Abstract
Although depressive symptoms have been linked to stroke, most research has been in relatively ethnically homogeneous, predominantly white, samples. Using the United States based Health and Retirement Study, we compared the relationships between elevated depressive symptoms and incident first stroke for Hispanic, black, or white/other participants (N = 18,648) and estimated the corresponding Population Attributable Fractions. The prevalence of elevated depressive symptoms was higher in blacks (27%) and Hispanics (33%) than whites/others (18%). Elevated depressive symptoms prospectively predicted stroke risk in the whites/other group (HR = 1.53; 95% CI: 1.36–1.73) and among blacks (HR = 1.31; 95% CI: 1.05–1.65). The HR was similar but only marginally statistically significant among Hispanics (HR = 1.33; 95% CI: 0.92–1.91). The Population Attributable Fraction, indicating the percent of first strokes that would be prevented if the incident stroke rate in those with elevated depressive symptoms was the same as the rate for those without depressive symptoms, was 8.3% for whites/others, 7.8% for blacks, and 10.3% for Hispanics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Stroke is the third leading cause of death in the United States (US), and a leading cause of major disability (Roger et al., 2011). Depressive symptoms have been shown to predict stroke onset, but little of this research has been conducted in African-American or American Hispanic populations (Bos et al., 2008; Glymour et al., 2010; Jonas & Mussolino, 2000; Larson et al., 2001; Ohira et al., 2001a, b; Ostir et al., 2001; Salaycik et al., 2007; Simons et al., 1998; Surtees et al., 2008). The relationship between depressive symptoms and stroke may differ for whites compared to racial/ethnic minorities, because of divergent medical, behavioral, or social responses to depressive symptoms or differential prevalence of other cardiovascular risk factors. Understanding the relationship between depressive symptoms and stroke in racial/ethnic minorities is especially important because of evidence that depression is undertreated in minorities (Alegría et al., 2008), potentially contributing to the heavy burden of stroke.
Racial and ethnic disparities in stroke
Although case-fatality rates have declined in recent years, reductions in stroke incidence rates remain an important population health goal (Roger et al., 2011). Identifying modifiable risk factors for stroke is especially important for addressing racial and ethnic disparities. In the US, current evidence suggests that strokes occur at higher incidence, at younger ages, and result in greater disability in both African-American and Hispanic populations compared to whites (Cooper et al., 2000; King & Williams, 1995; Trimble & Morgenstern, 2008). Among individuals ages 45–64 years, the stroke mortality rate for African Americans is 3–4 times higher than for whites, with a decreasing black-to-white mortality ratio with increasing age (Howard et al., 2007; King & Williams, 1995). The limited population-based incidence data available show stroke incidence rates in blacks that are more than double those for whites living in the same geographic region, including northern Manhattan in New York City or Greater Cincinnati in Ohio/Northern Kentucky (Kissela et al., 2004; Sacco et al., 1998). Stroke in US Hispanic populations has rarely been studied in cohorts, however, registry studies suggest a higher burden of disease compared to whites (Morgenstern et al., 2004; Sacco, et al., 1998). Further, some evidence suggests that both the impact and prevalence of stroke risk factors may differ for racial/ethnic minorities (Sacco et al., 2001), although there is substantial overlap of major risk factors (Smith et al., 2003). These findings suggest that associations established in primarily white samples may not adequately generalize and it is therefore critical to examine stroke risk factors in racial and ethnic minority populations. This concern is all the more relevant for psychologically mediated stroke risk factors, such as depression and related conditions.
Racial and ethnic patterns in depressive symptoms
Prior research is inconsistent with respect to the prevalence of depression in racial/ethnic minorities compared to whites, with some but not all studies finding lower prevalence of mood disorders in minorities (Alegría et al., 2008; Blazer et al., 1998; Kessler et al., 2005). Other research suggests racial and ethnic patterns observed in younger samples do not hold in the elderly and older Latinos in particular experience elevated prevalence of dysthymia and depression (Alegría et al., 2008; Jimenez et al., 2010). The divergent evidence may arise in part because of differences in expression of symptoms across populations (Das et al., 2006; Lewis-Fernandez et al., 2005). Evidence is more consistent that racial/ethnic minorities experience lower rates of depression treatment and higher chronicity of major depression (Alegría et al., 2008; Minsky et al. 2003; Simpson et al., 2007; Williams et al., 2007).
The evidence gap for depressive symptoms and stroke in racial/ethnic minorities
The prospective association between depressive symptoms and stroke incidence, although relatively well established in white populations, has rarely been examined in racial/ethnic minorities. To date, very few large scale studies have collected stroke data on multiple racial/ethnic groups within the same community or population. In the National Health and Nutrition Examination Survey I Epidemiological Follow-up Study (NHEFS) depressive symptoms predicted stroke in both whites and blacks, and the association was slightly stronger in blacks (Jonas & Mussolino, 2000). Similarly, using data from the NHEFS, Jonas et al. found that the association between depression and hypertension was higher for blacks than whites (Jonas et al., 1997). In the North Carolina Established Populations for the Epidemiologic Study of the Elderly (EPESE), positive affect was associated with lower risk of stroke in both blacks and whites, with similar magnitude of association for both races (Ostir et al., 2001). To our knowledge, no prospective study has assessed whether the association between depressive symptoms and stroke is consistent in Hispanic populations. Given concerns about under-diagnosis of mood disorders in minorities, and the burden of disease related to stroke, it is important to assess whether depressive symptoms may be a major stroke risk factor in minority populations. Brief depressive symptom screens such as typically used in epidemiologic studies may fail to predict stroke in minorities either because they do not measure mood disorders well in these populations or because mood disorder, even if well-measured, would not predict stroke. On the other hand, depression may prove an important modifiable stroke risk factor that could be readily identified with brief assessments. Depressive symptoms are potentially treatable, so it also valuable to understand the possible population health impact of ameliorating depressive symptoms in racial/ethnic minority groups.
We hypothesized that elevated depressive symptoms would have a similar relationship with stroke in US non-Hispanic whites, non-Hispanic blacks, and Hispanic adults. We also estimated the fraction of incident strokes that could have been prevented if individuals with elevated depressive symptoms experienced the same stroke rate as individuals without elevated depressive symptoms (i.e., the population attributable fraction) in each racial/ethnic group.
Methods
Participants
We used data from three enrollment cohorts (1992, 1993, and 1998) of the Health and Retirement Study (HRS), a longitudinal biennial national survey of US adults aged 50 + and their spouses. Technical details of study design and implementation have been previously published elsewhere (Juster & Suzman, 1995). For the 1992 enrolment cohort, alternative versions of the depressive symptom assessment were used before 1996, so we defined 1996 interviews “baseline” for this cohort. Data from biennial interviews (or proxy interviews for decedents) through 2006 were used. We restricted our sample to HRS participants age 50 + at the time of enrolment, born after 1899, and who reported they had no prior stroke at baseline interview.
From 23,639 age-eligible respondents, 1,741 (7.4%) were excluded due to prior stroke. From these 21,898 potentially eligible participants, we further excluded 1,710 (7.8%) due to missing information on baseline depressive symptoms, 891 (4.1%) due to missing covariates, 599 (2.7%) due to missing follow-up information, and 50 (0.2%) due to unknown failure date. Of 4,991 excluded age-eligible respondents, 865 (17.3%) were non-Hispanic blacks, 464 (9.3%) were Hispanic, and 3,663 (73.4%) were white/other race/ethnicity.
The HRS is sponsored by the National Institute on Aging (grant NIA U01AG009740) and is conducted by the University of Michigan. The HRS is approved by the University of Michigan Health Sciences Human Subjects Committee and this study is approved by the Harvard School of Public Health Human Subjects Committee.
Measures of stroke
At each interview, participants were asked to report on stroke history (“Has a doctor ever told you that you had a stroke?”). For those participants who were deceased or unable to participate directly in the interview, proxies (usually spouses) were interviewed. A small number of respondents volunteered that they had experienced a Transient Ischemic Attack (TIA). Because TIAs were not assessed consistently in the survey, we classified these individuals as not having a history of stroke. Respondents reported stroke month and year; for events with unknown date (n = 302) we assigned the median month for events reported by others in the same interview wave.
Measures of depressive symptoms
Depressive symptoms were assessed with an 8-item version of the Centers for Epidemiologic Study of Depression (CES-D) scale. Respondents scored questions with yes/no responses (“Now think about the past week and the feelings you have experienced. Please tell me if each of the following was true for you much of the time this past week. Much of the time during the past week … I felt depressed/felt that everything I did was an effort/my sleep was restless/could not get going/felt lonely/enjoyed life/felt sad/was happy.”) Based on established standards, elevated depressive symptoms were defined as a score of 3+ (Steffick, 2000). It has been shown in a subsample of HRS participants (n = 6,133) who completed both the CES-D and a short form of the World Health Organization’s Composite International Diagnostic Interview (CIDI-SF) that the cutpoint of 3+ on the CES-D had 71% sensitivity and 79% specificity for identifying major depressive episode according to DSM-IV criteria as implemented by the CIDI-SF. These results are not available stratified by race/ethnicity. In the current analytic sample, the CES-D scale had a Cronbach’s alpha of 0.78 for whites, 0.82 for Hispanics and 0.78 for blacks, suggesting similar reliability for all three groups.
Measures of covariates
Race/ethnicity was self-reported and we considered three groups: Hispanic (n = 1,313), non-Hispanic black (n = 2,557), and white/other (n = 14,778; 93% white and 7% categorized as Not Specified). Additional core demographic covariates included age, Southern birth, father’s and mother’s education of 8+ years, and missing indicators for unknown parental education. Parent’s education and region of birth were controlled because they predict stroke and temporally precede participants’ current depressive status (Glymour et al., 2008). Adult social risk factors included as covariates were: years of education, household income and wealth at baseline (income and wealth were natural log transformed to reduce skew), and marital status (divorced/widowed/never-married/currently married). We then adjusted for a set of well-established stroke risk factors that may also be affected by prior depressive symptoms: smoking status (current/past/never), overweight (BMI 25–<30) or obese (BMI 30+), moderate alcohol use (<3/day or <18/week), or heavy alcohol use (≥3/day or ≥18/week), and self-reported baseline diagnoses of hypertension, diabetes, or heart disease. Because this set of covariates potentially includes mediators of the effect of depressive symptoms on stroke, the coefficients should not be interpreted as “causal.”
Analyses
We used Cox proportional hazard models to estimate the hazard ratio (HR) for onset of first stroke associated with elevated depressive symptoms. We first analyzed the association between endorsing each of the 8 depressive symptoms at baseline and subsequent hazard of incident stroke in models stratified by race/ethnicity. We next evaluated the association between elevated depressive symptoms (3+ symptoms) and onset of stroke in each racial/ethnic group. We tested the null hypothesis that the association between elevated depressive symptoms and stroke was the same for each racial/ethnic group by estimating a pooled model including interaction terms for baseline depressive symptoms by black and depressive symptoms by Hispanic. As a sensitivity analysis, we repeated the primary analyses using accelerated failure time models with a Weibull distribution, but results were very similar so we present the Cox models only. To illustrate how the association between depressive symptoms at baseline and stroke risk persists over time, we used logistic models to estimate smoothed survival curves adjusted for baseline demographic variables. These models included terms for months since baseline, months squared, and the interaction of baseline elevated depressive symptoms with months and months squared. We explored cubic models, but the cubic coefficients were estimated as 1.000 (i.e. null at the 3rd decimal place) and so we dropped them.
Finally, we estimated the Population Attributable Fraction using the formula:
where pc is fraction of exposed cases (Rothman et al., 2008). The Population Attributable Fraction calculation reflects the fact that the impact of a risk factor on population patterns of disease is influenced by both the hazard associated with the risk factor and the percent of the population exposed to the risk factor. If the association is causal, it is interpreted as the fraction of events that could be eliminated if the risk factor were eliminated from the population. Analyses were conducted using SAS 9.2.
Results
The primary analyses included 18,648 individuals (152,437 person-years) who experienced 1,998 first strokes (Table 1). The prevalence of elevated depressive symptoms was higher in Hispanics (33%) and blacks (27%) than in the white/other group (18%). Among Hispanics, no individual symptom was significantly related to onset of stroke, but “everything was an effort” and “couldn’t get going” had HRs above 1.4 (Table 2). For black respondents, 5 of the 8 symptoms had statistically significant relationships with stroke incidence, but neither “everything was an effort” nor the two positive emotions “enjoyed life” and “was happy” were significantly associated. Among whites, endorsement of any individual depressive symptom significantly predicted subsequent stroke onset. The magnitude of the relationship was strongest for “everything was an effort” and “felt depressed.”
The hazard ratio associated with 3+ elevated depressive symptoms was only marginally statistically significant (p < 0.10) among Hispanics [HR = 1.33 (95% CI: 0.92–1.91)]. The associations between elevated depressive symptoms and first stroke risk were of similar magnitude in whites/others [HR = 1.53 (95% CI: 1.36–1.73)], and in non-Hispanic blacks [HR = 1.31 (95% CI: 1.05–1.65)] (Table 3). Adjusting for adult social risk factors slightly attenuated the relationships for blacks and whites/others; elevated baseline depression predicted elevated stroke in whites/others [HR = 1.40 (95% CI: 1.24–1.58)], but hazard ratios were marginally significant for blacks [HR = 1.25 (95% CI: 0.99–1.58)] and Hispanics [HR = 1.36 (95% CI: 0.93–2.00)]. Additionally adjusting for well-established adult stroke risk factors, which may mediate the effect of depressive symptoms on stroke, further attenuated the associations, so that there was no evidence of an association between elevated depressive symptoms and stroke onset among Hispanics (HR = 0.99). However, the CIs from these models were quite wide and included the HR estimate for both blacks (HR = 1.12) and the white/other group (HR = 1.28). In models adjusted only for demographic covariates, interaction terms for race/ethnicity by elevated depressive symptoms were not statistically significant for blacks (p = 0.20) or Hispanics (p = 0.39), indicating no evidence of interaction (on a multiplicative scale) between elevated depressive symptoms and race.
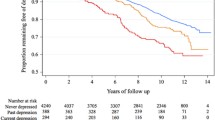
Predicted survival curves (Fig. 1) suggest that elevated depressive symptoms predicted higher risk of stroke for several years after the depression assessment was completed. For all three racial ethnic groups, the interactions between baseline depressive symptoms and time elapsed since assessment were very close to the null (not shown), indicating that the relationship between baseline depressive symptoms and stroke risk was similar across the entire follow-up period.
Smoothed survival curves by baseline elevated depressive symptoms, adjusted for demographic covariates (age at baseline, southern birth, mother’s and father’s education) with time-varying relationship between month of follow-up and baseline depressive symptoms. a Stroke-free survival among Hispanics. b Stroke-free survival among blacks. c Stroke-free survival among whites/others. Solid line: not elevated depressive symptoms at baseline, dashed line: elevated depressive symptoms at baseline
Based on the demographic-adjusted HRs and the prevalence of elevated depressive symptoms, the Population Attributable Fraction for elevated depressive symptoms and incident stroke was highest for Hispanics (10.3%) compared to the Population Attributable Fraction for whites/others (8.3%) or blacks (7.8%).
Discussion
In a large national study with over 8 years of average follow-up, we found that elevated depressive symptoms predicted stroke incidence in whites and blacks, and that hazard ratios were elevated but only marginally statistically significant for Hispanics. Hazard ratio point estimates for Hispanics were similar to those for blacks, although the p-values did not meet the conventional α < 0.05 criterion for statistical significance. However, this was likely due to reduced statistical power to detect an effect among Hispanics, given the smaller number of older Hispanics than older blacks.
Furthermore, the prevalence of elevated depressive symptoms was highest in Hispanics and lowest in whites. The Population Attributable Fraction is one gauge of the public health importance of an exposure, and reflects both the hazard associated with the exposure and the prevalence of the exposure. The Population Attributable Fraction for depression and incident stroke was quite high for all three groups, but highest among Hispanics because of the high prevalence of elevated depressive symptoms. Interpreting the Population Attributable Fraction depends on the assumption that the relationship between depressive symptoms and stroke is causal. If so, our results suggest that in this population of Hispanics, just over 10% of incident strokes could have been prevented by eliminating depressive symptoms or eliminating the stroke risk associated with depressive symptoms. This estimate should be interpreted cautiously because it is uncertain whether the effect of depressive symptoms on stroke is causal. To put the Population Attributable Fraction estimate in perspective, the American Heart Association/American Stroke Association Guidelines for the Primary Prevention of Stroke suggest a population attributable risk of 5–27% for diabetes and around 9% for high total cholesterol (Goldstein et al. 2011).
Although the association between prior depressive symptoms and stroke incidence has been demonstrated in several studies (Glymour et al., 2010; Jonas & Mussolino, 2000; May et al., 2002; Ohira et al., 2001a, b), only two studies have examined this association specifically among blacks (Jonas & Mussolino, 2000; Ostir, et al., 2001) and to our knowledge no prior study has examined depressive symptoms and stroke in Hispanics. Despite the long follow-up and national sample in NHEFS, that analysis included only 83 strokes among blacks (Jonas & Mussolino, 2000), compared to 334 in the current study. Our findings are largely consistent with the NHEFS results, although we found that the association between depressive symptoms and stroke was similar across all three racial/ethnic groups. Furthermore, the point estimates in our results were generally lower than the hazard ratio point estimates reported in NHEFS. This may be attributable to the older population in our sample and the focus on first (rather than any) stroke.
The single symptom analyses should be interpreted very cautiously. First, these analyses are not corrected for multiple comparisons. More importantly, the CES-D items were validated as a combined scale (Hertzog et al., 1990; Irwin et al., 1999; Radloff, 1977; Steffick, 2000), including studies in racial/ethnic minority populations (Mahard, 1988; Roberts, 1980). These validations generally focused on correspondence between CES-D and clinical syndromes such as major depression, rather than the association of CES-D with risk of future illness, as is our goal in the current analysis. Symptoms and expression of depression may vary across cultural groups (Alegría & McGuire, 2003; Brown et al., 1996; Li & Hicks, 2010; Steffens et al., 1997). For example, Uebelacker et al. report that symptoms of sleep disturbance were more discriminating for DSM-IV diagnosed major depressive disorder among non-Hispanic whites than Hispanics, but symptoms of fatigue were more discriminating among Hispanics (Uebelacker et al., 2009). Blazer reported a similar factor structure for CES-D among older whites and African-Americans, although, consistent with our results, he reported that African-Americans were significantly more likely to endorse the items “felt depressed”, “felt lonely”, and “everything was an effort” (Blazer, et al., 1998).
Our findings demonstrate that the CES-D, despite its brevity, is an important and useful measure of depressive symptomatology for both blacks and Hispanics, but our results also suggest some items may be better indicators of stroke risk. The original CES-D scale was found to have four domains: Depressive Affect, Somatic Symptoms, Well-Being, and Interpersonal Relations. The modified CES-D scale we use here has no items corresponding to Interpersonal Relations, but items corresponding to each of the other three domains. We found that the well-being symptoms were not as common as other depressive symptoms for any racial/ethnic group and did not significantly predict stroke for either blacks or Hispanics (although point estimates for well-being items among blacks were fairly high). This is in contrast to previous work showing that positive affect was associated with reduced risk of stroke in both African Americans and whites (Ostir et al., 2001). However, that research was based on a cohort that did not include Hispanics and so we cannot directly compare results to ours.
Given that we found good inter-item reliability of the 8-item scale for all three racial/ethnic groups, our findings support use of a combined scale in research. However, the marked difference in prevalence and apparent toxicity of certain symptoms, especially in Hispanics, suggests future research might explore domain-specific associations with health outcomes for each racial/ethnic group. These results may also be of interest in future work developing culturally appropriate depression screens.
The HRS has important strengths for this study, including a large, diverse sample drawn from across the United States and longitudinal follow-up of up to 13 years. However, HRS also has several limitations relevant in our analyses. Outcomes are based on self- or proxy-reports, without medical verification. Prior research suggests that self-reports of diagnoses of major acute medical events, such as stroke, are fairly accurate but not perfect. For example, a study of Olmsted County Minnesota reported a sensitivity of 78.4% and a specificity of 98.6% for prevalent self-reported stroke or TIA. This corresponds to a positive predictive value of 67%, which is fairly consistent with findings in other studies (Bots et al., 1996; Engstad et al., 2000), including the NHEFS (Bergmann et al., 1998). In previous analyses, we have found that well-documented cardiovascular risk factors have roughly similar associations with stroke in the HRS sample as found in other studies with medical-record verification (Glymour & Avendano, 2009), suggesting this is an appropriate data set for exploration of new risk factors.
An additional limitation of HRS is that stroke subtypes cannot be assessed. Prior research provides limited evidence that depressive symptoms increase risk of ischemic but not hemorrhagic stroke (Ohira et al., 2001a, b). Because most strokes in US populations are ischemic, our results are likely driven by the association between depressive symptoms and ischemic stroke. However, we cannot evaluate this supposition.
Most importantly, this study is observational and therefore cannot establish causality. We were not able to adjust for several potential common causes of depressive symptoms and stroke. There are many reasons to question the causal direction relating depressive symptoms and cerebrovascular disease (Williams, 2005). For example, several studies show that stroke increases risk of depression, and depressive symptoms may be a symptom of subclinical cerebrovascular disease that will ultimately manifest in clinical stroke (Wendell et al. 2010). The prospective design of our study helps address the possibility of reverse causation from cerebrovascular disease to depressive symptoms, as illustrated in the survival curves showing that baseline depressive symptoms predict stroke onset years later. If this association is entirely attributable to reverse causation, it suggests that subclinical CVD influences mood several years before manifesting as a stroke. It is important to evaluate this in future research because it implies apparently healthy individuals are experiencing neurological damage years before stroke diagnosis. The current analyses cannot conclusively establish the causal direction, however.
The typical interpretation of the Population Attributable Fraction is based on the assumption that the exposure is causally linked to the outcome. Because of the uncertainty regarding the causal direction, we have emphasized a more conservative interpretation of the Population Attributable Fraction, as the fraction of strokes that could have been eliminated if the exposed had the same stroke rate as the unexposed.
Much remains unknown about the relationship between depressive symptoms and stroke in the overall US population. Further research is needed to clarify if depressive symptoms connote equal level of risk for ischemic versus hemorrhagic stroke and for different stroke mechanisms.
The clinical importance of the depression-stroke link is highlighted by Population Attributable Fractions approaching 10%. Although prior estimates of the prevalence of depression in adult white and minority populations vary widely, (Alegría et al., 2008; Blazer et al., 1998; Ford et al., 2007; Jimenez et al., 2010; Kessler et al., 2005; Takeuchi et al., 2007) we found that elevated depressive symptoms were common in all three racial/ethnic groups, with the greatest prevalence among Hispanics.
We found that the association between elevated depressive symptoms and incidence of first stroke was similar in whites, blacks, and Hispanics, although confidence intervals included the null value for Hispanics. These findings add to the growing body of evidence that depression increases risk of stroke, and extends this relationship to black and Hispanic adults. Improved diagnosis and treatment of depression, particularly in elderly minorities, may help reduce stroke rates, although direct evidence on the cardiovascular effects of treatment is needed.
References
Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C., Takeuchi, D., et al. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59, 1264–1272.
Alegría, M., & McGuire, T. (2003). Rethinking a universal framework in the psychiatric symptom-disorder relationship. Journal of Health and Social Behavior, 44, 257–274.
Bergmann, M. M., Byers, T., Freedman, D. S., & Mokdad, A. (1998). Validity of self-reported diagnoses leading to hospitalization: A comparison of self-reports with hospital records in a prospective study of American adults. American Journal of Epidemiology, 147, 969–977.
Blazer, D., Landerman, L., Hays, J., Simonsick, E., & Saunders, W. (1998). Symptoms of depression among community-dwelling elderly African-American and white older adults. Psychological Medicine, 28, 1311–1320.
Bos, M. J., Linden, T., Koudstaal, P. J., Hofman, A., Skoog, I., Breteler, M. M. B., et al. (2008). Depressive symptoms and risk of stroke: The Rotterdam Study. Journal of Neurology and Neurosurgery Psychiatry, 79, 997–1001.
Bots, M. L., Looman, S. J., Koudstaal, P. J., Hofman, A., Hoes, A. W., & Grobbee, D. E. (1996). Prevalence of stroke in the general population: The Rotterdam study. Stroke, 27, 1499–1501.
Brown, C., Schulberg, H. C., & Madonia, M. J. (1996). Clinical presentations of major depression by African Americans and whites in primary medical care practice. Journal of Affective Disorders, 41, 181–191.
Cooper, R., Cutler, J., Desvigne-Nickens, P., Fortmann, S. P., Friedman, L., Havlik, R., et al. (2000). Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States—Findings of the National Conference on Cardiovascular Disease Prevention. Circulation, 102, 3137–3147.
Das, A. K., Olfson, M., McCurtis, H. L., & Weissman, M. M. (2006). Depression in African Americans: Breaking barriers to detection and treatment. Journal of Family Practice, 55, 30–39.
Engstad, T., Bonaa, K. H., & Viitanen, M. (2000). Validity of self-reported stroke—The Tromso study. Stroke, 31, 1602–1607.
Ford, B. C., Bullard, K. M., Taylor, R. J., Toler, A. K., Neighbors, H. W., & Jackson, J. S. (2007). Lifetime and 12-month prevalence of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition disorders among older African Americans: Findings from the national survey of American life. American Journal of Geriatric Psychiatry, 15, 652–659.
Glymour, M. M., & Avendano, M. (2009). Can self-reported strokes be used to study stroke incidence and risk factors? Evidence from the health and retirement study. Stroke, 40, 873–879.
Glymour, M. M., Avendaño, M., Haas, S. A., & Berkman, L. F. (2008). Lifecourse social conditions and racial disparities in incidence of first stroke. Annals of Epidemiology, 18, 904–912.
Glymour, M. M., Maselko, J. M., Gilman, S. E., Patton, K. K., & Avendano, M. (2010). Depressive symptoms predict incident stroke independently of memory impairments. Neurology, 75, 2063–2070.
Goldstein, L., Bushnell, C., Adams, R., Appel, L., Braun, L., Chaturvedi, S., et al. (2011). Guidelines for the primary prevention of stroke. A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 42, 517–584.
Hertzog, C., Van Alstine, J., Usala, P., Hultsch, D., & Dixon, R. (1990). Measurement properties of the Center for Epidemiological Studies Depression Scale (CES-D) in older populations. Psychological Assessment, 2, 64–72.
Howard, G., Labarthe, D. R., Hu, J., Yoon, S., & Howard, V. J. (2007). Regional differences in African Americans’ high risk for stroke: The remarkable burden of stroke for Southern African Americans. Annals of Epidemiology, 17, 689–696.
Irwin, M., Artin, K., & Oxman, M. (1999). Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Archives of Internal Medicine, 159, 1701–1704.
Jimenez, D. E., Alegría, M., Chen, C., Chan, D., & Laderman, M. (2010). Prevalence of psychiatric illnesses in older ethnic minority adults. Journal of the American Geriatrics Society, 58, 256–264.
Jonas, B. S., Franks, P., & Ingram, D. D. (1997). Are symptoms of anxiety and depression risk factors for hypertension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. [Article]. Archives of Family Medicine, 6, 43–49.
Jonas, B. S., & Mussolino, M. E. (2000). Symptoms of depression as a prospective risk factor for stroke. Psychosomatic Medicine, 62, 463–471.
Juster, F., & Suzman, R. (1995). An overview of the health and retirement study. Journal of Human Resources, 30, S7–S56.
Kessler, R., Berglund, P., Demler, O., Jin, R., Merikangas, K., & Walters, E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602.
King, G., & Williams, D. R. (1995). Race and health: A multidimensional approach to African American health. In B. C. Amick (Ed.), Society and health (pp. xvi, 374). New York, NY: Oxford University Press.
Kissela, B., Schneider, A., Kleindorfer, D., Khoury, J., Miller, R., Alwell, K., et al. (2004). Stroke in a biracial population the excess burden of stroke among blacks. Stroke, 35, 426–431.
Larson, S. L., Owens, P. L., Ford, D., & Eaton, W. (2001). Depressive disorder, dysthymia, and risk of stroke: Thirteen-year follow-up from the Baltimore epidemiologic catchment area study. Stroke, 32, 1979–1983.
Lewis-Fernandez, R., Das, A. K., Alfonso, C., Weissman, M. M., & Olfson, M. (2005). Depression in US Hispanics: Diagnostic and management considerations in family practice. The Journal of the American Board of Family Medicine, 18, 282–296.
Li, Z., & Hicks, M. H. (2010). The CES-D in Chinese American women: Construct validity, diagnostic validity for major depression, and cultural response bias. Psychiatry Research, 175, 227–232.
Mahard, R. E. (1988). The CES-D as a measure of depressive mood in the elderly Puerto Rican population. Journal of Gerontology, 43, 24–25.
May, M., McCarron, P., Stansfeld, S., Ben-Shlomo, Y., Gallacher, J., Yarnell, J., et al. (2002). Does psychological distress predict the risk of ischemic stroke and transient ischemic attack? The Caerphilly Study. Stroke, 33, 7–12.
Minsky, S., Vega, W., Miskimen, T., Gara, M., & Escobar, J. (2003). Diagnostic patterns in Latino, African American, and European American psychiatric patients. Archives of General Psychiatry, 60, 637–644.
Morgenstern, L., Smith, M., Lisabeth, L., Risser, J., Uchino, K., & Garcia, N. (2004). Excess stroke in Mexican Americans compared with non-Hispanic Whites. American Journal of Epidemiology, 160, 376–383.
Ohira, T., Iso, H., Satoh, S., Sankai, T., Tanigawa, T., & Ogawa, Y. (2001a). Prospective study of depressive symptoms and risk of stroke among Japanese. Stroke, 32, 903–907.
Ohira, T., Iso, H., Satoh, S., Sankai, T., Tanigawa, T., Ogawa, Y., et al. (2001b). prospective study of depressive symptoms and risk of stroke among Japanese editorial comment : Is depression a risk factor for ischemic stroke? Stroke, 32, 907–908.
Ostir, G. V., Markides, K. S., Peek, M. K., & Goodwin, J. S. (2001). The association between emotional well-being and the incidence of stroke in older adults. Psychosomatic Medicine, 63, 210–215.
Radloff, L. (1977). The CES-D scale: a self-report depression scale for research in the general population. Journal of Applied Psychological Measurement, 1, 385–401.
Roberts, R. E. (1980). Reliability of the CES-D Scale in different ethnic contexts. Psychiatry Research, 2, 125–134.
Roger, V. L., Go, A. S., Lloyd-Jones, D. M., Adams, R. J., Berry, J. D., Brown, T. M., et al. (2011). Heart Disease and Stroke Statistics 2011 Update: A report from the American Heart Association. Circulation, 123, e18–e209.
Rothman, K. J., Greenland, S., & Lash, T. L. (2008). Modern epidemiology (3rd ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Sacco, R. L., Boden-Albala, B., Abel, G., Lin, I. F., Elkind, M., Hauser, W. A., et al. (2001). Race-ethnic disparities in the impact of stroke risk factors—The Northern Manhattan Stroke Study. Stroke, 32, 1725–1731.
Sacco, R. L., Boden-Albala, B., Gan, R., Chen, X., Kargman, D. E., Shea, S., et al. (1998). Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. American Journal of Epidemiology, 147, 259–268.
Salaycik, K. J., Kelly-Hayes, M., Beiser, A., Nguyen, A.-H., Brady, S. M., Kase, C. S., et al. (2007). Depressive symptoms and risk of stroke: The Framingham Study. Stroke, 38, 16–21.
Simons, L. A., McCallum, J., Friedlander, Y., & Simons, J. (1998). Risk factors for ischemic stroke: Dubbo study of the elderly. Stroke, 29, 1341–1346.
Simpson, S. M., Krishnan, L. L., Kunik, M. E., & Ruiz, P. (2007). Racial disparities in diagnosis and treatment of depression: A literature review. Psychiatric Quarterly, 78, 3–14.
Smith, M. A., Risser, J. M. H., Lisabeth, L. D., Moye, L. A., & Morgenstern, L. B. (2003). Access to care, acculturation, and risk factors for stroke in Mexican Americans: The Brain Attack Surveillance in Corpus Christi (BASIC) project. Stroke, 34, 2671–2675.
Steffens, D. C., Artigues, D. L., Ornstein, K. A., & Krishnan, K. R. (1997). A review of racial differences in geriatric depression: Implications for care and clinical research. Journal of the National Medical Association, 89, 731–736.
Steffick, D. (2000). Documentation of affective functioning measures in the health and retirement study. HRS Documentation Report DR-005. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf.
Surtees, P. G., Wainwright, N. W. J., Luben, R. N., Wareham, N. J., Bingham, S. A., & Khaw, K. T. (2008). Psychological distress, major depressive disorder, and risk of stroke. Neurology, 70, 788–794.
Takeuchi, D. T., Alegria, M., Jackson, J. S., & Williams, D. R. (2007). Immigration and mental health: Diverse findings in Asian, black, and Latino populations. American Journal of Public Health, 97, 11–12.
Trimble, B., & Morgenstern, L. B. (2008). Stroke in minorities. Neurologic Clinics, 26, 1177–1190.
Uebelacker, L., Strong, D., Weinstock, L., & Miller, I. (2009). Use of item response theory to understand differential functioning of DSM-IV major depression symptoms by race, ethnicity and gender. Psychological Medicine, 39, 591–601.
Wendell, C., Hosey, M., Lefkowitz, D., Katzel, L., Siegel, E., Rosenberger, W., et al. (2010). Depressive symptoms are associated with subclinical cerebrovascular disease among healthy older women, not men. American Journal of Geriatric Psychiatry, 18, 940–947.
Williams, L. (2005). Depression and stroke: cause or consequence? Seminars in Neurology, 25, 396–409.
Williams, D. R., Gonzalez, H. M., Neighbors, H., Nesse, R., Abelson, J. M., Sweetman, J., et al. (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites—Results from the National Survey of American Life. Archives of General Psychiatry, 64, 305–315.
Acknowledgments
The authors gratefully acknowledge financial support from the American Heart Association grants 09PRE2080078 and 10SDG2640243, the NIH National Research Service Award (NRSA) training grant (T32-HL098048-01) and from the Milton Fund of Harvard University.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Glymour, M.M., Yen, J.J., Kosheleva, A. et al. Elevated depressive symptoms and incident stroke in Hispanic, African-American, and White older Americans. J Behav Med 35, 211–220 (2012). https://doi.org/10.1007/s10865-011-9356-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-011-9356-2