Abstract
The objective of this study was to investigate changes in sedentary and active behaviors when previously inactive adults start exercising in the morning or evening. One-hundred adults with overweight or obesity (BMI ≥ 25 kg/m2) were recruited for a 12-week intervention and randomized to one of three groups: (i) morning exercise (AMEx; 0600–0900); (ii) evening exercise (PMEx; 1600–1900); or (iii) waitlist control. AMEx and PMEx were prescribed self-paced aerobic exercise to achieve a weekly total of 250 min via a combination of supervised and unsupervised training. Sedentary and active behavior times were measured at baseline, mid- and post-intervention using the multimedia activity recall for children and adults. Time spent engaging in physical activity was significantly increased from baseline at both mid- (+ 14–22 min·day−1) and post-intervention (+ 12–19 min·day−1), for AMEx and PMEx. At 12-weeks, participants in both morning and evening exercise groups reported increased time spent Sleeping (+ 36 and + 20 min·day−1, respecitively), and reduced time spent watching TV/playing videogames (− 32 and − 25 min·day−1, respectively). In response to an exercise stimulus, previously inactive adults make encouraging modifications in how they use their time, and the patterns of change are similar with morning and evening exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The health benefits of exercise for reducing the risk of non-communicable diseases such as cardiovascular disease, type II diabetes and some cancers, are well documented (Centers for Disease Control & Prevention, 2018). Despite this, 44.5% of Australian adults are either inactive (14.8%), or have low levels of physical activity (29.7%) (Australian Government Department of Health, 2017), often attributed to a self-reported lack of time (Sallis & Hovell, 1990).
The number of hours in a day is fixed and finite, distributed between obligatory time (such as time spent working, sleeping, domestic activities, commuting or eating) and discretionary time (the remaining ‘free’ time) (Goodin et al., 2002; Mekary et al., 2009). Some activities are seemingly ‘inelastic’ and require a fixed amount of time (such as work commitments) while others seem to be ‘elastic’ (such as sleep, screen time, eating, and exercise) (Olds et al., 2012). Physical activity researchers have started to consider individuals’ whole-of-day activity patterns to help understand how people use their time (Baere et al., 2015; Gomersall et al., 2014), and therefore, to identify timeframes when new activities, such as exercise, can realistically be incorporated and sustained. However, to ‘make time’ for a new exercise program, time must be drawn from another activity/activities. These activity ‘modifications’ can have important health consequences; i.e., the activities that are displaced may enhance, or mitigate the positive effects of exercise (Chastin et al., 2015; Gomersall et al., 2014; Mekary et al., 2009, 2013). Gomersall and colleagues investigated the changes in use-of-time across a 6-week physical activity intervention in a sample of 129 insufficiently active adults (Gomersall et al., 2014). The researchers found that time to accommodate increased physical activity predominantly displaced time spent watching television, suggesting an encouraging activity modification. Eleven participants dropped out of the study due to ‘being unable to make the time commitment’. When considering individual’s social, work and family commitments, previously inactive individuals may try to accommodate exercise at a time-of-day which is not sustainable long-term.
To improve compliance and adherence to exercise, the concept of temporal consistency has been proposed. Regularly performing an activity at a specific time, may be important for long-term adherence as it aids in creating a ‘protected time’ for exercise habits (Kaushal & Rhodes, 2015; Rhodes & Bruijn, 2010). Morning and evening (before and after work) are key windows of opportunity to incorporate exercise (Bailey & Jung, 2014; Brooker et al., 2021; Schumacher et al., 2019). The few studies which have investigated the influence of exercise time-of-day on physical activity participation / exercise adherence report mixed findings. Burn et al. (Burn et al., 2017) reported greater compliance in the ‘after-work’ (i.e., afternoon/evening) group compared with the ‘in-work’ (i.e., at lunchtime) group in their 40-day work-place physical activity intervention (70% v. 26%, respectively). Other studies have compared morning and evening periods; some favour morning (Bailey & Jung, 2014; Bond et al., 2017), and others report no difference in rates of exercise adherence between morning and evening periods (Blasio et al., 2010; Brooker et al., 2019; in press; Creasy et al., 2022). While there is agreement that regular exercise plays an important role in improving general health and maintaining energy balance, there remains a distinct lack of evidence regarding an optimal time-of-day for exercise to maximize compliance.
The activity swaps in response to morning or evening exercise are not understood, and are likely to be different. For example, a person who embarks on a new morning exercise program may forego their recreational walk (Sahlqvist et al., 2013).This type of displacement could result in a negligible net increase in overall physical activity and thus, energy expenditure, attenuating the benefits of the added exercise. Conversely, the addition of morning exercise to an individual’s existing routine may lead to a displacement in sleep, whereby individuals wake up earlier for exercise. This hypothesis is supported by the work by Gomersall et al. (2014) who found a trend for reduced sleep (− 30–− 41 min·day−1) when individuals were prescribed 150 and 300 min of moderate-vigorous physical activity per week for six weeks, compared with a control group of usual activity, suggesting that individuals may substitute sleep to fit in exercise. If sleep is displaced as a result of increased activity, the positive benefits of exercise may be attenuated, if baseline sleep duration is low (Chaput, 2014). Another possible scenario, for example as could be seen with the addition of a new evening exercise program, is time could be drawn from sedentary activities such as watching television (Olds et al., 2011), a displacement which would likely result in an overall increase in physical activity (Dunstan et al., 2010). There is observational and experimental evidence to support the hypothesis that changing patterns of time use are likely to have flow on effects for health (Chastin et al., 2015; Gomersall et al., 2014). For example, in a longitudinal sample of 4,558 adult females, Mekary and colleagues studied the isotemporal substitution effects of physical activity and sedentary behavior on weight status (Mekary et al., 2009). They found that changes in weight status were dependent on what activity was displaced by exercise in the overall time budget; an increase of 30 min·day−1 resulted in a weight loss of 1.6 kg if it displaced a brisk walk, compared to a weight loss of 3.7 kg if it displaced TV viewing.However, there are no studies which have compared the impact of exercise time-of-day on patterns of time use.
Therefore, the objective of this study was to investigate how previously inactive adults restructure their time when they undertake morning or evening exercise. This study was conducted within a larger randomized controlled trial aimed at investigating the influence of time-of-day of exercise on cardiometabolic health (Brooker et al., 2019; in press).
Methods
This study was registered with the Australian New Zealand Clinical Trials Registry (blind for peer review) and approved by the Bellberry Human Research Ethics Committee (HREC2016-02-130). Informed consent was obtained from all individual participants included in this study. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. The intervention is reported in accordance with CONSORT (See Supplementary Material).
Participants were recruited from the local community and metropolitan universities via electronic media and print advertising. Interested individuals were screened for eligibility by web-based or telephone survey, which included stage one of the Adult Pre-exercise Screening System, developed by Exercise and Sports Science Australia (Exercise & Sports Science Australia, 2012). To be included in the study, individuals were required to be: (i) insufficiently active (accumulating < 150 min of moderate-vigorous physical activity per week, by self-report); (ii) overweight or obese (body mass index (BMI) ≥ 25 kg/m2); and (iii) weight stable in the previous three months (± 3 kg by self-report). Individuals were considered ineligible if they: (i) were pregnant, or had plans to become pregnant over the course of the study; (ii) participated in shift work; (iii) were currently participating in a weight loss program; or (iv) were using any medication or supplements that would affect food intake, appetite or physical activity levels, weight loss, or metabolism. Individuals deemed eligible and who obtained medical clearance (as required based on their responses to the Adult Pre-exercise Screening System), or did not require it, attended the laboratory for their baseline assessment. Ineligible individuals, and those who failed to obtain medical clearance were excluded from the study.
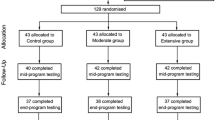
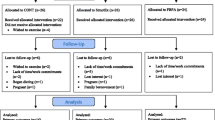
This study used a three-armed, randomized controlled trial design, with a 12-week lifestyle intervention. Following baseline testing, participants were randomized into one of two intervention groups, or a waitlist control group (CON) at a 2:2:1 ratio using permuted block randomisation with multiple, randomized block sizes by a researcher external to the study. Due to the nature of the intervention, participant blinding was not possible. Participants allocated to CON were asked to continue with their day-to-day activities and were offered the exercise program after all formal testing was completed. The two intervention conditions comprised of a 12-week exercise program in which participants were prescribed a minimum of 250 min of moderate-vigorous exercise per week; the dose of exercise recommended by the American College of Sports Medicine to elicit clinically significant weight loss (Donnelly et al., 2009). Participants randomized to the morning group (AMEx) were required to exercise between 0600–0900, and 1600–1900 for those in the evening group (PMEx). The time periods were chosen to coincide with diurnal hormone patterns, and for convenience based on when most people could accommodate exercise (i.e., before or after work), to enhance any physiological adaptations which may occur as a result of exercising at either time-of-day, and maximize adherence to the sessions (Brooker et al., 2021).
The exercise program included both supervised and unsupervised exercise sessions. Participants completed an initial four-week supervised exercise training phase, of five 50 min sessions per week. Over the remaining eight weeks, exercise sessions were tapered by one session per fortnight until two sessions per week was reached, which was then maintained for the remainder of the intervention. Supervised sessions consisted of self-paced brisk-walking or running on a treadmill. All supervised exercise sessions were conducted at the School of Human Movement and Nutrition Sciences at The University of Queensland, St. Lucia, Australia. The secondary component of the intervention involved several constituents of theoretical approaches to encourage behavior change. Informational and behavioral approaches were the focus of the intervention. Strategies used to enhance behavior change are outlined in Supplementary Table A1.
Self-reported use-of-time was measured using the adult version of the MARCA; a computerised 24-h recall tool which asks participants to recall all activities from their previous day (midnight to midnight), in increments as small as five minutes. The MARCA was administered by a computer-assisted telephone interview in an open-ended format, using meal times as reference points in a segmented day format, on two occasions approximately one week apart. Each time, two consecutive days were recalled; therefore, at each measurement participants were asked to recall four days (two weekend and two weekdays). Where possible, recalled days were kept consistent between measurement occasions. During the recall, the interviewer selected an appropriate activity from a list of over 500 activities, based on an expanded version of the Ainsworth compendium (Ainsworth et al., 2011).
Time use profiles were cleaned and checked; firstly, any activities entered as ‘other’ were identified and replaced with a similar activity (based on body position and energy expenditure) from the compendium; next, any time use profiles with missing data (< 24-h, or 1440 min) were identified and excluded; finally, participants with < 2 time use profiles recorded or did not include one weekend day per assessment period were excluded. To determine time use, participants’ individual time use profiles were established by calculating the time spent in major ‘activity sets’ and collapsed hierarchically into domains based on similarity and to preserve comparability with previous studies(Gomersall et al., 2014). Eleven mutually exclusive ‘Superdomains’ were used; physical activity, computer, active transport, passive transport, quiet time, self-care, socio-cultural, work/study, chores, sleep, and TV/Videogames (previously established in greater detail (Gomersall et al., 2010), and described in Supplementary Table A2).
All data were analysed using the statistical package for social sciences (SPSS) version 25 (IBM, New York, USA). Statistical significance was set at an alpha of p < 0.05. All results are reported as Mean (Standard Deviation), unless specified otherwise. Linear mixed modelling with fixed and random effects was used to assess changes over time and differences among groups, estimated by a restricted maximum likelihood algorithm. Group (AMEx, PMEx, CON), time (0, 6, 12), and group × time interaction were treated as fixed factors; participants were treated as a random factor with individual intercepts. Model residuals were formally assessed for normality by use of the Shapiro–Wilk test and visual inspection of histogram plots. Fishers Least Significant Difference test was used for posthoc analyses to compare mean changes in time use between groups at each assessment period. A priori power calculations determined that with an alpha of 0.05 and 80% power, we could detect a small effect size (Cohen’s d = 0.3) with a sample of 95 (n = 38 for intervention groups; n = 19 for CON).
Results
One-hundred participants were randomly allocated to AMEx (n = 40), PMEx (n = 40), or CON (n = 20) groups. Eighty-two participants completed the intervention. Reasons for drop-out were due to personal, work or family reasons (n = 12), being unable to make the time commitment (n = 4) or medical reasons (n = 2). Participants were recruited on a rolling basis from June 2016 to May 2017. Follow-up testing was completed in August 2017.
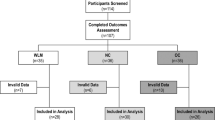
Ninety-seven participants had ≥ 2 time use profiles recorded at baseline and were included in the analysis (Fig. 1). In accordance with the CONSORT statement, significance testing of baseline differences was not performed (Boer et al., 2015; Schulz et al., 2010). Demographic characteristics appear to be similar between groups; mean age and body mass index were 41 ± 12, 38 ± 11, and 38 ± 10 years, and 31.1 ± 4.3, 32.0 ± 5.9, and 29.3 ± 3.6 kg·m−2, respectively. Seventy-six per cent of participants were female, most (77%) were in full-time employment, and university-educated (83%; Table 1).
The average time (minutes/day) spent in each time use Superdomain across all timepoints for all groups is shown in Table 2. To be considered eligible to participate in this study, participants who enrolled were not meeting the physical activity guidelines of 150–300 min·wk−1 of moderate intensity activity / 75–150 min·wk−1 of vigorous activity, or an equivalent combination of both (Australian Government Department of Health & Ageing, 2014). According to baseline estimates, on average, participants were spending less than 70 min·wk−1 being physically active (Table 2). Time spent engaging in Physical Activity was significantly increased from baseline at both mid- (14–22 min·day−1) and post-intervention (12–19 min·day−1), for AMEx and PMEx. By mid-intervention, individuals in both exercise groups were meeting physical activity guidelines (AMEx, 154 min·wk−1; PMEx, 196 min·wk−1) and activity levels remained higher than baseline values at post-intervention (AMEx, 189 min·wk−1; PMEx, 126 min·wk−1). Although there were no significant differences in time spent engaging in PA between AMEx and PMEx during the intervention, there were some subtle differences which are worth acknowledging. Participants in AMEx continued to increase, albeit non-significantly, the time they spent in PA between mid- and post-intervention (21.9 versus 27.3 min·day−1, respectively; p = 0.330). In contrast, there was a decline in PA between mid- and post-intervention in the PMEx group (28.1 versus 17.7 min·day−1, respectively; p = 0.049). Relative to baseline values, time spent in Active Transport was also significantly increased at mid-intervention (16–19 min·day−1) for intervention groups, but these changes were no longer significant from baseline by the end of the intervention (Table 2).
For AMEx, time spent in Self Care significantly increased by 11 min·day−1 at mid-intervention, but this was no longer significantly different from baseline at post-intervention. At the end of the intervention, participants reported spending more time engaging in Physical Activity and Sleep (12–19 min·day−1, and 20–36 min·day−1, respectively), relative to baseline. To accommodate this time, a significant decrease was seen in the Television/Videogames domain (25–32 min·day−1). There were no significant changes in the time participants spent: using the Computer, in Passive Transport, in Quiet Time, performing Chores, in Work and Study, or in Socio-Cultural activites in either AMEx or PMEx.
There were no significant changes observed in any of the 11 time use Superdomains during the intervention for CON at either mid- or post-intervention assessment. Figure 2 illustrates the shifts in time use among Superdomains in all groups, relative to baseline values.
Change in time (min·day−1) spent in the 11 Superdomains, relative to baseline, measured by MARCA. (A) AMEx, mid-intervention; (B) AMEx, post-intervention; (C) PMEx, mid-intervention; (D) PMEx, post-intervention; (E) CON, mid-intervention; (F) CON, post-intervention. Note The radar chart use a radial display of the 11 Superdomains on different quantitative axes. Each axis represents a quantitiat for each superdomain. Data plotted on the zero axis represents the time spent (min·day−1) in that superdomain is equal to the baseline value. Positive values (i.e., > 0) indicate more time was spent in that superdomain compared with baseline, and negative values (i.e., < 0) indicate less time was spent in that superdomain compared with baseline. Abbreviations MARCA, multimedia activity recall for children and adults; AMEx, morning exercise; PMEx, evening exercise; CON, control; PA, physical activity; TV, television; min: minutes
In response to the intervention, the patterns of change in AMEx and PMEx were similar, and both AMEx and PMEx were statistically different from CON for time spent in Physical Activity, Active Trasnport, Passive Transport and TV/Videogames (Table 3).
Discussion
How individuals restructure the timing of their behaviors can influence the effectiveness of exercise, and have important health consequences, depending on what activities are displaced (Chastin et al., 2015; Gomersall et al., 2014; Mekary et al., 2009, 2013; Olds et al., 2012). The objective of this study was to investigate how previously inactive adults restructure their time when they undertake morning or evening exercise. Time spent engaging in physical activity was significantly increased from baseline at both mid- and post-intervention for AMEx and PMEx. There were some significant shifts in time use during the intervention period, and the patterns of change were similar between the intervention groups. Participants reported more time spent sleeping, and less time watching television/playing videogames in both AMEx and PMEx. The shifts in time use in this study likely have important health benefits.
According to baseline estimates, on average, participants spent approximately two hours per day watching television (range 114 to 157 min·day−1). In this study, the addition of exercise, prescribed at a volume of ≥ 250 min·wk−1 largely displaced time previously spent sedentary (i.e., watching television). In the intervention groups, Television viewing decreased by approximately 30 min·day−1. This would appear to be an important reduction; Stamatakis and colleagues estimate that watching two or more hours of television per day increases cardiovascular disease risk by 125% (Stamatakis et al., 2011).
Both intervention groups reported an increase in Active Transport at mid-intervention and higher levels of both Active Transport compared with participants in the control group. However, these changes and differences were no longer significant post-intervention. By design, the number of supervised exercise sessions reduced from mid- (4 sessions·wk−1) to post-intervention (2 sessions·wk−1), which may explain this finding (i.e., individuals did not have to travel to the exercise venue as frequently). These findings suggest that active transport may be an added benefit to supervised sessions beyond the prescribed exercise alone. Higher levels of active transport have also been associated with cardiometabolic and nutritional benefits including lower BMI, lower waist circumference, lower cholesterol and higher vitamin D (Passi-Solar et al., 2020). Without examining intervention effects using a time use approach, the nuanced ripple effects of changes in time would not be identified and the additional understanding which can be used to adapt future research would be unrealised.
Regular exercise is advocated to improve sleep quality, either by accelerating sleep onset or increasing the depth of sleep, and is routinely included in sleep hygiene recommendations (Buman & King, 2010; Chennaoui et al., 2015). However, it has been suggested that exercising close to retiring to bed may disrupt sleep, and thus, previous sleep hygiene recommendations have been to exercise 5–6-h before bedtime, and avoid activity for 3-h before bed (Morin et al., 1134; Schutte-Rodin et al., 2008). This is unsubstantiated, and even contradicted in experimental trials (Benloucif et al., 2004; Buman & King, 2010; Buman et al., 2014; Larsen et al., 2019; Yoshida et al., 1998). In support of the more recent evidence, with the addition of exercise, participants in AMEx and PMEx reported more time spent sleeping (AMEx, + 36 min·day−1; PMEx, + 20 min·day−1). Short sleep duration has been associated with obesity risk; a meta-analysis of short sleep duration, including 604,509 adults, reported that, for a one hour reduction in sleep, there was an increase in BMI of 0.35 kg·m−2 (Cappuccio et al., 2008). According to baseline estimates, participants in our study had an average sleep duration of more than seven hours (range 7.8 to 8.3 h·day−1). Therefore, the increase in sleep duration reported in our study during the intervention is unlikely to be of clinically significance.
This is the first study to examine changes in use-of-time in response to an exercise intervention prescribed at specific times of the day. In response to a 12-week exercise program performed in the morning (0600–0900) and the evening (1600–1900), we found no difference in how previously insufficiently active individuals spend, or reorganise their time to accommodate the new activity. Gomersall and colleagues investigated the changes in use-of-time across a 6-week physical activity intervention prescribed either 150 min·wk−1 or 300 min·wk−1 (Gomersall et al., 2014). The researchers found that time to accommodate increased physical activity was largely drawn from time spent watching television. However, there were no differences in patterns of change in time use between the intervention groups. Taken together, these findings suggest that, regardless of the dose or timing of exercise prescribed, the activities that people shift (or swap) to accommodate a short-term change in exercise participation are similar.
Traditionally, time use surveys have been used to capture data such as, how respondents spend their ‘free time’; residual time that remains after accounting for time spent in ‘paid labour’, ‘unpaid household labour’ and ‘personal care’. As in the case for the Time Use Survey conducted by the Australian Bureau of Statistics, respondents are asked to keep a diary of their daily activities for two consecutive days (Goodin et al., 2002). However, these surveys have been used to capture a population-level insight into how individuals use their time, rather than tracking change in time use in response to an intervention or stimulus, and require additional coding by the analysts. Therefore, a key strength of this study is the use of the MARCA, a validated, reliable, high-resolution 24-h recall tool, which enabled a comprensive examination of participants use of time (Gomersall et al., 2010). However, due to the self-reported nature of the tool, we cannot discount social desirability and recall bias. There are also some limits to the generalisability of our findings. The sample included in this study was one of convenience, predominantly recruited from students and staff at a metropolitan university, and with a bias toward females. This study was a pre-planned secondary analysis conducted within a larger randomized controlled trial aimed at investigating the influence of time-of-day of exercise on cardiometabolic health (Brooker et al., 2019). Thus, the study was not powered to detect statistical differences between groups for secondary outcomes, or an interaction over time. Therefore, null outcomes should be treated with caution and require replication. This study is also limited by its short, 12-week intervention duration. While the use of the MARCA minimized bias by requiring individuals to recount their whole of day (24-h) activity, we cannot rule out social desirability and recall bias (Althubaiti, 2016). Finally, no follow-up data on participants’ use of time after the cessation of the intervention were collected so it is unknown whether participants maintained their exercise, and if they continued to train at the prescribed times of day.
Patterns of time use present a novel way of examining the ripple effects of changes in daily activity patterns to accommodate for the time cost of exercise. This study used a randomized controlled trial to investigate how previously inactive adults restructure their time when they undertake morning or evening exercise. The time for exercise was larglely drawn from a discretionary time (watching TV), and the patterns of change in time use was similar when exercise was performed in the morning compared with the evening.
Availability of data and material
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- AMEx:
-
Morning exercise
- CON:
-
Control
- PMEx:
-
Evening exercise
References
Ainsworth, B. E., Haskell, W. L., Herrmann, S. D., et al. (2011). 2011 compendium of physical activities: A second update of codes and met values. Medicine and Science in Sports and Exercise, 43(8), 1575–1581.
Althubaiti, A. (2016). Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 9, 211–217.
Australian Government Department of Health. Physical activity and sedentary behaviour 2017 [cited 2018]. Available from: http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-active-evidence.htm.
Australian Government Department of Health and Ageing. (2014). Australia’s physical activity and sedentary behaviour guidelines. Canberra: Department of Health and Aged Care.
Bailey, K. J., & Jung, M. E. (2014). The early bird gets the worm! Congruency between intentions and behavior is highest when plans to exercise are made for the morning. Journal of Applied Biobehavioral Research., 19(4), 233–247.
Benloucif, S., Orbeta, L., Ortiz, R., et al. (2004). Morning or evening activity improves neuropsychological performance and subjective sleep quality in older adults. Sleep, 27(8), 1542–1551.
Bond, D. S., Raynor, H. A., Thomas, J. G., et al. (2017). Greater adherence to recommended morning physical activity is associated with greater total intervention-related physical activity changes in bariatric surgery patients. Journal of Physical Activity & Health., 14(6), 492–498.
Brooker, P.G., Gomersall, S.R., King, N.A., & Leveritt, M.D. (in press). The efficacy of morning versus evening exercise for weight loss: a randomized controlled trial. Obesity. https://doi.org/10.1002/oby.23605
Brooker, P. G., Gomersall, S. R., King, N. A., & Leveritt, M. D. (2019). The feasibility and acceptability of morning versus evening exercise for overweight and obese adults: A randomized controlled trial. Contemporary Clinical Trials Communications., 14, 100320.
Brooker, P. G., Jung, M. E., Kelly-Bowers, D., et al. (2021). Does the time-of-day of exercise influence the total volume of exercise? A cross-sectional analysis of objectively monitored physical activity among active individuals. Journal of Physical Activity & Health, 18(9), 1029–1036.
Buman, M. P., & King, A. C. (2010). Exercise as a treatment to enhance sleep. American Journal of Lifestyle Medicine., 4(6), 500–514.
Buman, M. P., Phillips, B. A., Youngstedt, S. D., Kline, C. E., & Hirshkowitz, M. (2014). Does nighttime exercise really disturb sleep? Results from the 2013 national sleep foundation sleep in america poll. Sleep Medicine., 15(7), 755–761.
Burke, L. E. (2011). Self-monitoring in weight loss: A systematic review of the literature. Journal of the American Dietetic Association, 111(1), 92–102.
Burn, N., Norton, L. H., Drummond, C., & Norton, K. I. (2017). Changes in physical activity behaviour and health risk factors following a randomised controlled pilot workplace exercise intervention. AIMS Public Health., 4(2), 189–201.
Cappuccio, F. P., Taggart, F. M., Kandala, N.-B., et al. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep, 31(5), 619–626.
Centers for Disease Control and Prevention. Physical activity and health 2018 [cited 2018]. Available from: https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm.
Chaput, J.-P. (2014). Sleep patterns, diet quality and energy balance. Physiology & Behavior., 134, 86–91.
Chastin, S. F. M., Palarea-Albaladejo, J., Dontje, M. L., & Skelton, D. A. (2015). Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A novel compositional data analysis approach. PLoS ONE, 10(10), e0139984.
Chennaoui, M., Arnal, P. J., Sauvet, F., & Léger, D. (2015). Sleep and exercise: A reciprocal issue? Sleep Medicine Reviews., 20, 59–72.
Creasy, S. A., Wayland, L., Panter, S. L., et al. (2022). Effect of morning and evening exercise on energy balance: A pilot study. Nutrients, 14(4), 816.
Dalle Grave, R., Calugi, S., Molinari, E., et al. (2005). Weight loss expectations in obese patients and treatment attrition: An observational multicenter study. Obesity Research, 13(11), 1961–1969.
De Baere, S., Lefevre, J., De Martelaer, K., Philippaerts, R., & Seghers, J. (2015). Temporal patterns of physical activity and sedentary behavior in 10–14 year-old children on weekdays. BMC Public Health, 15(1), 1–13.
de Boer, M. R., Waterlander, W. E., Kuijper, L. D. J., Steenhuis, I. H. M., & Twisk, J. W. R. (2015). Testing for baseline differences in randomized controlled trials: An unhealthy research behavior that is hard to eradicate. International Journal of Behavioral Nutrition and Physical Activity., 12(1), 4.
Di Blasio, A., Di Donato, F., Mastrodicasa, M., et al. (2010). Effects of the time of day of walking on dietary behaviour, body composition and aerobic fitness in post-menopausal women. The Journal of Sports Medicine and Physical Fitness., 50, 196–201.
Donnelly, J. E., Blair, S. N., Jakicic, J. M., et al. (2009). American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercis, 41(2), 459.
Dunstan, D. W., Barr, E. L. M., Healy, G. N., et al. (2010). Television viewing time and mortality: The australian diabetes, obesity and lifestyle study (ausdiab). Circulation, 121(3), 384–391.
Exercise and Sports Science Australia. Adult pre-exercise screening system (apss) 2012 [cited 2015 15 October]. Available from: https://www.essa.org.au/for-gps/adult-pre-exercise-screening-system/.
Garaulet, M., Pérez-Llamas, F., Zamora, S., & Tebar, F. J. (1999). Weight loss and possible reasons for dropping out of a dietary/behavioural programme in the treatment of overweight patients. Journal of Human Nutrition and Dietetics., 12(3), 219–227.
Gleeson-Kreig, J. M. (2006). Self-monitoring of physical activity: Effects on self-efficacy and behavior in people with type 2 diabetes. The Diabetes Educator, 32(1), 69–77.
Gomersall, S. R., Norton, K., Maher, C., English, C., & Olds, T. S. (2014). In search of lost time: When people undertake a new exercise program, where does the time come from? A randomized controlled trial. Journal of Science and Medicine in Sport., 18(1), 43.
Gomersall, S., Olds, T., & Ridley, K. (2010). Development and evaluation of an adult use-of-time instrument with an energy expenditure focus: The adult marca. Journal of Science and Medicine in Sport., 12, e76-e.
Goodin, R. E., Rice, J. M., Bittman, M., & Saudners, P. (2002). The time pressure illusion: Discretionary time versus free time. The Social Policy Research Centre, University of New South Wales.
Hayakawa, Y., Miki, H., Takada, K., & Tanaka, K. (2000). Effects of music on mood during bench stepping exercise. Perceptual and Motor Skills, 90(1), 307–314.
Kaushal, N., & Rhodes, R. E. (2015). Exercise habit formation in new gym members: A longitudinal study. Journal of Behavioral Medicine., 38(4), 652–663.
Larsen, P., Marino, F., Melehan, K., Guelfi, K. J., Duffield, R., & Skein, M. (2019). Evening high-intensity interval exercise does not disrupt sleep or alter energy intake despite changes in acylated ghrelin in middle-aged men. Experimental Physiology., 104(6), 826–836.
Mekary, R. A., Lucas, M., Pan, A., et al. (2013). Isotemporal substitution analysis for physical activity, television watching, and risk of depression. American Journal of Epidemiology, 178(3), 474–483.
Mekary, R. A., Willett, W. C., Hu, F. B., & Ding, E. L. (2009). Isotemporal substitution paradigm for physical activity epidemiology and weight change. American Journal of Epidemiology, 170(4), 519–527.
Messier, V., Hayek, J., Karelis, A. D., et al. (2010). Anthropometric, metabolic, psychosocial and dietary factors associated with dropout in overweight and obese postmenopausal women engaged in a 6-month weight loss programme: A monet study. British Journal of Nutrition, 103(8), 1230–1235.
Morin, C. M., Hauri, P. J., Espie, C. A., Spielman, A. J., Buysse, D. J., & Bootzin, R. R. (1999). Nonpharmacologic treatment of chronic insomnia. An american academy of sleep medicine review. Sleep, 22(8), 1134.
Mutsaerts MAQ, Kuchenbecker WKH, Mol BW, Land JA, Hoek A.(2013). Dropout is a problem in lifestyle intervention programs for overweight and obese infertile women: A systematic review. Human Reproduction.
National Health and Medical Research Council. (2013). Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in australia. Canberra, Australia.
Olds, T., Ferrar, K. E., Gomersall, S. R., Maher, C., & Walters, J. L. (2012). The elasticity of time: Associations between physical activity and use of time in adolescents. Health Education & Behavior, 39(6), 732–736.
Olds, T. S., Maher, C. A., & Matricciani, L. (2011). Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep, 34(10), 1299–1307.
Passi-Solar, Á., Margozzini, P., Cortinez-O’Ryan, A., Muñoz, J. C., & Mindell, J. S. (2020). Nutritional and metabolic benefits associated with active and public transport: Results from the chilean national health survey, ens 2016–2017. Journal of Transport & Health., 17, 100819.
Racette, S. B., Weiss, E. P., Villareal, D. T., et al. (2006). One year of caloric restriction in humans: Feasibility and effects on body composition and abdominal adipose tissue. Journals of Gerontology., 61(9), 943–950.
Rhodes, R. E., & de Bruijn, G.-J. (2010). Automatic and motivational correlates of physical activity: Does intensity moderate the relationship? Behavioral Medicine., 36(2), 44–52.
Sahlqvist, S., Goodman, A., Cooper, A. R., & Ogilvie, D. (2013). Change in active travel and changes in recreational and total physical activity in adults: Longitudinal findings from the iconnect study. The International Journal of Behavioral Nutrition and Physical Activity., 10(1), 28.
Sallis, J. F., & Hovell, M. F. (1990). Determinants of exercise behavior. Exercise and Sport Sciences Reviews., 18, 307–330.
Schulz, K. F., Altman, D. G., & Consort, M. D. (2010). statement: Updated guidelines for reporting parallel group randomised trials. BMJ, 2010, 340.
Schumacher, L. M., Thomas, J. G., Raynor, H. A., et al. (2019). Relationship of consistency in timing of exercise performance and exercise levels among successful weight loss maintainers. Obesity, 27(8), 1285–1291.
Schutte-Rodin, S. L., Broch, L., Buysee, D., Dorsey, C., & Sateia, M. (2008). Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine., 4(5), 487–504.
Stamatakis, E., Hamer, M., & Dunstan, D. W. (2011). Screen-based entertainment time, all-cause mortality, and cardiovascular events: Population-based study with ongoing mortality and hospital events follow-up. Journal of the American College of Cardiology., 57(3), 292–299.
Yoshida, H., Ishikawa, T., Shiraishi, F., & Kobayashi, T. (1998). Effects of the timing of exercise on the night sleep. Psychiatry and Clinical Neurosciences., 52(2), 139–140.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. PB was supported by an Australian Government Research Training Programme scholarship.
Author information
Authors and Affiliations
Contributions
PB was responsible for conceptualisation and design of the study, the acquisition, analysis and interpretation of data, and manuscript writing. SG contributed to design of the study, data interpretation and critical revision of the manuscript. NM contributed to the acquisition and analysis of data, and critical revision of the manuscript. NK and ML contributed to design of the study, data interpretation and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Not applicable.
Human and animal rights and Informed consent
This study was approved by the Bellberry Human Research Ethics Committee (HREC2016-02–130). All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brooker, P.G., Gomersall, S.R., King, N.A. et al. How do previously inactive individuals restructure their time to ‘fit in’ morning or evening exercise: a randomized controlled trial. J Behav Med 46, 429–439 (2023). https://doi.org/10.1007/s10865-022-00370-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-022-00370-x