Abstract
Background
Although the ectopic foci responsible for initiating atrial fibrillation (AF) are usually located in the pulmonary veins (PVs), non-PV sources may initiate AF in approximately 11% of unselected patients with paroxysmal or persistent AF. The superior vena cava (SVC) is one of the most frequent non-PV origins for initiating AF. This study aims to investigate the effect of empirical SVC isolation in redo AF ablation procedures.
Methods
Consecutive patients undergoing redo AF ablation procedures using a high-power short-duration protocol (HPSD) (50 W; ablation index guided; target AI 350 for posterior wall ablation, AI 450 for anterior wall ablation; CARTO 3 mapping system) were included. Patients with SVC isolation were compared to patients without SVC isolation. Periprocedural parameters and complications were recorded and analyzed. Short-term endpoints included intrahospital AF recurrence, midterm endpoint AF freedom after 3 months, and long-term endpoint AF freedom after 12 months.
Results
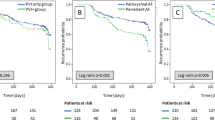
A total of 276 patients underwent repeat ablation for recurrent AF (67 ± 10 years; 57% male; 31.5% paroxysmal AF). The patients were divided into two groups: redo procedures with SVC isolation vs redo procedure without SVC isolation. Additional LA substrate modification was done based on intraprocedural voltage maps. Baseline characteristics did not differ significantly between the two groups. Median procedure time was 85.4 ± 27.1 min with ablation times of 14.0 ± 8.5 min. Intrahospital AF recurrence occurred in 32 patients (12%) with no difference among both groups: 17 patients (13%) SVC vs 15 patients (10%) No-SVC; p = 0.416. At 3-month follow-up, 47 (17%) presented an AF recurrence during the blanking period: 25 patients (19%) SVC vs 22 patients (15%) No-SVC; p = 0.304). After 12 months, 202 (73%) of all patients were in stable sinus rhythm with no significant difference between the two groups: 93 patients (73%) SVC vs 109 patients (74%) No-SVC; p = 0.853). No significant differences were noted when dividing the patients in paroxysmal or persistent AF with and without SVC isolation.
Conclusions
In our series of repeat AF ablation procedures, the addition of empirical SVC isolation to Re-PVI and LA substrate modification did not influence AF recurrence rates. This strategy can however be safe and useful in patients in whom SVC is identified as a trigger of AF.


Similar content being viewed by others
References
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al.; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics – 2019 Update: a report from the American Heart Association. Circulation 2019; 139(10): e56–e528.
Stroke risk in atrial fibrillation working group. Independent predic tors of stroke in patients with atrial fibrillation: a systematic review. Neurology. 2007;69(6):546–54.
Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Int Med. 2007;146(12):857–67.
Haïssaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339(10):659–66.
Santangeli P, Zado ES, Hutchinson MD, Riley MP, Lin D, Frankel DS, Supple GE, Garcia FC, Dixit S, Callans DJ, Marchlinski FE. Prevalence and distribution of focal triggers in persistent and long-standing persistent atrial fibrillation. Heart Rhythm. 2016;13(2):374–82.
Takigawa M, Takahashi A, Kuwahara T, Okubo K, Takahashi Y, Nakashima E, et al. Impact of non-pulmonary vein foci on the outcome of the second session of catheter ablation for paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2015;26:739–46.
Miyazaki S, Takigawa M, Kusa S, Kuwahara T, Taniguchi H, Okubo K, Nakamura H, Hachiya H, Hirao K, Takahashi A, Iesaka Y. Role of arrhythmogenic superior vena cava on atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25(4):380–6.
Ejima K, Kato K, Iwanami Y, et al. Impact of an empiric isolation of the superior vena cava in addition to circumferential pulmonary vein isolation on the outcome of paroxysmal atrial fibrillation ablation. Am J Cardiol. 2015;116(11):1711–6.
Wang XH, Liu X, Sun YM, Shi HF, Zhou L, Gu JN. Pulmonary vein isolation combined with superior vena cava isolation for atrial fibrillation ablation: a prospective randomized study. Europace. 2008;10(5):600–5.
Da Costa A, Levallois M, Romeyer-Bouchard C, Bisch L, Gate-Martinet A, Isaaz K. Remote controlled magnetic pulmonary vein isolation combined with superior vena cava isolation for paroxysmal atrial fibrillation: a prospective randomized study. Arch Cardiovasc Dis. 2015;108(3):163–71.
SP Sharma, RS Sangha, K Dahal, et al The role of empiric superior vena cava isolation in atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. J Interv Card Electrophysiol.2016; 48:61–67
Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20(1):e1–160.
Xu K, Wang Y, Wu S, et al. The role of superior vena cava in catheter ablation of long-standing persistent atrial fibrillation. Europace. 2017;19(10):1670–5.
Tao Z, Yunlong W, Zhuo L, Hua Z, Zhihong H, Ye W, Yongquan W, Xuejun R. Effect of combined pulmonary vein and superior vena cava isolation on the outcome of second catheter ablation for paroxysmal atrial fibrillation. Am J Cardiol; 2020; 125(12): 1845–1850.
F Spies, A Madaffari, G Voellmin, P Krisai, N Schaerli, T Reichlin, S Osswald, C Sticherling, M Kuhne, S Knecht, Empirical superior vena cava isolation in patients undergoing redo- catheter ablation procedure after recurrence of atrial fibrillation. Eur Heart J; 2020; 41:ehaa946.0597
Corrado Andrea, Bonso Aldo, Madalosso Michela, Rossillo Antonio, Themistoclakis Sakis, Di Biase Luigi, Natale Andrea, Raviele Antonio. Impact of systematic isolation of superior vena cava in addition to pulmonary vein antrum isolation on the outcome of paroxysmal, persistent, and permanent atrial fibrillation ablation: results from a randomized study. J Cardiovasc Electrophysiol. 2010;21 (1):1–5.
Bai R, Patel D, Di Biase L, et al. Phrenic nerve injury after catheter ablation: should we worry about this complication? J Cardiovasc Electrophysiol. 2006;17(9):944–8.
Chen G, Dong JZ, Liu XP, et al. Sinus node injury as a result of superior vena cava isolation during catheter ablation for atrial fibrillation and atrial flutter. Pacing Clin Electrophysiol. 2011;34(2):163–70.
Kim YG, Choi JI, Boo KY, Kim DY, Oh SK, Park HS, et al. Clinical and echocardiographic risk factors predict late recurrence after radiofrequency catheter ablation of atrial fibrillation. Sci Rep. 2019;9(1):6890.
Funding/Acknowledgements
The author Gelu Simu acknowledges funding received from the European Society of Cardiology in form of an ESC Training Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simu, G., Deneke, T., Ene, E. et al. Empirical superior vena cava isolation in patients undergoing repeat catheter ablation procedure after recurrence of atrial fibrillation. J Interv Card Electrophysiol 65, 551–558 (2022). https://doi.org/10.1007/s10840-022-01301-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01301-1