Abstract
Purpose
The aim of this study was to determine if transcutaneous CO2 monitoring (TCO2) is feasible to avoid hypercapnia during complex catheter ablation. Cumulative analgesic and anxiolytic effects during complex catheter ablation can rarely provoke hypoventilation and respiratory complications. End tidal CO2 monitors have limitations in non-ventilated patients, and frequent arterial blood gas sampling is impractical.
Methods
Consecutive patients undergoing catheter ablation for atrial fibrillation (AF) or ventricular tachycardia (VT) received continuous TCO2 monitoring. Procedural evaluation of TCO2 was performed concomitantly with point-of-care arterial blood gas testing. Endpoints included PCO2 protocol feasibility, TCO2/PCO2 agreement, and avoidance of hypercapnia-related procedural complications.
Results
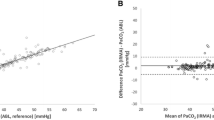
Fifty patients [AF n = 36 (72 %), VT n = 14 (28 %)] underwent catheter ablation (mean 221.7 ± 57.0 min duration, median 41.4 ± 21.1 min fluoroscopy) in which 6.0 ± 2.6 mg midazolam and 449 ± 225.5 mcg of fentanyl were administered. Monitoring protocol implementation was feasible in 50/50 (100 %) cases. Protocol-driven anesthesia consultation avoided an unplanned intubation in 1 case (2 %) and there was only 1 unplanned intubation (2 %) for oxygen desaturation due to heart failure without hypercapnia during a VT ablation (TCO2/PCO2 agreement <5 mmHg). There were no respiratory or pulseless electrical arrests (0 %) in the study. TCO2 and PCO2 correlated well (baseline: r = 0.75, p < 0.001; 1 h:r= 0.72, p < 0.001; 2 h: r = 0.55, p = 0.003; 3 h: r = 0.79, p = 0.02). However, desired agreement was lower than expected [baseline: 33/50 (66 %) < 5 mmHg, 48/50 (96 %) <10 mmHg; 1 h: 29/45 (64 %) < 5 mmHg, 39/45 (87 %) < 10 mmHg; 2 h: 14/26 (54 %) < 5 mmHg, 22/26 (85 %) < 10 mmHg; 3 h: 7/11 (64 %) < 5 mmHg, 10/11 (91 %) < 10 mmHg; >3 h: 1/3 (33 %) < 5 mmHg, 2/3 (66 %) < 10 mmHg].
Conclusion
Transcutaneous CO2 monitoring is feasible during complex catheter ablation and correlates with invasively obtained data. However, further development is needed to achieve the desired level of agreement.




Similar content being viewed by others
References
Rahimtoola, S. H., Zipes, D. P., Akhtar, M., et. al. (1987) Consensus statement of the conference on the state of the art of electrophysiology testing in the diagnosis and treatment of patients with cardiac arrhythmias. Circulation, 75(4).
Guidelines for clinical intracardiac electrophysiologic studies. (1989). A report of the American College of Cardiology/American Heart Association Task Force on assessment of diagnostic and therapeutic cardiovascular procedures. Circulation, 80(6)
Olkkola, K. T., & Ahonen, J. (2008). Midazolam and other benzodiazepines. Handbook of Experimenta Pharmcology, 182, 335–60.
Smydo, J. (1979). Delayed respiratory depression with fentanyl. Anesthesia Progress, 26(2), 47–78.
American Society of Anesthesiologists: Ad Hoc Committee on Credentialing Committee of Review: Ambulatory Surgical Care. Statement on granting privileges for administration of moderate sedation to practitioners who are not anesthesia professionals. Approved Oct 25, 2005 and last amended Oct 19,2011. https://www.asahq.org/. Accessed Oct 2014.
Cleveland Clinic EP complications database, queried May 2012. https://epcomplications.cvm.ccf.org/
De Oliveira, G. S., Ahmad, S., Fitzgerald, P. C., & McCarthy, R. J. (2010). Detection of hypoventilation during deep sedation in patients undergoing ambulatory gynaecological hysteroscopy: a comparison between transcutaneous and nasal end-tidal carbon dioxide measurements. British Journal of Anasthesia, 104(6), 774–78.
Cox, P., & Tobias, J. D. (2007). Noninvasive monitoring of PaCO2 during one-lung ventilation and minimal access surgery in adults: end-tidal versus transcutaensous techniques. Journal of Minimal Access Surgery, 3(1), 8–13.
Wilson, J., Russo, P., Russo, J., & Tobias, J. D. (2005). Noninvasive monitoring of carbon dioxide in infants and children with congenital heart disease: end-tidal versus transcutaneous techniques. Journal of Intensive Care Medicine, 20(5), 291–5.
Roediger, R., Beck-Schimmer, B., Theusinger, O. M., et al. (2011). The revised digital transcutaneous PCO2/SpO2 ear sensor is a reliable non-invasive monitoring tool in patients after cardiac surgery. Journal of Cardiovascular and Vascular Anesthesia, 25(2), 242–49.
Nosovitch, M. A., Johnson, J. O., & Tobias, J. D. (2002). Noninvasive intraoperative monitoring of carbon dioxide in children: end tidal versus transcutaneous techniques. Paediatric Anaesthesia, 12(1), 48–52.
Courtney, S. E., Kahn, D. J., Singh, R., et al. (2011). Bubble and ventilator-derived nasal continuous positive airway pressure in premature infants: work of breathing and gas exchange. Journal of Perinatology, 31(1), 44–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cantillon, D.J., Keene, L.M., Hakim, A. et al. Transcutaneous carbon dioxide monitoring to avoid hypercapnia during complex catheter ablations: a feasibility study. J Interv Card Electrophysiol 43, 307–311 (2015). https://doi.org/10.1007/s10840-015-0013-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0013-5