Abstract
Purpose
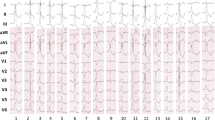
During cardiac mapping, it is critical to discriminate signals related to cardiac conduction versus those due to mechanical interaction with other cardiac structures such as valves. We sought to define characteristics that could facilitate discrimination of valve artifact from cardiac conduction signals.
Methods
Patients with structurally normal heart undergoing mapping for ventricular arrhythmias arising from the vicinity of the aortic valve between January 2013 and May 2015 were included. Potentials felt to reflect aortic valve opening (occurring at the end of the QRS after the local ventricular signal) were termed A1, and those felt to reflect valve closure were termed A2.
Results
A total of 24 patients had mapping in the sinuses of Valsalva, and 10 (average age 40 + 15, 60% male) were found to have additional signals (A1 and/or A2) notable during mapping. In all patients, intervals between A1 and A2 shortened after ectopic beats and lengthened after compensatory pauses. These variations in the interval matched the change in systolic duration on Doppler echocardiography. Overdrive atrial pacing was performed in four patients, which demonstrated progressive shortening of intervals between A1 and A2. Pacing always revealed local capture without affecting A1 or A2. In the one patient in whom ablation was performed in these areas, there was no effect on A1 or A2, suggesting these signals represented artifact.
Conclusions
Valve-related signals in the aortic sinuses are commonly seen and can be distinguished. The interval between A1 and A2 correlated with mechanical systole and varied in a physiologically predictable manner with heart rate changes.







Similar content being viewed by others
References
Del Carpio Munoz F, Buescher T, Asirvatham SJ. Teaching points with 3-dimensional mapping of cardiac arrhythmias: taking points: activation mapping. Circ Arrhythm Electrophysiol. 2011;4:e22–5.
Venkatachalam KL, Herbrandson JE, Asirvatham SJ. Signals and signal processing for the electrophysiologist: part I: electrogram acquisition. Circ Arrhythm Electrophysiol. 2011;4:965–73.
Srivathsan KS, Bunch TJ, Asirvatham SJ, Edwards WD, Friedman PA, Munger TM, et al. Mechanisms and utility of discrete great arterial potentials in the ablation outflow tract ventricular arrhythmias. Circ Arrhythm Electrophysiol. 2008;1:30–8.
Romero J, Ajijola O, Shivkumar K, Tung R. Characterization of aortic valve closure artifact during outflow tract mapping: correlation with hemodynamics and mechanical valves. Circ Arrhythm Electrophysiol. 2017;10
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The investigation was conducted according to an institutional review board (IRB)-approved protocol, approved by the Mayo Clinic.
Informed consent
As this was a retrospective review, only patients who had given consent to make their records available for research review were included according to the above IRB-approved protocol.
Electronic supplementary material
Supplementary Figure 1
Intervals with PVC. The sum of intervals between A1 after the QRS (preceding PVC) to the A2 after the PVC (systole and diastole due to the normal sinus beat + systole due to the PVC) and A2-A1 (diastole after the PVC) after the PVC was similar to the RR interval between the QRS preceding and following the PVC (equals two cardiac cycles). (GIF 372 kb)
Supplementary Figure 2
Pulse wave Doppler echo showing shortened systolic time after premature complex compared to systole after sinus beat (last beat) in the tracing. Also, note that post-PVC sinus beat has a longer systolic phase as shown by caliper measurement. (GIF 171 kb)
Supplementary Figure 3
Shown is the sum of intervals A1-A2 (systolic time) and A2-A1 (diastolic time), which is equal to the RR interval (one cardiac cycle) during pacing. (GIF 459 kb)
Supplementary Figure 4
Electromechanical delay. The timing of the aortic valve opening and closure relative to the QRS. (GIF 225 kb)
Supplementary Figure 5
Flow diagram depicting a practical approach to differentiate mechanical valve signals from true electrical and other non-physiological signals during mapping. LVOT = Left ventricular outflow tract. SOV = Sinuses of Valsalva. (GIF 335 kb)
Supplementary Figure 6
Complex diastolic signals noted when the catheter was in contact with mitral valve apparatus, likely due to the fluttering of mitral leaflets (diastasis) when in contact. (GIF 280 kb)
Rights and permissions
About this article
Cite this article
Kancharla, K., Munger, T.M., Nishimura, R.A. et al. Identification of valve-related artifact during cardiac mapping. J Interv Card Electrophysiol 50, 159–167 (2017). https://doi.org/10.1007/s10840-017-0293-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-017-0293-z