Abstract
Background
Focal atrial tachycardias (ATs) represent 5–15% of sustained supraventricular tachycardias (SVTs). Characteristic distribution of sites of origin and detailed electrophysiologic characterization of AT from specific sites of origin (SOO) have been described. Acute success and recurrence are less favorable than for other SVTs. In this series, we present our experience of focal AT ablation over a 10-year period.
Methods
We undertook a retrospective review of an electronically maintained database of all patients undergoing AT ablation at our institution between January 2011 and December 2020. Demographic, procedural, and outcomes data were reviewed.
Results
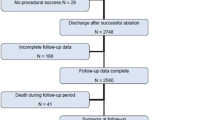
A total of 293 distinct atrial tachycardias were treated during 279 procedures in 256 patients, including 207 first AT ablations. Acutely successful AT suppression was achieved in 91% of first-time ablations. Acute success was dependent on SOO of AT with lowest rates of acute suppression in the para-Hisian region and the crista terminalis (CT). The most common reason for failure to acutely suppress the AT was proximity to a critical structure (phrenic nerve, sinus node, and AV node). 8.9% of patients in this series presented with a tachycardia-mediated cardiomyopathy (TCM). 48% of TCM patients underwent an ablation attempt during an acute medical admission. Among the TCM group, median LV ejection fraction increased from 25% (range 10–50%) to 55% (range 35–65%) with successful treatment of AT. Five patients undergoing a repeat procedure had planned pericardial access for displacement of the phrenic nerve to permit ablation of the AT, which was successful in all cases. Among patients without a pre-existing diagnosis of AF, peri-procedural AF was not associated with a higher incidence of a subsequent diagnosis of AF (odds ratio 1.169, 95% CI 0.4058–3.475, p = 0.7628). Median duration of follow-up was 832 days. By Kaplan–Meier estimate, recurrence-free survival was 78% (95% CI 67–88%).
Conclusions
In this series, focal AT ablation is associated with good acute results and a low rate of complications, but outcomes remain less favorable than previously reported for other forms of SVT.




Similar content being viewed by others
References
Roberts-Thomson KC, Kistler PM, Kalman JM. Focal atrial tachycardia I: clinical features, diagnosis, mechanisms, and anatomic location. Pacing Clin Electrophysiol. 2006;29:643–52.
Saoudi N, Cosío F, Waldo A, et al. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical bases: a statement from a joint expert group from the working group of arrhythmias of the European society of cardiology and the North American society of pacing and electrophysiology. Eur Heart J. 2001;22:1162–82.
Kalman JM, Olgin JE, Karch MR, Hamdan M, Lee RJ, Lesh MD. “Cristal tachycardias”: origin of right atrial tachycardias from the crista terminalis identified by intracardiac echocardiography. J Am Coll Cardiol. 1988;31:451–9.
Morris GM, Segan L, Wong G, et al. Atrial tachycardia arising from the crista terminalis, detailed electrophysiological features and long-term ablation outcomes. JACC Clin Electrophysiol. 2019;5:448–58.
Morton JB, Sanders P, Das A, Vohra JK, Sparks PB, Kalman JM. Focal atrial tachycardia arising from the tricuspid annulus: electrophysiologic and electrocardiographic characteristics. 2001.
Kistler PM, Sanders P, Hussin A, et al. Focal atrial tachycardia arising from the mitral annulus: electrocardiographic and electrophysiologic characterization. J Am Coll Cardiol. 2003;41:2212–9.
Kistler PM, Fynn SP, Haqqani H, et al. Focal atrial tachycardia from the ostium of the coronary sinus: electrocardiographic and electrophysiological characterization and radiofrequency ablation. J Am Coll Cardiol. 2005;45:1488–93.
Badhwar N, Kalman JM, Sparks PB, et al. Atrial tachycardia arising from the coronary sinus musculature: electrophysiological characteristics and long-term outcomes of radiofrequency ablation. J Am Coll Cardiol. 2005;46:1921–30.
Kistler PM, Sanders P, Fynn SP, et al. Electrophysiological and electrocardiographic characteristics of focal atrial tachycardia originating from the pulmonary veins: acute and long-term outcomes of radiofrequency ablation. Circulation. 2003;108:1968–75.
Zhao Z, Li X, Guo J. Electrophysiologic characteristics of atrial tachycardia originating from the superior vena cava. J Interv Card Electrophysiol. 2009;24:89–94.
Iwai S, Badhwar N, Markowitz SM, et al. Electrophysiologic properties of para-Hisian atrial tachycardia. Heart Rhythm. 2011;8:1245–53.
Beukema RJ, Smit JJJ, Adiyaman A, et al. Ablation of focal atrial tachycardia from the non-coronary aortic cusp: case series and review of the literature. Europace. 2015;17:953–61.
Chen C, Tai C, Chiang C, et al. Atrial tachycardias originating from the atrial septum: electrophysiologic characteristics and radiofrequency ablation. J Cardiovasc Electrophysiol. 2000;II:744–9.
Roberts-Thomson KC, Kistler PM, Haqqani HM, et al. Focal atrial tachycardias arising from the right atrial appendage: electrocardiographic and electrophysiologic characteristics and radiofrequency ablation. J Cardiovasc Electrophysiol. 2007;18:367–72.
Yun-Long W, Xue-Bin L, Xin Q, et al. Focal atrial tachycardia originating from the left atrial appendage: electrocardiographic and electrophysiologic characterization and long-term outcomes of radiofrequency ablation. J Cardiovasc Electrophysiol. 2007;18:459–64.
Kistler PM, Roberts-Thomson KC, Haqqani HM, et al. P-wave morphology in focal atrial tachycardia. Development of an algorithm to predict the anatomic site of origin. J Am Coll Cardiol. 2006;48:1010–7.
Kistler PM, Chieng D, Tonchev IR, et al. P-wave morphology in focal atrial tachycardia. JACC Clin Electrophysiol. 2021;7:1547–56.
Türkmen Y, Insulander P, Bastani H, et al. Focal atrial tachycardia-the localization differences between men and women: a study of 487 consecutive patients. Anatol J Cardiol. 2020;24:405–9.
Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. Eur Heart J. 2020;41:655–720.
Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2016;133:e506–74.
Bohnen M, Stevenson WG, Tedrow UB, et al. Incidence and predictors of major complications from contemporary catheter ablation to treat cardiac arrhythmias. Heart Rhythm. 2011;8:1661–6.
Frey B, Kreiner G, Gwechenberger M, Gössinger HD. Ablation of atrial tachycardia originating from the vicinity of the atrioventricular node: significance of mapping both sides of the interatrial septum. 2001.
Quesada A, Cózar R, Anguera I. Spanish Catheter Ablation Registry. 19th Official Report of the Heart Rhythm Association of the Spanish Society of Cardiology (2019). Revista Española de Cardiología (English Edition). 2020;73:1049–60.
Cózar León R, AngueraCamós I, Cano Pérez Ó. Spanish Catheter Ablation Registry. 20th Official Report of the Heart Rhythm Association of the Spanish Society of Cardiology (2020). Revista Española de Cardiología (English Edition). 2021;74:1072–83.
Chrispin J, Misra S, Marine JE, et al. Current management and clinical outcomes for catheter ablation of atrioventricular nodal re-entrant tachycardia. Europace. 2018;20:e51–9.
Tan ESJ, Chan SP, Seow S, et al. Outcomes of supraventricular tachycardia ablation: results from the Singapore ablation and cardiac devices registry. Pacing Clin Electrophysiol. 2022;45:50–8. https://doi.org/10.1111/pace.14410.
Medi C, Kalman JM, Haqqani H, et al. Tachycardia-mediated cardiomyopathy secondary to focal atrial tachycardia. Long-term outcome after catheter ablation. J Am Coll Cardiol. 2009;53:1791–7.
Ban JE, Park TY, Park SW. Percutaneous epicardial ablation of incessant atrial tachycardia originating from the left atrial appendage. J Thorac Dis. 2016;8:E1551–4.
Phillips KP, Natale A, Sterba R, et al. Percutaneous pericardial instrumentation for catheter ablation of focal atrial tachycardias arising from the left atrial appendage. J Cardiovasc Electrophysiol. 2008;19:430–3.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140:e125–51.
Acknowledgements
We are grateful to Leila Koplan for producing the image used for Fig. 2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Whitaker, J., Steiger, N., Romero, J. et al. 10-year single center experience of catheter ablation of focal atrial tachycardia. J Interv Card Electrophysiol 66, 1135–1144 (2023). https://doi.org/10.1007/s10840-022-01416-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01416-5