Abstract
Orthopedic and dental implant failure continues to be a significant concern due to localized bacterial infections. Previous studies have attempted to improve implant surfaces by modifying their texture and roughness or coating them with antibiotics to enhance antibacterial properties for implant longevity. However, these approaches have demonstrated limited effectiveness. In this study, we attempted to engineer the titanium (Ti) alloy surface biomimetically at the nanometer scale, inspired by the cicada wing nanostructure using alkaline hydrothermal treatment (AHT) to simultaneously confer antibacterial properties and support the adhesion and proliferation of mammalian cells. The two modified Ti surfaces were developed using a 4 h and 8 h AHT process in 1 N NaOH at 230 °C, followed by a 2-hour post-calcination at 600 °C. We found that the control plates showed a relatively smooth surface, while the treatment groups (4 h & 8 h AHT) displayed nanoflower structures containing randomly distributed nano-spikes. The results demonstrated a statistically significant decrease in the contact angle of the treatment groups, which increased wettability characteristics. The 8 h AHT group exhibited the highest wettability and significant increase in roughness 0.72 ± 0.08 µm (P < 0.05), leading to more osteoblast cell attachment, reduced cytotoxicity effects, and enhanced relative survivability. The alkaline phosphatase activity measured in all different groups indicated that the 8 h AHT group exhibited the highest activity, suggesting that the surface roughness and wettability of the treatment groups may have facilitated cell adhesion and attachment and subsequently increased secretion of extracellular matrix. Overall, the findings indicate that biomimetic nanotextured surfaces created by the AHT process have the potential to be translated as implant coatings to enhance bone regeneration and implant integration.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Metallic implants, primarily composed of titanium alloys, have become increasingly prevalent in dental and orthopedic applications over the last decade. In 2010, a staggering 7.2 million Americans underwent total joint replacement surgery, with 2.5 million receiving total hip replacements and 4.7 million undergoing total knee replacements [1]. Similarly, the number of dental implantations increased by 14% per year between 1999 and 2016 [2]. These trends are predicted to inflate exponentially, with projections estimating a 50% increase in hip and knee replacements by 2030 and a 23% increase in dental implants by 2026 [2, 3].
Despite their life-enhancing potential, standard metallic alloy-based implants are associated with numerous challenges. Among these, bone loss surrounding the implant is particularly noteworthy because of the potential bacterial infection in the micro-space due to poor soft tissue attachment. This leads to implant failure, causing revision surgeries that are more complicated and costly, further leading to a socioeconomic impact on the patient and a burden on the healthcare system [4,5,6,7]. Standard operating conditions and isolation of patients are often considered during surgical procedures to minimize the risk of bacterial infections [8, 9]. Efforts have also been made to prevent infections using antibiotics as the conventional treatment method [10]. However, this approach has led to the development of antimicrobial-resistant infections, which have become a growing problem in recent years. Chemical modification of the implant surface has also been reported to minimize bacterial attachment, thereby inhibiting biofilm formation [11,12,13]. Antibiotic coatings such as gentamicin have been immobilized on implant surfaces to kill the bacteria that adhere to the surface [14]. However, the gradual loss of coating while fitting the implant into the bone or during the micromotion of implants can create additional biological concerns, such as aggressive inflammatory response or bone necrosis, further increasing the probability of implant failure [15]. As the demand for metal-based implants continues to grow, it is crucial to address these challenges. There is a critical need to develop implant materials and strategies to promote enhanced integration with the host tissue as well as inherent antibacterial properties to achieve better long-term outcomes.
It is well established that the nanotextured surfaces with variable surface wettability, such as spinules/hair (hydrophobic), nano-grass (hydrophobic/hydrophilic), nanoneedles, spherical nano-cones, nano-hemispheres (hydrophilic), and nanopores (hydrophobic) are known to be toxic for different gram (+) and gram (-) species [16,17,18,19,20,21]. Besides, these nanotextured topographies are also known to provide cues for mammalian cell stimulation for improved cell attachment to the surface [22, 23]. Furthermore, recent studies have corroborated that naturally existing nanostructured surfaces found on insects and other living species can kill bacterial cells. The potential working mechanism could be rupturing the microbial cell wall through a contact-killing mechanism, thus offering an alternative solution [24, 25]. Therefore, synthesizing such biomimetic nanotextured implant surfaces can potentially reduce implant failure and minimize drug-resistant bacterial infections in healthcare settings.
Various methods have been employed in literature to prepare surfaces on titanium and its alloys, including chemical etching [26,27,28], sol-gel methods [29], anodization [30], and lithography [31]. Among these, chemical etching in alkali solutions stands out as a facile, high throughput, and cost-effective method capable of producing a titanate layer with randomly oriented nanostructures on the surface of titanium and its alloys [32]. Studies have shown that alkaline hydrothermal treatment (AHT) is being used to modify the surface of metals to enhance their chemical reactivity, adhesion properties, and hydrophilicity for biomedical applications [33, 34]. AHT is a potential approach to create nanostructures on the Ti alloy surface, which can elicit different biological responses depending upon the roughness, wettability, and other surface properties. The AHT is a function of the type of etching agent, its concentration, process time, and temperature [35]. For instance, Diu et al. used NaOH 1 M solution at a temperature of 240 °C for 3 and 8 h for their AHT process. They observed an effective response for their surface against gram-negative bacterial cell lines but not non-motile gram-positive bacteria [36]. Another group employed KOH & NaOH for AHT at 150 °C, resulting in different nanotextures [37]. Additionally, other researchers have investigated the influence of NaOH concentration of 1 M, 5 M and 10 M at 110 °C for 5 h, resulting in the development of varying nanotextures [38]. Even in our previous study, we utilized a 1 N NaOH solution as an etchant at 230 °C, examining two different processing times (4 and 8 h). We successfully created biomimetic nanotexture surfaces based on the cicada wing’s structure on medical grade 5 titanium (Ti) alloy, demonstrating inherent antibacterial properties for both gram-negative and gram-positive [26]. However, their biological responses to mammalian cell lines and surface properties have not been explored in-depth. Despite the considerable body of research on AHT applied to titanium implants, there remains a need for further exploration into the details of the process. Specifically, there is a gap in identifying the optimal processing parameters that influence the final biological and surface properties of the implants.
In this study, we aimed to develop biomimetic Ti surfaces for orthopedic and dental implant applications and evaluate the surface properties and their biological responses using an in vitro model. We hypothesized that the nanospikes created using AHT would allow the larger mammalian cells to adhere and proliferate.
2 Material and methods
2.1 Preparation of titanium alloy substrates
A titanium (Ti) grade 5 alloy sheet (McMaster-Carr, Elmhurst, IL, USA) of thickness 0.4 mm was cut into small flat square sections of 10 mm × 10 mm using a band saw. The cut Ti sections were subsequently polished with silicon carbide grinding papers ranging from coarse to very fine grit sizes # 220, 400, 1000, and 1500. During the grinding operation, a steady stream of water was applied to the metallic sections to drive away the ground particles. To maintain uniform grinding and suppress the development of deep grooves, the Ti sections were rotated 90° following each successive grinding. Finally, using 1500-grade grinding paper, mirror-finish samples were obtained. The samples were then ultrasonically washed in acetone for 10 min, ensuring that the samples did not stick to each other. Subsequently, the samples were rinsed with deionized water and air-dried before use for further experimentation.
2.2 Alkaline hydrothermal treatment (AHT)
The small sections of Ti alloys were placed in the acid digestion vessels (Model # 4745, Parr Instrument Company, Moline, IL, USA) for carrying out the AHT for two different reaction times of 4 h and 8 h following our previous study [26]. Briefly, the samples were placed in a polytetrafluoroethylene (PTFE) cup (23 ml capacity) with a cover housed within a metallic body and a screw cap of the acid digestion vessel. The PTFE cup was filled with 10 ml of 1 N sodium hydroxide (NaOH) solution, used as the reactant for alkaline hydrothermal treatment of Ti alloy samples, and was covered with the PTFE cover. The selection of a 1 N NaOH concentration was based on our established methodologies and previous research, ensuring consistency with existing literature [26, 36]. The number of metallic samples per vessel was limited to one to avoid sticking the metal pieces with one another. A corrosion disc (thinner foil) was placed above the PTFE cover along with a blow-off disc. Further, the threaded screw of the cap was lubricated with graphite powders to prevent jamming. The vessel was sealed by hand tightening the screw cap, and then it was turned not more than 1/8 turn using the hook spanner wrench provided by the manufacturer to avoid over-tightening. Once assembled, the digestion vessels were placed in an oven preheated at 230 °C to prepare two groups (4 h and 8 h) of samples. After the reaction, the vessels were removed from the oven and cooled down to room temperature before extracting the Ti sample from the acid digestion vessels. The Ti samples were then thoroughly rinsed with deionized water to remove the unreacted NaOH.
2.3 Post-alkaline hydrothermal treatment and calcination
The AHT processed samples for both groups were placed in a ceramic dish, with the polished surface facing upwards in the oven for 1 h at 230 °C. Subsequently, 0.6 M HCl was poured into the ceramic container and held for five minutes to allow ion exchange and conversion of sodium titanate to TiO2 [39, 40]. The samples were then thoroughly rinsed with deionized water to wash off any residual acid. Finally, the samples were transferred to a furnace maintained at 600 °C for 2 h for calcination to oxidize the samples completely. After calcination, the samples were stored, sterilized with 70% ethanol, and rinsed with phosphate buffer solution before subsequent experimentations.
In sum, three (3) groups of Ti samples were prepared: 1) Group 1: Negative Control (Ti samples with no AHT); Group 2: 4 h AHT (Ti samples subjected to 4 h of AHT at 230 °C); 3) Group 3: 8 h AHT (Ti samples subjected to 8 h of AHT at 230 °C); 4) Tissue culture polystyrene (TCPS) plates characterized by a roughness ranging from 0.1 to 5 nm [41], serve as the positive control, with cells cultured in a well plate.
2.4 Surface topology
The surface topography of the Ti specimens for the three groups was analyzed using a field emission scanning electron microscope (JEOL 6330 F, JEOL Ltd., Akishima-Shi, Tokyo, Japan). The specimens (n = 3 per group) were first sputter coated with a 10 nm layer of platinum before observing them under SEM at a voltage of 5 kV and a working distance of 15–16 mm. Further, the length and % area of the nanospikes was calculated from the observed images using ImageJ. The examination was conducted on randomly selected regions to provide representative images of the unique topology of the Ti plates in different groups.
2.5 Wettability
The wettability of different groups was determined by measuring the contact angles under ambient conditions (Temperature 20 °C, 40% humidity) using a sessile drop method with a goniometer (Ossila Limited, Sheffield, United Kingdom), as conducted previously [42]. Deionized water was employed as the solvent to carry out the test. A drop of water was placed on the surface of samples (n = 3/group), which was recorded for 10 s using a high-resolution camera. Three measurements were recorded at different locations on each specimen with sufficient spacing to prevent any interference from previous tests. The contact angle θ, which is the angle between the solid surface and the liquid interface, was measured using the measurement software provided with the instrument. The average contact angle of each group was determined and recorded.
2.6 Roughness
A Dektak XTL Stylus Profiler (Brucker, Billerica, MA) was employed to measure the surface roughness of all three groups of titanium samples. Three samples from each group were randomly selected, and the stylus of the profiler was moved three times for a 3 mm distance at a speed of 0.4 mm/sec and a force of 10 mg on different areas of each sample to provide a raw roughness value. Utilizing custom-written MATLAB code, the average values of the raw roughness for each group were recorded and compared.
2.7 In-vitro cell studies
Ti samples were randomly selected from each group. In addition to using 70% ethanol, the samples were sterilized with ultraviolet light for one hour in the cell culture hood before performing cell culture experiments. The human osteoblast cell line (hFOB 1.19, ATCC, Manassas, VA, USA) were cultured until passage 2 (P2) in a complete growth medium at 34 °C, and 5% CO2 in a humidified atmosphere, as previously reported [43]. Briefly, the cells were thawed and transferred into the complete media comprised of the base medium (Catalog # 11039021, Gibco, Fischer Scientific, Hanover Park, IL), which is a 1:1 mixture of DMEM/F-12 with 2.5 mM L-glutamine that was further supplemented with 10% fetal bovine (Catalog # 16000044, Fischer Scientific), 1% Penstrep (Catalog# 15140122, Fischer Scientific) to 1% and 0.3 mg/ml of G418 disulphate solution (Catalog# G8168, Sigma Aldrich Inc.). Cultivating osteoblasts at 34 °C rather than the more common 37 °C aligns closer with in vivo bone tissue conditions, ensuring experiments yield more applicable and meaningful outcomes. This temperature adjustment has been shown to not only bolster osteoblast differentiation and function but also to stimulate the expression of bone-specific genes and the synthesis of extracellular matrix components, effectively replicating the natural bone formation process more accurately [44, 45].
2.7.1 Cell Attachment and Adhesion (Cytoskeleton Imaging—DAPI, Phalloidin)
To explore cell adhesion and their morphology on different groups of Ti substrates, staining procedures were implemented, involving counterstaining with DAPI (stains nuclei) and Phalloidin-iFluor 594 Reagent (ab150117) (stains cytoskeleton) at a dilution of 1:1000 in PBS containing 1% BSA. After a 48-hour incubation, cells on different Ti substrates were washed twice with PBS and then moved to fresh wells in a new 48-well plate. Following this, hFOBs were fixed with a 4% paraformaldehyde solution (PFA) for 10 min, permeabilized with Triton X-100 (0.1 v/v%) for 5 min and stained with fluorescein phalloidin for 1 h. Cell nuclei were further labeled using DAPI (Invitrogen). Fluorescence imaging of all samples was performed using a confocal laser-scanning microscope equipped with a 10x objective lens (Zeiss, LSM800). The area of cell adhesion was analyzed using ImageJ (Rasband, W.S., ImageJ, U.S. National Institutes of Health, Bethesda, Maryland, USA) with the respective F-actin (red) and cell nuclei (blue) channels as previously reported [46]. The average cell area was calculated using the formula:
2.7.2 Cell Viability
To assess cell viability on Ti samples (n = 3/group), a live-dead assay employing Calcein AM/Ethidium homodimer was performed. Ti samples from each group were placed in a 48-well plate and seeded with the cells at a density of 2.5 × 105 cells/ ml. Following a 48 h incubation period, the samples were washed and transferred to the new wells before initiating the assay with the Live/Dead cell imaging kit 488/570 (ThermoFisher Scientific) in accordance with the manufacturer’s instructions. In brief, the samples underwent staining with Calcein AM and Ethidium homodimer in PBS solution for 15 min in a dark environment at room temperature. Subsequently, the samples were rinsed twice with phosphate-buffered saline to eliminate the background fluorescence and visualized using the Zeiss confocal laser-scanning microscope at excitation and emission wavelengths of 488 nm and 570 nm, respectively.
2.7.3 Cytotoxicity and proliferation assessment
The cytotoxicity of osteoblastic hFOB 1.19 cells exposed to the three different surfaces (n = 3/group) was evaluated using sulforhodamine B (SRB) assays. Cells were seeded at a density of 1 × 105 cells/ml and incubated in a standard cell culture environment for osteoblasts (5% CO2 and 34 °C) for 1, 3, and 7 days. The SRB assay was conducted using the CytoScanTM SRB Cytotoxicity Assay Kit (Catalog # 89028079, Fischer Scientific) as per a previously published method [47, 48], and the cellular viability was quantified by the colorimetric measurement of the cellular protein. The process involved fixing the cells on the sample surface, washing the fixing reagent, staining the protein within the viable cells with SRB dye, rinsing the cells to remove the unbound dye, and extracting the SRB-bound protein solution for quantification. The absorbance of the collected solutions was measured at 565 nm using a microplate reader, and cellular viability was reported as “Relative Survival” based on the absorbance values. The results were normalized such that the average absorbance of TCPS positive control group was equal to one. The background absorbance was subtracted, and each absorbance value was divided by the average absorbance value of the control group (data represented as mean ± standard error (SE)). A higher absorbance value indicates lower cell toxicity due to a more significant number of viable cells that can be correlated to cell proliferation.
2.7.4 Alkaline phosphatase activity
The quantification of cell differentiation for each group of Ti plates/substrates was conducted by measuring the Alkaline Phosphatase (ALP) activity of the control and exposed cells (n = 3/group) using a fluorometric assay (Catalog # 89028079, Fischer Scientific) as previously conducted [49]. The cells were plated on different substrates in a 24-well plate at a cell density of 1 × 105 cells/ml, and ALP activity was measured at respective time points. At each time point, cells were trypsinized from each sample, and the cell pellet obtained was homogenized in 100 µl of assay buffer. Then, 30 µl of cell lysate from each sample in triplicates was diluted with the assay buffer to a total volume of 110 µl and mixed with 20 µl of 0.5 mM of the non-fluorescent substrate 4 methylumbelliferyl phosphate (MU) and incubated for 30 min at room temperature in the dark. Background controls were prepared similarly using the assay buffer, which was mixed with the non-fluorescent substrate and 20 µl of stop solution. The reaction was stopped by adding 20 µl of stop solution (except for the background samples) and shaking gently. The fluorescence intensity was measured using a fluorescence microplate reader at Ex/Em 360/400 nm, with values corrected by subtracting the background control samples. The amount of 4-MU generated was calculated using a standard curve (prepared using the manufacturer’s instructions). ALP activity was calculated in mU/ml using the formula ALP activity = A/V/T (where A = amount of 4-MU generated, V = volume of samples in the assay well, and T = reaction time). To normalize the ALP activity of different groups at each time point, the ALP activity of each group was divided by the average ALP activity of the control group at the corresponding time point.
2.8 Statistics
The results for wettability, roughness, cytotoxicity, and ALP activity were expressed as mean ± standard deviation (SD) unless specified something else. Statistical analysis was done using SPSS (IBM, version 27). A one-way ANOVA with Tukey’s post-hoc test was performed to compare the means of different groups at a 5% level of significance unless stated otherwise.
3 Results
3.1 Surface topology
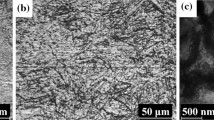
SEM imaging revealed different surface topographies for different groups as shown in Fig. 1. The negative control group (Group 1) exhibited a relatively smooth surface with minimal artifacts (Fig. 1a), whereas the surfaces of Group 2 (4 h) and Group 3 (8 h) AHT specimens displayed nanoflower structures containing randomly distributed nano-spikes (Fig. 1b, c) similar to nanostructures reported previously for hydrothermal etching of Ti [27]. We observed that the average height of the spikes ranged from 250 to 350 nm for the 4 h AHT group, whereas it measured in the range of 1000–1250 nm for the 8 h AHT group, as highlighted by the red lines (Fig. 1b, c). Additionally, the calculated spatial area of the nanospikes from both the 4 h and 8 h AHT images was approximately 37%.
SEM micrographs showing the surface topology of Ti specimens for different groups. a Nega-tive Control group exhibited relatively smooth surface with little artifacts while nanoflowers containing randomly distributed nano-spike structures in the range of 250–350 nm and 1000–1250 nm were ob-served in 4 h and 8 h AHT specimens respectively. Panel (b, c) as indicated by the red lines. Insets provide a closer, magnified view of the images
Fig. 1 SEM micrographs showing the surface topology of Ti specimens for different groups. Fig. 1a: Negative Control group exhibited relatively smooth surface with little artifacts while nanoflowers containing randomly distributed nano-spike structures in the range of 250–350 nm and 1000–1250 nm were observed in 4 h and 8 h AHT specimens respectively (Fig. 1b, c) as indicated by the red lines. Insets provide a closer, magnified view of the images.
3.2 Wettability
The average contact angle measured for the negative control group surface was 76.24 ± 5.29°. There was a statistically significant decrease (P = 0.004 and P = 0.000) in the contact angle for both the treatment groups (4 h and 8 h AHT) compared to the negative control group respectively. The average contact angle was 43.84 ± 11.55° and 25.16 ± 5.22° for the 4 h and 8 h AHT groups, respectively. Furthermore, there was a statistically significant difference (P = 0.008) between the contact angles for the 4 h and 8-hr AHT groups (Fig. 2a).
a Contact Angle measurement using Goniometer for different groups. b Surface Roughness measured using Dektak XTL Stylus Profiler. c Surface roughness height profile measured by randomly selecting one part of the surface from each group. We found a significant difference between the contact angles and roughness values of the negative control and the treatment groups, Group 1: Negative control; Group 2: 4 h AHT; Group 3: 8 h AHT, The “*” indicates that the difference between the groups was statistically significant (P < 0.05), mean ± SD, n = 3
3.3 Roughness
We observed a relatively smooth surface for the negative control group, with a roughness value of 130 ± 30 nm, which was statistically lower than the values of the treatment groups. The average roughness value for the 4 h AHT group was 260 ± 100 nm, higher than the negative control group value, while for the 8-hr AHT group, the average roughness value was 720 ± 80 nm, significantly higher than both the negative control group (P = 0.015) and the 4 h AHT group (P = 0.039) (Fig. 2b, c).
3.4 In-vitro cell studies
3.4.1 Cell attachment & adhesion
The cytoskeleton and nuclei of hFOB cells cultured on different Ti substrates (Negative Control, 4 h AHT, and 8 h AHT) for 48 h are illustrated in Fig. 3a–c. While hFOB cells on the negative control surface displayed elongated cell bodies, while those incubated on 4 h AHT and 8 h AHT surfaces exhibited spindle-like morphology with thinner and more elaborated cell extensions. Further, we found that the average cell area for the 8 h AHT group was statistically higher compared to 4 h AHT (P = 0.082) at 90% confidence level (Fig. 3h).
a–c Cytoskeleton (red fluorescence) and nuclei (blue fluorescence) staining showing the cell adhesion to the surface after 48 h of cell culture with different surface topologies. The surfaces appeared to have a different response to the cell attachment. Insets provide a closer, magnified view of the cells morphology and expansion. d–f Viability of cells in direct contact with the treated surfaced using confocal microscope (green fluorescence—viable cells, red fluorescence—dead cells) g Cell toxicity of osteoblastic cells normalized to TCPS positive control group on different surfaces showed a higher relative survivability of osteoblastic cells in the 8 h AHT group compared with the negative control and 4 h AHT groups on over a period of 7 days. The “*” indicates that the difference between the groups was statistically significant (P < 0.05). h Average cell area calculated from cytoskeleton staining, The “**” indicates that the difference between the groups was statistically significant difference (P < 0.1), Group 1: Negative control; Group 2: 4 h AHT; Group 3: 8 h AHT, mean ± SD, n = 3
3.4.2 Cell viability
The viability of the hFOB cells on the three different Ti substrates was observed after 48 h of culture. As shown in the representative images of the live-dead assay fluorescence images (Fig. 3d–f) the hFOB cells were found to be viable in all three Ti groups. It’s important to note that the overlapping arrangement of cells hindered our ability to quantify cell viability accurately.
3.4.3 Cytotoxicity and proliferation assessment
Osteoblastic cells exhibited successful adherence to the substrate surfaces, initiating a rapid proliferation phase as early as day 1, with a significant difference observed for the 8 h AHT group compared to both the negative control (P < 0.05) and the 4 h AHT group (P < 0.05). This proliferation trend continued over the 3-day incubation period, demonstrating a significant increase (P = 0.045 and P = 0.000) in the relative survival for both treatment groups (4 h and 8 h AHT) compared to the negative control group, respectively. Additionally, a statistically significant difference (P = 0.017) was observed in the relative survival between the 4 h and 8 h AHT groups. However, by Day 7, no significant difference in relative cell survival was observed between the negative control group and the treatment groups (Fig. 3g).
3.4.4 Alkaline phosphatase (ALP) assay
In this study, we utilized an ALP assay to evaluate the impact of different Ti nanotextured surfaces on the osteoblastic differentiation potential, without the addition of differentiation growth factors. The results, expressed as the mean ± standard deviation (U/ml), are presented in Fig. 4. After two weeks, the 8 h group samples exhibited the highest alkaline activity (1.42 ± 0.12 U/ml) among all three titanium surfaces tested. The 4 h group demonstrated an ALP activity of 1.36 ± 0.15 U/ml. The flat polished Ti control exhibited an activity of 1.00 ± 0.17 U/ml. Notably, the AHT-treated groups showed a statistically significant increase (P = 0.000) in ALP activity compared to the TCPS positive and Negative control groups. However, no significant difference (P = 0.821) was observed in the ALP activity of cells on the 4 h and 8 h treated group surfaces.
ALP activity in different groups using the fluorometric method over a period of 14 days. A statistical increase in ALP activity for cells in the 4 h and 8 h AHT groups compared to cells in TCPS positive and negative control groups was observed at week 2. The “*” indicates that the difference between the groups was statistically significant (P < 0.05), mean ± SD, n = 3
4 Discussion
We observed that the 4 h and 8 h AHT of Ti-grade 5 alloys specimen resulted in nano-scale features on the surface, facilitating the adhesion and proliferation of mammalian cells. The nano-scale features, resembling nanoflowers (Fig. 1a), developed on Ti surfaces through AHT had an average spike height of approximately 250–350 nm for the 4 h group and 1000–1250 nm for the 8 hr group. Both groups had similar spatial coverage, with the measured percent area being approximately 37%. This indicates a consistent distribution of the spikes over the unit area for both treatment groups. However, the length of these nanospikes significantly changed the surface topology, contact angle, and surface roughness of the treatment groups.
We then assessed surface wettability by measuring the contact angles of the treatment groups and compared our findings against those derived from the negative control group. A water contact angle is a standard to define whether the surface is hydrophilic (angle < 90°) or hydrophobic (angle > 90°) [50]. Our results revealed a noteworthy and statistically lower (P < 0.05) contact angle values of the treatment groups when compared to the flat-polished negative control group. The contact angles formed on the 4 h and 8 h AHT groups were 43.84 ± 11.55° and 25.16 ± 5.22° respectively, compared to the 76.24 ± 5.29° for the untreated smooth surface of the negative control group. This reduction implies an enhancement in wettability characteristics, indicative of a more hydrophilic surface.
Furthermore, our observations indicated a correlation between the duration of AHT and the increase in wettability. Specifically, surfaces subjected to an 8-hr AHT exhibited contact angle values that were statistically lower (P = 0.008) than those of the 4 h AHT groups, signifying a higher degree of wettability. This implies that the duration of AHT plays a pivotal role in influencing the wettability characteristics of the treated surfaces.
With more time for the AHT, we found a statistically significant increase (P < 0.05) in the roughness for the 8-hr AHT groups compared with negative control and 4-hr AHT groups. This may be due to the formation of nanospikes on the Ti alloy surface during the AHT, which involves a series of chemical reactions and physical processes. In brief, during the AHT process, the sodium hydroxide (NaOH) solution first reacts with the Ti alloy surface, leading to the formation of the titanium oxide (TiO2) layer. Then, the TiO2 layer undergoes a dissolution-precipitation process, where the dissolution of TiO2 is followed by the precipitation of TiO2 nanoparticles on the surface. Finally, the TiO2 nanoparticles coalesce to form nanospikes, which are vertically oriented structures with a high aspect ratio. The size and shape of the nanospikes depend on the AHT processing parameters, such as the temperature, pressure, and duration of treatment, as well as the composition of the Ti alloy and NaOH concentration [28, 51,52,53,54]. Therefore, in our case, 8-hr AHT formed longer nanospikes, which might have increased the roughness of this group compared with the 4-hr AHT group that had short nanospikes.
It has been established that cell adhesion depends on surface wettability and roughness, which can dictate cell-cell and cell-surface interactions and cell behavior [55, 56]. The enhanced wettability of the treated surfaces, achieved through alkaline hydrothermal treatment (AHT), is likely to improve the interaction with culture media in a manner similar to its interaction with DI water. This enhanced surface-media interaction is anticipated to facilitate a more favorable environment for competitive adsorption of fibronectin present in the culture medium leading to increased cell attachment and proliferation [57]. As shown previously, the cell attachment process progresses through three distinct stages marked by an increase in the number of attached cells with time (stage I), flattening of cells (stage II), until they reach the stable stage of elongation of cells (stage III) on the surface [58]. In our study, we observed the cells’ morphology starting from day 1 for all groups, at which point all the cells had reached a stable phase of attachment and organization.
Previous studies have indicated that surfaces with varying roughness can induce distinct phenotypes, affecting morphology, size, and cytoskeletal organization, with reported optimum surface roughness ranging from 0.13 to 4 µm [59,60,61,62]. In our study, the 8 h AHT group exhibited higher roughness of 0.72 ± 0.08 µm. This resulted in increased cell adhesion on this surface and was confirmed from our cell adhesion study where we found that the 8-hr AHT group had significantly higher value of average cell area compared to the 4-hr group (Fig. 3h). The observed spreading of cells on these surfaces is attributed to interactions with the nanostructures.
Moreover, diverse cell morphologies, such as elongated cell bodies and spindle-like shapes, were observed on the flat polished surface (negative control group) and in our treatment groups (4 h and 8 h AHT) respectively. This observation is consistent with findings from previous studies on osteoblast morphology, where similar phenotypes were documented on both smooth and rough surfaces [37, 63].
Our cell toxicity assay (Fig. 3g) suggested that the 8 h AHT group exhibited the lowest cytotoxicity among the tested surfaces before reaching the steady state phase on day 7, as evidenced by the higher relative survivability of the osteoblastic cells. These cytotoxic results can be linked to cell adhesion and proliferation, indicating that the 8 h AHT group might have allowed for more cell attachment than the 4 h AHT group. These findings were further confirmed through cytoskeleton staining and Live/Dead assay after 48 h hFOB culture on different Ti substrates. Indeed, the two distinct topographies primarily varied in the size and shape of their surface structures. This difference in surface structures also influences their mechanobactericidal activity as shown previously in our study [26].
The alkaline phosphatase (ALP) activity, indicative of osteoblastic activity and differentiation and providing valuable insights into the bone formation potential of the surface was measured for four groups: TCPS positive control, negative control, 4 h AHT, and 8 h AHT groups. The results indicated that the 8-hr AHT group exhibited the highest ALP activity, which was significantly higher (P < 0.05) than that of the TCPS positive and negative control groups. These findings correlate with the observed morphology in cytoskeleton staining, indicating that the increased cell attachment area or improved cell-surface interaction might have contributed to an increase in ALP activity levels. This increase, in turn, could potentially support enhanced matrix mineralization. Similar effects were observed in previous studies, where higher roughness levels ensured better tissue adhesion and integration between the implant and bone, subsequently positively impacting the healing time after implantation [64, 65]. Moreover, osteogenic differentiation is recognized as a multistep process characterized by a peak in ALP activity, followed by a subsequent decline during the mineralization phase [66]. The 8 h AHT sample results suggest that the osteogenic differentiation process was still ongoing after a period of 2 weeks.
In our previous study, even though we followed a similar methodology for preparing treatment group 4 h AHT and 8 h AHT, our primary emphasis was on assessing the antibacterial properties of those modified surfaces. The results in that prior study revealed significant bactericidal properties for Gram-positive and Gram-negative bacteria and motile/non-motile bacterial strains [26]. When considering our prior findings in conjunction with the current results of this study, it overall suggests that the biomimetic nanospikes inspired by the cicada wing structure, created by AHT, not only enhance the adhesion and proliferation of bone cells on biomimetic surfaces—particularly the 8 h AHT surfaces—leading to enhanced bone mineralization, but may also potentially provide inherent antibacterial properties simultaneously. These findings have important implications for the advancement of new implant materials that can promote osseointegration and improve the long-term success of orthopedic and dental implants while preventing bacterial infections. In particular, biomimetic surfaces created by AHT may have potential applications in developing implant coatings or surface modifications that can enhance bone regeneration and integration and could simultaneously prevent bacterial infection.
Although our results are encouraging for the development of smart surfaces for metallic implants that can promote the adherence, proliferation, and differentiation capability of osteoblastic cells to enhance osseointegration and possess an inherent ability to eradicate bacteria on contact, the long-term stability of these nanostructures are yet to be assessed. Additionally, all our investigations were conducted in vitro, highlighting the need to evaluate further their clinical efficacy in ex vivo and in vivo models. Furthermore, all our investigations were conducted in vitro, emphasizing the need to evaluate their clinical efficacy further using ex vivo and in vivo models. Additionally, while we chose the hFOB 1.19 cell line for its relevance to osteoblast behavior and widespread use in bone-related research, it may not fully represent the diversity of cell responses in clinical scenarios. To address this limitation and better mimic the complex cellular environment encountered clinically, future studies should incorporate primary cells derived from patient samples or co-culture systems involving multiple cell types to provide a more comprehensive understanding.
5 Conclusions
In conclusion, our study highlights the efficacy of alkaline hydrothermal treatment in creating biomimetic surfaces with nanospikes on Ti alloy surfaces. Our findings demonstrate that both the 4-hour and 8-hour AHT of Ti-grade 5 alloy specimens resulted in nano-scale features on the surface, which significantly enhanced the adhesion and proliferation of mammalian cells. Specifically, the longer duration of AHT led to the formation of longer nanospikes, increased surface roughness, and improved wettability, all of which contributed to enhanced osteoblast adhesion and proliferation. The observed effects on cell adhesion and proliferation suggest that these nanotextured surfaces hold promise for improving clinical outcomes, such as faster osseointegration and reduced implant failure rates. Furthermore, the bactericidal properties of these surfaces further enhance their potential for clinical application, as they may help reduce the risk of post-operative infections. However, it is important to note that further research is necessary to fully understand the long-term stability of surface nanostructures and their clinical effectiveness. This underscores the importance of continued investigation into the potential benefits and challenges associated with implementing this innovative approach in orthopedic and dental implant.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Kremers HM, Larson DR, Crowson CS. et al. J Bone Joint Surg. 2015;97:1386
Elani H, Starr J, Da Silva J, Gallucci G. J Dent Res. 2018;97:1424–30.
Etkin C, Springer B. Arthroplast Today. 2017;3:67–9.
Sansone V, Pagani D, Melato M. Clin Case Miner Bone Metab. 2013;10:34
Muratore M, Quarta E, Quarta L, Calcagnile F, Grimaldi A, Orgiani MA, et al. Clin cases Miner bone Metab. 2012;9:50–5.
Liaw K, Delfini RH, Abrahams JJ. Seminars in Ultrasound, CT and MRI. 2015;36:424–33.
Tao B, Lin C, He Y, et al. Chem Eng J. 2021;423:130176.
Song Z, Borgwardt L, Høiby N, Wu H, Sørensen, A Borgwardt A. Orthopedic Rev. 2013;5:65–71.
Strachan CJL. J Hospital Infect. 1995;30:54–63. https://doi.org/10.1016/0195-6701(95)90006-3
Romanò CL, Scarponi S, Gallazzi E, Romanò D, Drago L. J Orthop Surg Res. 2015;10:157.
Chouirfa H, Bouloussa H, Migonney V, Falentin-Daudré C. Acta Biomaterialia. 2019;83:37–54.
Bazaka K, Jacob MV, Crawford RJ, Ivanova EP. Appl Microbiol Biotechnol. 2012;95:299–311.
Yoshinari M, Kato T, Matsuzaka K, Hayakawa T, Shiba K. Biofouling. 2010;26:103–10.
Fuchs T, Stange R, Schmidmaier G, Raschke MJ. Arch Orthop Trauma Surg. 2011;131:1419–25.
Zhang B, Myers D, Wallace G, Brandt M, Choong P. Int J Mol Sci. 2014;15:11878–921.
Ivanova EP, Hasan J, Webb HK, Gervinskas G, Juodkazis S, Truong VK, et al. Nat Commun. 2013;4:2838.
Hasan J, Raj S, Yadav L, Chatterjee K. RSC Adv. 2015;5:44953–9.
Fisher LE, Yang Y, Yuen M-F, Zhang W, Nobbs AH, Su B. Biointerphases. 2016;11:011014.
May PW, Clegg M, Silva TA, Zanin H, Fatibello-Filho O, Celorrio V, et al. J Mater Chem B. 2016;4:5737–46.
Hizal F, Zhuk I, Sukhishvili S, Busscher HJ, van der Mei HC, Choi C-H. ACS Appl Mater interfaces. 2015;7:20304–13.
Bhadra CM, Khanh Truong V, Pham VT, et al. Sci Rep. 2015;5:16817.
Holban AM, Gestal MC, Grumezescu AM. Curr Med. Chem. 2014;21:3375–82.
Stevens MM, George JH. Science. 2005;310:1135–8.
Tripathy A, Sen P, Su B, Briscoe WH. Adv colloid interface Sci. 2017;248:85–104.
Jaggessar A, Shahali H, Mathew A, Yarlagadda PK. J Nanobiotechnol. 2017;15:1.
Elliott DT, Wiggins RJ, Dua R. J Biomed Mater Res Part B: Appl Biomater. 2021;109:973–81.
Vishnu J, Manivasagam VK, Gopal V, Garcia CB, Hameed P, Manivasagam G, et al. Nanomed: Nanotechnol, Biol Med. 2019;20:102016.
Zavala MÁL, Morales SAL, Ávila-Santos M. Heliyon. 2017;3:e00456.
Chang Y-C, Lee C-Y, Chiu H-T. ACS Appl Mater interfaces. 2014;6:31–5.
Sjöström T, McNamara LE, Yang L, Dalby MJ, Su B. ACS Appl Mater Interfaces. 2012;4:6354–61.
Dickson MN, Liang EI, Rodriguez LA, Vollereaux N, Yee AF. Biointerphases. 2015;10:021010.
Guo Z, Jiang N, Chen C, Zhu S, Zhang L, Li Y. Sci Rep. 2017;7:4155.
Lin L, Wang H, Ni M, Rui Y, Cheng TY, Cheng CK, et al. J Orthop Transl. 2014;2:35–42.
Al Mustafa M, Agis H, Müller HD, Watzek G, Gruber R. Clin Oral Implants Res. 2015;26:15–9.
Dong W, Zhang T, Epstein J, Cooney L, Wang H, Li Y, et al. Chem Mater. 2007;19:4454–9.
Diu T, Faruqui N, Sjöström T, Lamarre B, Jenkinson HF, Su B, et al. Sci Rep. 2014;4:7122.
Bright R, Hayles A, Wood J, Ninan N, Palms D, Visalakshan RM, et al. Nanomaterials. 2022;12:1140.
Huang Y-Z, He S-K, Guo Z-J, Pi JK, Deng L, Dong L, et al. Mater Sci Eng: C. 2019;94:1–10.
Feist TP, Davies PK. J solid state Chem. 1992;101:275–95.
Suzuki Y, Pavasupree S, Yoshikawa S, Kawahata R. J Mater Res. 2005;20:1063–8.
Lavenus S, Pilet P, Guicheux J, Weiss P, Louarn G, Layrolle P. Acta biomaterialia. 2011;7:1525–34.
Gill P, Musaramthota V, Munroe N, Datye A, Dua R, Haider W, et al. Mater Sci Eng: C. 2015;50:37–44.
Dua R, Centeno J, Ramaswamy S. J Biomed Mater Res Part B: Appl Biomater. 2014;102:922–32.
Subramaniam M, Jalal SM, Rickard DJ, Harris SA, Bolander ME, Spelsberg TC. J Cell Biochem. 2002;87:9–15.
Harris SA, Enger RJ, Riggs LB, Spelsberg TC. J Bone Miner Res. 1995;10:178–86.
Brugmans M, Cassiman JJ, Vanderheydt L, Oosterlinck AJ, Vlietinck R, Van Den Berghe H. Cytometry: J Int Soc Anal Cytol. 1983;3:262–8.
Gill P, Munroe N, Dua R, Ramaswamy S. J Biomater Nanobiotechnol. 2011;3:10–3.
Lordeus M, Estrada A, Stewart D, et al. Journal of Long-Term Effects of Medical Implants. 2015;25:1–2.
Dua R, Sharufa O, Terry J, et al. Front Bioeng Biotechnol. 2023;11:1202499.
Cheng CT, To S. Fly Cutting Technology for Ultra-precision Machining. 2023;393–412.
Lee N, Park J, Miralami R, Yu F, Skaines N, Armstrong M, et al. Biomimetics. 2022;7:91.
Anitha V, Banerjee AN, Joo SW, Min BK. Nanotechnology. 2015;26:355705.
Jaggessar A, Tesfamicheal T, Wang H, Yan C, Yarlagadda PK. Procedia Manuf. 2019;30:373–9.
Lu CL, Lin YH, Wong WW, Lin HH, Ho MW, Wang NC, et al. Chem Phys Lett. 2011;508:258–64.
Al-Azzam N, Alazzam A. Plos one. 2022;17:e0269914.
Arima Y, Iwata H. Biomaterials. 2007;28:3074–82.
Wei J, Igarashi T, Okumori N, Igarashi T, Maetani T, Liu B, et al. Biomed Mater. 2009;4:045002.
Majhy B, Priyadarshini P, Sen A. RSC Adv. 2021;11:15467–76.
Li Y, Xiong J, Wong CS, Hodgson PD, Wen Ce. Tissue Engineering Part A. 2009;15:3151–9.
Zareidoost A, Yousefpour M, Ghaseme B, Amanzadeh A. J Mater Sci: Mater Med. 2012;23:1479–88.
Zhang Y, Chen SE, Shao J, van den Beucken JJ. ACS Appl Mater interfaces. 2018;10:36652–63.
Sola-Ruiz MF, Perez-Martinez C, Labaig-Rueda C, Carda C, Martín De Llano JJ. Int J Mol Sci. 2017;18:823.
Levin M, Spiro RC, Jain H, Falk MM. Med Devices: Evid Res. 2022;15:103–19.
Wang C, Gao S, Lu R, Wang X, Chen S. Cells. 2022;11:3417.
Piszczek P, Radtke A, Ehlert M, Jędrzejewski T, Sznarkowska A, Sadowska B, et al. J Clin Med. 2020;9:342.
Przekora A. Mater Sci Eng: C. 2019;97:1036–51.
Acknowledgements
The authors would like to thank Drs. Neelam Azad and Anand Iyer for providing access and resources to their Tissue Culture laboratory at Hampton University. Additionally, the authors would like to express their appreciation for the support of Stan Frukhbeyn and Anthony Giuseppetti and resources extended by the American Dental Association Science & Research Institute (ADASRI), which played a pivotal role in the completion of this research endeavor.
Funding
This work was supported by the National Science Foundation (Grant # 2100498).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hadady, H., Alam, A., Khurana, I. et al. Optimizing alkaline hydrothermal treatment for biomimetic smart metallic orthopedic and dental implants. J Mater Sci: Mater Med 35, 31 (2024). https://doi.org/10.1007/s10856-024-06794-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-024-06794-y