Abstract
Purpose
We aimed to report the clinical and immunological characteristics of variant type X91+ chronic granulomatous disease (CGD) in a Chinese cohort.
Methods
The clinical manifestations and immunological phenotypes of patients with X91+ CGD were collected. A dihydrorhodamine (DHR) analysis was performed to evaluate neutrophil function. Gp91phox protein expression was determined using extracellular staining with the monoclonal antibody (mAb) 7D5 and flow cytometry.
Results
Patients with X91+ CGD accounted for 8% (7/85) of all patients with CGD. The median age of onset in the seven patients with X91+ CGD was 4 months. Six patients received the BCG vaccine, and 50% (3/6) had probable BCG infections. Mycobacterium tuberculosis infection was prominent. The most common sites of infection were the lung (6/7), lymph nodes (5/7), and soft tissue (3/7). Two patients experienced recurrent oral ulcers. The stimulation index (SI) of the patients with X91+ CGD ranged widely from 1.9 to 67.3. The difference in the SI among the three groups of patients (X91+ CGD, X91− CGD, and X910 CGD) was statistically significant (P = 0.0071). The three groups showed no significant differences in onset age, diagnosis age, or severe infection frequency. CYBB mutations associated with X91+ CGD were commonly located in the second transmembrane or intracellular regions. Three novel X91+ CGD–related mutations (c.1462–2 A > T, c.1243C > T, and c.925G > A) were identified.
Conclusions
Variant type X91+ CGD may result in varied clinical manifestations. Moreover, the laboratory findings might indicate a moderate neutrophil SI. We should deepen our understanding of variant X91+ CGD to prevent missed diagnoses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic granulomatous disease (CGD) is a rare inherited primary immunodeficiency (PID) with an incidence of 1 case per 200,000 to 250,000 live births worldwide [1]. The pathogenesis of CGD is characterized by dysfunctional nicotinamide adenine dinucleotide phosphate (NADPH) oxidase and decreased or no superoxide anion (O2−) production, resulting in significantly reduced bactericidal activities of neutrophils and other phagocytes. The clinical patterns of patients with CGD generally include early-onset recurrent bacterial, tuberculous, or fungal infection, especially with catalase-positive microbes, involving the lung, lymph nodes, liver, and bone [2]. The respiratory burst of neutrophils has been previously detected using the nitroblue tetrazolium (NBT) test and is currently detected with the dihydrorhodamine-1,2,3 (DHR) test in clinical practice. The respiratory burst of neutrophils is defective in patients with CGD.
NADPH oxidase is a complex composed of membrane-bound gp91phox and p22phox and cytosolic p47phox, p67phox, and p40phox. Gp91phox and p22phox together form the heterodimer cytochrome b558. Gp91phox is the enzymatic core of the NADPH oxidase complex, while other components play a regulatory role in the NADPH oxidase complex. The gp91phox protein is encoded by the cytochrome b-245 β chain (CYBB) gene mapped to chromosome Xp21.1-p11.4, and its mutation results in X-linked CGD, accounting for 70% of CGD cases overseas and approximately 85% of cases in China [1, 3]. Most patients with X-linked CGD neither produce superoxide nor express gp91phox, and this type of CGD is named classic type X-linked CGD (X910 CGD). However, some patients with CYBB mutations have low expression levels of functional or partially functional gp91phox (X91− CGD) or normal expression levels of nonfunctional or partially functional gp91phox (X91+ CGD) [1, 4]. X91− CGD and X91+ CGD caused by CYBB mutations are named variant type X-linked CGD. The characteristics of variant type X-linked CGD, especially X91+ CGD, differ from classical CGD, which may interfere with the rapid diagnosis of X-linked CGD using the stimulation index (SI) of DHR and the expression of the gp91 protein.
However, few patients with X91+ CGD have been reported to date. In this study, we report the clinical and immunological characteristics of seven Chinese patients with X91+ CGD, focus on the relationship with SI, and review the literature to further document the rare CYBB gene mutations resulting in variant type X-linked CGD.
Methods
This study was approved by the Ethics Committee of Children’s Hospital of Fudan University. Written informed consent was obtained from the parents of all patients.
Patients and Clinical Data
Children with CGD who were admitted to our hospital between January 2018 and March 2021 were enrolled in this study. CGD was diagnosed according to the clinical manifestations, laboratory findings, and genetic data. The relevant data are summarized in detail in Table 1. Previous studies of patients with variant type X91+ CGD and mutations reported in PubMed from 1987 to November 2021 were reviewed.
Definition of Terms
The age of the last follow-up was defined as the pretransplant visit for transplant patients, and November 2021 or death for nontransplant patients. Severe infection events were defined as infections requiring hospitalization for systemic anti-infective therapy or surgical treatment. The frequency of severe infection events per patient-year refers to the total number of severe infection events/the duration of the effective observation years. Sites of infections were described according to the clinical manifestations: lung, lymph node, perianal, gastrointestinal tract, bone, bloodstream, skin and soft tissue, liver, spleen, abdominal (abdominal abscess and peritonitis), central nervous system, and urinary tract. Noninfectious complications included oral ulcers, elevated levels of liver enzymes, ulcerative colitis, and anemia. The diagnostic criterion for BCG disease was described in a previous publication [2]. Mycobacterium tuberculosis infection was considered based on pulmonary and lymph node infection characteristics, a positive PPD test, T-SPOT assay, and effectiveness of anti-tuberculosis treatment. Here, we defined the calculation of M. tuberculosis infection as the total number of patients receiving anti-tuberculosis treatment and those with BCG disease. PPD positivity was defined as an induration diameter > 5 mm after 48–72 h. Fungal infection was defined as a positive galactomannan (GM) test or the isolation of a fungus from samples. Bacterial infection was defined as detecting pathogenic bacteria using cultures or metagenomics next-generation sequencing (mNGS).
Routine Immune Function Evaluation
Routine blood counts and immunological functional analyses were performed. We used the nephelometry method to detect immunoglobulins, including IgG, IgA, and IgM, as previously reported, and lymphocyte subsets were measured using flow cytometry (Becton Dickinson, Franklin Lakes, NJ, USA).
Evaluation of Neutrophil Function
A DHR analysis was performed to measure the respiratory burst of neutrophils by assessing reactive oxygen species (ROS). Blood was collected and treated with the anticoagulant heparin sodium. Samples were stimulated with 0.01 mg/ml phorbol-12-myristate-14-acetate (PMA) for 15 min and then incubated with dihydrorhodamine-1,2,3 (0.03 mg/ml) for 5 min, followed by red blood cell lysis and PBS washes [2]. The flow cytometry analysis was performed as previously described using a FACSCanto II flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA) [5]. Since we purchased a new flow cytometer in January 2021, the channel template set was AF488 from January 2008 to December 2020, and the channel template set changed to FITC from January 2021. The stimulation index (SI), which is defined as the geometric fluorescence intensity of PMA-stimulated neutrophils relative to the geometric fluorescence intensity of unstimulated neutrophils, was calculated to evaluate neutrophil function [6]. The SI was detected by monitoring the FITC channel in only one patient with X-linked CGD (P4).
Expression of the gp91phox Protein
The expression of the gp91phox protein was determined using extracellular staining with the monoclonal antibody (mAb) 7D5, which detects flavocytochrome b558 in the NADPH oxidase complex at the cell surface, and flow cytometry. Peripheral blood samples were added to two tubes. FITC anti-flavocytochrome b558 (MBL) or an isotype-matched control antibody (BD Biosciences) was added to the reaction system and incubated for 15 min for staining, followed by red blood cell lysis and PBS washes. The expression of gp91phox protein on peripheral blood neutrophils was analyzed using a FACSCanto II flow cytometer. Each time we performed the experiment, we included a sample from a healthy control in the same batch. The gp91phox protein was detected using the FITC channel in three patients, including one with X910 and two with X91+ (P1 and P4).
Gene Analysis
Genomic DNA was extracted from the EDTA-anticoagulated blood of patients and their parents using the QIAmp® DNA Blood Mini Kit (Qiagen, Hilden, Germany). The concentration and quantity of the DNA samples were measured using a NanoDrop ultraviolet spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA) and then prepared for next-generation sequencing by a panel including all previously reported immunodeficiency genes.
In accordance with the instructions of the SureSelect Human All Exon Kit, the genomic DNA underwent ultrasonic fragmentation, end repair, adapter connection, and hybridization. The captured DNA library was sequenced on the Illumina HiSeq 2000 platform (Illumina, San Diego, CA). The raw data were converted to a VCF file containing the basic information for the mutation sites through splicing and comparison. We completed the variation annotation using ANNOVAR and VEP software. The annotation of the mutation frequency referred to databases, including the 1000 Genomes Project, the ExAC Browser, and internal databases. Mutations were predicted using SIFT, PolyPhen-2, and MutationTaster software. Deletions were identified by performing an NGS coverage depth analysis [7], and point mutations were confirmed by Sanger sequencing. The minimum allele frequency (MAF) was searched in the Gnomad database.
Statistical Analysis
Data were analyzed using STATA 15.0 software. Categorical variables were displayed as numbers and percentiles. We used the Kruskal–Wallis rank sum test to analyze the differences among the three groups (X91+, X91−, and X910 CGD). The specific source of the significant differences was then determined by a two-by-two comparison between the two groups. The tests were Bonferroni corrected. Pearson correlation analysis was used to assess the correlation between the two quantitative variables. P values < 0.05 were considered statistically significant.
Results
X-linked CGD Distribution
Between January 2018 and March 2021, a total of 85 patients with CGD were admitted to the Children’s Hospital of Fudan University. Patients were diagnosed with CGD according to their clinical manifestations, immune phenotype, and genetic results. The most common mutation in the CYBB gene inherited from the X chromosome was detected in 68 patients (80%). Autosomal recessive CGD (AR-CGD) was detected in a minority of the patients and was attributed to CYBA mutations (7%), NCF1 mutations (7%), and NCF2 mutations (6%) (Fig. 1A).
Based on the expression level of the gp91 protein, we further classified patients with X-linked CGD carrying CYBB mutations into X910, X91−, and X91+ CGD. In comparisons to both healthy controls and other primary immunodeficiencies (PIDs) including NCF1/NCF2 mutant CGD, we defined the gp91 expression level in patients with X91+ as > 70%, X91− as 5–70%, and X910 as < 5%. X91+ CGD accounted for 8% (7/85) of all CGD patients (Fig. 2A).
Comparison of GP91 protein expression and stimulation index in patients with X-linked CGD. A GP91 protein expression levels in different groups, including X91+, X91−, X910, CGD with NCF1/NCF2, other PIDs, and healthy adults. B SI in different groups of patients with X-linked CGD and healthy adults. **A statistically significant difference was observed among the three groups (X91+, X91−, and X910 CGD) (P = 0.0071). Further analysis showed that the SI of X91+ CGD was statistically higher than that of X910 CGD (P = 0.002). C Correlation analysis between SI and GP91 protein expression (P < 0.001). D Correlation analysis between SI and age of onset (P = 0.1687). E Correlation analysis between SI and age of diagnosis (P = 0.0041). F Correlation analysis between SI and frequency of severe infections (P = 0.0661). GP91 protein levels in three patients and the SI in one patient were detected using the FITC channel after changing to a new flow cytometer, including one patient with X910 CGD and two patients with X91+ CGD (SI of 1.9 for P4)
Clinical Manifestations of X91+ CGD
Overview
Here, we report seven patients with X91+ CGD exhibiting different neutrophil stimulation indices and varying clinical presentations (Table 1). The median age of onset was 4 months (range, 0.5–24 months), and two patients had early clinical manifestations during the neonatal period. The median age of diagnosis was 22 months, and three patients were diagnosed after 5 years of age. None of the patients were products of a consanguineous union and two (P1 and P7) had a positive family history (Fig. 1B). The uncle of patient 1 (P1) died of unknown causes at the age of 10 years. Two uncles and one oldest brother of P7 died of fever and pulmonary infection within the age of 5 years. The second brother of P7 presented with regional BCG infection and recurrent pulmonary tuberculosis.
Infection Characteristics
Infections were the most common clinical symptoms and varied in severity. The patients had different sites of infections, such as lung (6/7), lymph nodes (5/7), skin and soft tissue (3/7), perianal (2/7), blood stream (2/7), bone (1/7), and gastrointestinal tract (1/7) infections. Pneumonia was common, most with recurrent infections. In terms of the etiology, these patients were at high risk for M. tuberculosis (5/7), bacterial (3/7), and fungal (1/7) infections (supplemental data 1: S1). One patient was considered to have a definite fungal infection due to a positive galactomannan (GM) test in bronchoalveolar lavage fluid (BALF). Bacteria including Burkholderia gladioli, Corynebacterium striatum, and Klebsiella pneumoniae were detected in the pus or respiratory secretions by culture or mNGS. Mycobacterium neogold (reads, 78) was detected in the blood of one patient with osteomyelitis and multiple bone destruction.
M. tuberculosis infection was considered a prominent manifestation of X91+ CGD patients. With the exception of P3, all patients received the BCG vaccine at birth, according to the vaccination records, and 50% (3/6) had probable BCG infections. P1 and P4 presented with left axillary lymph node enlargement at 3–4 months old with delayed healing of BCG vaccination sites. P4 had persistent lymph node enlargement with intermittent fever, and his chest CT showed bilateral lung infection. His PPD test was strongly positive (+ + +) at the age of 15 months. P5 presented with suppuration at the BCG vaccination site at 5 months, followed by clavicular and scapular lymph node enlargement. At the age of 7, he developed recurrent fever with cervical lymph node enlargement. The pathology of the lymph node biopsy was suggestive of tuberculosis, and the PPD test was positive. P6 had a chest CT showing diffuse bilateral lung lesions and a positive PPD test (+ +); therefore, M. tuberculosis was considered. P7 suffered from recurrent fever and lymph node enlargement beginning at the age of 4 years, and his chest CT was notable for miliary tuberculosis and lymph node calcification. He also had a positive PPD test.
Noninfectious Complications
Two patients (P2 and P7) experienced recurrent oral ulcers. Two had a temporary liver function impairment characterized by elevated liver enzyme levels. Lastly, two patients (P1 and P6) developed anemia.
Treatment and Follow-up
Most patients (5/7) received prophylactic sulfamethoxazole (SMZ). Five symptomatic patients received double, triple, or quadruple anti-tuberculosis medications consisting of isoniazide and rifampicin with or without ethambutol and pyrazinamide, and responded to the treatment. Six patients underwent antifungal treatment, including voriconazole, fluconazole, or itraconazole. Two patients (P2 and P7) received interferon gamma (IFN-γ) therapy and were in good condition during the follow-up period. Three patients received hematopoietic stem cell transplantation (HSCT), and all survived. Four patients who did not receive HSCT were still alive, as confirmed by clinical follow-up.
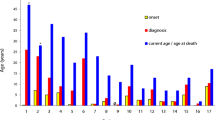
Comparison Between X91+ and Other X-linked CGD Types
Patients with X-linked CGD carrying CYBB mutations were divided into classic type X-linked CGD (X910 CGD) and variant type X-linked CGD, including X91− CGD and X91+ CGD based on gp91 expression (Fig. 2A). In our cohort, the SI of the seven patients with X91+ CGD varied widely from 1.9 to 67.3, including five with an SI ≥ 20 (Fig. 2B and Fig. 3). The SI ranged from 1.2 to 35.7 in patients with X910 CGD, including 74.5% (38/51) of patients with an SI ≤ 5, while the SI in patients with X91− CGD was less than 5, with only one exception. The difference in the SI among the three groups (X91+ CGD, X91− CGD, and X910 CGD) was statistically significant (P = 0.0071), and a higher SI was associated with higher gp91 protein expression (r = 0.6402, P < 0.001) (Fig. 2C). Correlation analysis between the SI and the age of onset (P = 0.1687), the age of diagnosis (P = 0.0041), and the frequency of severe infections (P = 0.0661) was performed (Fig. 2D, E, and F).
GP91 expression and the DHR assay for patients 1–7 with X91+ CGD. Gp91 assay: isotype control (blue) and GP91 antibody (red) are shown. The Y-axis represents the cell count. The X-axis is the fluorescence intensity. The % represents the expression of gp91 on the patient compared to the control. DHR assay: unstimulated (blue) and PMA-stimulated (red) neutrophils are shown. The Y-axis represents the cell count. The X-axis is the fluorescence intensity. The SI of each patient is marked. HC: healthy control. Samples from P1 (gp91 expression) and P4 (gp91 expression and DHR) were analyzed with the FITC channel, and the other samples were analyzed using the AF488 channel
We further compared the clinical characteristics of the three groups (X91+ CGD, X91− CGD, and X910 CGD) in terms of onset age, diagnosis age, infection frequency, infection sites, and other parameters (Table 2). Patients with X910, X91−, and X91+ CGD showed no significant differences in onset age, diagnosis age, or severe infection frequency. Lung, lymph node, and skin infections were common infection sites in patients with X91+, X910, and X91− CGD. Approximately half of the patients with X91+ and X910 CGD had definite or probable BCG infections. Among patients without HSCT treatment, all patients with X91+ and X91− CGD survived, but two patients with X910 CGD died.
X91+ CGD Gene Mutations and Literature Review
Six missense mutations and one splice site mutation of the CYBB gene were detected in the seven patients with X91+ CGD. Four X91+ CGD–related CYBB mutations were reported previously, including c.162G > C, c.170C > A, c.1223G > A, and c.1244C > A, while c.1462–2 A > T and c.1243C > T resulted in amino acid (AA) changes similar to those previously reported at the same location. The c.925G > A mutation has been previously reported to be related to X91− CGD.
Then, we searched PubMed and found 35 cases of variant type X91+ CGD with available data [1, 2, 4, 8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32], which contained 27 mutations (Table 3). The distribution of loci at the DNA and protein levels is summarized in Fig. 4. Mutations related to X91+ CGD, which are mainly located in exons 3, 9, 10, 12, and 13, included 24 missense mutations, one splicing mutation, one deletion mutation, and one deletion/insertion mutation. In the structure of the protein encoded by the CYBB gene, two mutations (p. Arg54Ser and p. Ala57Glu) are located in regions encoding the second transmembrane region, most of the other mutations are located in the potential flavin adenine dinucleotide (FAD)– and NADPH-binding domains, and two mutations (p. Cys546Pro and p. Glu568Lys) are located in regions encoding the C-terminal tail, which is essential for NADPH oxidase complex assembly. Therefore, these loci associated with X91+ CGD were concentrated in the second transmembrane or intracellular segment.
CYBB gene mutations in patients with X91+ CGD in our cohort and previous reports. The bar above shows the distribution of CYBB gene mutations in the cDNA detected in patients with X91− (top panel) and X91+ (bottom panel) CGD. The bar below shows the distribution of CYBB gene mutations in the protein detected in patients with X91+ CGD. The mutation sites identified in our cohort are marked in red. *Novel mutations related to X91+ CGD in our study
Among 24 patients with X91+ CGD for whom definite clinical records of recurrent infection were available, pulmonary infection, including pneumonia and pulmonary abscess, was the most common presentation (14/24). Other clinical manifestations included skin or perianal involvement (9/24), lymphadenitis (7/24), diarrhea (6/24), hepatic abscess (5/24), and sepsis (4/24). One patient experienced disseminated intravascular coagulation (DIC) due to Pseudomonas cepacia infection. Although recurrent infection was common, most patients recovered after antibacterial or antifungal treatment. Only two patients died at the ages of 10 months and 5 years due to severe pneumonia.
X91− CGD–related mutations [1, 4, 10, 17, 18, 20, 22, 25, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57] included splicing, deletion, and missense mutations. X91− CGD involved mutations across all domains and was not limited to the specific segment as observed in X91+ CGD.
Discussion
CGD is a rare primary immunodeficiency resulting from the inability of neutrophils to generate respiratory bursts and produce O2−. CYBB mutations encoding gp91phox result in X-linked CGD. Typical X-linked CGD accounts for more than 90% of X-linked CGD cases [10], with a pattern of early-onset disease characterized by lack of gp91phox expression and low neutrophil SI. Therefore, the combination of low SI and lack of gp91phox expression is often used in the rapid clinical diagnosis of X-linked CGD. Approximately 80% (51/64) of patients in our cohort had X910 CGD, while other patients had specific GP91 protein signatures. The proportion of X91+ CGD was higher than expected.
Gp91phox is composed of 570 amino acids. The N-terminus contains six transmembrane regions, in which two hemes are coordinated by four histidines. The C-terminus of gp91phox is a cytosolic tail containing NADPH- and FAD-binding sites. The C-terminal cytosolic tail of gp91phox is responsible for transferring electrons from intracellular NADPH to FAD, and this reaction activity is called iodonitrotetrazolium (INT) diaphorase activity. Two hemes are aligned in series and are responsible for transferring electrons from reduced FAD (FADH2) to extracellular or intravesicular O2, thus forming O2−. Resting-state gp91phox binds to p22phox and localizes to the cellular membrane. After receiving activation signals, p47phox, p40phox, and p67phox translocate to the gp91phox-p22phox heterodimer to form the NADPH oxidase complex [58]. Western blotting was used to analyze gp91phox in the past, while flow cytometry–based extracellular staining with monoclonal antibody (mAb) 7D5 is currently used to analyze gp91phox levels [1, 2].
The review showed that X91+ CGD–associated mutations were often located in the second transmembrane or intracellular regions, including potential FAD/NADPH-binding domains, which may be hot spots. Different mutation sites lead to different changes in protein function. Mutations p. Arg54Ser and p. Ala57Glu are located at the second transmembrane region of gp91phox. Positively charged Arg54 is hydrogen bonded to the outer heme. Mutated gp91phox with uncharged Ser54 has a redox potential of − 300 mV, thus blocking electrons exiting from heme to form O2− [59]. In vitro experiments confirmed normal FADH2 levels [60] but no O2− production by the Arg54Ser mutation [17]. A similar mechanism is observed for p. Ala57Glu. Ala57 is an uncharged amino acid; however, glutamic acid is negatively charged and much larger than Ala, thus inhibiting electron exit from the transmembrane passage [11]. The mutation p. Glu309Lys is located in the region between the membrane and dehydrogenase domain and is involved in p65-p22phox binding [61]. P415 is located at the intracellular NADPH-binding region of gp91phox. The mutation p. Pro415His disrupts the consensus sequence for an NADPH-binding site (GXGXGXXPF) and causes NADPH binding defects [62, 63]. Therefore, p. Pro415His-mutated gp91phox does not produce O2−, although gp91phox expression levels, FAD incorporation, and NADPH oxidase assembly are normal. Presumably, p. Pro415Ser results in similar changes to p. Pro415His. Studies suggested that the p. Gly408Glu mutation strongly inhibited the translocation of p47phox and p67phox to the phagosomal membranes of the mutants [62]. Defective FAD incorporation results in a deficiency in NADPH oxidase activity. This mutation presumably causes defective complex assembly, directly interferes with FAD/NADPH binding, and disrupts electron transfer [62, 63]. According to the analyses of the previously reported mutations c.1462-2A > G and c.1462-2A > C, we hypothesize that the c.1462-2A > T mutation removes the 3′ splice acceptor site of intron 11 and results in a partial p. Ala488_Glu497del mutation in the gp91phox protein [1, 9]. In wild-type gp91phox, residues 484 to 503 form an α-helical loop lying over the NADPH-binding cleft [31]. For patients carrying the c.1462–2 mutation, loss of this structure subsequently disturbs NADPH binding and electron transfer to FAD. Therefore, the normally expressed gp91 protein is nonfunctional or partially functional and results in defective neutrophils in these patients.
Notably, a high neutrophil SI detected using the DHR123 test does not indicate mild symptoms or a good prognosis for patients with variant type X-linked CGD. Although DHR has the advantages of requiring a small blood volume, short time, and convenience compared with direct superoxide detection, it has limitations in terms of molecular mechanism [64]. NADPH oxidase transfers electrons to molecular oxygen to generate O2−, which is dismutated to hydrogen peroxide (H2O2). Although to a lesser extent and lower priority, electrons can leak from FADH2 in the NADPH oxidase enzyme, directly producing H2O2 without the intermediate O2−. For neutrophils with normal FADH2 but no O2−, such as p. Arg54Ser, neutrophil respiratory burst tests indicate the H2O2 produced by FADH2, and thus the SI does not fully reflect O2− levels which represent the function of NADPH oxidase [32]. The partial production of H2O2 generation is not sufficient to protect patients with X91+ CGD from severe infections, under conditions with a high bacterial load [26]. In our study, all patients with CGD had a lower SI than healthy controls. Patients with X91+ variant–type CGD could have a higher SI than patients with X91− or X910 CGD, but the three groups showed no significant differences in onset age, diagnosis age, or severe infection frequency. The SI was not statistically correlated with the age of onset or the frequency of severe infections. In the cohort analyzed by Wu et al., a patient with an SI of 40.15 died of severe pneumonia within 1 year of age, while a patient with an SI of 1.99 was still alive at 10 years of age [46]. Therefore, the SI may have more value in the diagnosis of CGD than in the prediction of disease severity. The diagnosis of CGD should be considered when SI is below the normal range. For patients with X91+ CGD and a slightly lower SI, physicians should evaluate their manifestation and make the diagnosis carefully to avoid delay. Bacterial killing tests and superoxide quantification tests should be performed if necessary.
Interestingly, the same mutations in different patients sometimes result in different phenotypes. For example, the mildest case of CYBB c.1462–2 A > G mutation remained healthy until the age of 69 years, while one of his grandsons died at the age of 5 years [9]. In our cohort, male patients in the family of P7 also presented the disease with varying severity. Two uncles and his oldest brother died of fever and lung infection within 5 years after birth, while P7 and his second brother survived to the ages of 8 and 16 years, respectively. Similar conditions were reported in patients carrying other mutations [10, 23, 55], indicating that other factors are involved in the immune defense of CGD patients [1, 9, 26, 65]. Clinical symptoms, SI, protein expression, and gene analysis should be considered for a comprehensive evaluation of patients with variant type X-linked CGD, especially X91+ CGD.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
The study was approved by the ethics committee of Children’s Hospital of Fudan University.
References
Roos D, van Leeuwen K, Hsu AP, Priel DL, Begtrup A, Brandon R, et al. Hematologically important mutations: X-linked chronic granulomatous disease (fourth update). Blood Cells Mol Dis. 2021;90: 102587.
Zhou Q, Hui X, Ying W, Hou J, Wang W, Liu D, et al. A cohort of 169 chronic granulomatous disease patients exposed to BCG vaccination: a retrospective study from a single center in Shanghai, China (2004–2017). J Clin Immunol. 2018;38(3):260–72.
Gao LW, Yin QQ, Tong YJ, Gui JG, Liu XY, Feng XL, et al. Clinical and genetic characteristics of Chinese pediatric patients with chronic granulomatous disease. Pediat Allerg Imm-UK. 2019;30(3):378–86.
Roos D, Boer MD, Kuribayashi F, Meischl C, Weening RS, Segal AW, et al. Mutations in the X-linked and autosomal recessive forms of chronic granulomatous disease. Blood. 1996;87(5):1663–81.
Mauch L, Lun A, O’Gorman MR, Harris JS, Schulze I, Zychlinsky A, et al. Chronic granulomatous disease (CGD) and complete myeloperoxidase deficiency both yield strongly reduced dihydrorhodamine 123 test signals but can be easily discerned in routine testing for CGD. Clin Chem. 2007;53(5):890–6.
Vowells SJ, Sekhsaria S, Malech HL, Shalit M, Fleisher TA. Flow cytometric analysis of the granulocyte respiratory burst: a comparison study of fluorescent probes. J Immunol Methods. 1995;178(1):89–97.
Wang J, Yu H, Zhang VW, Tian X, Feng Y, Wang G, et al. Capture-based high-coverage NGS: a powerful tool to uncover a wide spectrum of mutation types. Genet Med. 2016;18(5):513–21.
Mollin M, Beaumel S, Vigne B, Brault J, Roux-Buisson N, Rendu J, et al. Clinical, functional and genetic characterization of 16 patients suffering from chronic granulomatous disease variants - identification of 11 novel mutations in CYBB. Clin Eep Immunol. 2021;203(2):247–66.
SCHAPIRO B NPKM. Chronic granulomatous-disease presenting in a 69-year-old man. New Engl J Med. 1991;325(25):1765–90.
Ishibashi F, Nunoi H, Endo F, Matsuda I, Kanegasaki S. Statistical and mutational analysis of chronic granulomatous disease in Japan with special reference to gp91-phox and p22-phox deficiency. Hum Genet. 2000;106(5):473–81.
T ArigaI Y SKT. A newly recognized point mutation in the cytochrome b558 heavy chain gene replacing alanine57 by glutamic acid, in a patient with cytochrome b positive X-linked chronic granulomatous disease. Eur J Pediatr. 1993;152:469–72.
Tefano Dusi KANM. Nicotinamide-adenine dinucleotide phosphate oxidase assembly and activation in EBV-transformed B lymphoblastoid cell lines of normal and chronic granulomatous disease patients. J Immunol. 1998;161(9):4968–74.
Marie Jose Stasia BLAM. Molecular and functional characterization of a new X-linked chronic granulomatous disease variant (X91þ) case with a double missense mutation in the cytosolic gp91phox C-terminal tail. Biochim Biophys Acta. 2002;1586(3):316–30.
Clara Bionda XJLR. Functional analysis of two-amino acid substitutions in gp91 phox in a patient with X-linked flavocytochrome b558-positive chronic granulomatous disease by means of transgenic PLB-985 cells. Hum Genet. 2004;115(5):418–27.
Leusen AUJ, Meischl C, Eppink M, Hilarius P, de Boer M, Weening R, et al. Four novel mutations in the gene encoding gp91-phox of human NADPH oxidase: consequences for oxidase assembly. Blood. 2000;95(2):666–73.
Bakri F, Martel C, Khuri-Bulos N, Mahafzah A, El-Khateeb M, Al-Wahadneh A, et al. First report of clinical, functional, and molecular investigation of chronic granulomatous disease in nine Jordanian families. J Clin Immunol. 2009;29(2):215–30.
Rae J, Newburger PE, Dinauer MC, Noack D, Hopkins PJ, Kuruto R, et al. X-linked chronic granulomatous disease: mutations in the CYBB gene encoding the gp91- phox component of respiratory-burst oxidase. Am J Hum Genet. 1998;62(6):1320–31.
Dinauer MC, Curnutte JT, Rosen H, Orkin SH. A missense mutation in the neutrophil cytochrome b heavy chain in cytochrome-positive X-linked chronic granulomatous disease. J Clin Invest. 1989;84(6):2012–6.
Jurkowska M, Kurenko-Deptuch M, Bal J, Roos D. The search for a genetic defect in Polish patients with chronic granulomatous disease. Arch Immunol Ther Exp. 2004;52(6):441–6.
Kannengiesser C, Gérard B, El Benna J, Henri D, Kroviarski Y, Chollet-Martin S, et al. Molecular epidemiology of chronic granulomatous disease in a series of 80 kindreds: identification of 31 novel mutations. Hum Mutat. 2008;29(9):E132–49.
Leusen JH, de Boer M, Bolscher BG, Hilarius PM, Weening RS, Ochs HD, et al. A point mutation in gp91-phox of cytochrome b558 of the human NADPH oxidase leading to defective translocation of the cytosolic proteins p47-phox and p67-phox. J Clin Invest. 1994;93(5):2120–6.
Stasia MJ, Bordigoni P, Floret D, Brion JP, Bost-Bru CC, Michel GR, et al. Characterization of six novel mutations in the CYBB gene leading to different sub-types of X-linked chronic granulomatous disease. Hum Genet. 2005;116(1–2):72–82.
Azuma H, Oomi H, Ueda D, Sasaki K, Makita Y, Tomizawa K, et al. Cytochrome b positive X-linked chronic granulomatous disease: a normal cell surface expression of cytochrome b. Eur J Pediatr. 1992;151(4):279–82.
Jirapongsananuruk O, Niemela JE, Malech HL, Fleisher TA. CYBB mutation analysis in X-linked chronic granulomatous disease. Clin Immunol. 2002;104(1):73–6.
Roesler J, Heyden S, Burdelski M, Schäfer H, Kreth H, Lehmann R, et al. Uncommon missense and splice mutations and resulting biochemical phenotypes in German patients with X-linked chronic granulomatous disease. Exp Hematol. 1999;27(3):505–11.
Wolach B, Broides A, Zeeli T, Gavrieli R, de Boer M, van Leeuwen K, et al. Two X-linked chronic granulomatous disease patients with unusual NADPH oxidase properties. J Clin Immunol. 2011;31(4):560–6.
Lugo Reyes SO, Mahlaoui N, Prando C, Blancas Galicia L, Hubeau M, Blanche S, et al. Variant of X-linked chronic granulomatous disease revealed by a severe Burkholderia cepacia invasive infection in an infant. Case Reports Immunol. 2013.
Blancas-Galicia L, Santos-Chavez E, Deswarte C, Mignac Q, Medina-Vera I, Leon-Lara X, et al. Genetic, immunological, and clinical features of the first Mexican cohort of patients with chronic granulomatous disease. J Clin Immunol. 2020;40(3):475–93.
Martel C, Mollin M, Beaumel S, Brion JP, Coutton C, Satre V, et al. Clinical, functional and genetic analysis of twenty-four patients with chronic granulomatous disease - identification of eight novel mutations in CYBB and NCF2 genes. J Clin Immunol. 2012;32(5):942–58.
Kalsoom K, Khan TA, Asif H, Iqbal A. A novel missense mutation in the NADPH binding domain of CYBB abolishes the NADPH oxidase activity in a male primary immunodeficiency patient with increased susceptibility to infections. Eur J Immunol. 2017;47:173.
Boog B, Quach A, Costabile M, Smart J, Quinn P, Singh H, et al. Identification and functional characterization of two novel mutations in the alpha-helical loop (residues 484–503) of CYBB/gp91(phox) resulting in the rare X91(+) variant of chronic granulomatous disease. Hum Mutat. 2012;33(3):471–5.
Cross AR, Heyworth PG, Rae J, Curnutte JT. A variant X-linked chronic granulomatous disease patient (X91+) with partially functional cytochrome b. J Biol Chem. 1995;270(14):8194–200.
Newburger PE, Skalnik DG, Hopkins PJ, Eklund EA, Curnutte JT. Mutations in the promoter region of the gene for gp9l-phox in X-linked chronic granulomatous disease with decreased expression. J Clin Invest. 1994;94:1205–11.
Stasia MJ, Brion J, Boutonnat J, Morel F. Severe clinical forms of cytochrome b–negative chronic granulomatous disease (X91−) in 3 brothers with a point mutation in the promoter region of CYBB. J Infect Dis. 2003;188(10):1593–604.
Defendi F, Decleva E, Martel C, Dri P, Stasia MJ. A novel point mutation in the CYBB gene promoter leading to a rare X minus chronic granulomatous disease variant–impact on the microbicidal activity of neutrophils. Biochim Biophys Acta. 2009;1792(3):201–10.
Suzuki S, Kumatori A, Haagen IA, Fujii Y, Sadat MA, Jun HL, et al. PU.1 as an essential activator for the expression of gp91phox gene in human peripheral neutrophils, monocytes, and B lymphocytes. Proc Natl Acad Sci U S A. 1998;95(11):6085–90.
WEENING R S DBMK. Point mutations in the promoter region of the CYBB gene leading to mild chronic granulomatous disease. Clin Exp Immunol. 2000;122(3):410–7.
Glaser J, Dienethal MG, Mann O, von Eiff M, Pausch J. Chronic granulomatosis: a rare differential diagnosis in liver granulomas in adulthood. Dtsch Med Wschr. 1995;120:646–8.
Porter CD, Kuribayashi F, Parkar MH, Roos D, Kinnon C. Detection of gp91-phox precursor protein in B-cell lines from patients with X-linked chronic granulomatous disease as an indicator for mutations impairing cytochrome b558 biosynthesis. Biochem J. 1996;315(Pt 2 (2)):571–5.
von Goessel H, Hossle JP, Seger R, Gungor T. Characterization of 17 new cases of X-linked chronic granulomatous disease with seven novel mutations in the CYBB gene. Exp Hematol. 2006;34(4):528–35.
Di Matteo G, Giordani L, Finocchi A, Ventura A, Chiriaco M, Blancato J, et al. Molecular characterization of a large cohort of patients with chronic granulomatous disease and identification of novel CYBB mutations: an Italian multicenter study. Mol Immunol. 2009;46(10):1935–41.
Hui YF, Chan SY, Lau YL. Identification of mutations in seven Chinese patients with x-linked chronic granulomatous disease. Blood. 1996;88(10):4021–8.
Brunner J, Dockter G, Rosen-Wolff A, Roesler J. X-linked chronic granulomatous disease (CGD) caused by an intra-exonic splice mutation (CYBB exon 3, c.252G-A) is mimicking juvenile sarcoidosis. Clin Exp Rheumatol. 2007;25(2):336–8.
de Boer M, van Leeuwen K, Geissler J, Belohradsky BH, Kuijpers TW, Roos D. Mutation in an exonic splicing enhancer site causing chronic granulomatous disease. Blood Cells Mol Dis. 2017;66:50–7.
Bolscher BG, de Boer M, de Klein A, Weening RS, Roos D. Point mutations in the beta-subunit of cytochrome b558 leading to X- linked chronic granulomatous disease. Blood. 1991;77(11):2482–7.
Wu J, Wang W, Zhang Y, Chen T. Clinical features and genetic analysis of 48 patients with chronic granulomatous disease in a single center study from Shanghai, China (2005–2015): new studies and a literature review. J Immunol Res. 2017;2017:1–17.
JENDROSSEK V RANB. An in-frame triplet deletion within the gp91-phox gene in an adult X-linked chronic granulomatous disease patient with residual NADPH-oxidase activity. Eur J Haematol. 1997;2(58):78–85.
Bu-Ghanim HN, Segal AW, Keep NH, Casimir CM. Molecular analysis in three cases of X91- variant chronic granulomatous disease. Blood. 1995;86(9):3575–82.
Jakobsen MA, Katzenstein TL, Valerius NH, Roos D, Fisker N, Mogensen TH, et al. Genetical analysis of all Danish patients diagnosed with chronic granulomatous disease. Scand J Immunol. 2012;76(5):505–11.
LIN S J HYFC. Molecular quality control machinery contributes to the leukocyte NADPH oxidase de¢ciency in chronic granulomatous disease. Biochim Biophys Acta. 2002;1586(3):275–86.
Yoshida LS, Saruta F, Yoshikawa K, Tatsuzawa O, Tsunawaki S. Mutation at histidine 338 of gp91phox depletes FAD and affects expression of cytochrome b558 of the human NADPH oxidase. J Biol Chem. 1998;273(43):27879–86.
Wolach B, Gavrieli R, de Boer M, Gottesman G, Ben-Ari J, Rottem M, et al. Chronic granulomatous disease in Israel: clinical, functional and molecular studies of 38 patients. Clin Immunol. 2008;129(1):103–14.
Tsuda M, Kaneda M, Sakiyama T, Inana I, Owada M, Kiryu C, et al. A novel mutation at a probable heme-binding ligand in neutrophil cytochrome b558 in atypical X-linked chronic granulomatous disease. Hum Genet. 1998;103(4):377–81.
de Oliveira E, Prando C, Lopez J, Arango J, Buzolin M, Rehder J, et al. High-performance liquid chromatography underpartially denaturing conditions (dHPLC) is a fast andcost-effective method for screening moleculardefects: four novel mutations found in X-linked chronic granulomatous disease. Scand J Immunol. 2012;76(2):158–66.
Sacco KA, Smith MJ, Bahna SL, Buchbinder D, Burkhardt J, Cooper MA, et al. NAPDH oxidase-specific flow cytometry allows for rapid genetic triage and classification of novel variants in chronic granulomatous disease. J Clin Immunol. 2020;40(1):191–202.
Kulkarni M, Hule G, de Boer M, van Leeuwen K, Kambli P, Aluri J, et al. Approach to molecular diagnosis of chronic granulomatous disease (CGD): an experience from a large cohort of 90 Indian patients. J Clin Immunol. 2018;38(8):898–916.
Zurro NB, Tavares De Albuquerque JA, Franca TT, Vendramini P, Arslanian C, Tavares-Scancetti F, et al. A novel mutation in CYBB gene in a patient with chronic colitis andrecurrent pneumonia due to X-linked chronic granulomatous disease. Pediater Blood Cancer. 2018;65(12).
Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87(1):245–313.
Cross AR, Segal AW. The NADPH oxidase of professional phagocytes—prototype of the NOX electron transport chain systems. Biochim Biophys Acta. 2004;1657(1):1–22.
Picciocchi A, Debeurme F, Beaumel S, Dagher M, Grunwald D, Jesaitis AJ, et al. Role of putative second transmembrane region of Nox2 protein in the structural stability and electron transfer of the phagocytic NADPH oxidase. J Biol Chem. 2011;286(32):28357–69.
Beaumel S, Grunwald D, Fieschi F, Stasia MJ. Identification of NOX2 regions for normal biosynthesis of cytochrome b558 in phagocytes highlighting essential residues for p22phox binding. Biochem J. 2014;464(3):425–37.
Debeurme F, Picciocchi A, Dagher M, Grunwald D, Beaumel S, Fieschi F, et al. Regulation of NADPH oxidase activity in phagocytes. J Biol Chem. 2010;285(43):33197–208.
Robinson JM, Badwey JA. The NADPH oxidase complex of phagocytic leukocytes: a biochemical and cytochemical view. Histochem Cell Biol. 1995;103(3):163–80.
Al-Riyami AZ, Al-Zadjali S, Al-Mamari S, Al-Said B, Al-Qassabi J, Al-Tamemi S. Correlation between flow cytometry and molecular findings in autosomal recessive chronic granulomatous disease: a cohort study from Oman. Int J Lab Hematol. 2018;40(5):592–6.
Yu L, Cross AR, Zhen L, Dinauer MC. Functional analysis of NADPH Oxidase in granulocytic cells expressing a ▵488-497 gp91phox deletion mutant. Blood. 1999;94(7):2497–504.
Acknowledgements
We thank the patients and their families for their cooperation.
Author information
Authors and Affiliations
Contributions
Bijun Sun and Zeyu Zhu contributed to the study conception and design, and drafted the manuscript. Xiaoying Hui completed the experimental data section. Jinqiao Sun, Wenjie Wang, Wenjing Ying, Qinhua Zhou, and Haili Yao contributed to the study design and data collection. Jia Hou and Xiaochuan Wang gave academic feedback and revised the manuscript. All authors have reviewed the final manuscript and agreed to be accountable for the work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent to Participate
Written informed consent was obtained from the parents.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, B., Zhu, Z., Hui, X. et al. Variant Type X91+ Chronic Granulomatous Disease: Clinical and Molecular Characterization in a Chinese Cohort. J Clin Immunol 42, 1564–1579 (2022). https://doi.org/10.1007/s10875-022-01324-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-022-01324-3