Abstract
To overcome self-control difficulties, people can commit to their health goals by voluntarily accepting deadlines with consequences. In a commitment lottery, the winners are drawn from all participants, but can only claim their prize if they also attained their gym-attendance goals. In a 52-week, three-arm trial across six company gyms, we tested if commitment lotteries with behavioral economic underpinnings would promote physical activity among overweight adults. In previous work, we presented an effective 26-week intervention. In the present paper we analyzed maintenance of goal attainment at 52-week follow-up and the development of weight over time. We compared weight and goal attainment (gym attendance ≥ 2 per week) between three arms that—in the intervention period- consisted of (I) weekly short-term lotteries for 13 weeks; (II) the same short-term lotteries in combination with an additional long-term lottery after 26 weeks; and (III) a control arm without lottery-deadlines. After a successful 26-week intervention, goal attainment declined between weeks 27 and 52 in the long-term lottery arm, but remained higher than in the control group. Goal attainment did not differ between the short-term lottery arm and control arm. Weight declined slightly in all arms in the first 13 weeks of the trial and remained stable from there on. Commitment lotteries can support regular gym attendance up to 52 weeks, but more research is needed to achieve higher levels of maintenance and weight loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization has identified physical inactivity as the fourth leading risk factor for global mortality, accounting for 3.2 million deaths annually (Forouzanfar et al., 2016). While many people know that regular physical activity (PA) is beneficial for their health and can contribute to weight management (Hildebrandt et al., 2007), most Americans (79%) and Europeans (66%) do not meet recommended levels of PA (CDC, 2014; Lee et al., 2012; Eurobarometer, 2014). Besides, overweight and obese individuals generally exercise less than normal-weight individuals (CBS & RIVM, 2014) and the prevalence of obesity has more than doubled since 1980 (WHO, 2015): approximately 70% of Americans and 62% of Europeans are currently overweight or obese. Consequently, research in the field of health promotion has yielded numerous effective ways for people to change their health behaviors (Hoeymans et al., 2014). Still, most short-term interventions only have short-term effects (Van den Berg & Schoemaker, 2010). Although many people intend to improve their health by exercising on a regular basis for longer periods, the majority fails to follow through (Kooreman & Prast, 2010).
The progressing field of behavioral economics has identified systematic and predictable decision patterns that can explain why people make decisions that deviate from their own long-term health goals. Failures of self-control have been associated with present bias: the human tendency to disproportionally overweigh costs and benefits that are immediate (e.g., exercising vs. relaxing) over those that are delayed (e.g., good health in the future) (Ainslie, 1975; Laibson, 1997). Consequently, people often intend to exercise on a regular basis, but eventually attend their gym less frequently than they had planned to (DellaVigna & Malmendier, 2006; Schumacher et al., 2017). In the present work, we aimed to test whether some of the same decision-biases that contribute to unhealthy behaviors can be used to durably assist individuals who have trouble sticking to their PA goals.
There is increasing behavioral economic evidence for the notion that people who foresee their self-control troubles can benefit from -and are willing to use- interventions that are known as commitment devices (Bryan et al., 2010). Commitment devices are defined as voluntarily imposed arrangements that restrict future behavior to avoid temptation (Rogers et al., 2014). For example, people cut up their credit cards or embrace withdrawal penalties on their savings account to avoid overspending and undersaving in the future (Beshears et al., 2015; Bryan et al., 2010) or request nearby deadlines for their work to preempt procrastination (Ariely & Wertenbroch, 2002). Likewise, Dutch employees are happy with mandatory pension savings because they fear that otherwise they would not save enough for retirement (Van Rooij et al., 2007).
Psychologically grounded commitment devices have also been tested as a tool to support health behavior change (Rogers et al., 2014). Based on the principle that humans dislike losses more than they like gains of equal size (Kahneman & Tversky, 1979), individuals have agreed to forfeit their monetary deposits at voluntarily imposed deadlines if they do not quit smoking or fail to stick to their diet (Giné et al., 2010; Halpern et al., 2012; Volpp et al., 2008). Recently, lottery-based commitment devices have also been demonstrated to support weight loss, medication adherence and walking (Kimmel et al., 2012; Patel et al., 2016a, b; Volpp et al., 2008). The lotteries aimed to tap into the human tendency to avoid regret (Christy et al., 2016; Ferrer et al., 2012; Zeelenberg & Pieters, 2007) by only awarding prizes to lottery winners who attained their health goals and informing unsuccessful lottery winners on their forgone prizes.
For the present trial, we utilized previous psychological and behavioral economic knowledge to design lottery deadlines aimed at assisting overweight adults in attaining their weekly gym attendance goals. In our commitment lotteries we also used the guarantee of feedback by only awarding prizes to lottery winners who attained their attendance goals and informing unsuccessful lottery winners on their forgone prizes as a way to emphasize the deadlines.
As we presented in previous work (Van der Swaluw et al., 2018), in the current sample, 13 weekly lotteries (short-term lottery arm) supported regular gym attendance. After the 13 weekly lotteries, participants in our trial attended their gym considerably less. Adding an additional long-term lottery deadline after 26 weeks (long-term lottery arm) partly averted the decline in gym attendance, indicating that a long-term lottery deadline can help sustain regular gym attendance up to 13 additional weeks. The adjusted probability of goal attainment (week-gym attendance ≥ 2) in weeks 1–13 was 57% in the short-term lottery arm, 66% in the long-term lottery arm and 25% in the control arm. In both lottery arms, 8 out of the 13 weekly winners were eligible for their prize. Between weeks 14–26, the probability of week-goal attainment was highest in the long-term lottery arm (51%) versus 23% in the other arms. The majority of participants (55%) in the long-term lottery arm was eligible to claim the prize in week 26 if they would have won it.
For the present paper, we analyzed gym attendance after all lotteries ended.
Although there is evidence that commitment devices (e.g., voluntary imposed deadlines with consequences) in the health domain are effective in the short-run, the long-term effects are often unsatisfactory (John et al., 2011; Patel et al., 2016a, b; Royer et al., 2012). Consequently, one of the key challenges in the application of commitment devices is either safeguarding maintenance of behavior change after an intervention or continuing its application (Halpern et al., 2012; Rogers et al., 2014). We focused on the former and with this purpose we examined individual goal attainment (week-gym attendance ≥ 2) after the interventions.
After all deadlines had passed, gym attendance was monitored up to week 52 in all arms to examine maintenance of behavior change. Specifically, we questioned whether goal attainment differed between the long-term lottery arm, the short-term lottery arm and the control arm between weeks 27 and 52. We hypothesized that goal attainment in the lottery arms would decline between weeks 27 and 52, but still be significantly higher than goal attainment in the control arm and would be highest in the long-term lottery arm (Van der Swaluw et al., 2016).
We additionally studied weight patterns over the course of the trial. Next to –among others– genetic, sociocultural, economic and environmental factors, modifiable behaviors (diet and PA) markedly contribute to the development of overweight and obesity (Bray et al., 2016). As such, regular PA can contribute to weight loss and weight management (Fogelholm, 2010; Fogelholm & Kukkonen-Harjula, 2000). Furthermore, overweight has been associated with self-control problems (Ikeda et al., 2010; Schlam et al., 2013), while commitment lotteries aim to combat this. Hence, we also explored the effect of the interventions on the development of weight over the 52 weeks of this trial.
Method
Interventions
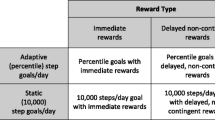
We compared two intervention arms to a control arm. Participants in all arms set the goal to exercise twice per week. Participation was free of charge and all participants were offered monthly statistics on their progress. The control arm was also actively monitored, but was neither aware of- nor participated in the lotteries. In all arms, participants were supervised as usual by the gym staff and were free to choose their preferred mode of exercise. All gyms were equipped to facilitate endurance training, strength training and standardized group classes (e.g., circuit training). As a normal part of the gym membership, participants had access to a variety of ready-to-use training schedules that fit different exercise goals (e.g., weight loss vs. enhancing stamina).
Short-term lottery arm
Participants in the short-term lottery arm participated in 13 weekly lotteries worth €100 each of the first 13 weeks of the trial. The weekly winners were randomly drawn out of all participants in this arm and were communicated to all by email and text message. The weekly winners were only eligible for their prize if they attended their gym at least twice that week (the week goal). Of key importance was also that lottery winners who did not attain their goal were informed about their forfeited prize. If a participant won one of the weekly lotteries, but did not attain the week goal in that week, it was communicated that “you won the lottery this week, but cannot claim your prize since you did not meet your goal of attending the gym twice”. Participants were fully informed and reminded about the possibility of this counterfactual feedback and the course of the lotteries. All other candidates in this arm were informed whether the prize was granted or forfeited. In each of the 13 weeks, the winner was drawn out of all participants regardless of prior performance. Thus, every new week meant a renewal of the commitment to exercise twice a week.
Long-term lottery arm
The first 13 weeks in the long-term lottery arm were identical to the short-term lottery arm. Participants knew prior to the trial that weeks 14–26 would also be part of the intervention. After 26 weeks a luxury family-vacation voucher was ascribed to a randomly drawn participant in this arm. Again, the winner was communicated to all participants by email and text message. Participants knew and were reminded that they would always learn the outcome of the lottery, but that the prize could only be claimed if the winner had attained his or her goal in at least 9 of the second 13 weeks (70% between weeks 14 and 26). We guaranteed that the prize would eventually be awarded: if the winner was not eligible for the prize, he or she would be informed of the forgone prize and another winner would be drawn until the prize could be awarded according to the rules mentioned above.
Design and setting
The study design and details on randomization, blinding, eligibility, recruitment and measurement protocols have been published before (Van der Swaluw et al., 2016). In brief, we set up a three-arm, parallel group, cluster randomized trial running for 52 weeks with 163 participants in six company gyms (clusters) across the Netherlands. Figure 1 displays the trial flow over 52 weeks. The gyms were branches of international fitness agency High Five, which provides corporate fitness training in 36 organizations across the Netherlands. The trial was reviewed and approved by the Tilburg University Ethical Review Board (EC-2014.42a) and is registered in the Dutch Trial Register (NTR5559). The lottery drawings were performed by the independent Game Management Department of the Dutch State Lottery under supervision of a notary.
The six gyms were randomized to one of three arms. As such, every arm contained two gyms. Participants were eligible if they expressed in a survey their goal to exercise twice or more per week, were between the ages of 18–65, were overweight (25 ≤ BMI < 40) and had not planned a leave of absence of more than 4 weeks in the first 26 weeks of the trial. Participants were blinded from the other trial arms. Informed consent was obtained from all individual participants included in the study. Table 1 displays the baseline data of participants in all three arms.
Outcomes and measures
Of primary interest in this trial was goal-attainment (week-gym attendance ≥ 2) measured at the participant level. We provided all gyms with an iPad connected via Wi-Fi, which allowed us to monitor attendance in real time. Throughout the 52 weeks of the trial, participants were required to check in at the iPad with their name or three digit study-ID when entering their gym. All gyms were provided with identical scales to measure weight (KERN™; 0.1% precision). Upon registering their attendance, participants were asked to weigh (without shoes) and to enter their weight (kilograms, 1 decimal) into the iPad. Participants could also select the option; “I already entered my weight this week”, or “I will enter my weight later this week”. Hence, weight was assessed on a weekly basis. At baseline, 13-, 26- and 52 weeks, participants were supervised by the gym personnel in entering their weight. Baseline attendance levels and demographics were assessed via an additional online questionnaire.
Analyses
Participants were the primary unit of inference in all analyses. Analyses followed the intention-to-treat principle and were conducted in R version 3.4.0 with statistical significance set at p < 0.05. Planned analyses can also be found in the trial protocol (Van der Swaluw et al., 2016).
To evaluate the effect of the interventions on goal attainment per week, we performed three multi-level logistic regression analyses with goal attainment from weeks 1–13, 14–26, and 27–52 as the dependent variable respectively. These measurements are nested within participants who are clustered within gyms. The three trial-arms, time, self-reported baseline attendance, age and sex were entered as fixed effects. Random intercepts were added for both the participants and the gyms. A random slope for time on the participant level was also included in the model and hereby allowed for different time patterns among individuals. Week 42 of the trial was excluded from the analyses, because gyms were closed in that week as a result of the new-year holiday season.
When there are few gyms per arm, treatment effects may correlate with intra cluster (gym) effects. By adding the random intercept for gyms, the model estimated the treatment effects, while accounting for the clustered data pattern in gyms. Additionally, sensitivity analyses were performed by excluding each gym from the models once and comparing effects of the reduced data models to the full model.
To assess the effect of the interventions on weight in each trial-period, multi-level linear regression analyses were performed with weight (kilograms) as the dependent variable. Linear multi-level modelling has shown to be a reliable technique to handle missing longitudinal outcome data (Peters et al., 2012) and was used to fit weight patterns over time, despite missing outcome measurements of participants who did not enter their weight that week. As before, these measurements are nested within participants who are clustered within gyms. Again, random intercepts were added for both the participants and the gyms. A random slope on the participant level was also added. The three trial-arms, time, baseline BMI, age and sex were included in all models as fixed effects.
Results
Goal attainment
Figure 2 displays percentages of goal attainment per arm per week. Results on goal-attainment in the first 26 weeks of the trial have been presented before (Van der Swaluw et al., 2018). Between weeks 27- 52, the aggregated percentage of goal attainment was 24% in the long-term lottery arm and 16 and 15% in the short-term arm and control arm respectively. Table 2 displays the time-adjusted odds ratios of goal attainment in each trial period.
In the logistic mixed model fitting weekly goal attainment between weeks 27–52, the long-term lottery arm had significantly higher odds of goal attainment than the control arm (OR 7.88, 95% CI 1.18–52.51, p = 0.03) and non-significant higher odds than the short-term lottery arm (OR 4.31, 95% CI 0.83–22.36, p = 0.08). The difference in goal attainment between the short-term lottery arm and the control arm was not statistically significant (OR 1.84, 95% CI 0.30–11.54, p = 0.15).
Sensitivity analyses
The intervention effect between weeks 27 and 52 was only sensitive to the sequential exclusion of control gyms from the models. If we excluded the best performing gym from the control arm, the intervention effect of the short-term lottery arm became statistically significant. If we excluded the least performing gym from the control arm, the effect of the long-term lottery arm remained qualitatively similar, but was no longer statistically significant.
Weight
Table 3 displays the output of the linear mixed models describing weight in each trial period. In the first 13 weeks of the trial, weight declined slightly over time in the control arm (B: − 0.09, SE: 0.03, p = 0.002), the short-term lottery arm (B: − 0.08, SE: 0.02, p = 0.001) and the long-term lottery arm (B: − 0.06, SE: 0.03, p = 0.02). The decline in weight did not differ between arms. Between weeks 14–26 and weeks 27–52, the models display neither a significant decline of weight over time, nor significant differences between arms.
Discussion
The 52-week follow-up analyses of our cluster randomized trial show moderately sustained levels of goal attainment (gym week-attendance ≥ 2) six months after completing a 26-week lottery intervention. Up to one year after the start of the intervention, participants who entered 13 weekly commitment lotteries (weeks 1–13), followed by an additional lottery 13 weeks later (weeks 14–26) were more likely to attend their gym twice per week than participants in the control arm. In the same follow-up period, goal attainment in the short-term lottery arm (13 weekly commitment lotteries) did not differ from the control arm or long-term lottery arm. Weight declined slightly in the first 13 weeks of the trial in all arms and remained stable from there on.
The present study may contribute to the pursuit of methods for sustainable behavior change. Commitment lotteries have been used relatively sporadically in the field of health promotion. Starting a decade ago, Volpp et al. (2008) have offered lotteries to overweight participants to support their weight loss attempts. While their lotteries were effective for 16 weeks, participants regained weight after the intervention. Likewise, Patel et al. (2016a, b) have effectively used team-based lotteries to stimulate walking for 13 weeks, but differences between intervention and control deteriorated during the 26-week follow-up period. Although there is evidence for their short-term effectiveness, the longevity of commitment lotteries is unsatisfactory. In the present trial, we observe a significantly higher likelihood of goal attainment in the long-term lottery arm than control in the six months after the intervention. The observation that the long-term lottery-arm does not underperform the control arm during follow-up implies that the 26-week intervention has had a net effect on gym attendance over a 1-year period.
Still, in the interpretation of our results, some nuance is warranted. In Fig. 2 it can be observed that levels of goal attainment in the long-term lottery arm dropped after the 26-week lottery deadline. Accordingly, average week-goal attainment in the long-term lottery arm halved during follow-up, relative to weeks 14–26. Therefore, it cannot be concluded that participants in the long-term lottery arm remained equivalently committed to their gym attendance goal as before. Similar to previous studies, behavior change is shown to be challenging to maintain after commitment lotteries end.
Nonetheless, the tested combination of short-term lotteries and a long-term lottery in this trial provides novel and useful insights that can be built upon in future trials to help optimize the long-term effectiveness of commitment lotteries. For example, for the winner to be eligible for the long-term lottery prize, he or she had to attain at least 9 week-goals between weeks 14–26. The majority of participants in the long-term lottery arm did so. Therefore, future studies can experiment by lengthening the long-term lottery deadline (e.g., to 36 weeks (John et al., (2011) to test if this will further stimulate sustained goal attainment. This exploration may result in a deadline that is nearby enough to be salient in the present, while being lengthy enough to promote sustained behavior change after the deadline.
Similar to previous research, behavioral economic and psychological insights on decision-making could be well incorporated in health promotion (Loewenstein et al., 2012). First, to leverage present bias (the overweighing of the present), we imposed nearby deadlines to draw the consequences of procrastination nearer (Ariely & Wertenbroch, 2002). Second, because people tend to overestimate small probabilities, a lottery is an effective and scalable tool to make missing the deadlines potentially costly for participants (Kahneman & Tversky, 1979). Third, we leveraged the human tendency to avoid regret by drawing the lottery prize from all participants and informing non-eligible winners on their forgone prize (Zeelenberg & Pieters, 2004, 2007). Fourth, while we aimed to stimulate long-term behavior change, we used week-goals to fit individuals’ impatience and to facilitate the human tendency of using of temporal landmarks (e.g., Mondays) to relegate misfortune to the past and have a fresh start (Dai et al., 2014; O’Donoghue & Rabin, 1999).
The results of this trial also offer several practical insights for health professionals, policy makers, insurers or employers who aim to support people in achieving their health goals. Next to its effectiveness, the costs of prevention are considered a key aspect in the determination of its value to businesses and society (Van den Berg & Schoemaker, 2010). The use of psychological and behavioral economic insights in the design of the lotteries can enhance the psychological impact of money that is spent and could offer the opportunity to implement commitment lotteries at low costs. To stimulate regular gym attendance up to 52 weeks in the long-term lottery arm, we spent only €2.21 per participant per week (awarded prizes ÷ participants ÷ weeks). In perspective; this is 0.6% of the Dutch minimum week-wage (€361.25). The costs in future applications may be further reduced if participants are also willing to pay for their wish to commit, similar to self-imposed withdrawal penalties on savings accounts (Beshears et al., 2015) or betting one’s money on personal health goals with a deposit contract (Halpern et al., 2012). It would be valuable to explore the characteristics of participants and potential organizers of commitment lotteries that contribute to the optimal balance between attractiveness and effectiveness.
Despite their potential, commitment devices remain underused (Halpern et al., 2012; Rogers et al., 2014)- a fact that might be explained by the range of open issues on their implementation. For example, employees or patients outside the interventions may resent others receiving lottery prizes (Loewenstein et al., 2012) (which may also be circumvented by asking participants to pay for lottery tickets). Besides, commitment lotteries were especially effective while they were active and -analogous to drugs- lost most of their effectiveness once people stopped ‘taking them’. This finding stimulates thinking about the type of commitment device that maintains its impact over repeated (and possibly infinite) application. While goal attainment declined over time in our trial (see Fig. 2), the decline of goal attainment over time did not differ significantly between the lottery arms and the control arm. Therefore, it would be interesting to design and test similar commitment lotteries that, like many commercial lotteries, are endlessly repeated and accessible.
Another issue surrounding the applicability of commitment lotteries is their target population. The majority of our sample was male (69.3%), which was similar to the general population of the six gyms (69.8% male). Nonetheless, future studies would benefit from enrolling an even proportion of females and males. A meta-analysis by Haff et al. (2015) that compared the effectiveness of several commitment lotteries between demographic groups found no gender differences, nor differences in education or broad ranges of income (except a slight reduced effect with incomes > $87.500). In previous analyses, we also observed no differences in intervention-effectiveness between income- or education categories (Van der Swaluw et al., 2018). This may be an indication of commitment lotteries being broadly applicable. A next step in the development of commitment devices could be the assessment of design features that contribute to their efficacy and feasibility across different populations. Hence, although there is increasing evidence for the effectiveness of commitment lotteries, more applied research could enhance their wide-spread practicability.
Commitment lotteries aimed at promoting regular PA did not result in substantial weight loss. After a moderate decline in weeks 1–13, weight remained stable over time in all arms, which is contrary to projections of overweight and obesity progressing over time (Wang et al., 2008). Considering that medical complications and associated health care costs rise progressively as BMI increases (Cawley & Meyerhoefer, 2012), stable weight is not all bad. Nonetheless, no meaningful weight loss was achieved as a result of increased PA, meaning that most participants remained exposed to the increased risks of cardiovascular diseases, diabetes type 2 and cancers that are associated with overweight and obesity (Forouzanfar et al., 2016; WHO, 2013). Our findings are in line with the general conception that regular exercise can contribute to weight loss but often not solely (Fogelholm, 2010; Fogelholm & Kukkonen-Harjula, 2000). In some occasions, increases in PA have also been found to result in weight gain by calorie compensation (McCaig et al., 2016).
To achieve significant and sustained weight loss, regular PA is only one part of the multicomponent (lifestyle training, nutrition and PA) interventions that are acknowledged to be effective (Bray et al., 2016). Still, weight loss interventions that include an exercise component are often more effective than interventions that do not (de Roon et al., 2017; Jeffery et al., 2003). Given that overweight individuals generally exercise less than normal weight individuals (CBS & RIVM, 2014), any multicomponent weight loss intervention that also encompasses PA might still benefit from including commitment lotteries for PA.
This trial is subject to several limitations. First, while it is clear that commitment lotteries did not promote meaningful weight loss, it remains unclear why this was the case in this trial (e.g., due to the type of exercise, calorie compensation, loss of fat that may have been compensated by increased muscle mass). We chose to focus on gym attendance as our main dependent variable, rather than weight loss, because this is under more direct volitional control by the participants. In future instances, it may be valuable to explore the need for additional weight loss guidance when participants enter commitment lotteries for PA. A second limitation is that our trial limited the promotion of regular PA to gym attendance, while activities with lower intensity (e.g., walking and recreational cycling) are also known to promote health outcomes (Fogelholm, 2010). The benefit of our approach is the novel and scalable context in which commitment lotteries were shown to be effective (company gyms), while exercise was supervised by the gym personnel. Third, our trial included no more than six gyms and randomization at the gym level increased the potential influence of intra gym effects in the effectiveness of the interventions. The sensitivity analysis (where we excluded the best performing control-gym from the model) reduced the sustained effect of the long-term lottery to non-significance. We accounted for intra-gym influences in our multi-level analyses and randomization at the gym level had the benefit that treatment contamination was minimized. Still, future studies can potentially avoid these issues by enrolling more gyms.
Conclusion
Regular PA has numerous health benefits. While many people aim to exercise on a regular basis, there are multiple predictable behavioral patterns that hamper the progression of a health-intention to sustained behavior. Effective and scalable support of long-term regular exercise is needed. Commitment lotteries that were designed to leverage psychological knowledge on decision-making can help cope with the challenges of health behavior change at low costs. While the 26-week intervention supported regular PA up to 52 weeks, levels of gym attendance declined after all deadlines had passed. Participants did not remain equivalently committed as before the long-term lottery deadline. Future research in broader populations could reveal to what degree commitment lotteries remain effective over longer time periods or if they are endlessly accessible.
References
Ainslie, G. (1975). Specious reward: a behavioral theory of impulsiveness and impulse control. Psychological Bulletin, 82(4), 463.
Ariely, D., & Wertenbroch, K. (2002). Procrastination, deadlines, and performance: self-control by precommitment. Psychological Science, 13(3), 219–224.
Beshears, J., Choi, J. J., Harris, C., Laibson, D., Madrian, B. C., & Sakong, J. (2015). Self control and commitment: can decreasing the liquidity of a savings account increase deposits? National Bureau of Economic Research, w21474, 1–53.
Bray, G. A., Fruhbeck, G., Ryan, D. H., & Wilding, J. P. (2016). Management of obesity. The Lancet, 387(10031), 1947–1956.
Bryan, G., Karlan, D., & Nelson, S. (2010). Commitment devices. Annual Review of Economics., 2(1), 671–698.
Cawley, J., & Meyerhoefer, C. (2012). The medical care costs of obesity: an instrumental variables approach. Journal of Health Economics, 31(1), 219–230.
CBS & RIVM. (2014). Gezondheidsenquête/Leefstijlmonitor. Retrieved from statline.cbs.nl
Centers for Disease Control and Prevention, Division of Nutrition, P. A., and Obesity. (2014). Facts about Physical Activity. Retrieved from https://www.cdc.gov/physicalactivity/data/facts.htm
Christy, S. M., Winger, J. G., Raffanello, E. W., Halpern, L. F., Danoff-Burg, S., & Mosher, C. E. (2016). The role of anticipated regret and health beliefs in HPV vaccination intentions among young adults. Journal of Behavioral Medicine, 39(3), 429–440.
Dai, H., Milkman, K. L., & Riis, J. (2014). The fresh start effect: Temporal landmarks motivate aspirational behavior. Management Science, 60(10), 2563–2582.
de Roon, M., van Gemert, W. A., Peeters, P. H., Schuit, A. J., & Monninkhof, E. M. (2017). Long-term effects of a weight loss intervention with or without exercise component in postmenopausal women: A randomized trial. Preventive Medicine Reports, 5, 118–123.
DellaVigna, S., & Malmendier, U. (2006). Paying not to go to the gym. The American Economic Review, 96, 694–719.
Ferrer, R. A., Klein, W. M. P., Zajac, L. E., Land, S. R., & Ling, B. S. (2012). An affective booster moderates the effect of gain- and loss-framed messages on behavioral intentions for colorectal cancer screening. Journal of Behavioral Medicine, 35(4), 452–461.
Fogelholm, M. (2010). Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obesity Reviews, 11(3), 202–221.
Fogelholm, M., & Kukkonen-Harjula, K. (2000). Does physical activity prevent weight gain – a systematic review. Obesity Reviews, 1(2), 95–111.
Forouzanfar, M. H., Afshin, A., Alexander, L. T., Anderson, H. R., Bhutta, Z. A., Biryukov, S., et al. (2016). Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet, 388(10053), 1659.
Giné, X., Karlan, D., & Zinman, J. (2010). Put your money where your butt is: a commitment contract for smoking cessation. American Economic Journal: Applied Economics, 2, 213–235.
Haff, N., Patel, M. S., Lim, R., Zhu, J., Troxel, A. B., Asch, D. A., et al. (2015). The role of behavioral economic incentive design and demographic characteristics in financial incentive-based approaches to changing health behaviors: a meta-analysis. American Journal of Health Promotion, 29(5), 314–323.
Halpern, S. D., Asch, D. A., & Volpp, K. G. (2012). Commitment contracts as a way to health. BMJ. British Medical Journal, 344(1), e522–e522.
Hildebrandt, V. H., Ooijendijk, W. T. M., & Hopman-Rock, M. (2007). Trendrapport bewegen en gezondheid 2004/2005: TNO.
Hoeymans, N., Van Loon, A., Van den Berg, M., Harbers, M., Hilderink, H., Van Oers, J., & Schoemaker, C. (2014). Een gezonder Nederland: Volksgezondheid Toekomst Verkenning 2014: RIVM.
Ikeda, S., Kang, M.-I., & Ohtake, F. (2010). Hyperbolic discounting, the sign effect, and the body mass index. Journal of Health Economics, 29(2), 268–284.
Jeffery, R. W., Wing, R. R., Sherwood, N. E., & Tate, D. F. (2003). Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? The American Journal of Clinical Nutrition, 78(4), 684–689.
John, L., Loewenstein, G., Troxel, A., Norton, L., Fassbender, J., & Volpp, K. (2011). Financial Incentives for Extended Weight Loss: A Randomized, Controlled Trial. Journal of General Internal Medicine, 26(6), 621–626.
Kahneman, D., & Tversky, A. (1979). Prospect theory: An analysis of decision under risk. Econometrica: Journal of the Econometric Society, 47(2), 263–291.
Kimmel, S. E., Troxel, A. B., Loewenstein, G., Brensinger, C. M., Jaskowiak, J., Doshi, J. A., et al. (2012). Randomized trial of lottery-based incentives to improve warfarin adherence. American Heart Journal, 164(2), 268–274.
Kooreman, P., & Prast, H. (2010). What Does Behavioral Economics Mean for Policy? Challenges to Savings and Health Policies in the Netherlands. De Economist, 158(2), 101–122.
Laibson, D. (1997). Golden eggs and hyperbolic discounting. Quarterly Journal of Economics, 112(2), 443–477.
Lee, I. M., Shiroma, E. J., Lobelo, F., Puska, P., Blair, S. N., & Katzmarzyk, P. T. (2012). Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet, 380, 219–229.
Loewenstein, G., Asch, D. A., Friedman, J. Y., Melichar, L. A., & Volpp, K. G. (2012). Can behavioural economics make us healthier? BMJ: British Medical Journal (Online), 344.
McCaig, D. C., Hawkins, L. A., & Rogers, P. J. (2016). Licence to eat: Information on energy expended during exercise affects subsequent energy intake. Appetite, 107, 323–329.
O’Donoghue, T., & Rabin, M. (1999). Doing it now or later. American Economic Review, 89(1), 103–124.
Patel, M. S., Asch, D. A., Rosin, R., Small, D. S., Bellamy, S. L., Eberbach, K., et al. (2016a). Individual versus team-based financial incentives to increase physical activity: A randomized, controlled trial. Journal of General Internal Medicine, 31, 1–9.
Patel, M. S., Asch, D. A., Roy Rosin, M., Small, D. S., Bellamy, S. L., Heuer, J., et al. (2016b). b. Framing Financial Incentives To Increase Physical Activity Among Overweight And Obese Adults. Annals of Internal Medicine, 164(6), 385–394.
Peters, S. A. E., Bots, M. L., den Ruijter, H. M., Palmer, M. K., Grobbee, D. E., Crouse, J. R., et al. (2012). Multiple imputation of missing repeated outcome measurements did not add to linear mixed-effects models. Journal of Clinical Epidemiology, 65(6), 686–695.
Rogers, T., Milkman, K. L., & Volpp, K. G. (2014). Commitment devices: Using initiatives to change behavior. JAMA, 311(20), 2065–2066.
Royer, H., Stehr, M. F., & Sydnor, J. R. (2012). Incentives, commitments and habit formation in exercise: Evidence from a field experiment with workers at a fortune-500 company. National Bureau of Economic Research., 7, 51–84.
Schlam, T. R., Wilson, N. L., Shoda, Y., Mischel, W., & Ayduk, O. (2013). Preschoolers’ Delay of Gratification Predicts their Body Mass 30 Years Later. The Journal of Pediatrics, 162(1), 90–93.
Schumacher, L. M., Arigo, D., & Thomas, C. (2017). Understanding physical activity lapses among women: responses to lapses and the potential buffering effect of social support. Journal of Behavioral Medicine, 40(5), 740–749.
Strategy, Corporate Communication Actions and Eurobarometer Unit (2014). Sport and physical activity. Special Eurobarometer 412.
Van den Berg, M. & Schoemaker, C.G. (2010). Effecten van preventie. Deelrapport van de VTV 2010 Van gezond naar beter: Rijksinstituut voor Volksgezondheid en Milieu.
Van der Swaluw, K., Lambooij, M. S., Mathijssen, J. J. P., Schipper, M., Zeelenberg, M., Berkhout, S., et al. (2018). Commitment lotteries promote physical activity among overweight adults: a cluster randomized trial. Annals of Behavioral Medicine: In press.
Van der Swaluw, K., Lambooij, M. S., Mathijssen, J. J. P., Schipper, M., Zeelenberg, M., Polder, J. J., et al. (2016). Design and protocol of the weight loss lottery- a cluster randomized trial. Contemporary Clinical Trials, 49, 109–115.
Van Rooij, M. C., Kool, C. J., & Prast, H. M. (2007). Risk-return preferences in the pension domain: are people able to choose? Journal of Public Economics, 91(3), 701–722.
Volpp, K. G., John, L. K., Troxel, A. B., Norton, L., Fassbender, J., & Loewenstein, G. (2008). Financial incentive–based approaches for weight loss: A randomized trial. JAMA, 300(22), 2631–2637.
Wang, Y., Beydoun, M. A., Liang, L., Caballero, B., & Kumanyika, S. K. (2008). Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity, 16(10), 2323–2330.
World Health Organization (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020.
World Health Organization (2015). Global Health Observatory data repository. Retrieved from http://apps.who.int/gho/data/node.main.A897A?lang=en
Zeelenberg, M., & Pieters, R. (2004). Consequences of regret aversion in real life: The case of the Dutch postcode lottery. Organizational Behavior and Human Decision Processes, 93(2), 155–168.
Zeelenberg, M., & Pieters, R. (2007). A theory of regret regulation 1.0. Journal of Consumer Psychology, 17(1), 3–18.
Acknowledgements
This study was funded by the Strategic Program of the National Institute for Public Health and Environment (Grant Number S13300101WL). We thank High Five Health Promotion and the Dutch State Lottery for their comprehensive cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics and data statement
The material in the manuscript has been acquired according to modern ethical standards and has been approved by the legally appropriate ethical committee. The article does not contain material copied from anyone else and all material which derives from prior work, including from the same authors, is properly attributed to the prior publication by proper citation. The datasets generated and analyzed during the current study are not publicly available due to national privacy laws and according medical ethical considerations. The data is stored in accordance with the Tilburg University data management policy and is subjected to periodic scientific audits.
Conflict of interest
Koen van der Swaluw, Mattijs S. Lambooij, Jolanda J.P. Mathijssen, Maarten Schipper, Marcel Zee-lenberg, Stef Berkhout, Johan J. Polder and Henriëtte M. Prast declare that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
van der Swaluw, K., Lambooij, M.S., Mathijssen, J.J.P. et al. Physical activity after commitment lotteries: examining long-term results in a cluster randomized trial. J Behav Med 41, 483–493 (2018). https://doi.org/10.1007/s10865-018-9915-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-018-9915-x