Abstract
This study investigates the long-term relationship between individuals’ health state changes over time and burdens due to out-of-pocket medical expenses (OOP) in later years. We kept track of 5540 individuals’ health trajectories and their accumulated OOP using the HRS data from 1992 to 2010. American adults between 50 and 70 years old spend on average $27,000 on OOP, and have five common health trajectory patterns (Multi-Morbidity, Co-Morbidity, Mild Disease, Late Event, and No Disease). However, their OOPs differed substantially depending on the pattern of health trajectory. The most costly pattern of Multi-Morbidity needed $18,823 more than the least costly No Disease pattern. Older adults with the most costly pattern spent most of OOP on either prescription drugs or doctor/dental visits. Additionally, we found that the OOP burden of prescription medications was substantially relieved by the Medicare Part D implementation. These findings have several important implications for individuals, financial educators, and policy makers.
Similar content being viewed by others
Notes
Sequence analysis has been developed and applied in many different social science fields such as psychology, economics, and political science to identify the typical patterns of life course trajectories (Aassve et al. 2007; Anyadike-Danes and McVicar 2010; Blair-Loy 1999; Halpin and Chan 1998; Martin et al. 2008; McVicar and Anyadike-Danes 2002; Pollock 2007; Pollock et al. 2002; Salmela-Aro et al. 2011).
Again, we note the accumulated OOP for the four categories is for the period from 1996 to 2010.
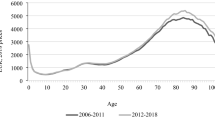
Medicare Part D, which began on January 1, 2006, gives the Medicare-eligible population of seniors’ access to a subsidized market for non-mandatory standardized prescription drug coverage through contracts sponsored by private insurance firms (Heiss et al. 2013).
References
Aassve, A., Billari, F. C., & Piccarreta, R. (2007). Strings of adulthood: A sequence analysis of young British women’s work-family trajectories. European Journal of Population, 23, 369–388. doi: 10.1007/s10680-007-9134-6.
Abbott, A. (1995). Sequence analysis: New methods for old ideas. Annual Review of Sociology, 21, 93–113. doi: 10.1146/annurev.so.21.080195.000521.
Abbott, A., & Hrycak, A. (1990). Measuring resemblance in sequence data: An optimal matching analysis of musicians’ careers. American Journal of Sociology, 96(1), 144–185. doi: 10.1086/229495.
Anyadike-Danes, M., & McVicar, D. (2010). My brilliant career: Characterizing the early labor market trajectories of British women from generation X. Sociological Methods and Research, 38(3), 482–512. doi: 10.1177/0049124110362968.
Barban, N. (2013). Family trajectories and health: A life course perspective. European Journal of Population, 29(4), 357–385. doi: 10.1007/s10680-013-9296-3.
Baulch, B., & Quisumbing, A. (2011). Testing and adjusting for attrition in household panel data. Chronic Poverty Research Centre (CPRC) Toolkit Note. Retrieved from http://www.chronicpoverty.org/uploads/assets/files/toolbox/CPRC_TOOLKIT_NOTE_ON_ATTRITION-revfinal.pdf.
Blair-Loy, M. (1999). Career patterns of executive women in finance: An optimal matching analysis. American Journal of Sociology, 104(5), 1346–1397. doi: 10.1086/210177.
Carpenter, J., & Kenward, M. (2012). Multiple imputation and its application. Hoboken, NJ: Wiley.
Christiansen, C. B., Olesen, J. B., Gislason, G., Lock-Hansen, M., & Torp-Pedersen, C. (2013). Cardiovascular and non-cardiovascular hospital admissions associated with atrial fibrillation: A Danish nationwide, retrospective cohort study. BMJ Open, 3(1), e001800. doi: 10.1136/bmjopen-2012-001800.
Crystal, S., Johnson, R. W., Harman, J., Sambamoorthi, U., & Kumar, R. (2000). Out-of-pocket health care costs among older Americans. Journals of Gerontology: Social Sciences, 55B(1), S51-S62. doi: 10.1093/geronb/55.1.S51.
Cunningham, P. J. (2009). Chronic burdens: The persistently high out-of-pocket health care expenses faced by many Americans with chronic conditions. Issue Brief, 63, 1–14. Retrieved from http://www.amcp.org/workarea/downloadasset.aspx?id=12137.
de Jager, D. J., Grootendorst, D. C., Jager, K. J., van Dijk, P. C., Tomas, L. M., Ansell, D., … & Wetzels, J. F. (2009). Cardiovascular and noncardiovascular mortality among patients starting dialysis. Journal of the American Medical Association, 302(16), 1782–1789. doi: 10.1001/jama.2009.1488.
Dijkstra, W., & Taris, T. (1995). Measuring the agreement between sequences. Sociological Methods and Research, 24(2), 214–231. doi: 10.1177/0049124195024002004.
Durbin, R., Eddy, S., Krogh, A., & Mitchison, G. (1998). Biological sequence analysis. Cambridge: Cambridge University Press.
Fahlman, C., Lynn, J., Doberman, D., Gabel, J., & Finch, M. (2006). Prescription drug spending for Medicare+ Choice beneficiaries in the last year of life. Journal of Palliative Medicine, 9(4), 884–893. doi: 10.1089/jpm.2006.9.884.
Gerber, Y., Melton, L. J., McNallan, S. M., Jiang, R., Weston, S. A., & Roger, V. L. (2013). Cardiovascular and noncardiovascular disease associations with hip fractures. The American Journal of Medicine, 126(2), 169.e19–169.e26. doi: 10.1016/j.amjmed.2012.06.032.
Guralnik, J. M., LaCroix, A. Z., Everett, D. F., & Kovar, M. G. (1989). Aging in the eighties: The prevalence of comorbidity and its association with disability. Retrieved from https://permanent.access.gpo.gov/gpo33200/ad170.pdf.
Hair, J. F. Jr., Black, W. C., Babin, B. J., & Anderson, R. E. (2006). Multivariate data analysis. Upper Saddle River, NJ: Pearson Prentice Hall.
Halpin, B., & Chan, T. W. (1998). Class careers as sequences: An optimal matching analysis of work-life histories. European Sociological Review, 14(2), 111–130. doi: 10.1093/oxfordjournals.esr.a018230.
Heiss, F., Leive, A., McFadden, D., & Winter, J. (2013). Plan selection in Medicare Part D: Evidence from administrative data. Journal of Health Economics, 32, 1325–1344. doi: 10.1016/j.jhealeco.2013.06.006.
Heron, M. (2015). Deaths: Leading causes for 2012. National Vital Statistics Reports, 64(10). Retrieved from https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_10.pdf.
HRS. (2011). Sample Sizes and Response Rates. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/sample response.pdf.
Hwang, W., Weller, W., Ireys, H., & Anderson, G. (2001). Out-of-pocket medical spending for care of chronic conditions. Health Affairs, 20(6), 267–278. doi: 10.1377/hlthaff.20.6.267.
Kim, H., Shin, S., & Zurlo, K. A. (2015). Sequential patterns of health conditions and financial outcomes in late life: Evidence from the Health and Retirement Study. The International Journal of Aging and Human Development, 81(1–2), 54–82. doi: 10.1177/0091415015614948.
Kim, H., Yoon, W., & Zurlo, K. A. (2012). Health shocks, out-of-pocket medical expenses and consumer debt among middle-aged and older Americans. Journal of Consumer Affairs, 46(3), 357–380. doi: 10.1111/j.1745-6606.2012.01236.x.
Kim, M. H., Johnston, S. S., Chu, B. C., Dalal, M. R., & Schulman, K. L. (2011). Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circulation: Cardiovascular Quality and Outcomes, 4(3), 313–320. doi: 10.1161/CIRCOUTCOMES.110.958165.
Lloyd-Jones, D. M., Dyer, A. R., Wang, R., Daviglus, M. L., & Greenland, P. (2007). Risk factor burden in middle age and lifetime risks for cardiovascular and non-cardiovascular death (Chicago Heart Association Detection Project in Industry). The American Journal of Cardiology, 99(4), 535–540. doi: 10.1016/j.amjcard.2006.09.099.
Marshall, S., McGarry, K., & Skinner, J. S. (2011). The risk of out-of-pocket health care expenditure at the end of life. In Explorations in the economics of aging (pp. 101–128). Retrieved from http://www.nber.org/chapters/c11935.pdf.
Martin, P., Schoon, I., & Ross, A. (2008). Beyond transitions: Applying optimal matching analysis to life course research. International Journal of Social Research Methodology, 11(3), 179–199. doi: 10.1080/13645570701622025.
McVicar, D., & Anyadike-Danes, M. (2002). Predicting successful and unsuccessful transitions from school to work by using sequence methods. Journal of the Royal Statistical Society: Series A (Statistics in Society), 165(2), 317–334. doi: 10.1111/1467-985X.00641.
Mills, D. (2016, April 28). Price of cancer drugs has skyrocketed since 2000. Healthline. Retrieved from http://www.healthline.com/health-news/price-of-cancer-drugs-hasskyrocketed#1.
Muscari, A., Bianchi, G., Forti, P., Giansante, C., Giovagnoli, M., Magalotti, D., … & Zoli, M. (2013). A comparison of risk factors as predictors of cardiovascular and non-cardiovascular mortality in the elderly people–relevance of N-terminal pro-B-type natriuretic peptide and low systolic blood pressure. International Journal of Clinical Practice, 67(11), 1182–1191. doi: 10.1111/ijcp.12195.
National Health Council. (2014). About Chronic Diseases. Retrieved from http://www.nationalhealthcouncil.org/sites/default/files/NHC_Files/Pdf_Files/AboutChronicDisease.pdf.
Paez, K. A., Zhao, L., & Hwang, W. (2009). Rising out-of-pocket spending for chronic conditions: A ten-year trend. Health Affairs, 28(1), 15–25. doi: 10.1377/hlthaff.28.1.15.
Piccarreta, R., & Billari, F. C. (2007). Clustering work and family trajectories by using a divisive algorithm. Journal of the Royal Statistical Society: Series A (Statistics in Society), 170(4), 1061–1078. doi: 10.1111/j.1467-985X.2007.00495.x.
Pollock, G. (2007). Holistic trajectories: A study of combined employment, housing and family careers by using multiple sequence analysis. Journal of the Royal Statistical Society: Series A (Statistics in Society), 170(1), 167–183. doi: 10.1111/j.1467-985X.2006.00450.x.
Pollock, G., Antcliff, V., & Ralphs, R. (2002). Work orders: Analyzing employment histories using sequence data. International Journal of Social Research Methodology, 5(2), 91–105. doi: 10.1080/13645570110062432.
Rogowski, J., Lillard, L. A., & Kington, R. (1997). The financial burden of prescription drug use among elderly persons. The Gerontologist, 37(4), 475–482. doi: 10.1093/geront/37.4.475.
Salmela-Aro, K., Kiuru, N., Nurmi, J., & Eerola, M. (2011). Mapping pathways to adulthood among Finnish university students: Sequences, patterns, variations in family and work related roles. Advances in Life Course Research, 16(1), 25–41. doi: 10.1016/j.alcr.2011.01.003.
Sambamoorthi, U., Shea, D., & Crystal, S. (2003). Total and out-of-pocket expenditures for prescription drugs among older persons. The Gerontologist, 43(3), 345–359. doi: 10.1093/geront/43.3.345.
Schoenberg, N. E., Kim, H., Edwards, W., & Fleming, S. T. (2007). Burden of common multiple morbidity constellations on out-of-pocket medical expenditures among older adults. The Gerontologist, 47(4), 423–437. doi: 10.1093/geront/47.4.423.
Smith, J. P. (1999). Healthy bodies and thick wallets: The dual relation between health and economic status. The Journal of Economic Perspectives, 13(2), 144–166. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3697076/pdf/nihms461647.pdf.
Smith, J. P. (2003). Consequences and predictors of new health events. In Analyses in the economics of aging (pp. 213–237). Retrieved from http://www.nber.org/chapters/c10362.pdf.
Stamler, J., Stamler, R., Neaton, J. D., Wentworth, D., Daviglus, M. L., Garside, D., … & Greenland, P. (1999). Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: Findings for 5 large cohorts of young adult and middle-aged men and women. Journal of the American Medical Association, 282(21), 2012–2018. doi: 10.1001/jama.282.21.2012.
Stewart, S. T. (2004). Do out of pocket health expenditures rise with age among older Americans? The Gerontologist, 44(1), 48–57. doi: 10.1093/geront/44.1.48.
Stovel, K., Savage, M., & Bearman, P. (1996). Ascription into achievement: Models of career systems at Lloyds Bank, 1890–1970. American Journal of Sociology, 102(2), 358–399. doi: 10.1086/230950.
Wallace, R. B., & Herzog, A. R. (1995). Overview of the health measures in the Health and Retirement Study. The Journal of Human Resources, 30, S84–S107. doi: 10.2307/146279.
Watson, N., & Wooden, M. (2009). Identifying factors affecting longitudinal survey response. In Methodology of longitudinal surveys (pp. 157–182). doi: 10.1002/9780470743874.ch10.
Wolff, J. L., Starfield, B., & Anderson, G. (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine, 162(20), 2269–2276. doi: 10.1001/archinte.162.20.2269.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Appendix
Appendix
See Tables 8, 9, 10, 11 and 12.
Rights and permissions
About this article
Cite this article
Shin, S., Kim, H. Health Trajectories of Older Americans and Medical Expenses: Evidence from the Health and Retirement Study Data Over the 18 Year Period. J Fam Econ Iss 39, 19–33 (2018). https://doi.org/10.1007/s10834-017-9542-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10834-017-9542-7