pract. 2022;10(4):1077–83.
Hagan JB, Fasano MB, Spector S, Wasserman RL, Melamed I, Rojavin MA, et al. Efficacy and safety of a new 20% immunoglobulin preparation for subcutaneous administration, IgPro20, in patients with primary immunodeficiency. J Clin Immunol. 2010;30:734–45.
Jolles S, Bernatowska E, de Gracia J, Borte M, Cristea V, Peter HH, et al. Efficacy and safety of Hizentra® in patients with primary immunodeficiency after a dose-equivalent switch from intravenous or subcutaneous replacement therapy. Clin Immunol. 2011;141:102–14.
Borte M, Pac M, Serban M, Gonzalez-Quevedo T, Grimbacher B, Jolles S, et al. Efficacy and safety of 20% SCIg, a new 20% immunoglobulin preparation for subcutaneous administration, in pediatric patients with primary immunodeficiency. J Clin Immunol. 2011;31:752–61.
Gallagher J, Patel NC. Subcutaneous immunoglobulin replacement therapy with Hizentra® is safe and effective in two infants. J Clin Immunol. 2012;32(3):474–6. https://doi.org/10.1007/s10875-011-9645-0.
Wingard JR, Hsu J, Hiemenz JW. Hematopoietic stem cell transplantation: an overview of infection risks and epidemiology. Infect Dis Clin North Am. 2010;24(2):257.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Shapiro R. Subcutaneous immunoglobulin: rapid push vs. infusion pump in pediatrics. Pediatr Allergy Immunol. 2013;24:49–53.
Thomas MJ, Brennan VM, Chapel HH. Rapid subcutaneous immunoglobulin infusions in children. Lancet. 1993;342:1432–3.
Wasserman RL, Melamed I, Nelson RP, Knutsen AP, Fasano MB, Stein MR, et al. Pharmacokinetics of subcutaneous IgPro20 in patients with primary immunodeficiency. Clin Pharmacokinetics. 2011;50:405–14.
Kanegane H, Imai K, Yamada M, Takada H, Ariga T, Bexon M, et al. Efficacy and safety of IgPro20, a subcutaneous immunoglobulin, in Japanese patients with primary immunodeficiency diseases. J Clin Immunol. 2014;34:204–11.
Borte M, Quinti I, Soresina A, Fernandez-Cruz E, Ritchie B, Schmidt DS, et al. Efficacy and safety of subcutaneous Vivaglobin® replacement therapy in previously untreated patients with primary immunodeficiency: a prospective, multicenter study. J Clin Immunol. 2011;31:952–61.
Abolhassani H, Sadaghiani MS, Aghamohammadi A, Ochs HD, Rezaei N. Home-based subcutaneous immunoglobulin versus hospital-based intravenous immunoglobulin in treatment of primary antibody deficiencies: systematic review and meta-analysis. J Clin Immunol. 2012;32:1180–92.
Jolles S, Rojavin MA, Lawo J-P, Melson R, Wasserman RL, Borte M, et al. Long-term efficacy and safety of Hizentra® in patients with primary immunodeficiency in Japan, Europe, and the United States: a review of 7 phase 3 trials. J Clin Immunol. 2018;38:864–75.
Shulman RJ, Smith EO, Rahman S, Gardner P, Reed T, Mahoney D. Single- vs double-lumen central venous catheters in pediatric oncology patients. Am J Dis Child. 1988;142(8):893–5.
Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81(9):1159.
Schmidli J, Widmer MK, Basile C, de Donato G, Gallieni M, Gibbons CP, et al. Vascular access: 2018 clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2018;55(6):757.
Halperin S, Kohl KS, Gidudu J, Ball L, Hammer SJ, Heath P, et al. Cellulitis at injection site: case definition and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine. 2007;25(31):5803–20.
Bailey E, Kroshinsky D. Cellulitis: diagnosis and management. Dermatol Ther. 2011;24(2):229–39.
Patel K, Parmar S, Shah S, Shore T, Gergis U, Mayer S, et al. Comparison of subcutaneous versus intravenous alemtuzumab for graft-versus-host disease prophylaxis with fludarabine/melphalan-based conditioning in matched unrelated donor allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22(3):456–61.
Ramachandran V, Kolli SS, Strowd LC. Review of graft-versus-host disease. Dermatol Clin. 2019;37(4):569–82.
Gardulf A, Nicolay U, Asensio O, Bernatowska E, Bock A, Costa-Carvalho BT, et al. Children and adults with primary antibody deficiencies gain quality of life by subcutaneous IgG self-infusions at home. J Allergy Clin Immunol. 2004;114:936–42.
Nicolay U, Kiessling P, Berger M, Gupta S, Yel L, Roifman CM, et al. Health-related quality of life and treatment satisfaction in North American patients with primary immunodeficiency diseases receiving subcutaneous IgG self-infusions at home. J Clin Immunol. 2006;26:65–72.
Mallick R, Jolles S, Kanegane H, Agbor-Tarh D, Rojavin M. Treatment satisfaction with subcutaneous immunoglobulin replacement therapy in patients with primary immunodeficiency: a pooled analysis of six Hizentra® studies. J Clin Immunol. 2018;38:886–97.
Anterasian C, Duong R, Gruenemeier P, Ernst C, Kitsen J, Geng B. Quality of life differences for primary immunodeficiency patients on home SCIG versus IVIG. J Clin Immunol. 2019;39:814–22.
Checkley W, Epstein LD, Gilman RH, Black RE, Cabrera L, Sterling CR. Effects of Cryptosporidium parvum infection in Peruvian children: growth faltering and subsequent catch-up growth. Am J Epidemiol. 1998;148:497–506.
Kabir I. Malek Ma, Mazumder RN, Rahman MM, Mahalanabis D. Rapid catch-up growth of children fed a high-protein diet during convalescence from shigellosis. Am J Clin Nutr. 1993;57:441–5.
Richard SA, Black RE, Checkley W. Revisiting the relationship of weight and height in early childhood. Adv Nutr. 2012;3:250–4.
Golden MH. Is complete catch-up possible for stunted malnourished Children? Eur J Clin Nutr. 1994;48:S58-70.
Ashworth A. Growth rates in children recovering from protein-calorie malnutrition. Br J Nutr. 1969;23:835–45.
Myers KC, Howell JC, Wallace G, Dandoy C, El-Bietar J, Lane A, et al. Poor growth, thyroid dysfunction and vitamin D deficiency remain prevalent despite reduced intensity chemotherapy for hematopoietic stem cell transplantation in children and young adults. Bone Marrow Transplant. 2016;51(7):980–4.
Acknowledgements
DM contributed to statistics. We thank the patients and families who contributed to this study.
Funding
This work was supported through an Investigator Initiated Research grant awarded to Niraj Patel, funding by CSL Behring LLC, King of Prussia, PA, USA, and conducted at Atrium Health in Charlotte, NC, USA, while Dr. Patel was affiliated with Atrium Health.
Author information
Authors and Affiliations
Contributions
NCP wrote the drafts of the manuscript, prepared the tables, and revised the original manuscripts for resubmission. All co-authors contributed to and edited drafts of the original and revised manuscripts and tables and approved the final submitted version.
Corresponding author
Ethics declarations
Ethics Approval
This is a retrospective review study. The Atrium Health Research Ethics Committee has confirmed that no ethical approval is required.
Consent to Participate
Informed consent was obtained from all individual participants in this study.
Consent to Publish
Not applicable.
Competing Interests
NCP receives honoraria for Speaker’s Bureau and research funding from CSL Behring and Takeda and honoraria for Speaker’s Bureau from Horizon Therapeutics. JH receives research funding from CSL Behring and ADMA Biologics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patel, N.C., Torgerson, T., Thakar, M.S. et al. Safety and Efficacy of Hizentra® Following Pediatric Hematopoietic Cell Transplant for Treatment of Primary Immunodeficiencies. J Clin Immunol 43, 1557–1565 (2023). https://doi.org/10.1007/s10875-023-01482-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-023-01482-y