Abstract
Purpose
To assess the role of intense physical activity (PA) on recurrence after ventricular tachycardia (VT) ablation in arrhythmogenic cardiomyopathy (ACM).
Methods
We retrospectively analyzed 63 patients with definite diagnosis of ACM who underwent to catheter ablation (CA) of VT. PA was quantified in METs per week by IPAQ questionnaire in 51 patients. VT-free survival time after ablation was analyzed by Kaplan–Meier’s curves.
Results
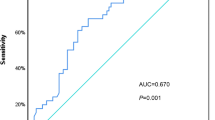
The weekly amount of PA was higher in patients with VT recurrence (2303.1 METs vs 1043.5 METs, p = 0.042). The best cutoff to predict VT recurrence after CA was 584 METs/week (AUC = 0.66, sensibility = 85.0%, specificity = 45.2%). Based on this cutoff, 34 patients were defined as high level athletes (Hi-PA) and 17 patients as low-level athletes (Lo-PA). During a median follow-up of 32.0 months (11.5–65.5), 22 patients (34.9%) experienced VT recurrence. Lo-PA patients had a longer VT-free survival, compared with Hi-PA patients (82.4% vs 50.0%, log-rank p = 0.025). At Cox multivariate analysis, independent predictors of the VT recurrence were PA ≥ 584 METs/week (Hi-PA) (HR = 2.61, CI 95% 1.03–6.58, p = 0.04) and late potential (LP) abolition (HR = 0.38, CI 95% 0.16–0.89, p = 0.03).
Conclusions
PA ≥ 584 METs/week and LP abolition were independent predictors of VT recurrence after ablation.



Similar content being viewed by others
Availability of data and material (data transparency)
The study data will be made available to other researchers from the corresponding author upon reasonable request for purposes of reproducing the results.
Abbreviations
- AMC:
-
Arrhythmogenic cardiomyopathy
- CA:
-
Catheter ablation
- LV:
-
Left ventricle (LV)
- PA:
-
Physical activity
- RV:
-
Right ventricle
- SCD:
-
Sudden cardiac death
- TWI:
-
T-wave inversion
- VTT:
-
Ventricular tachycardia
References
Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med. 1988;318(3):129–33.
Saberniak J, Hasselberg NE, Borgquist R, Platonov PG, Sarvari SI, Smith HJ, Ribe M, Holst AG, Edvardsen T, Haugaa KH. Vigorous physical activity impairs myocardial function in patients with arrhythmogenic right ventricular cardiomyopathy and in mutation positive family members. Eur J Heart Fail. 2014;16(12):1337–44.
Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G. Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation. 2004;110(14):1879–84.
Wichter T, Paul M, Wollmann C, Acil T, Gerdes P, Ashraf O, Tjan TD, Soeparwata R, Block M, Borggrefe M, Scheld HH, Breithardt G, Bocker D. Implantable cardioverter/defibrillator therapy in arrhythmogenic right ventricular cardiomyopathy: single-center experience of long-term follow-up and complications in 60 patients. Circulation. 2004;109(12):1503–8.
James CA, Bhonsale A, Tichnell C, Murray B, Russell SD, Tandri H, Tedford RJ, Judge DP, Calkins H. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol. 2013;62(14):1290–7.
Fontaine G, Frank R, Rougier I, Tonet JL, Gallais Y, Farenq G, Lascault G, Lilamand M, Fontaliran F, Chomette G, et al. Electrode catheter ablation of resistant ventricular tachycardia in arrhythmogenic right ventricular dysplasia: experience of 13 patients with a mean follow-up of 45 months. Eur Heart J. 1989;10(Suppl D):74–81.
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DM, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, Zareba W. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Eur Heart J. 2010;31(7):806–14.
Strath SJ, Kaminsky LA, Ainsworth BE, Ekelund U, Freedson PS, Gary RA, Richardson CR, Smith DT, Swartz AM, Lifestyle American Heart Association Physical Activity Committee of the Council on, Health Cardiometabolic, Exercise Cardiac Rehabilitation Cardiovascular, Cardiology Prevention Committee of the Council on Clinical, and Council. Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American Heart Association. Circulation. 2013;128(20):2259–79.
Mannocci A, Di Thiene D, Del Cimmuto A, Masala D, Boccia A, De Vito E, La Torre G. International physical activity questionnaire: validation and assessment in an Italian sample. Italian J Public Health. 2021;7:369–76.
Levine BD, Baggish AL, Kovacs RJ, Link MS, Maron MS, Mitchell JH. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 1: classification of sports: dynamic, static, and impact: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2350–5.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14.
Sosa E, Scanavacca M, d’Avila A, Pilleggi F. A new technique to perform epicardial mapping in the electrophysiology laboratory. J Cardiovasc Electrophysiol. 1996;7(6):531–6.
Marchlinski FE, Callans DJ, Gottlieb CD, Zado E. Linear ablation lesions for control of unmappable ventricular tachycardia in patients with ischemic and nonischemic cardiomyopathy. Circulation. 2000;101(11):1288–96.
Venlet J, Piers SRD, Kapel GFL, de Riva M, Pauli PFG, van der Geest RJ, Zeppenfeld K. Unipolar endocardial voltage mapping in the right ventricle: optimal cutoff values correcting for computed tomography-derived epicardial fat thickness and their clinical value for substrate delineation. Circ Arrhythm Electrophysiol. 2017;10(8):e005175.
Hutchinson MD, Gerstenfeld EP, Desjardins B, Bala R, Riley MP, Garcia FC, Dixit S, Lin D, Tzou WS, Cooper JM, Verdino RJ, Callans DJ, Marchlinski FE. Endocardial unipolar voltage mapping to detect epicardial ventricular tachycardia substrate in patients with nonischemic left ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2011;4(1):49–55.
Cano O, Hutchinson M, Lin D, Garcia F, Zado E, Bala R, Riley M, Cooper J, Dixit S, Gerstenfeld E, Callans D, Marchlinski FE. Electroanatomic substrate and ablation outcome for suspected epicardial ventricular tachycardia in left ventricular nonischemic cardiomyopathy. J Am Coll Cardiol. 2009;54(9):799–808.
Vergara P, Trevisi N, Ricco A, Petracca F, Baratto F, Cireddu M, Bisceglia C, Maccabelli G, Della Bella P. Late potentials abolition as an additional technique for reduction of arrhythmia recurrence in scar related ventricular tachycardia ablation. J Cardiovasc Electrophysiol. 2012;23(6):621–7.
Whyte GP. Clinical significance of cardiac damage and changes in function after exercise. Med Sci Sports Exerc. 2008;40(8):1416–23.
Wilson M, O’Hanlon R, Prasad S, Deighan A, Macmillan P, Oxborough D, Godfrey R, Smith G, Maceira A, Sharma S, George K, Whyte G. Diverse patterns of myocardial fibrosis in lifelong, veteran endurance athletes. J Appl Physiol (1985). 2011;110(6):1622–6.
Trivax JE, Franklin BA, Goldstein JA, Chinnaiyan KM, Gallagher MJ, deJong AT, Colar JM, Haines DE, McCullough PA. Acute cardiac effects of marathon running. J Appl Physiol (1985). 2010;108(5):1148–53.
Pelliccia A, Maron BJ, De Luca R, Di Paolo FM, Spataro A, Culasso F. Remodeling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002;105(8):944–9.
Luthi P, Zuber M, Ritter M, Oechslin EN, Jenni R, Seifert B, Baldesberger S, AttenhoferJost CH. Echocardiographic findings in former professional cyclists after long-term deconditioning of more than 30 years. Eur J Echocardiogr. 2008;9(2):261–7.
Heidbuchel H, Hoogsteen J, Fagard R, Vanhees L, Ector H, Willems R, Van Lierde J. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias: role of an electrophysiologic study in risk stratification. Eur Heart J. 2003;24(16):1473–80.
La Gerche A, Robberecht C, Kuiperi C, Nuyens D, Willems R, de Ravel T, Matthijs G, Heidbuchel H. Lower than expected desmosomal gene mutation prevalence in endurance athletes with complex ventricular arrhythmias of right ventricular origin. Heart. 2010;96(16):1268–74.
Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, Grosgogeat Y. Right ventricular dysplasia: a report of 24 adult cases. Circulation. 1982;65(2):384–98.
Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42(11):1959–63.
Kirchhof P, Fabritz L, Zwiener M, Witt H, Schafers M, Zellerhoff S, Paul M, Athai T, Hiller KH, Baba HA, Breithardt G, Ruiz P, Wichter T, Levkau B. Age- and training-dependent development of arrhythmogenic right ventricular cardiomyopathy in heterozygous plakoglobin-deficient mice. Circulation. 2006;114(17):1799–806.
Sen-Chowdhry S, Syrris P, Ward D, Asimaki A, Sevdalis E, McKenna WJ. Clinical and genetic characterization of families with arrhythmogenic right ventricular dysplasia/cardiomyopathy provides novel insights into patterns of disease expression. Circulation. 2007;115(13):1710–20.
Lie OH, Rootwelt-Norberg C, Dejgaard LA, Leren IS, Stokke MK, Edvardsen T, Haugaa KH. Prediction of life-threatening ventricular arrhythmia in patients with arrhythmogenic cardiomyopathy: a primary prevention cohort study. JACC Cardiovasc Imaging. 2018;11(10):1377–86.
Vergara P, Tzou WS, Tung R, Brombin C, Nonis A, Vaseghi M, Frankel DS, Di Biase L, Tedrow U, Mathuria N, Nakahara S, Tholakanahalli V, Bunch TJ, Weiss JP, Dickfeld T, Lakireddy D, Burkhardt JD, Santangeli P, Callans D, Natale A, Marchlinski F, Stevenson WG, Shivkumar K, Sauer WH, Della Bella P. Predictive score for identifying survival and recurrence risk profiles in patients undergoing ventricular tachycardia ablation: the I-Vt score. Circ Arrhythm Electrophysiol. 2018;11(12):e006730.
Vaseghi M, Hu TY, Tung R, Vergara P, Frankel DS, Di Biase L, Tedrow UB, Gornbein JA, Yu R, Mathuria N, Nakahara S, Tzou WS, Sauer WH, Burkhardt JD, Tholakanahalli VN, Dickfeld TM, Weiss JP, Bunch TJ, Reddy M, Callans DJ, Lakkireddy DR, Natale A, Marchlinski FE, Stevenson WG, Della Bella P, Shivkumar K. Outcomes of catheter ablation of ventricular tachycardia based on etiology in nonischemic heart disease: an international ventricular tachycardia ablation center collaborative study. JACC Clin Electrophysiol. 2018;4(9):1141–50.
Kirubakaran S, Bisceglia C, Silberbauer J, Oloriz T, Santagostino G, Yamase M, Maccabelli G, Trevisi N, Della Bella P. Characterization of the arrhythmogenic substrate in patients with arrhythmogenic right ventricular cardiomyopathy undergoing ventricular tachycardia ablation. Europace. 2017;19(6):1049–62.
Bai R, Di Biase L, Shivkumar K, Mohanty P, Tung R, Santangeli P, Saenz LC, Vacca M, Verma A, Khaykin Y, Mohanty S, Burkhardt JD, Hongo R, Beheiry S, Dello Russo A, Casella M, Pelargonio G, Santarelli P, Sanchez J, Tondo C, Natale A. Ablation of ventricular arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy: arrhythmia-free survival after endo-epicardial substrate based mapping and ablation. Circ Arrhythm Electrophysiol. 2011;4(4):478–85.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Paolo Della Bella is consultant for St. Jude Medical and has received honoraria for lectures from Biosense Webster, St. Jude Medical, and Biotronik. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Pasquale Vergara and Luigi Pannone are shared first authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vergara, P., Pannone, L., Calvo, F. et al. Physical activity volume in patients with arrhythmogenic cardiomyopathy is associated with recurrence after ventricular tachycardia ablation. J Interv Card Electrophysiol 65, 15–24 (2022). https://doi.org/10.1007/s10840-021-01019-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-01019-6