Abstract
Many drug-resistance mutations in HIV-1 reverse transcriptase fall within cytotoxic T lymphocytes (CTL) epitopes, but studies of the response to these epitopes in patients with virological failure are lacking. We therefore compared IFN-γ ELISPOT responses to the YV9 epitope (RT181-189) covering the lamivudine resistance mutation, M184V, in HLA-A2+ antiretroviral treatment (ART)-naive patients (n = 19), to those found in HLA-A2+ patients with virological failure (n = 15). Ten ART-naive patients had an ELISPOT response to the wild-type epitope that cross-reacted with the mutant epitope. Two patients with virological failure showed a specific response to the 184V mutant epitope. Responses against YV9 were strongly associated (p = 0.005) with the presence of a 177E mutation, and the same tendency was observed in an independent cohort of patients (n = 22). These results indicate that variants in flanking residues may influence CTL responses to conserved subdominant HIV-1 epitopes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytotoxic T lymphocytes (CTL) play an important role in the control of HIV-1 replication, both during primary [1] and chronic infection. CTL with many different specificities are involved in the control of viral replication during acute infection [2], while in chronic infection several groups have reported that Gag-specific CTL are associated with lower viral load (VL) [3–6], indicating a major role for Gag-specific CTL in limiting HIV-1 replication. However, associations between HIV-1 sequence polymorphisms in the Pol and Nef genes and the HLA class I genotype of the infected individual have provided evidence that CTL directed against epitopes in HIV-1 protease (PR), reverse transcriptase (RT), and Nef proteins also exert selection pressure on the virus during chronic infection [7, 8].
Most studies of the antiviral effects of CTL have involved antiretroviral-naive patients, and much less is known concerning the role of CTL in patients undergoing antiretroviral therapy (ART). Although several studies have documented a reduction in the frequency of HIV-specific CTL in the peripheral blood after the initiation of ART [9–11], HIV-specific CTL can still be detected in patients after suppression of viral replication, and one recent longitudinal study has shown that these CTL recover multiple effector functions with prolonged ART [12]. It is currently not known whether the HIV-specific CTL that are present during ART can suppress the residual viremia that remains despite effective ART [13], or limit virological failure (VF) due to the accumulation of drug-resistance mutations. Nevertheless, since many drug-resistance mutations in the HIV-1 PR and RT fall within CTL epitopes [14–19], it has been proposed that CTL directed against these epitopes might limit the replication of drug-resistant viruses.
These previous studies have defined which drug-resistance mutations can be targeted by CTL, but for the most part they concerned patient groups with diverse drug-resistance mutations, occurring within several different CTL epitopes restricted by a variety of HLA molecules. For each particular epitope/drug-resistance mutation combination, the number of patients studied was small, making it difficult to reach conclusions concerning the frequency of these CTL responses in patients with drug-resistant virus, and their role in vivo. One exception was the report by Karlsson et al. who studied the response to the HLA-A2-restricted PR76-84 epitope. They found that most HLA-A2+ patients with protease inhibitor (PI)-resistant virus had a detectable response to this epitope [16], even though it was infrequently targeted in untreated HLA-A2+ patients [20].
In order to test whether these findings can be generalized to other epitopes containing drug-resistance mutations, we chose to study the CTL response against epitopes covering the M184V mutation in RT that confers resistance to lamivudine (3TC)[21] and emtricitabine (FTC). Our choice was motivated by three main factors. Firstly, 3TC and FTC are unique among the nucleotide RT inhibitors, in that a single mutation at position 184 confers complete (>1,000-fold) resistance to the drug. Hence, almost all patients with VF under ART incorporating 3TC or FTC harbor viruses with a resistance mutation at position 184, predominantly 184V. Secondly, the M184V mutation carries a well-characterized fitness cost to the virus, and is therefore not detectable in antiretroviral-naive patients. Thirdly, the two epitopes described in the literature as covering the M184V mutation, VL9 (RT179-187) [22] and YV9 (RT181-189) [14], are restricted by HLA-A2, which is the most frequent HLA class I allele. Nevertheless, it is still unclear from the literature which of the two reported HLA-A2-restricted epitopes is dominant, and there is currently no data concerning CTL responses directed against either of the two epitopes in patients with active replication of 3TC-resistant virus.
We therefore compared the frequency and magnitude of IFN-γ ELISPOT responses to the VL9 and YV9 epitopes in HIV-1-infected antiretroviral-naive patients and patients with VF despite ART incorporating 3TC. Peptides representing both the wild-type and the 184V sequences were systematically tested, as were peptides representing the immunodominant HLA-A2-restricted epitopes in Gag and RT. We found that the YV9 epitope, but not VL9, was frequently targeted in HLA-A2+ patients, and that the presence of an ELISPOT response to YV9 was correlated with viral load and viral sequence polymorphism upstream of the epitope. These two factors explained why most of the patients we studied with VF did not generate a CTL response specifically targeting the M184V mutation, and overall, our results confirm that naturally occurring variants in flanking residues can influence the development of CTL responses to conserved subdominant HIV-1 epitopes.
Patients and Methods
Patients
In Nantes, two groups of HIV-1-infected patients were enrolled in the study from March 2006 to April 2008: patients who had never received any antiretroviral treatment (“ART-Naive” group) and patients with virological failure (VL > 50 copies/ml) despite ART including 3TC, or patients whose viral genome sequencing had shown the presence of the M184V mutation in the previous 12 months ("3TC" group). One patient receiving lamivudine monotherapy for concurrent HBV infection was also included in the 3TC Group. In Erlangen, 21 patients receiving ART and one patient during treatment interruption were enrolled from February 2008 to July 2010. All patients gave informed consent, and the study was authorized by the ethical review boards of Nantes University Hospital and the University of Erlangen-Nuremberg.
Cell Preparation and Flow Cytometry
On the occasion of one of their regular hospital visits, participating patients gave 15 mL peripheral blood collected on heparinized tubes, and PBMC were isolated by ficoll density gradient centrifugation. Cells were cryo-preserved in 50% FCS, 40% RPMI, and 10% DMSO in liquid nitrogen. HLA-A2+ patients were identified by flow cytometry after staining whole blood with phycoerythrin (PE)-conjugated anti-HLA-A2 (clone BB7.2, Serotec, Cergy St Christophe, France). PBMC from HLA-A2+ patients were thawed and used for further experiments.
The phenotype of CD8+ lymphocytes was studied by staining cryo-preserved PBMC with the following monoclonal antibody combinations: CD4/CD8/HLA-DR/CD38, CD4/CD8/CD27/CD28, CD4/CD8/IgG2a and CD4/CD8/CD279. All antibodies used were from BD Biosciences (Pont de Claix, France). Data were acquired on a FACS Canto flow cytometer and analyzed using FACS Diva software.
IFN-γ ELISPOT Assay
IFN-γ secretion by viral peptide-specific CD8+ T cells was quantified by the ELISPOT assay performed as previously described [23]. Briefly, 96-well nitrocellulose plates (Millipore, Molsheim, France) were coated with 1 μg/mL mouse monoclonal anti-human IFN-γ (clone 1-D1-K, Mabtech, Sophia Antipolis, France) overnight at 4°C. Plates were washed, then blocked for 2 h at 37°C with complete medium (RPMI 1640 containing 10% FCS, 4 mM l-glutamine, 50 U/mL penicillin, and 50 μg/ml streptomycin). Cells were plated in triplicates at 1 × 105 viable cells per well and stimulated with different peptides (NeoMPS, Table I) at a final concentration of 3 μM. Positive control wells were plated at 1,500 viable cells per well and stimulated with PMA (500 ng/ml) + ionomycin (50 ng/ml). Plates were incubated overnight at 37°C with 5% CO2. Wells were washed with PBS 0.05% Tween 20 and filled with 100 μL of biotinylated monoclonal mouse anti-human IFN-γ antibody (Clone 7-B6, Mabtech, Sophia Antipolis, France) at 1 μg/mL, followed by alkaline phosphatase-labeled extravidin (Sigma, St Quentin Fallavier, France). Finally spots were developed with BCIP/ NBT reagent (Sigma).
IFN-γ spot-forming cells (SFC) were counted using an automated ELISPOT reader (Autoimmun Diagnostika Gmbh, Strassberg, Germany) and their number expressed as SFC/106 PBMC. Signals were considered positive if the mean value of the triplicate was greater than (1) the mean + 2 SD of negative control wells and (2) the mean of negative control wells + 50 SFC/106 PBMC.
CTL Lines and Clones
CTL lines were generated by stimulating PBMC with the 10-μM YV9M peptide for 3 h, then sorting IFN-γ-secreting cells using magnetic beads following the manufacturer's instructions (MACS, Miltenyi, Paris, France). Sorted cells were cultured with 1 μg/mL PHA-L + 150 U/mL IL-2 together with irradiated feeder cells (1 × 104 EBV-B cells + 1 × 105 PBMC from an unrelated donor per well) in U-bottomed 96-well plates. Clones were obtained by limiting dilution, and clonality was confirmed by TCR sequencing.
For patients analyzed in Erlangen, short-term cultures were performed before testing for peptide-specific responses. PBMC (5 × 106) were stimulated with 6 μg/mL YV9M peptide in 1 mL with complete medium supplemented with 10 mM Hepes and 10 U/mL recombinant interleukin-2 (Proleukin, Chiron, CA, USA). After 10 days, cells were tested for recognition of the YV9M peptide in a gamma-IFN ELISPOT assay as described above.
Functional Avidity
CTL lines and the 8D10 clone were stimulated overnight by serial peptide dilutions (from 3 μM to 0.3 pM) of the YV9M and YV9V peptides using 200 (CTL clone) or 1,000 (CTL lines) effector cells per well, together with 30,000 HLA-A2+ EBV-B cells as targets. IFN-γ SFC were counted at each dilution, and EC50 values (concentration required to induce a half-maximal number of SFC) were calculated using the NCGC Curve Fit software (http://ncgc.nih.gov/pub/openhts/curvefit/). Functional avidity was calculated as the inverse of the EC50.
Presentation of YV9 Epitope by Transfected HEK 293 Cells
The 177E mutation was introduced into a codon-optimized Gag-Pol expression vector (pHDMH_gpm2, supplied by Dr. D. Brand, University of Tours, France) by site-directed mutagenesis using the Quick-Change kit (Agilent, Massy, France). The following primers were used: forward–gcagaaccccgaGatcgtgatctaccag, reverse–tagatcacgatCtcggggttctgcttgc.
Wild-type (177D) or mutant (177E) plasmids were transfected into HEK-293 cells using the Attractene reagent (Qiagen, Courtaboeuf, France) according to the manufacturer's recommendations. Forty-eight hours later, transfected cells were harvested by pipetting in Ca2+- and Mg2+-free PBS and distributed in triplicate into the wells of an ELISPOT plate coated with IFN-γ-capture antibody. Either the 8D10 CTL clone or a clone specific for the HLA-A2-restricted SL9 epitope was added, and the plate was incubated overnight before revelation and counting of IFN-γ spots as described above. Twenty thousand target cells and 2,000 to 50,000 effector cells were used per well.
HIV-1 RT Sequencing
Viral RNA was purified from plasma samples using a MagnaPure LC instrument (Roche), and the N-terminal and central domains of the RT gene were then amplified using a one-step RNA PCR kit (Takara Bio, distributed by Lonza, St-Beauzire, France) and the following primers: MJ4C–AGTGCTTTGGYYCCCCTRAGGAGT, MJ3 AGTAGGACCTACACCTGTCA. PCR products were purified; sequencing reactions were performed using a BigDye Terminator kit and analyzed on a 3130 Genetic Analyzer (Applied Biosystems).
Statistics
Quantitative variables (VL, CD4 counts, and SFC counts) were compared by the Wilcoxon two-sample test (http://www.fon.hum.uva.nl/Service/Statistics/Wilcoxon_Test.html). For paired data, the Wilcoxon signed-rank test (http://www.fon.hum.uva.nl/Service/Statistics/Signed_Rank_Test.html) was used. Qualitative values (positive or negative response to peptide stimulus) were compared by two-tailed Fisher exact test (http://statpages.org/ctab2x2.html). All calculations were carried out using web-based resources listed at http://www.statpages.org. Differences were considered significant when p < 0.05.
Results
Clinical, Immunological, and Virological Characteristics of Patient Groups
The "ART-naïve" group consisted of 19 HLA-A2+ ART-naive patients. The "3TC group" was composed of 15 HLA-A2+ patients who either (1) had ongoing VF despite receiving ART incorporating 3TC or (2) harbored drug-resistant virus with the M184V mutation documented within the previous 12 months. Median age and peripheral CD4+ T-lymphocyte counts were similar in the two groups, while VL (p = 0.003) and nadir CD4 counts (p < 0.001) were significantly lower in the 3TC group (Table II). In addition, the proportion of activated CD38+HLA-DR+ CD8+ T lymphocytes was significantly lower in the 3TC group, although the proportion of differentiated CD27−CD28− effector CTL and the level of expression of PD-1 in the total CD8+ lymphocyte population were equivalent in ART-naive and 3TC patients (Table II).
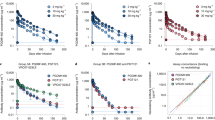
A High Proportion of Treatment-Naive HLA-A2+ Patients Generate a Cross-Reactive Response to the YV9 epitope
Within the ART-naive group, 10/19 patients had a detectable ELISPOT response to the YV9M peptide (median, 177; range, 52–1,100 SFC/106 PBMC), and nine patients also recognized YV9V (median, 110; range, 57–1,086 SFC/106 PBMC). In comparison, 8/19 ART-naive patients had an ELISPOT response against the IV9 epitope in RT (median, 343; range, 116–1,807 SFC/106 PBMC), and 10/19 showed a response against the SL9 Gag epitope (median, 191.5; range, 63–2,140 SFC/106 PBMC) (Fig. 1a). Therefore, in antiretroviral-naive patients, ELISPOT responses against YV9 were similar, both in frequency and in magnitude to those directed against the dominant HLA-A2-restricted CTL epitopes in RT and Gag. In contrast, no ELISPOT responses against the VL9 epitope were detected in the 17 ART-naive patients tested with the VL9M and VL9V peptides.
Cross-reactive IFN-γ ELISPOT response against YV9M and YV9V in ART-naive patients. a IFN-γ ELISPOT responses against HLA-A2-restricted epitopes SL9, IV9, and YV9 in ART-naive patients. Only positive responses (mean value of the triplicate >mean + 2 SD of negative control wells and >50 SFC/106 PBMC above negative control wells) are shown. b Strong correlation between ELISPOT responses to the YV9M and YV9V peptides in HLA-A2+ ART-naive patients. Patients with a positive ELISPOT response to either peptide (black circles) and those with a negative response to both YV9M and YV9V peptides (white circles) are shown. c Functional avidity of the 8D10 clone derived from patient 181 against YV9M and YV9V peptides. d Functional avidity of CTL lines from three patients against YV9M and YV9V peptides. Patient numbers are indicated in the inset panel, and the functional avidity of the clone from patient 181 is also shown for comparison
As expected, the M184V mutation was not detectable in circulating virus from ART-naive patients (data not shown). Hence, recognition of the YV9V peptide by PBMC from treatment-naive patients cannot be due to an immune response generated against virus bearing 184V, but could represent cross-reactivity of the CTL response generated against wild-type virus expressing the YV9M epitope. Indeed, ELISPOT responses against YV9V in the ART-naive patient group were strongly correlated with responses against YV9M (Fig. 1b). The same patients responded to both peptides, and since the slope of the regression equation was equal to 1, the number of cells responding to each peptide was the same in each patient. This strongly implies that the same cells responded to both peptides, as it is extremely unlikely that two different populations of CTL with distinct specificities (i.e., VY9M-specific CTL and YV9V-specific CTL) would be so similar in number in all ten patients. Furthermore, a CTL clone obtained from treatment-naive patient 181 recognized the YV9M and YV9V peptides with the same functional avidity (Fig. 1c, d), proving that a single TCR can recognize both peptide-HLA-A2 complexes with equal efficacy. The cross-reactivity of CTL cell lines from a further three patients was also analyzed. Functional avidity towards the YV9M peptide was greater than 109 M−1 in all three CTL lines, but somewhat lower towards YV9V in two of the three cell lines (Fig. 1d), indicating a degree of preferential recognition of the wild-type peptide in these patients.
Four patients in the ART-naive group with ELISPOT responses to YV9M subsequently received ART. Three of the four patients achieved a full virological response, but despite the suppression of viral replication, these three patients maintained a detectable response against YV9M and YV9V (Fig. 2a, b, d). In the fourth patient, ELISPOT responses against both YV9M and YV9V were undetectable 1 year after the initiation of ART (Fig. 2c). These results indicate that ELISPOT responses against YV9M generated before the initiation of ART can persist at a detectable level during ART.
YV9-specific ELISPOT persists after initiation of ART. Line graphs show evolution of VL (right-hand scale) after initiation of ART with treatments as indicated (EFV efavirenz, TDF tenofovir, FTC emtricitabine, SQV saquinavir, RTV ritonavir, ZDV zidovudine, 3TC lamivudine, ATV atazanavir). Open bars represent IFN-γ ELISPOT response (left-hand scale) to YV9M; closed bars represent responses to YV9V. Time is indicated as the number of days after initiation of ART
Memory Response to YV9M and Specific Recognition of YV9V in 3TC Patients
ELISPOT responses against the HLA-A2-restricted epitopes SL9 and IV9 in the 3TC group (Fig. 3a) were equivalent, both in terms of frequency and magnitude, to those observed in the ART-naive group, and 4/15 patients in the 3TC group had a positive ELISPOT response to YV9. Although the frequency of responses to YV9 was somewhat lower in the 3TC group compared to the ART-naive group, this difference was not significant (p = 0.17, Fisher's exact test). As in ART-naive patients, no ELISPOT responses were detected against either the VL9M or VL9V peptides in patients with 3TC-resistant virus.
Selective IFN-γ ELISPOT response against YV9V in two 3TC patients. IFN-γ ELISPOT responses against HLA-A2-restricted epitopes SL9, IV9 and YV9 in patients with VF despite ART incorporating 3TC. For SL9 and IV9, only positive responses (mean value of the triplicate > mean + 2 SD of negative control wells and >50 SFC/106 PBMC above negative control wells) are shown. For YV9, responses against YV9M and YV9V are shown for each 3TC subject responding to one of the two peptides. Patient code numbers are shown in the inset box
Two distinct types of response to the YV9 epitope were observed in the 3TC group. As seen in the ART-naive group, the ELISPOT response in patients 180 and 228 cross-reacted with YV9M and YV9V suggesting that the YV9-specific response in these patients represented memory CTL initially generated against the wild-type virus before the initiation of ART. In contrast, patients 48 and 193 had a positive ELISPOT response against YV9V but not YV9M, indicating that these patients had generated an immune response specifically directed against the 3TC-resistant virus (Fig. 3).
Association of 177E Polymorphism with Positive ELISPOT Responses to YV9 Epitope
Unlike other patients in the 3TC group, virus sequences from patients 48 and 193 carried a D177E mutation at position 177 in RT (data not shown). In order to test whether the presence of 177E was correlated with a detectable ELISPOT response to YV9, we pooled data from both ART-naive and 3TC groups. Sequences were obtained from 18 ART-naive patients, so sequences from a total of 33 patients were considered. Overall, eight patients carried the 177E mutation, of whom seven had an ELISPOT response to either YV9M or YV9V. Among the 25 patients whose virus did not harbor 177E, only seven had a detectable ELISPOT to the YV9 epitope (Fig. 4a). The presence of an ELISPOT response against YV9 was therefore associated with the presence of the 177E mutation in plasma virus (p = 0.005, Fisher's exact test). Logistic regression showed that this association was independent of both patient group and any of the immunological parameters that we measured (current and nadir CD4 count, and percentage of activated, effector, or exhausted CD8+ T cells). However, in a two-factor model, the presence of a YV9-specific ELISPOT response was strongly associated with 177E in plasma virus (p < 0.02) and marginally associated with plasma VL (p = 0.06).
Correlation between RT177E polymorphism and presence of an ELISPOT response against the YV9 epitope. a Proportion of YV9 responders in the Nantes and Erlangen cohorts as a function of sequence polymorphism at the RT177 position. The inset figures above each column show the number of patients responding to the YV9 peptide over the number of patients tested. Statistical significance was tested by Fisher's exact test. b Effect of 177D/E polymorphism on presentation of the YV9 epitope. HEK 293 cells were transfected with plasmids coding for the Gag-Pol polyprotein with either 177D (white bars) or 177E (black bars) in the RT protein. Transfected cells were co-cultured in triplicate with CTL clones specific for the YV9 epitope in RT or the SL9 epitope in Gag. Activation of clones was detected by IFN-γ ELISPOT, and results are presented as mean SFC/106 effector cells with error bars representing the standard deviation. One representative experiment of four is shown. Statistical significance was tested by Student's t test
To confirm the association between the 177E mutation and the immune response to the YV9 epitope, data were obtained from an independent cohort of patients. As these patients were receiving ART, PBMC cultures were stimulated with YV9M peptide for 10 days before testing for the presence of YV9-specific cells by IFN-γ ELISPOT. Despite this difference in methodology, a higher frequency of YV9-specific responses in patients carrying viruses with 177E was also seen in this group of patients, although the association was not statistically significant (Fig. 4a).
To test the effect of the polymorphism at position 177 on processing and presentation of the YV9 epitope, the 177E mutation was introduced into a plasmid coding for a codon-optimized Gag-Pol polyprotein. The wild-type (177D) and mutated (177E) plasmids were transfected into HEK 293 cells which were then co-cultured with either the YV9-specific 8D10 CTL clone, or with a CTL clone specific for the SL9 epitope in Gag. Presentation of the SL9 epitope was not significantly different between 177D and 177E Gag-pol plasmids, whereas activation of the YV9-specific clone was significantly greater after transfection with the 177E Gag-pol plasmid compared to the 177D plasmid (Fig. 4b). These results indicate that the 177E mutation allowed more efficient presentation of the YV9 epitope.
Discussion
In this work we initially analyzed the ELISPOT response to the HLA-A2-restricted YV9 epitope in two groups of patients seropositive for HIV-1: ART-naive patients carrying 3TC-sensitive (184M) virus and patients with virological failure due to the presence of the 184V mutation in the RT protein. In addition to the fact that patients in the 3TC group had ongoing antiviral therapy, the two patient groups were distinct in terms of VL, duration of infection, nadir CD4+ T-cell count, and the degree of CD8+ T-cell activation. Despite these differences, the levels of ELISPOT responses against the HLA-A2-restricted SL9 and IV9 epitopes that we used as positive controls were remarkably similar in the two groups. Therefore, patients in the 3TC group did not have a global reduction in the HLA-A2-restricted cellular immune response compared to patients in the treatment-naive group. This was consistent with the observation that neither PD-1 expression, indicating cell senescence or “exhaustion,” nor the proportion of CD27−CD28− effector cells in CD8+ lymphocytes was different between groups.
Overall, we found frequent responses to the YV9 epitope but not the overlapping VL9 epitope. This is consistent with previous studies [24, 25] and confirms that YV9, rather than VL9, is the dominant HLA-A2-restricted epitope in this region of the RT protein. ART-naive patients with positive ELISPOT responses against the YV9M epitope also recognized the VY9V epitope, even though virus in these patients carried the wild-type 184M sequence. Analyses of three CTL lines and one CTL clone showed that responses generated against the YV9M peptide displayed either complete or partial cross-reactivity between YV9M and YV9V. Complete cross-reactivity was characterized by recognition of both peptides with identical functional avidities, while partial cross-reactivity involved preferential recognition of the YV9M peptide. None of the treatment-naive patients developed an ELISPOT response to YV9 that showed preferential recognition of the YV9V epitope.
In the 3TC group, two patients also had a cross-reactive ELISPOT response to YV9. The persistence of YV9-specific ELISPOT responses generated in ART-naive patients after initiation of therapy, and the YV9M/YV9V cross-reactivity observed in ART-naive patients suggested that these were memory responses generated before treatment, rather than de novo CTL responses generated against 3TC-resistant virus. However, since we did not have access to cells sampled before the initiation of therapy for any of the patients in the 3TC group, it was not possible to confirm that this was the case.
In addition, patients 48 and 193 in the 3TC group had ELISPOT responses specifically directed against YV9V. As none of the patients in the ART-naive group developed responses with this specificity, it is reasonable to conclude that these two patients had developed an immune response directed against mutant virus. Development of a response specifically targeting drug-resistant virus is therefore possible, but occurs only in a minority of patients with virological failure under 3TC—only two of the 13 3TC patients with no evidence of a memory YV9M-specific response developed a response to YV9V. Since ELISPOT responses to the SL9 and IV9 epitopes were similar in the 3TC group compared to the ART-naive group, and there was no evidence for a lack of CTL effectors (CD27-CD28- cells) or more extensive CTL exhaustion in patients in the 3TC group, failure to mount a de novo response against YV9V was probably not due to general impairment of the cellular immune response in the 3TC group. We therefore examined virological parameters that might explain why only these two patients developed a response against YV9V.
Interestingly, a D177E polymorphism just upstream of the YV9 epitope was present in virus sequences from patients 48 and 193, but not in any of the other patients in the 3TC group. Overall 177E was strongly associated with the presence of a detectable ELISPOT response against either YV9V or YV9M in the Nantes cohort. The same tendency was also observed in an independent group of patients with ongoing ART studied in Erlangen. Although data from both sites showed that more than 80% of patients whose virus carried 177E mounted a response to the YV9 epitope, there was a higher frequency of YV9-specific responses in patients without 177E in the Erlangen cohort. This may have been related to methodological differences between the two sites, as ELISPOT responses were tested after the expansion of peptide-specific CTL in culture in Erlangen, whereas in Nantes, ELISPOT responses were tested directly on thawed PBMC. Higher sensitivity of the assay used in Erlangen could therefore have resulted in more responses being detected in patients without 177E. We also considered whether virus subtype could contribute to the association that we observed, since 177E is frequently found in the RT of non-subtype B viruses. However, most of the patients included in the Nantes and Erlangen cohorts were infected with subtype B viruses, and the association between 177E and an ELISPOT response against YV9 remained significant (p = 0.01) in the Nantes cohort if the analysis was restricted to patients with the subtype B virus.
Previous studies have shown that mutations in N-terminal flanking residues can modify epitope processing and presentation [26–28], and the initial data that we report here indicate that the 177E mutation has a direct effect on the presentation of the YV9 epitope. However, we have also found that YV9-specific cell lines recognize target cells infected with recombinant vaccinia virus expressing RT protein with 177D just upstream of the YV9 epitope (data not shown). Taken together, these results suggest that although the YV9 epitope can be processed and presented from RT proteins containing 177D, presentation is enhanced by the 177E polymorphism. This is consistent with the observation that some patients carrying virus with 177D–particularly those with higher viral loads–did have detectable ELISPOT responses to the YV9 epitope. Based on the effects of sequence polymorphism on antigen processing, Tenzer and colleagues suggested that "the specific sequence of any transmitted virus may affect the likelihood of CTL priming" [29]. The strong positive correlation between the presence of 177E and the development of a response against YV9 that we observed seems to confirm this prediction and, to the best of our knowledge, constitutes the first reported example of such an effect.
In conclusion, we have shown that although CD8+ T-cell responses against the YV9M epitope occur frequently in treatment-naive patients, most patients with 3TC-resistant virus do not develop an immune response specifically directed against the YV9V epitope that carries the M184V resistance mutation. Questions arising from this work include whether YV9-specific CTL can inhibit the replication of HIV-1, in particular 3TC-resistant virus, and whether the 177E polymorphism could affect the antiviral efficacy of YV9-specific CTL.
Abbreviations
- ART:
-
Antiretroviral treatment
- SFC:
-
Spot-forming cells
- VF:
-
Virological failure
- VL:
-
Viral load
- 3TC:
-
Lamivudine
References
Koup RA, Safrit JT, Cao Y, Andrews CA, McLeod G, Borkowsky W, et al. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J Virol. 1994;68:4650–5.
Jones NA, Wei X, Flower DR, Wong M, Michor F, Saag MS, et al. Determinants of human immunodeficiency virus type 1 escape from the primary CD8+ cytotoxic T lymphocyte response. J Exp Med. 2004;200:1243–56.
Edwards BH, Bansal A, Sabbaj S, Bakari J, Mulligan MJ, Goepfert PA. Magnitude of functional CD8+ T-cell responses to the Gag protein of human immunodeficiency virus type 1 correlates inversely with viral load in plasma. J Virol. 2002;76:2298–305.
Zuñiga R, Lucchetti A, Galvan P, Sanchez S, Sanchez C, Hernandez A, et al. Relative dominance of Gag p24-specific cytotoxic T lymphocytes is associated with human immunodeficiency virus control. J Virol. 2006;80:3122–5.
Geldmacher C, Currier JR, Herrmann E, Haule A, Kuta E, McCutchan F, et al. Cd8 t-cell recognition of multiple epitopes within specific Gag regions is associated with maintenance of a low steady-state viremia in human immunodeficiency virus type 1-seropositive patients. J Virol. 2007;81:2440–8.
Kiepiela P, Ngumbela K, Thobakgale C, Ramduth D, Honeyborne I, Moodley E, et al. Cd8+ t-cell responses to different HIV proteins have discordant associations with viral load. Nat Med. 2007;13:46–53.
Moore CB, John M, James IR, Christiansen FT, Witt CS, Mallal SA. Evidence of HIV-1 adaptation to HLA-restricted immune responses at a population level. Science. 2002;296:1439–43.
Brumme ZL, John M, Carlson JM, Brumme CJ, Chan D, Brockman MA, et al. HLA-associated immune escape pathways in HIV-1 subtype b Gag, Pol and Nef proteins. PLoS ONE. 2009;4:e6687.
Kalams SA, Goulder PJ, Shea AK, Jones NG, Trocha AK, Ogg GS, et al. Levels of human immunodeficiency virus type 1-specific cytotoxic t-lymphocyte effector and memory responses decline after suppression of viremia with highly active antiretroviral therapy. J Virol. 1999;73:6721–8.
Ogg GS, Jin X, Bonhoeffer S, Dunbar PR, Nowak MA, Monard S, et al. Quantitation of HIV-1-specific cytotoxic T lymphocytes and plasma load of viral RNA. Science. 1998;279:2103–6.
Ogg GS, Jin X, Bonhoeffer S, Moss P, Nowak MA, Monard S, et al. Decay kinetics of human immunodeficiency virus-specific effector cytotoxic T lymphocytes after combination antiretroviral therapy. J Virol. 1999;73:797–800.
Rehr M, Cahenzli J, Haas A, Price DA, Gostick E, Huber M, et al. Emergence of polyfunctional CD8+ T cells after prolonged suppression of human immunodeficiency virus replication by antiretroviral therapy. J Virol. 2008;82:3391–404.
Palmer S, Maldarelli F, Wiegand A, Bernstein B, Hanna GJ, Brun SC, et al. Low-level viremia persists for at least 7 years in patients on suppressive antiretroviral therapy. Proc Natl Acad Sci USA. 2008;105:3879–84.
Samri A, Haas G, Duntze J, Bouley JM, Calvez V, Katlama C, et al. Immunogenicity of mutations induced by nucleoside reverse transcriptase inhibitors for human immunodeficiency virus type 1-specific cytotoxic t cells. J Virol. 2000;74:9306–12.
Mason RD, Bowmer MI, Howley CM, Gallant M, Myers JCE, Grant MD. Antiretroviral drug resistance mutations sustain or enhance CTL recognition of common HIV-1 Pol epitopes. J Immunol. 2004;172:7212–9.
Karlsson AC, Deeks SG, Barbour JD, Heiken BD, Younger SR, Hoh R, et al. Dual pressure from antiretroviral therapy and cell-mediated immune response on the human immunodeficiency virus type 1 protease gene. J Virol. 2003;77:6743–52.
Schmitt M, Harrer E, Goldwich A, Bäuerle M, Graedner I, Kalden JR, et al. Specific recognition of lamivudine-resistant HIV-1 by cytotoxic T lymphocytes. AIDS. 2000;14:653–8.
Stratov I, Dale CJ, Chea S, McCluskey J, Kent SJ. Induction of T-cell immunity to antiretroviral drug-resistant human immunodeficiency virus type 1. J Virol. 2005;79:7728–37.
Mueller YM, Bojczuk PM, Halstead ES, Kim AHJ, Witek J, Altman JD, et al. IL-15 enhances survival and function of HIV-specific CD8+ T cells. Blood. 2003;101:1024–9.
Karlsson AC, Chapman JM, Heiken BD, Hoh R, Kallas EG, Martin JN, et al. Antiretroviral drug therapy alters the profile of human immunodeficiency virus type 1-specific T-cell responses and shifts the immunodominant cytotoxic T-lymphocyte response from Gag to Pol. J Virol. 2007;81:11543–8.
Gu Z, Gao Q, Li X, Parniak MA, Wainberg MA. Novel mutation in the human immunodeficiency virus type 1 reverse transcriptase gene that encodes cross-resistance to 2′,3′-dideoxyinosine and 2′,3′-dideoxycytidine. J Virol. 1992;66:7128–35.
Harrer E, Harrer T, Barbosa P, Feinberg M, Johnson RP, Buchbinder S, et al. Recognition of the highly conserved YMDD region in the human immunodeficiency virus type 1 reverse transcriptase by HLA-a2-restricted cytotoxic T lymphocytes from an asymptomatic long-term nonprogressor. J Infect Dis. 1996;173:476–9.
Dalod M, Harzic M, Pellegrin I, Dumon B, Hoen B, Sereni D, et al. Evolution of cytotoxic T lymphocyte responses to human immunodeficiency virus type 1 in patients with symptomatic primary infection receiving antiretroviral triple therapy. J Infect Dis. 1998;178:61–9.
Karlsson AC, Iversen AKN, Chapman JM, de Oliviera T, Spotts G, McMichael AJ, et al. Sequential broadening of CTL responses in early HIV-1 infection is associated with viral escape. PLoS ONE. 2007;2:e225.
Schmitt-Haendle M, Bachmann O, Harrer E, Schmidt B, Bäuerle M, Harrer T. Recognition patterns of HLA-a2-restricted human immunodeficiency virus-1-specific cytotoxic T-lymphocytes in a cohort of HIV-1-infected individuals. Viral Immunol. 2005;18:627–36.
Draenert R, Le Gall S, Pfafferott KJ, Leslie AJ, Chetty P, Brander C, et al. Immune selection for altered antigen processing leads to cytotoxic T lymphocyte escape in chronic HIV-1 infection. J Exp Med. 2004;199:905–15.
Milicic A, Price DA, Zimbwa P, Booth BL, Brown HL, Easterbrook PJ, et al. CD8+ T cell epitope-flanking mutations disrupt proteasomal processing of HIV-1 Nef. J Immunol. 2005;175:4618–26.
Le Gall S, Stamegna P, Walker BD. Portable flanking sequences modulate CTL epitope processing. J Clin Invest. 2007;117:3563–75.
Tenzer S, Wee E, Burgevin A, Stewart-Jones G, Friis L, Lamberth K, et al. Antigen processing influences HIV-specific cytotoxic T lymphocyte immunodominance. Nat Immunol. 2009;10:636–46.
Acknowledgments
This work was supported by the Association de Recherche sur le SIDA et les Infections des Immunodéprimés (ARSIID) and grants from the DFG (DFG grant HA 2331/2-1) the Hector Foundation (TH), and IZKF (TH: A27). Y.P. was the recipient of a scholarship awarded by the Région des Pays de la Loire. The authors would like to thank Bernard Besse and Olivier Barre for HIV-1 RT gene sequencing, and Christelle Retière and Anne Hosmalin for useful comments on the manuscript. We would particularly like to thank the patients who agreed to participate in this study.
Conflict of Interest
The author declares no financial or commercial conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pacheco, Y., Allavena, C., Guilloux, Y. et al. The Immune Response to the RT181-189 Epitope in HIV-1-Infected Patients is Associated with Viral Sequence Polymorphism Flanking the Epitope. J Clin Immunol 31, 681–689 (2011). https://doi.org/10.1007/s10875-011-9520-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-011-9520-z