Abstract
Background or Purpose
Superior vena cava isolation (SVCI) is widely performed adjunctively to atrial fibrillation (AF) ablation. Right phrenic nerve injury (PNI) is a complication of this procedure. The purpose of the study is to determine the optimal PNI prevention method in SVCI.
Methods
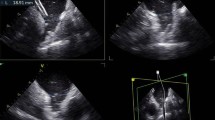
A total of 1656 patients who underwent SVCI between 2009 and 2022 were retrospectively examined. PNI was diagnosed based on the diaphragm position and movement in the upright position on chest radiographs before and after SVCI.
Results
With the introduction of various PN monitoring systems over the years, the incidence of SVCI-associated PNI has decreased. However, complete PNI avoidance has not been achieved. PNI incidence according to fluoroscopy-guided PN monitoring, high-output pace-guided, compound motor action potential-guided, and 3-dimensional electro-anatomical mapping (EAM) systems was 8.1% (38/467), 2.7% (13/476), 2.4% (4/130), and 2.8% (11/389), respectively. However, a high-power, short-duration (50 W/7 s) radiofrequency (RF) energy application only on PNI risk points tagged by a 3-dimensional EAM system completely avoids PNI (0%; 0 /160 since April 2021). PNI showed no symptoms and recovered within an average of 188 days post-SVCI, except for a few patients who required > 1 year.
Conclusions
Although PNI incidence decreased annually with the introduction of various monitoring systems, these monitoring systems did not prevent PNI completely. Most notably, the delivery of a high-power, short-duration RF energy only on risk points tagged by EAM prevented PNI completely. PNI recovered in all patients. The application of higher-power, shorter-duration RF energy on risk points tagged by EAM appears to be an optimal PNI prevention maneuver.






Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- PNI:
-
Phrenic nerve injury
- HPSD:
-
High-power, short-duration
- LPLD:
-
Low-power, long-duration
- SVC:
-
Superior vena cava
- SVCI:
-
Superior vena cava isolation
- CA:
-
Catheter ablation
- AF:
-
Atrial fibrillation
- PV:
-
Pulmonary vein
- PVI:
-
Pulmonary vein isolation
- LA:
-
Left atrium
- CMAP:
-
Compound motor action potential
- 3D:
-
Three-dimensional
- EAM:
-
Electro-anatomical mapping
References
Tsai CF, Tai CT, Hsieh MH, Lin WS, Yu WC, Ueng KC, et al. Initiation of atrial fibrillation by ectopic beats originating from the superior vena cava: electrophysiological characteristics and results of radiofrequency ablation. Circulation. 2000;102:67–74.
Shah D, Haissaguerre M, Jais P, Hocini M. Nonpulmonary vein foci: do they exist? Pacing Clin Electrophysiol. 2003;26:1631–5.
Miyazaki S, Takigawa M, Kusa S, Kuwahara T, Taniguchi H, Okubo K, et al. Role of arrhythmogenic superior vena cava on atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25:380–6.
Miyazaki S, Taniguchi H, Kusa S, Ichihara N, Nakamura H, Hachiya H, et al. Factors predicting an arrhythmogenic superior vena cava in atrial fibrillation ablation: insight into the mechanism. Heart Rhythm. 2014;11:1560–6.
Arruda M, Mlcochova H, Prasad SK, Kilicaslan F, Saliba W, Patel D, et al. Electrical isolation of the superior vena cava: an adjunctive strategy to pulmonary vein antrum isolation improving the outcome of AF ablation. J Cardiovasc Electrophysiol. 2007;18:1261–6.
Corrado A, Bonso A, Madalosso M, Rossillo A, Themistoclakis S, Di Biase L, et al. Impact of systematic isolation of superior vena cava in addition to pulmonary vein antrum isolation on the outcome of paroxysmal, persistent, and permanent atrial fibrillation ablation: results from a randomized study. J Cardiovasc Electrophysiol. 2010;21:1–5.
Kang KW, Pak HN, Park J, Park JG, Uhm JS, Joung B, et al. Additional linear ablation from the superior vena cava to right atrial septum after pulmonary vein isolation improves the clinical outcome in patients with paroxysmal atrial fibrillation: prospective randomized study. Europace. 2014;16:1738–45.
Ejima K, Kato K, Iwanami Y, Henmi R, Yagishita D, Manaka T, et al. Impact of an empiric isolation of the superior vena cava in addition to circumferential pulmonary vein isolation on the outcome of paroxysmal atrial fibrillation ablation. Am J Cardiol. 2015;116:1711–6.
Li JY, Jiang JB, Zhong GQ, Ke HH, He Y. Comparison of empiric isolation and conventional isolation of superior vena cava in addition to pulmonary vein isolation on the outcome of paroxysmal atrial fibrillation ablation. Int Heart J. 2017;58:500–5.
Zhang T, Wang Y, Liang Z, Zhao H, Han Z, Wang Y, et al. Effect of combined pulmonary vein and superior vena cava isolation on the outcome of second catheter ablation for paroxysmal atrial fibrillation. Am J Cardiol. 2020;125:1845–50.
Omuro T, Yoshiga Y, Ueyama T, Shimizu A, Ono M, Fukuda M, et al. An impact of superior vena cava isolation in non-paroxysmal atrial fibrillation patients with low voltage areas. J Arrhythm. 2021;37:965–74.
Overeinder I, Osorio TG, Calburean PA, Bisignani A, Bala G, Sieira J, et al. Comparison between superior vena cava ablation in addition to pulmonary vein isolation and standard pulmonary vein isolation in patients with paroxysmal atrial fibrillation with the cryoballoon technique. J Interv Card Electrophysiol. 2021;62:579–86.
Chang HY, Lo LW, Lin YJ, Chang SL, Hu YF, Feng AN, et al. Long-term outcome of catheter ablation in patients with atrial fibrillation originating from the superior vena cava. J Cardiovasc Electrophysiol. 2012;23:955–61.
Knecht S, Zeljkovic I, Badertscher P, et al. Role of empirical isolation of the superior vena cava in patients with recurrence of atrial fibrillation after pulmonary vein isolatio—a multi-center analysis. J Interv Card Electrophysiol 2022 Aug 18. https://doi.org/10.1007/s10840-022-01314-w.
Sanchez-Quintana D, Cabrera JA, Climent V, Farre J, Weiglein A, Ho SY. How close are the phrenic nerves to cardiac structures? Implications for cardiac interventionalists. J Cardiovasc Electrophysiol. 2005;16:309–13.
Sacher F, Monahan KH, Thomas SP, Davidson N, Adragao P, Sanders P, et al. Phrenic nerve injury after atrial fibrillation catheter ablation: characterization and outcome in a multicenter study. J Am Coll Cardiol. 2006;47:2498–503.
Franceschi F, Dubuc M, Guerra PG, Khairy P. Phrenic nerve monitoring with diaphragmatic electromyography during cryoballoon ablation for atrial fibrillation: the first human application. Heart Rhythm. 2011;8:1068–71.
Murakami T, Yamaji H, Numa K, Kawamura H, Murakami M, Higashiya S, et al. Adaptive-servo ventilation combined with deep sedation is an effective strategy during pulmonary vein isolation. Europace. 2013;15:951–6.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Europace. 2018;20:157–208.
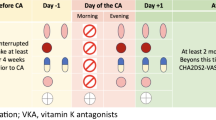
Yamaji H, Murakami T, Hina K, Higashiya S, Kawamura H, Murakami M, et al. Usefulness of dabigatran etexilate as periprocedural anticoagulation therapy for atrial fibrillation ablation. Clin Drug Investig. 2013;33:409–18.
Goyal R, Gracia E, Fan R. The role of superior vena cava isolation in the management of atrial fibrillation. J Innov Card Rhythm Manag. 2017;8:2674–80.
Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics. 2012;32:E51-70.
Bhaskaran A, Chik W, Pouliopoulos J, Nalliah C, Qian P, Barry T, et al. Five seconds of 50–60 W radio frequency atrial ablations were transmural and safe: an in vitro mechanistic assessment and force-controlled in vivo validation. Europace. 2017;19:874–80.
Kusa S, Hachiya H, Sato Y, Hara S, Ohya H, Miwa N, et al. Superior vena cava isolation with 50 W high power, short duration ablation strategy. J Cardiovasc Electrophysiol. 2021;32:1602–9.
Parikh V, Kowalski M. Comparison of phrenic nerve injury during atrial fibrillation ablation between different modalities, pathophysiology and management. J Atr Fibrillation. 2015;8:1314.
Bai R, Patel D, Di Biase L, Fahmy TS, Kozeluhova M, Prasad S, et al. Phrenic nerve injury after catheter ablation: should we worry about this complication? J Cardiovasc Electrophysiol. 2006;17:944–8.
Tripp HF, Bolton JW. Phrenic nerve injury following cardiac surgery: a review. J Card Surg. 1998;13:218–23.
Author information
Authors and Affiliations
Contributions
(1) Substantial contributions to the conception and design or to the acquisition, analysis, or interpretation of the data: H.Y., S.H., T.M, H.K., M.M., S.K., and S.K.
(2) Substantial contributions to the drafting of the articles or critical revision of important intellectual content: H.Y., H.K., S.H., and S.K.
(3) Final approval of the version to be published: all authors.
(4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved: H.Y., S.H., T.M, H.K., M.M., S.K., and S.K.
Corresponding author
Ethics declarations
Ethics approval
Our study complied with the principles of the Declaration of Helsinki and was approved by the Institutional Ethics Committee for Human Research of the Okayama Heart Clinic.
Consent to participate
Written informed consent for the use of data without personally identifiable information was obtained from all patients.
Permission to reproduce material from other sources
This study did not reproduce any material from other sources.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamaji, H., Higashiya, S., Murakami, T. et al. Optimal prevention method of phrenic nerve injury in superior vena cava isolation: efficacy of high-power, short-duration radiofrequency energy application on the risk points. J Interv Card Electrophysiol 66, 1465–1475 (2023). https://doi.org/10.1007/s10840-022-01449-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01449-w