Abstract
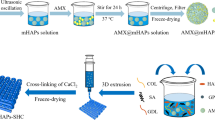
A clinical need continues for consistent bone remodeling within problematic sites such as those of fracture nonunion, avascular necrosis, or irregular bone formations. In attempt to address such needs, a biomaterial system is proposed to induce early inflammatory responses after implantation and to provide later osteoconductive scaffolding for bone regeneration. Biomaterial-induced inflammation would parallel the early stage of hematoma-induced fracture repair and allow scaffold-promoted remodeling of osseous tissue to a healthy state. Initiation of the wound healing cascade by two human concentrated platelet releasate-containing alginate/β-tricalcium phosphate biocomposites has been studied in vitro using the TIB-71™ RAW264.7 mouse monocyte cell line. Inflammatory responses inherent to the base material were found and could be modulated through incorporation of platelet releasate. Differences in hydrogel wt% (2 vs. 8 %) and/or calcium phosphate granule vol.% (20 vs. 10 %) allowed for tuning the response associated with platelet releasate-associated growth factor elution. Tunability from completely suppressing the inflammatory response to augmenting the response was observed through varied elution profiles of both releasate-derived bioagents and impurities inherent to alginate. A 2.5-fold upregulation of inducible-nitric oxide synthase gene expression followed by a tenfold increase in nitrite media levels was induced by inclusion of releasate within the 8 wt%/10 vol.% formulation and was comparable to an endotoxin positive control. Whereas, near complete elimination of inflammation was seen when releasate was included within the 2 wt%/20 vol.% formulation. These in vitro results suggested tunable interactions between the multiple platelet releasate-derived bioagents and the biocomposites for enhancing hematoma-like fracture repair. Additionally, minimally invasive delivery for in situ curing of the implant system via injection was demonstrated in rat tail vertebrae using microcomputed tomography.







Similar content being viewed by others
References
Dimitriou R, Jones E, McGonagle D, Giannoudis PV. Bone regeneration: current concepts and future directions. BMC Med. 2011;9(66):1–10.
Bauer TW. An overview of the histology of skeletal substitute materials. Arch Pathol Lab Med. 2007;131(2):217–24.
Kolk A, Handschel J, Drescher W, Rothamel D, Kloss F, Blessmann M, et al. Current trends and future perspectives of bone substitute materials—from space holders to innovative biomaterials. J Craniomaxillofac Surg. 2012. [Epub ahead of print].
Janicki P, Schmidmaier G. What should be the characteristics of the ideal bone graft substitute? Combining scaffolds with growth factors and/or stem cells. Injury. 2011;42(Suppl 2):S77–81.
Kalfas IH. Principles of bone healing. Neurosurg Focus. 2001;10(4);E1:1–4.
Kolar P, Schmidt-Bleek K, Schell H, Gaber T, Toben D, Schmidmaier G, et al. The early fracture hematoma and its potential role in fracture healing. Tissue Eng B. 2010;16(4):427–34.
Sun Y, Feng Y, Zhang CQ, Chen SB, Cheng XG. The regenerative effect of platelet-rich plasma on healing in large osteochondral defects. Int Orthop. 2010;34(4):589–97.
Burg KJ, Porter S, Kellam JF. Biomaterial developments for bone tissue engineering. Biomaterials. 2000;21(23):2347–59.
Williams DF. On the mechanisms of biocompatibility. Biomaterials. 2008;29(20):2941–53.
El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, et al. Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. J Periodontol. 2007;78(4):661–9.
Mehta S, Watson JT. Platelet rich concentrate: basic science and current clinical applications. J Orthop Trauma. 2008;22(6):432–8.
McCanless JD, Jennings LK, Cole JA, Bumgardner JD, Haggard WO. In vitro differentiation and biocompatibility of mesenchymal stem cells on a novel platelet releasate-containing injectable composite. J Biomed Mater Res A. 2012;100(1):220–9.
McCanless JD, Jennings LK, Cole JA, Bumgardner JD, Haggard WO. Induction of the early inflammatory-mediated cellular responses of fracture healing in vitro using platelet releasate-containing alginate/CaPO4 biomaterials for early osteoarthritis prevention. J Biomed Mater Res A. 2012;100(5):1107–14.
Haggard WO, McCanless JD, Inventors; University of Memphis, Assignee. Provisional patent application: Biomaterial composition and method of use, 6 May 2011.
Beamer B, Hettrich C, Lane J. Vascular endothelial growth factor: an essential component of angiogenesis and fracture healing. HSS J. 2010;6(1):85–94.
Ma PX. Alginate for tissue engineering. In: Ma PX, Elisseeff J, editors. Scaffolding in tissue engineering. Boca Raton: CRC Press; 2006. p. 13–25.
Nunamaker EA, Purcell EK, Kipke DR. In vivo stability and biocompatibility of implanted calcium alginate disks. J Biomed Mater Res A. 2007;83(4):1128–37.
Kong H, Mooney DJ. Polysaccharide-based hydrogels in tissue engineering. In: Dumitriu S, editor. Polysaccharides: structural diversity and functional versatility. 2nd ed. New York: CCR Press; 2005. p. 817–38.
White MM, Jennings LK. Appendix. Platelet protocols: research and clinical laboratory procedures. San Diego: Academic Press; 1999. p. 99–101.
Nicolin V, Ponti C, Narducci P, Grill V, Bortul R, Zweyer M, et al. Different levels of the neuronal nitric oxide synthase isoform modulate the rate of osteoclastic differentiation of TIB-71 and CRL-2278 RAW 264.7 murine cell clones. Anat Rec A. 2005;286(2):945–54.
Lock EF, Ziemiecke R, Marron J, Dittmer DP. Efficiency clustering for low-density microarrays and its application to QPCR. BMC Bioinform. 2010;11(386):1–8.
McCanless J, Cole J, Jennings L, Bumgardner J, Haggard W, editors. Biomaterial-assessed fracture healing as a model for the early prevention of joint degeneration: in vitro osteochondrogenesis, angiogenesis, immune response, and ex vivo injection delivery (in review). 58th Annual Meeting of the Orthopaedic Research Society, San Franscisco, CA; 2012.
Goldring SR. The role of bone in osteoarthritis pathogenesis. Rheum Dis Clin N Am. 2008;34(3):561–71.
Motamedi K, Seeger LL. Benign bone tumors. Radiol Clin N Am. 2011;49(6):1115–34, v.
Schmidhammer R, Zandieh S, Mittermayr R, Pelinka LE, Leixnering M, Hopf R, et al. Assessment of bone union/nonunion in an experimental model using microcomputed technology. J Trauma. 2006;61(1):199–205.
Mora R, Paley D. Nonunion of the long bones: diagnosis and treatment with compression–distraction techniques. New York: Springer; 2006.
Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423(6937):337–42.
Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5(12):953–64.
Tanaka T, Saito M, Chazono M, Kumagae Y, Kikuchi T, Kitasato S, et al. Effects of alendronate on bone formation and osteoclastic resorption after implantation of beta-tricalcium phosphate. J Biomed Mater Res. 2010;93(2):469–74.
Semple JW, Italiano JE Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264–74.
Brass L. Understanding and evaluating platelet function. Hematol Am Soc Hematol Educ Program. 2010;2010:387–96.
Leslie M. Cell biology. Beyond clotting: the powers of platelets. Science (New York, NY). 2010;328(5978):562–4.
dos Santos EA, Farina M, Soares GA, Anselme K. Surface energy of hydroxyapatite and beta-tricalcium phosphate ceramics driving serum protein adsorption and osteoblast adhesion. J Mater Sci Mater Med. 2008;19(6):2307–16.
Aslam R, Speck ER, Kim M, Crow AR, Bang KW, Nestel FP, et al. Platelet Toll-like receptor expression modulates lipopolysaccharide-induced thrombocytopenia and tumor necrosis factor-alpha production in vivo. Blood. 2006;107(2):637–41.
Shiraki R, Inoue N, Kawasaki S, Takei A, Kadotani M, Ohnishi Y, et al. Expression of Toll-like receptors on human platelets. Thromb Res. 2004;113(6):379–85.
Haselmayer P, Grosse-Hovest L, von Landenberg P, Schild H, Radsak MP. TREM-1 ligand expression on platelets enhances neutrophil activation. Blood. 2007;110(3):1029–35.
Washington AV, Gibot S, Acevedo I, Gattis J, Quigley L, Feltz R, et al. TREM-like transcript-1 protects against inflammation-associated hemorrhage by facilitating platelet aggregation in mice and humans. J Clin Investig. 2009;119(6):1489–501.
Mitani T, Terashima M, Yoshimura H, Nariai Y, Tanigawa Y. TGF-beta1 enhances degradation of IFN-gamma-induced iNOS protein via proteasomes in RAW 264.7 cells. Nitric Oxide. 2005;13(1):78–87.
Gruber R, Karreth F, Fischer MB, Watzek G. Platelet-released supernatants stimulate formation of osteoclast-like cells through a prostaglandin/RANKL-dependent mechanism. Bone. 2002;30(5):726–32.
Cuetara BL, Crotti TN, O’Donoghue AJ, McHugh KP. Cloning and characterization of osteoclast precursors from the RAW264.7 cell line. In Vitro Cell Dev Biol Anim. 2006;42(7):182–8.
Gurevitch O, Slavin S, Resnick I, Khitrin S, Feldman A. Mesenchymal progenitor cells in red and yellow bone marrow. Folia Biol (Praha). 2009;55(1):27–34.
Muguruma Y, Yahata T, Miyatake H, Sato T, Uno T, Itoh J, et al. Reconstitution of the functional human hematopoietic microenvironment derived from human mesenchymal stem cells in the murine bone marrow compartment. Blood. 2006;107(5):1878–87.
Wang ML, Massie J, Perry A, Garfin SR, Kim CW. A rat osteoporotic spine model for the evaluation of bioresorbable bone cements. Spine J. 2007;7(4):466–74.
Acknowledgments
The authors would like to acknowledge Dr. Thomas Sutter and Quynh Tran from the W. Harry Feinstone Center for Genomic Research for use of the iCycler and discussions on qRT-PCR data analysis. We also thank Dr. Richard A. Smith, Dr. Jinsong Huang, and Dr. Anobel Maghsoodpour for help in capturing data and software analysis pertaining to μCT. We also recognize Dr. John L. Williams from The University of Memphis for participation in the first author’s doctoral advisory committee and review of the current work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCanless, J.D., Jennings, L.K., Bumgardner, J.D. et al. Hematoma-inspired alginate/platelet releasate/CaPO4 composite: initiation of the inflammatory-mediated response associated with fracture repair in vitro and ex vivo injection delivery. J Mater Sci: Mater Med 23, 1971–1981 (2012). https://doi.org/10.1007/s10856-012-4672-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4672-9