Abstract
Purpose
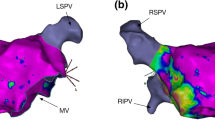
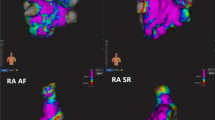
Left atrial (LA) fibrosis plays an important role in the pathogenesis and perpetuation of atrial fibrillation (AF). It may be identified by bipolar voltage (BiV) mapping, but quantification of fibrosis which previously relied on visual estimation of scar has been shown to be inaccurate. Our aim was to use a novel automated voltage histogram analysis (VHA) tool to quantify LA scar burden accurately in patients with AF.
Methods
LA voltage was assessed in 100 consecutive patients undergoing first pulmonary vein isolation (PVI) for paroxysmal or persistent AF using a circular multielectrode catheter to create high-density LA BiV maps which were analysed using the VHA tool after the procedure.
Results
High-density electro-anatomic maps took 10 min to create and contained a median of 1049 points. The VHA algorithm accurately quantified the burden of Diseased LA Tissue (≤ 0.5 mV) and Dense LA Scar (≤ 0.2 mV) with a median of 17.8% and 3.5% respectively. A quartile classification was applied based on diseased LA tissue burden. Patients in class IV with the highest diseased LA burden were older (p < 0.0001), more likely female (p = 0.0095), had higher CHA2DS2-VASc scores (p = 0.0024) and were more likely to have persistent rather than paroxysmal AF (p = 0.0179) than those in classes I–III.
Conclusions
The VHA algorithm is able to quantify percentage surface area voltage rapidly and according to preset ranges for the first time. The algorithm offers the potential for classification of patients undergoing AF ablation into different classes of diseased LA burden, which may have diagnostic, therapeutic and prognostic implications.


Similar content being viewed by others
References
Velagapudi P, Turagam MK, Leal MA, Kocheril AG. Atrial fibrosis: a risk stratifier for atrial fibrillation. Expert Rev Cardiovasc Ther. 2013;11(2):155–60. https://doi.org/10.1586/erc.12.174.
Schreiber D, Rieger A, Moser F, Kottkamp H. Catheter ablation of atrial fibrillation with box isolation of fibrotic areas: lessons on fibrosis distribution and extent, clinical characteristics, and their impact on long-term outcome. J Cardiovasc Electrophysiol. 2017;28(9):971–83. https://doi.org/10.1111/jce.13278.
Yang G, Yang B, Wei Y, Zhang F, Ju W, Chen H, et al. Catheter ablation of nonparoxysmal atrial fibrillation using electrophysiologically guided substrate modification during sinus rhythm after pulmonary vein isolation. Circ Arrhythm Electrophysiol. 2016;9(2):e003382. https://doi.org/10.1161/CIRCEP.115.003382.
Mahnkopf C, Badger TJ, Burgon NS, Daccarett M, Haslam TS, Badger CT, et al. Evaluation of the left atrial substrate in patients with lone atrial fibrillation using delayed-enhanced MRI: implications for disease progression and response to catheter ablation. Heart Rhythm. 2010;7(10):1475–81. https://doi.org/10.1016/j.hrthm.2010.06.030.
Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F, et al. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014;311(5):498–506. https://doi.org/10.1001/jama.2014.3.
Travers J, Keelan E, Keaney J, Szeplaki G, Valentine J, Hayam G, et al. Comparison of a novel tool for automatic measurement of left atrial scar burden with visual estimation in patients undergoing ablation of atrial fibrillation. Cardiostim World Congress; June 2016. Nice: EP Europace; 2016.
Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124(20):2264–74. https://doi.org/10.1161/CIRCULATIONAHA.111.019893.
Nattel S, Burstein B, Dobrev D. Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol. 2008;1(1):62–73. https://doi.org/10.1161/CIRCEP.107.754564.
Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995;92(7):1954–68.
de Groot NM, Houben RP, Smeets JL, Boersma E, Schotten U, Schalij MJ, et al. Electropathological substrate of longstanding persistent atrial fibrillation in patients with structural heart disease: epicardial breakthrough. Circulation. 2010;122(17):1674–82. https://doi.org/10.1161/CIRCULATIONAHA.109.910901.
Oakes RS, Badger TJ, Kholmovski EG, Akoum N, Burgon NS, Fish EN, et al. Detection and quantification of left atrial structural remodeling with delayed-enhancement magnetic resonance imaging in patients with atrial fibrillation. Circulation. 2009;119(13):1758–67. https://doi.org/10.1161/CIRCULATIONAHA.108.811877.
Peters DC, Wylie JV, Hauser TH, Nezafat R, Han Y, Woo JJ, et al. Recurrence of atrial fibrillation correlates with the extent of post-procedural late gadolinium enhancement: a pilot study. JACC Cardiovasc Imaging. 2009;2(3):308–16. https://doi.org/10.1016/j.jcmg.2008.10.016.
Hunter RJ, Jones DA, Boubertakh R, Malcolme-Lawes LC, Kanagaratnam P, Juli CF, et al. Diagnostic accuracy of cardiac magnetic resonance imaging in the detection and characterization of left atrial catheter ablation lesions: a multicenter experience. J Cardiovasc Electrophysiol. 2013;24(4):396–403. https://doi.org/10.1111/jce.12063.
Ammar-Busch S, Buiatti A, Tatzber A, Reents T, Bourier F, Semmler V, et al. Predictors of low voltage areas in persistent atrial fibrillation: is it really a matter of time? J Interv Card Electrophysiol. 2018. https://doi.org/10.1007/s10840-018-0471-7.
Masuda M, Fujita M, Iida O, Okamoto S, Ishihara T, Nanto K, et al. Comparison of left atrial voltage between sinus rhythm and atrial fibrillation in association with electrogram waveform. Pacing Clin Electrophysiol. 2017;40(5):559–67. https://doi.org/10.1111/pace.13051.
Yagishita A, S DEO, Cakulev I, Gimbel JR, Sparano D, Manyam H, et al. Correlation of left atrial voltage distribution between sinus rhythm and atrial fibrillation: identifying structural remodeling by 3-D electroanatomic mapping irrespective of the rhythm. J Cardiovasc Electrophysiol. 2016;27(8):905–12. https://doi.org/10.1111/jce.13002.
Vlachos K, Efremidis M, Letsas KP, Bazoukis G, Martin R, Kalafateli M, et al. Low-voltage areas detected by high-density electroanatomical mapping predict recurrence after ablation for paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2017;28:1393–402. https://doi.org/10.1111/jce.13321.
Ling Z, McManigle J, Zipunnikov V, Pashakhanloo F, Khurram IM, Zimmerman SL, et al. The association of left atrial low-voltage regions on electroanatomic mapping with low attenuation regions on cardiac computed tomography perfusion imaging in patients with atrial fibrillation. Heart Rhythm. 2015;12(5):857–64. https://doi.org/10.1016/j.hrthm.2015.01.015.
Squara F, Frankel DS, Schaller R, Kapa S, Chik WW, Callans DJ, et al. Voltage mapping for delineating inexcitable dense scar in patients undergoing atrial fibrillation ablation: a new end point for enhancing pulmonary vein isolation. Heart Rhythm. 2014;11(11):1904–11. https://doi.org/10.1016/j.hrthm.2014.07.027.
Kapa S, Desjardins B, Callans DJ, Marchlinski FE, Dixit S. Contact electroanatomic mapping derived voltage criteria for characterizing left atrial scar in patients undergoing ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25(10):1044–52. https://doi.org/10.1111/jce.12452.
Acknowledgements
The technical support and assistance of Laura Deery, Gal Hayam and Tal Baron of Biosense-Webster® in the development and use of the voltage histogram analysis tool and in the provision of a laptop computer for offline analysis using the VHA tool is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study. All procedures performed in our study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and approved by our institutional research ethics committee. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
GS reports personal fees from Johnson and Johnson Medical, Abbott and Biotronik; other authors have no conflicts of interests to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Herczeg, S., Walsh, K., Keaney, J.J. et al. Quantitative assessment of left atrial scar using high-density voltage mapping and a novel automated voltage analysis tool. J Interv Card Electrophysiol 59, 5–12 (2020). https://doi.org/10.1007/s10840-019-00570-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00570-7