Abstract
Traditional wound dressings are essential for the treatment of acute and superficial wounds. However, complex wounds require the use of bioactive dressings that promote healing alongside providing a safe barrier for the coverage of the wound site. The addition of growth factors is usually the primary choice to fabricate functionalized wound dressing. However, it is also the main reason for the increase in the cost of a wound dressing and may be associated with several drawbacks, such as the need for a precise drug delivery system to be able to be administered at a narrow effective dose range. 2-deoxy-D-ribose (2dDR) is a cost-effective and promising pro-angiogenic agent that indirectly stimulates vascular endothelial growth factor production to stimulate angiogenesis, and consecutively accelerate wound healing. In this study, we aimed to fabricate a novel wound dressing from 2dDR-loaded decellularized spinach leaves and evaluated its bioactivity on human endothelial cells in vitro. Our results demonstrated that a biocompatible wound dressing biomaterial could successfully be fabricated via the decellularization of spinach leaves using chemical decellularization. The success of decellularization was confirmed quantitatively and qualitatively via determination of the DNA content and Fourier transform infrared spectroscopy, respectively. 2dDR was then easily incorporated into the dressings via physical absorption and released from them in 5 days. The release of 2dDR-releasing decellularized spinach leaves was observed to increase the viability and metabolic activity of human endothelial cells in vitro over 7 days. In conclusion, we demonstrated the fabrication of a novel functionalized biomaterial combining decellularized plant tissues with a promising pro-angiogenic agent, and 2dDR-loaded decellularized spinach leaves appear to have great potential to be used as a bioactive wound dressing to promote angiogenesis and, consecutively, wound healing.
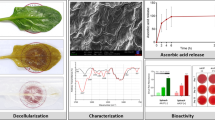
Graphical abstract








Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Andleeb A, Dikici S, Waris TS et al (2020) Developing affordable and accessible pro-angiogenic wound dressings; incorporation of 2 deoxy D-ribose (2dDR) into cotton fibres and wax-coated cotton fibres. J Tissue Eng Regen Med 14:973–988. https://doi.org/10.1002/term.3072
Azam M, Dikici S, Roman S et al (2019) Addition of 2-deoxy-d-ribose to clinically used alginate dressings stimulates angiogenesis and accelerates wound healing in diabetic rats. J Biomater Appl 34:463–475. https://doi.org/10.1177/0885328219859991
Mele E (2016) Electrospinning of natural polymers for advanced wound care: towards responsive and adaptive dressings. J Mater Chem B 4:4801–4812. https://doi.org/10.1039/c6tb00804f
Distler JHW, Hirth A, Kurowska-Stolarska M et al (2003) Angiogenic and angiostatic factors in the molecular control of angiogenesis. Q J Nucl Med 47:149–161. https://doi.org/10.1007/s00393-007-0172-6
Pierce GF, Vande Berg J, Rudolph R et al (1991) Platelet-derived growth factor-BB and transforming growth factor beta1 selectively modulate glycosaminoglycans, collagen, and myofibroblasts in excisional wounds. Am J Pathol 138:629–646
Takeshita S, Zheng LP, Brogi E et al (1994) Therapeutic angiogenesis. A single intraarterial bolus of vascular endothelial growth factor augments revascularization in a rabbit ischemic hind limb model. J Clin Investig 93:662–670. https://doi.org/10.1172/JCI117018
Grazul-Bilska AT, Johnson ML, Bilski JJ et al (2003) Wound healing: the role of growth factors. Drugs Today 39:787–800. https://doi.org/10.1358/dot.2003.39.10.799472
Tonnesen MG, Feng X, Clark RAF (2000) Angiogenesis in wound healing. J Investig Dermatol Symp Proc 5:40–46. https://doi.org/10.1046/j.1087-0024.2000.00014.x
Jung SM, Yoon GH, Lee HC, Shin HS (2015) Chitosan nanoparticle/PCL nanofiber composite for wound dressing and drug delivery. J Biomater Sci Polym Ed 26:252–263. https://doi.org/10.1080/09205063.2014.996699
Croisier F, Atanasova G, Poumay Y, Jérôme C (2014) Polysaccharide-coated PCL nanofibers for wound dressing applications. Adv Healthc Mater 3:2032–2039. https://doi.org/10.1002/adhm.201400380
Augustine R, Kalarikkal N, Thomas S (2016) Electrospun PCL membranes incorporated with biosynthesized silver nanoparticles as antibacterial wound dressings. Appl Nanosci (Switzerland) 6:337–344. https://doi.org/10.1007/s13204-015-0439-1
Ignatova M, Manolova N, Markova N, Rashkov I (2009) Electrospun non-woven nanofibrous hybrid mats based on chitosan and PLA for wound-dressing applications. Macromol Biosci 9:102–111. https://doi.org/10.1002/mabi.200800189
Toncheva A, Paneva D, Manolova N, Rashkov I (2011) Electrospun poly(L-lactide) membranes containing a single drug or multiple drug system for antimicrobial wound dressings. Macromol Res 19:1310–1319. https://doi.org/10.1007/s13233-011-1206-0
Amini F, Semnani D, Karbasi S, Banitaba SN (2019) A novel bilayer drug-loaded wound dressing of PVDF and PHB/Chitosan nanofibers applicable for post-surgical ulcers. Int J Polym Mater Polym Biomater 68:772–777. https://doi.org/10.1080/00914037.2018.1506982
Francis L, Meng D, Locke IC et al (2016) Novel poly(3-hydroxybutyrate) composite films containing bioactive glass nanoparticles for wound healing applications. Polym Int 65:661–674. https://doi.org/10.1002/pi.5108
Ndlovu SP, Ngece K, Alven S, Aderibigbe BA (2021) Gelatin-based hybrid scaffolds: promising wound dressings. Polymers (Basel) 13:2959. https://doi.org/10.3390/polym13172959
Lee SB, Kim YH, Chong MS et al (2005) Study of gelatin-containing artificial skin V: fabrication of gelatin scaffolds using a salt-leaching method. Biomaterials 26:1961–1968. https://doi.org/10.1016/j.biomaterials.2004.06.032
Ramnath V, Sekar S, Sankar S et al (2012) Preparation and evaluation of biocomposites as wound dressing material. J Mater Sci Mater Med 23:3083–3095. https://doi.org/10.1007/s10856-012-4765-5
Gipson IK, Spurr-Michaud SJ, Tisdale AS (1988) Hemidesmosomes and anchoring fibril collagen appear synchronously during development and wound healing. Dev Biol 126:253–262. https://doi.org/10.1016/0012-1606(88)90136-4
Samadian H, Salehi M, Farzamfar S et al (2018) In vitro and in vivo evaluation of electrospun cellulose acetate/gelatin/hydroxyapatite nanocomposite mats for wound dressing applications. Artif Cells Nanomed Biotechnol 46:964–974. https://doi.org/10.1080/21691401.2018.1439842
Shahzadi L, Yar M, Jamal A et al (2016) Triethyl orthoformate covalently cross-linked chitosan-(poly vinyl) alcohol based biodegradable scaffolds with heparin-binding ability for promoting neovascularisation. J Biomater Appl 31:582–593. https://doi.org/10.1177/0885328216650125
Yar M, Gigliobianco G, Shahzadi L et al (2016) Production of chitosan PVA PCL hydrogels to bind heparin and induce angiogenesis. Int J Polym Mater Polym Biomater 65:466–476. https://doi.org/10.1080/00914037.2015.1129959
Bölgen N, Demir D, Yalçın MS, Özdemir S (2020) Development of Hypericum perforatum oil incorporated antimicrobial and antioxidant chitosan cryogel as a wound dressing material. Int J Biol Macromol 161:1581–1590. https://doi.org/10.1016/j.ijbiomac.2020.08.056
Pal P, Dadhich P, Srivas PK et al (2017) Bilayered nanofibrous 3D hierarchy as skin rudiment by emulsion electrospinning for burn wound management. Biomater Sci 5:1786–1799. https://doi.org/10.1039/c7bm00174f
Dong RH, Jia YX, Qin CC et al (2016) In situ deposition of a personalized nanofibrous dressing via a handy electrospinning device for skin wound care. Nanoscale 8:3482–3488. https://doi.org/10.1039/c5nr08367b
Dikici S, Aldemir Dikici B, Macneil S, Claeyssens F (2021) Decellularised extracellular matrix decorated PCL PolyHIPE scaffolds for enhanced cellular activity, integration and angiogenesis. Biomater Sci 9:7297–7310. https://doi.org/10.1039/d1bm01262b
Koosehgol S, Ebrahimian-Hosseinabadi M, Alizadeh M, Zamanian A (2017) Preparation and characterization of in situ chitosan/polyethylene glycol fumarate/thymol hydrogel as an effective wound dressing. Mater Sci Eng, C 79:66–75. https://doi.org/10.1016/j.msec.2017.05.001
Schmitt T, Katz N, Kishore V (2021) A feasibility study on 3D bioprinting of microfat constructs towards wound healing applications. Front Bioeng Biotechnol 9:642. https://doi.org/10.3389/fbioe.2021.707098
Shafiee A, Cavalcanti AS, Saidy NT et al (2021) Convergence of 3D printed biomimetic wound dressings and adult stem cell therapy. Biomaterials 268:120558. https://doi.org/10.1016/j.biomaterials.2020.120558
Yu Y, Alkhawaji A, Ding Y, Mei J (2016) Decellularized scaffolds in regenerative medicine. Oncotarget 7:58671–58683. https://doi.org/10.18632/oncotarget.10945
Badylak SF (2004) Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol 12:367–377. https://doi.org/10.1016/j.trim.2003.12.016
Uygun BE, Soto-Gutierrez A, Yagi H et al (2010) Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nat Med 16:814–820. https://doi.org/10.1038/nm.2170
Sarig U, Au-Yeung GCT, Wang Y et al (2012) Thick acellular heart extracellular matrix with inherent vasculature: a potential platform for myocardial tissue regeneration. Tissue Eng Part A 18:2125–2137. https://doi.org/10.1089/ten.TEA.2011.0586
Dew L, English WR, Chong CK, MacNeil S (2016) Investigating neovascularization in rat decellularized intestine: An in vitro platform for studying angiogenesis. Tissue Eng Part A 22:1317–1326. https://doi.org/10.1089/ten.tea.2016.0131
Melo E, Kasper JY, Unger RE et al (2015) Development of a bronchial wall model: triple culture on a decellularized porcine trachea. Tissue Eng Part C Methods 21:909–921. https://doi.org/10.1089/ten.TEC.2014.0543
Sabetkish S, Kajbafzadeh AM, Sabetkish N et al (2015) Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix liver scaffolds. J Biomed Mater Res A 103:1498–1508. https://doi.org/10.1002/jbm.a.35291
Modulevsky DJ, Cuerrier CM, Pelling AE (2016) Biocompatibility of subcutaneously implanted plant-derived cellulose biomaterials. PLoS ONE 11:e0157894. https://doi.org/10.1371/journal.pone.0157894
Helenius G, Bäckdahl H, Bodin A et al (2006) In vivo biocompatibility of bacterial cellulose. J Biomed Mater Res A 76:431–438. https://doi.org/10.1002/jbm.a.30570
Fontana JD, De Souza AM, Fontana CK et al (1990) Acetobacter cellulose pellicle as a temporary skin substitute. Appl Biochem Biotechnol 24–25:253–264. https://doi.org/10.1007/BF02920250
Gershlak JR, Hernandez S, Fontana G et al (2017) Crossing kingdoms: using decellularized plants as perfusable tissue engineering scaffolds. Biomaterials 125:13–22. https://doi.org/10.1016/j.biomaterials.2017.02.011
Dikici S, Claeyssens F, MacNeil S (2019) Decellularised baby spinach leaves and their potential use in tissue engineering applications: studying and promoting neovascularisation. J Biomater Appl 34:546–559. https://doi.org/10.1177/0885328219863115
Toker M, Rostami S, Kesici M et al (2020) Decellularization and characterization of leek: a potential cellulose-based biomaterial. Cellulose 27:7331–7348. https://doi.org/10.1007/s10570-020-03278-4
Walawalkar S, Almelkar S (2021) Fabricating a pre-vascularized large-sized metabolically-supportive scaffold using Brassica oleracea leaf. J Biomater Appl 36:165–178. https://doi.org/10.1177/0885328220968388
Gorbenko N, Rinaldi G, Sanchez A, Merna N (2023) Small-caliber vascular grafts engineered from decellularized leaves and cross-linked gelatin. Tissue Eng Part A 29:397–409. https://doi.org/10.1089/ten.tea.2022.0223
Contessi Negrini N, Toffoletto N, Farè S, Altomare L (2020) Plant tissues as 3D natural scaffolds for adipose, bone and tendon tissue regeneration. Front Bioeng Biotechnol 8:723. https://doi.org/10.3389/fbioe.2020.00723
Yancopoulos GD, Davis S, Gale NW et al (2000) Vascular-specific growth factors and blood vessel formation. Nature 407:242–248. https://doi.org/10.1038/35025215
Cao R, Eriksson A, Kubo H et al (2004) Comparative evaluation of FGF-2-, VEGF-A-, and VEGF-C-induced angiogenesis lymphangiogenesis, vascular fenestrations, and permeability. Circ Res 94:664–670. https://doi.org/10.1161/01.RES.0000118600.91698.BB
Cheng SY, Nagane M, Huang HS, Cavenee WK (1997) Intracerebral tumor-associated hemorrhage caused by overexpression of the vascular endothelial growth factor isoforms VEGF121 and VEGF165 but not VEGF189. Proc Natl Acad Sci U S A 94:12081–12087. https://doi.org/10.1073/pnas.94.22.12081
Priestle JP, Paris CG (1996) Experimental techniques and data banks. In: Guidebook on Molecular Modeling in Drug Design. pp 139–217
Finnis C, Dodsworth N, Pollitt CE et al (1993) Thymidine phosphorylase activity of platelet-derived endothelial cell growth factor is responsible for endothelial cell mitogenicity. Eur J Biochem. https://doi.org/10.1111/j.1432-1033.1993.tb17651.x
Sengupta S, Sellers LA, Matheson HB, Fan TPD (2003) Thymidine phosphorylase induces angiogenesis in vivo and in vitro: an evaluation of possible mechanisms. Br J Pharmacol 139:219–231. https://doi.org/10.1038/sj.bjp.0705216
Dikici S, Yar M, Bullock AJ et al (2021) Developing wound dressings using 2-deoxy-d-ribose to induce angiogenesis as a backdoor route for stimulating the production of vascular endothelial growth factor. Int J Mol Sci 22:11437. https://doi.org/10.3390/ijms222111437
Dikici S (2022) A “sweet” way to increase the metabolic activity and migratory response of cells associated with wound healing: deoxy-sugar incorporated polymer fibres as a bioactive wound patch. Turk J Biol 46:41–56. https://doi.org/10.3906/biy-2108-27
Dikici S, Claeyssens F, MacNeil S (2020) Bioengineering vascular networks to study angiogenesis and vascularization of physiologically relevant tissue models in vitro. ACS Biomater Sci Eng 6:3513–3528. https://doi.org/10.1021/acsbiomaterials.0c00191
Dikici S, Mangir N, Claeyssens F et al (2019) Exploration of 2-deoxy-D-ribose and 17β-Estradiol as alternatives to exogenous VEGF to promote angiogenesis in tissue-engineered constructs. Regen Med 14:179–197. https://doi.org/10.2217/rme-2018-0068
Dikici S, Bullock AJ, Yar M et al (2020) 2-deoxy-D-ribose (2dDR) upregulates vascular endothelial growth factor (VEGF) and stimulates angiogenesis. Microvasc Res 131:104035. https://doi.org/10.1016/j.mvr.2020.104035
Dikici S, Aldemir Dikici B, Bhaloo SI et al (2019) Assessment of the angiogenic potential of 2-deoxy-D-ribose using a novel in vitro 3D dynamic model in comparison with established in vitro assays. Front Bioeng Biotechnol 7:451. https://doi.org/10.3389/fbioe.2019.00451
Aldemir Dikici B, Dikici S, Reilly GC et al (2019) A novel bilayer polycaprolactone membrane for guided bone regeneration: combining electrospinning and emulsion templating. Materials 12:2643. https://doi.org/10.1007/s10856-019-6332-9
Kanwar R, Rathee J, Salunke DB, Mehta SK (2019) Green nanotechnology-driven drug delivery assemblies. ACS Omega 4:8804–8815. https://doi.org/10.1021/acsomega.9b00304
Neishabouri A, Soltani Khaboushan A, Daghigh F et al (2022) Decellularization in tissue engineering and regenerative medicine: evaluation, modification, and application methods. Front Bioeng Biotechnol 10:805299. https://doi.org/10.3389/fbioe.2022.805299
Fontana G, Gershlak J, Adamski M et al (2017) Biofunctionalized plants as diverse biomaterials for human cell culture. Adv Healthc Mater 6:1–16. https://doi.org/10.1002/adhm.201601225
Modulevsky DJ, Lefebvre C, Haase K et al (2014) Apple derived cellulose scaffolds for 3D mammalian cell culture. PLoS ONE. https://doi.org/10.1371/journal.pone.0097835
Salehi A, Mobarhan MA, Mohammadi J et al (2020) Efficient mineralization and osteogenic gene overexpression of mesenchymal stem cells on decellularized spinach leaf scaffold. Gene 757:144852. https://doi.org/10.1016/j.gene.2020.144852
Jansen K, Evangelopoulou M, Pou Casellas C et al (2021) Spinach and chive for kidney tubule engineering: the limitations of decellularized plant scaffolds and vasculature. AAPS J 23:11. https://doi.org/10.1208/s12248-020-00550-0
Stavolone L, Lionetti V (2017) Extracellular matrix in plants and animals: hooks and locks for viruses. Front Microbiol 8:1760. https://doi.org/10.3389/fmicb.2017.01760
Roberts K (1989) The plant extracellular matrix. Curr Opin Cell Biol 1:1020–1027. https://doi.org/10.1016/0955-0674(89)90074-4
Harris AF, Lacombe J, Liyanage S et al (2021) Supercritical carbon dioxide decellularization of plant material to generate 3D biocompatible scaffolds. Sci Rep 11:3643. https://doi.org/10.1038/s41598-021-83250-9
Modulevsky DJ, Lefebvre C, Haase K et al (2014) Apple derived cellulose scaffolds for 3D mammalian cell culture. PLoS ONE 9:e97835. https://doi.org/10.1371/journal.pone.0097835
Cheng YW, Shiwarski DJ, Ball RL et al (2020) Engineering aligned skeletal muscle tissue using decellularized plant-derived scaffolds. ACS Biomater Sci Eng 6:3046–3054. https://doi.org/10.1021/acsbiomaterials.0c00058
Mitchell SM, Pajovich HT, Broas SM et al (2022) Molecular dynamics simulations and in vitro studies of hybrid decellularized leaf-peptide-polypyrrole composites for potential tissue engineering applications. J Biomol Struct Dyn. https://doi.org/10.1080/07391102.2021.2023643
Schwartz SJ, von Elbe JH (1983) Kinetics of chlorophyll degradation to pyropheophytin in vegetables. J Food Sci 48:1303–1306. https://doi.org/10.1111/j.1365-2621.1983.tb09216.x
Aldemir Dikici B, Reilly GC, Claeyssens F (2020) Boosting the osteogenic and angiogenic performance of multiscale porous polycaprolactone scaffolds by in vitro generated extracellular matrix decoration. ACS Appl Mater Interfaces 12:12510–12524. https://doi.org/10.1021/acsami.9b23100
Han Y, Han L, Yao Y et al (2018) Key factors in FTIR spectroscopic analysis of DNA: the sampling technique, pretreatment temperature and sample concentration. Anal Methods 10:2436–2443. https://doi.org/10.1039/C8AY00386F
Chen H (2014) Chemical composition and structure of natural lignocellulose. In: Biotechnology of Lignocellulose: Theory and Practice. Chemical Industry Press, Beijing, p 25–71
Bilirgen AC, Toker M, Odabas S et al (2021) Plant-based scaffolds in tissue engineering. ACS Biomater Sci Eng 7:926–938. https://doi.org/10.1021/acsbiomaterials.0c01527
Jorfi M, Foster EJ (2015) Recent advances in nanocellulose for biomedical applications. J Appl Polym Sci 132:41719. https://doi.org/10.1002/app.41719
Miyamoto T, Takahashi S, Ito H et al (1989) Tissue biocompatibility of cellulose and its derivatives. J Biomed Mater Res 23:125–133. https://doi.org/10.1002/jbm.820230110
Lee J, Jung H, Park N et al (2019) Induced osteogenesis in plants decellularized scaffolds. Sci Rep 9:20194. https://doi.org/10.1038/s41598-019-56651-0
Saito T, Kimura S, Nishiyama Y, Isogai A (2007) Cellulose nanofibers prepared by TEMPO-mediated oxidation of native cellulose. Biomacromol 8:2485–2491. https://doi.org/10.1021/bm0703970
Kumar V, Yang T (2002) HNO3/H3PO4–NANO2 mediated oxidation of cellulose—preparation and characterization of bioabsorbable oxidized celluloses in high yields and with different levels of oxidation. Carbohydr Polym 48:403–412. https://doi.org/10.1016/S0144-8617(01)00290-9
Entcheva E, Bien H, Yin L et al (2004) Functional cardiac cell constructs on cellulose-based scaffolding. Biomaterials 25:5753–5762. https://doi.org/10.1016/j.biomaterials.2004.01.024
Liao S, Wang W, Uo M et al (2005) A three-layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane for guided tissue regeneration. Biomaterials 26:7564–7571. https://doi.org/10.1016/j.biomaterials.2005.05.050
Das AAK, Bovill J, Ayesh M et al (2016) Fabrication of living soft matter by symbiotic growth of unicellular microorganisms. J Mater Chem B 4:3685–3694. https://doi.org/10.1039/C5TB02489G
Betlej I, Salerno-Kochan R, Krajewski KJ et al (2020) The influence of culture medium components on the physical and mechanical properties of cellulose synthesized by kombucha microorganisms. BioResources 15:3125–3135. https://doi.org/10.15376/biores.15.2.3125-3135
Bai Z, Dan W, Yu G et al (2018) Tough and tissue-adhesive polyacrylamide/collagen hydrogel with dopamine-grafted oxidized sodium alginate as crosslinker for cutaneous wound healing. RSC Adv 8:42123–42132. https://doi.org/10.1039/C8RA07697A
Kong Y, Tang X, Zhao Y et al (2020) Degradable tough chitosan dressing for skin wound recovery. Nanotechnol Rev 9:1576–1585. https://doi.org/10.1515/ntrev-2020-0105
Jin SG, Kim KS, Yousaf AM et al (2015) Mechanical properties and in vivo healing evaluation of a novel Centella asiatica-loaded hydrocolloid wound dressing. Int J Pharm 490:240–247. https://doi.org/10.1016/j.ijpharm.2015.05.058
Minsart M, Van Vlierberghe S, Dubruel P, Mignon A (2022) Commercial wound dressings for the treatment of exuding wounds: an in-depth physico-chemical comparative study. Burns Trauma 10:tkac024. https://doi.org/10.1093/burnst/tkac024
Ajiteru O, Lee OJ, Kim J-H et al (2022) Fabrication and characterization of a myrrh hydrocolloid dressing for dermal wound healing. Colloid Interface Sci Commun 48:100617. https://doi.org/10.1016/j.colcom.2022.100617
Yar M, Shahzadi L, Mehmood A et al (2017) Deoxy-sugar releasing biodegradable hydrogels promote angiogenesis and stimulate wound healing. Mater Today Commun 13:295–305. https://doi.org/10.1016/j.mtcomm.2017.10.015
Burkhardt F, Spies BC, Wesemann C et al (2022) Cytotoxicity of polymers intended for the extrusion-based additive manufacturing of surgical guides. Sci Rep 12:7391. https://doi.org/10.1038/s41598-022-11426-y
Acknowledgements
The authors acknowledge the Izmir Institute of Technology (IZTECH BAP) Research Foundation (Grant no: 2021IYTE-1-0057) and Health Institutes of Türkiye (TUSEB) (Grant no: 2023-A4-01-31614) for financially supporting this study.
Author information
Authors and Affiliations
Contributions
SD contributed to the experimental design, analysis, data acquisition, interpretation of data, statistical analysis, and drafting of the manuscript. ÇÇ contributed to the experimental design, analysis, data acquisition, interpretation of data, and drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Ethical approval
Not applicable.
Additional information
Handling Editor: Stephen Eichhorn.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dikici, S., Çavdaroğlu, Ç. Development of pro-angiogenic wound dressings from 2-deoxy-D-ribose (2dDR)-loaded decellularized plant leaves. J Mater Sci 58, 16428–16444 (2023). https://doi.org/10.1007/s10853-023-09064-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-023-09064-4