Abstract
Drug delivery systems (DDS) based on poly (lactide-co-glycolide) (PLGA) microspheres and nanospheres have been separately studied in previous works as a means of delivering bioactive compounds over an extended period of time. In the present study, two DDS having different sizes of the PLGA spheres were compared in morphology, drug (dexamethasone) loading efficiency and drug release kinetics in order to investigate their feasibility with regard to production of medical combination devices for orthopedic applications. The loaded PLGA spheres have been produced by the oil-in-water emulsion/solvent evaporation method following two different schemes. Their morphology was assessed by scanning electron microscopy and the drug release was monitored in phosphate buffer saline solution at 37°C for 550 h using high performance liquid chromatography. The synthesis schemes used produced spheres with two different and reproducible size ranges (20 ± 10 and 1.0 ± 0.4 μm) having a smooth outer surface and regular shape. The drug loading efficiency of the 1.0 μm spheres was found to be 11% as compared to just 1% for the 20 μm spheres. Over the 550 h release period, the larger spheres (diameter 20 ± 10 μm) released 90% of the encapsulated dexamethasone in an approximately linear fashion whilst the relatively small spheres (diameter 1.0 ± 0.4 μm) released only 30% of the initially loaded dexamethasone, from which 20% within the first 25 h. The changes observed were mainly attributed to the difference in surface area between the two types of spheres as the surface texture of both systems was visibly similar. As the surface area per unit volume increases in the synthesis mixture, as is the case for the 1.0 μm spheres formulation, the amount of polymer-water interfaces increases allowing more dexamethasone to be encapsulated by the emerging polymer spheres. Similarly, during the release phase, as the surface area per unit volume increases, the rate of inclusion of water into the polymer increases, permitting faster diffusion of dexamethasone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
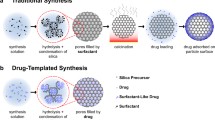
Poly (lactide-co-glycolide) (PLGA) has been studied for many years as a suitable drug delivery material, mainly due to its chemical biocompatibility [1, 2], total biodegradability, and non-toxic degradation products [3]. Because of these factors it can be also considered for the production of medical combination devices with microtextured metallic implants (drug/device), such as drug eluting orthopedic implants. A micro- or nano-spherical matrix for drug delivery is preferred in this case as the texture of the metallic biomaterial can be maintained and potentially the drug release profile can be extended over longer durations relative to other formulations such as films. However, in order to consider such a system, the individual components must first be assessed.
A common method for the sustained release of drugs is the production of a PLGA microsphere formulation by the oil-in-water emulsion and solvent evaporation technique, where the drug is evenly distributed throughout a soluble PLGA matrix and then emulsified. Once the organic solvent evaporates off, a suspension of solid microparticles is left. The bioactive can be co-dissolved in the PLGA if hydrophobic [4], or produced as a double emulsion or suspension if not [5]. The hydrophilicity of this polymer is defined by the lactide:glycolide ratio and can be used to alter the release rate in a microparticulate formulation [6]. The polymer molecular weight also influences the drug release rate [7]. The rate of degradation is inversely proportional to the proportion of lactide monomer in the polymer strands [1], and the rate of diffusion of drugs through the polymer matrix inversely proportional to the molecular weight of the PLGA polymer.
Microscale spheres are typically used in applications where the drugs must be delivered to only one site without diffusing away, such as the reduction of inflammation near glucose sensors [8], controlled release of insulin [9], or delivery of morphogenetic proteins for bone growth [10]. It has been considered [1] that the most effective size range for this is 10–200 μm. Where smaller than 10 μm, the microspheres become subject to not only diffusion, but are able to be phagocytosed by immune cells. This has the two downsides of not only the immune cells being capable of transporting the microspheres away from their intended site, but due to the phagocytosis the microspheres are much more rapidly broken down inside the acidic vesicles causing rapid release and potentially negating the slow release effect. Using microspheres larger than 200 μm may have a deleterious effect upon the tissue structure of the implantation site, potentially causing an increased immune response and unnecessary inflammation. Additionally, due to the increased radius and decreased surface area, the rate of water permeation and matrix degradation would be diminished, reducing the maximum possible rate of drug release.
The work undertaken in this paper was performed in order to assess the drug release kinetics and system efficiencies of two different PLGA sphere formulations (i.e. 20 vs. 1 μm spheres) in the view of further research towards the application of these systems for orthopedic medical combination devices. In this case, the drug delivery systems would become an integral part of the device providing a sustained drug release from, for example, a titanium hip stem. The model drug used in this investigation, dexamethasone (C22H29FO5), is a hydrophobic anti-inflammatory corticosteroid that is used to treat many inflammatory responses [8] and known to induce osteoblast differentiation [11]. The PLGA spheres loaded with dexamethasone have been produced by a similar method (oil-in-water emulsion/solvent evaporation) following two different schemes. Their morphology (size and shape), the drug loading efficiency and the drug release profiles in phosphate buffer saline solution at 37°C over a period of 550 h have been investigated.
2 Materials and methods
2.1 Materials
Poly (lactide-co-glycolide) (MW: 40,000–75,000, 50:50), dexamethasone (98%), poly (vinyl alcohol) (MW: 30,000–70,000), sodium azide, disodium hydrogen phosphate, sodium dihydrogen phosphate, acetic acid, sodium acetate and all solvents were purchased from Sigma Aldrich chemicals. Distilled, deionised water (ddH2O) was provided from Millipore.
Phosphate buffered saline (PBS) was made up as the simulated body fluid with the following concentrations: 0.24 g/l potassium dihydrogenphosphate, 1.44 g/l sodium hydrogenphosphate, 0.2 g/l potassium chloride, 8 g/l sodium chloride and 0.1 g/l sodium azide at pH 7.0.
2.2 Sphere synthesis
2.2.1 Scheme 1
Spheres were synthesised following a modified version of the oil-in-water emulsion/solvent evaporation method used by T. Hickey [4]. 400 mg PLGA and 80 mg dexamethasone were co-dissolved in 40 ml dichloromethane:methanol 9:1. 5 ml fractions of this solution was added each to 100 ml 0.2% w/v PVA solution in ddH2O, and stirred at 1,250 rpm for 30 min. The resulting emulsion was left to stir at 60 rpm for a further 18 h so that the organic solvents could evaporate and let the spheres harden. The spheres were then recovered from solution by filtration, and washed on the filter with ddH2O to remove excess PVA and unencapsulated dexamethasone. The resulting slurry was dried fully in a lyophiliser over 24 h, producing a fine white powder.
2.2.2 Scheme 2
This scheme was aimed at synthesis of significantly smaller spheres. They were produced following a modified version of the route explored by Sahoo et al. [12]. About 500 mg PLGA and 100 mg dexamethasone were codissolved in 10 ml dichloromethane:methanol 9:1. This solution was added to 60 ml of 0.2% w/v PVA solution, and vortexed at 13,500 rpm for 6 min. The resulting milky white emulsion was sonicated at 20 W for a further 5 min, before being topped up to approx. 100 ml with more 0.2% PVA, and allowed to stir at 60 rpm overnight to harden. The resulting spheres were recovered by ultracentrifugation for 15 min at 18,000×g. The supernatant was poured off, and the resulting solids washed with ddH2O, resuspended, and centrifuged a second time, in order to remove excess PVA and unencapsulated dexamethasone. The resulting slurry was freeze dried as above.
2.3 Scanning electron microscopy (SEM) and size analysis
Pictures of each type of PLGA spheres were taken using a JEOL 5400 SEM at 10 kV after gold sputter coating. These were then submitted to visual analysis by AnalySIS software in order to produce a size distribution for each sample. At least 150 data points were used to get an accurate distribution of sizes. After the drug release experiment, samples of each type of degraded PLGA sphere were analysed by SEM.
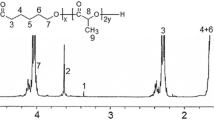
2.4 Drug loading efficiency
About 10 mg of each dried sphere type was dissolved in approx. 0.7 g acetonitrile. These samples were run on a High Performance Liquid Chromatography (HPLC) machine HPLC fitted with a reverse phase Varian Chromsphere C18 column (250 × 4.6 mm) with a running buffer of 60% acetonitrile, 40% sodium acetate buffer at pH 4.8. The concentration of dexamethasone was resolved using a Varian Prostar spectrometer reading at 254 nm, with a dexamethasone peak at 3.62 min. The drug loading efficiency (DLE) was calculated using the following formula:
The maximum encapsulation was taken to be the point where all the supplied dexamethasone was encapsulated in the spheres.
2.5 Release profile assay
About 60 mg of each sphere type were split between 3 separate samples of 25 ml PBS at pH 7.0 and incubated at 37°C, 30 rpm for the length of sampling. Samples of 1.7 ml were removed and filtered through a 220 nm polyester membrane to remove the PLGA spheres. The incubated sample was then topped up to 25 ml with fresh, filtered PBS.
Each removed sample was run on an HPLC as described above, with a dexamethasone peak at 3.62 min, and a peak corresponding to the simulated body fluid at 1.76 min.
3 Results and discussion
3.1 Spheres morphology
SEM images of the spheres produced by the two different synthesis schemes are shown in Fig. 1. A significant difference in the size of the two types of spheres was obtained. The images were further processed for size distribution and the findings are included in Fig. 2. In addition, the particles revealed a smooth outer surface and a regular spherical shape. A low surface roughness is important for extended drug release. Any irregularities will cause an increase in surface area, creating a much faster diffusive release of dexamethasone.
It is visible from the SEM images that the small spheres (Fig. 1b) are more agglomerated and clumped showing a more powder-like arrangement. Their visualization by SEM was relatively more difficult due to a high degree of charging and sample melting under the electron beam.
From the size analysis results (Fig. 2), it can be observed that the two different synthesis schemes generated separate size ranges: 20 ± 10 μm and 1.0 ± 0.4 μm, respectively. The distribution of sizes for the large sphere formulation was relatively broad and may be connected to the differences between the synthesis methods, for example the stirring speed. If the spheres were to be placed onto a metallic microtextured biomaterial, more of the underlying texture would be maintained when using the 1.0 μm spheres.
3.2 Drug loading efficiency
The drug loading efficiency for the 1.0 μm spheres was calculated to be 11.2% whereas for the 20 μm spheres, 0.9%. This difference is likely due to the increased emulsion surface area generated in the second synthesis scheme used for the small spheres, allowing more of the dexamethasone to remain incorporated within the PLGA matrix as it forms. During the first scheme, much of the dexamethasone is released into the aqueous component, where it likely forms microcrystalline deposits due to its extremely low partition coefficient. These deposits are lost in the washing steps.
3.3 Drug release profile
Over the course of 550 h (Fig. 3), the 20 μm spheres released 90% of their calculated yield of dexamethasone exhibiting a roughly linear profile, whilst the 1.0 μm spheres released 30% out of which 20% in very early stages (less than 25 h). A closer look at the release profile of the 20 μm spheres suggests the existence of three distinctive zones, namely the first 150 h, 150–300 h, and 300–550 h. For the first 150 h the relatively high release rates may be attributed to diffusion of dexamethasone from the sphere subsurface. In the next 150 h, the release slows drastically down to only 0.02%/h suggesting a depletion of dexamethasone from within the available diffusion distance from the surface. In the last 250 h a climb in release to an average of 0.23%/h was observed as the polymer is degraded following water inclusion into its structure thus allowing for a combined diffusion–degradation mechanism of dexamethasone release. Figures 4a, b show SEM images of the spheres after degradation for 550 h. A clear surface porosity for the spheres produced by scheme 1, and also some degree of particle swelling was visible (Fig. 4a). The release profile follows the trend previously shown by Hickey et al. [4] for 11 μm size PLGA spheres.
By going down with the size of the loaded spheres, significant changes occurred in the release profile of dexamethasone (Fig. 3). Initially, the 1.0 μm spheres released dexamethasone at a rate of 5% per hour, but this fell to just 0.02%/h after 25 h, and this rate of release was held on average from 25 h until the end of the experiment. This is in line with the trends in release shown in the literature [13]. Such a rapid initial burst can be mostly associated with diffusion from the outermost layers of the particle surface, as in the case with the burst for the 20 μm spheres. For the first 6 h the release for the 1.0 μm spheres was much faster than the 20 μm spheres, with a rate of almost 5%/h at its peak, against 0.6%/h for the 20 μm spheres over this time. This difference can be attributed to the difference in surface area per unit volume of the two particle sizes, allowing dexamethasone to diffuse faster from the smaller spheres due to the increased amount of polymer-water interfaces and decreased average path distance to solution. The possibility of some of the smaller spheres to start already undergoing degradation can not be excluded.
Additionally, by moving down with the size of the spheres, the proportion of released dexamethasone within the 550 h sampled was reduced from over 90–30%.
In the papers by Lu et al. [9] and Sahoo et al. [12] it is reported that the surface of PLGA particles produced by the methods used in this paper are coated by a stable layer of PVA. Also, as the particle size decreases, the amount of PVA associated with the surface increases because of the increased surface area per unit volume allowing more PVA to collect onto the sphere surface during synthesis. Once in the release experiment this thickened layer of PVA (associated with smaller particles) may cause an exterior hydrogel to occur around the spheres, acting as a diffusion barrier for encapsulated drugs and limiting their total release. This could be minimised by further optimising the synthesis procedure. Figure 4b shows a SEM image of the 1 μm spheres after 550 h of degradation. It can be clearly seen that there are undegraded spheres still associated with PVA after this time. However, the amount of spheres still visible was significantly less than the initial quantity in the sample, suggesting that the 1 μm spheres were entirely degraded when free in solution.
When comparing the two types of spheres in the view of a possible application for medical combination devices, the 20 μm spheres may offer some advantages as they are less likely to be removed from the desired peri-implant area (for example in case they become detached from the device surface) or rapidly broken down by an immune response. The drug release profile makes them feasible for applications where a sustained release is needed over a longer period (in this case about 23 days). However, the drug loading efficiency is low.
The 1.0 μm spheres show a much higher drug loading efficiency reducing the amount of polymer matrix needed to get the same amount of drug released. Being significantly smaller in size, this formulation can maintain more of the initial implant surface texture, and would have more surface area contact with the implant, reducing the probability of being removed physically from the implant surface. The system exhibited a burst release of the drug (about 20% in one day) and the total amount of drug released over the 550 h period represented only about 30% of the loaded dexamethasone. Therefore, further work has to be performed in order to increase the percentage of drug released and, when required, extend the duration of the release. Factors such as lactide:glycolide ratio [3, 6] and polymer molecular weight are affecting the rate of diffusion [7] and could be investigated in regard to prolonging drug release. In addition, investigation into the use of an alternative emulsifier should also be performed, as it is possible that the PVA used in this study could have contributed to the low total yield released from the 1.0 μm spheres.
With regard to the effect of dexamethasone on osteoblast cells, previous work [11] has shown that a concentration of 10 μM is suitable for differentiation over a period of 28 days. Both sizes of sphere easily produce a concentration of over 10 μM within the primary layer of cells within the first hour after implantation. However, the larger, slower releasing spheres seem to be more suitable for inducing osteoblast differentiation, as it is important to maintain adequate concentrations to these cells over as much of the full period of 28 days as possible to induce a cellular response.
It has been shown [14] that a dose of 0.5 μg/mm2 is necessary for immunosuppression in the vicinity of bioimplants. With the spheres produced by these means such doses can be achieved. It would require a loading of about 0.05 mg/mm2 of the 20 μm spheres, or only 0.005 mg/mm2 of the 1 μm spheres due to the increased drug loading efficiency of the smaller spheres. It is interesting to note that the fundamental immune response is primarily within the first few hours to days of implantation [1], and thus a high dose of dexamethasone would be advised through this period. This would be an excellent use of the 1 μm spheres. Follow-up studies will be performed to investigate the drug release kinetics for such a system from a solid substrate.
4 Conclusions
Two different sizes (i.e. 20 and 1.0 μm) of PLGA spheres loaded with dexamethasone were produced by the oil-in-water emulsion/solvent evaporation method using two synthesis schemes. Their morphology, drug loading efficiency and drug release profile were investigated and compared. Dexamethasone release was monitored in phosphate buffer saline solution at 37°C for a period of 550 h using the HPLC analysis.
The results indicated formation of spheres with two different and reproducible size ranges, uniform shape and smooth outer surfaces. The different size of the produced spheres affected significantly the drug loading efficiency, the release profiles and the doze of the released drug. The 1.0 μm formulation showed higher loading efficiency (11 vs. 1%), a burst release of the drug in the first day and a maximum of about 30% release of the encapsulated dexamethasone until the end of the 23 days experiment. In comparison, the 20 μm formulation exhibited an almost linear release profile with about 90% of the encapsulated drug being released by the end of the experiment. However, the drug loading efficiency was significantly lower. The main differences observed were explained taking into consideration the relatively higher amount of polymer-water interfaces generated during the synthesis of the 1.0 μm spheres that enabled more dexamethasone to be encapsulated in the resultant spheres. Similarly, during the release phase, the larger surface area per unit volume favored faster water inclusion into the polymer and therefore easier drug diffusion and possible polymer scission.
Both formulations have attractive features for potential use in medical combination devices to control osteoblast differentiation and/or immune suppression in the peri-implant area. In order to achieve both effects, a combined system of large and small spheres immobilized on the implant surface could be a solution.
References
J.M. Anderson, M.S. Shive, Adv. Drug Deliv. Rev. 28, 5 (1997). doi:10.1016/S0169-409X(97)00048-3
A.A. Ignatius, L.E. Claes, Biomaterials 17, 831 (1996). doi:10.1016/0142-9612(96)81421-9
X.S. Wu, N. Wang, J. Biomater. Sci. Polym. Ed. 12, 21 (2001). doi:10.1163/156856201744425
T. Hickey, D. Kreutzer, D.J. Burgess, F. Moussy, J. Biomed. Mater. Res. 61, 180 (2002). doi:10.1002/jbm.10016
U. Bilati, E. Allemann, E. Doelker, Eur. J. Pharm. Biopharm. 59, 375 (2005). doi:10.1016/j.ejpb.2004.10.006
G.B. Wei, G.J. Pettway, L.K. McCauley, P.X. Ma, Biomaterials 25, 345 (2004). doi:10.1016/S0142-9612(03)00528-3
S. Jaraswekin, S. Prakongpan, R. Bodmeier, J. Microencapsul. 24, 117 (2007). doi:10.1080/02652040701233655
T. Hickey, D. Kreutzer, D.J. Burgess, F. Moussy, Biomaterials 23, 1649 (2002). doi:10.1016/S0142-9612(01)00291-5
J. Liu, S.M. Zhang, P.P. Chen, L. Cheng, W. Zhou, W.X. Tang, Z.W. Chen, C.M. Ke, J. Mater. Sci. Mater. Med. 18, 2205 (2007). doi:10.1007/s10856-007-3010-0
D.H.R. Kempen, L. Lu, T.E. Hefferan, L.B. Creemers, A. Maran, K.L. Classic, W.J.A. Dhert, M.J. Yaszemski, Biomaterials 29, 3245 (2008). doi:10.1016/j.biomaterials.2008.04.031
M. Jager, J. Fischer, W. Dohrn, X.N. Li, D.C. Ayers, A. Czibere, W.C. Prall, S. Lensing-Hohn, R. Krauspe, J. Orthop. Res. 26, 1440 (2008). doi:10.1002/jor.20565
S.K. Sahoo, J. Panyam, S. Prabha, V. Labhasetwar, J. Control. Release 82, 105 (2002). doi:10.1016/S0168-3659(02)00127-X
C. Gomez-Graete, N. Tsapis, M. Besnard, A. Bochot, E. Fattal, Int. J. Pharm. 331, 153 (2007). doi:10.1016/j.ijpharm.2006.11.028
B.S.F. Santiago Jimenez-Valero, Catheter. Cardiovasc. Interv. 70, 492 (2007). doi:10.1002/ccd.21131
Acknowledgements
The support of Michel van der Brink from the Laboratory for Process Equipment (TU Delft) for the scanning electron microscopy investigations is greatly appreciated.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dawes, G.J.S., Fratila-Apachitei, L.E., Mulia, K. et al. Size effect of PLGA spheres on drug loading efficiency and release profiles. J Mater Sci: Mater Med 20, 1089–1094 (2009). https://doi.org/10.1007/s10856-008-3666-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-008-3666-0