Abstract
Studies on the treatment of attention-deficit/hyperactivity disorder (ADHD) in adolescence indicate small to moderate treatment effects (e.g., of parent training). Self-help interventions might overcome structural and personal barriers to treatment utilization. The present proof-of-concept study examined the feasibility and effectiveness of a twelve-month, telephone-assisted self-help (TASH) intervention for caregivers of adolescents with ADHD. This intervention comprised 8 booklets on the management of ADHD-related problems and 14 telephone counseling sessions. Sixty-six caregivers participated in the study with a one-group pretest-posttest design (intention-to-treat sample). Of these, forty-three families completed the intervention in accordance with the study protocol (per-protocol sample). Compared to families with early discontinuation (n = 23, drop-out sample), adolescents in the per-protocol sample demonstrated a higher level of caregiver-rated emotional problems and a lower level of quality of life at pre-assessment. Caregivers in the per-protocol sample showed high adherence and reported high satisfaction with the intervention. Analyses of the per-protocol sample yielded significant, moderate to large pre-to-post improvements in caregiver-rated ADHD symptoms (primary outcome; d = 0.81, 95% confidence interval [0.51, 1.11]), oppositional, emotional and behavioral problems and quality of life of the adolescents, and caregiver self-efficacy during the intervention. In intention-to-treat analyses, which considered data of all 66 participants who had originally participated in the study, the pre-post differences in ADHD symptoms, emotional and behavioral problems, and quality of life remained at their significant level. These results provide initial support for the feasibility and effectiveness of the TASH intervention. Its efficacy compared to control conditions remains to be examined.
Highlights
-
Clinical guidelines recommend the use of parent training in the treatment of adolescents with ADHD.
-
In case of barriers to treatment utilization, low-threshold self-help interventions might be a viable treatment alternative.
-
This study evaluated a twelve-month telephone-assisted self-help intervention for caregivers of adolescents with ADHD using a pre-post design.
-
Per-protocol analyses revealed pre-post improvements in several outcomes, inter alia caregiver-rated ADHD symptoms. Caregivers indicated high satisfaction.
-
The study provides initial support for the feasibility and effectiveness of the intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Attention-deficit/hyperactivity disorder (ADHD) is a highly prevalent disorder in childhood and adolescence (worldwide pooled prevalence: 3.4%; Polanczyk et al., 2015). Although ADHD symptom severity tends to decline with age (e.g., Döpfner et al., 2015; Faraone et al., 2006), symptoms often persist into adolescence (Barkley et al., 1990; Bussing et al., 2010) and adulthood (Faraone et al., 2006). Adolescent ADHD is associated with high rates of comorbidities, especially with oppositional defiant disorder (ODD), but also with anxiety disorders and depression (Bussing et al., 2010). Moreover, affected adolescents experience functional impairment and reduced quality of life (Bussing et al., 2010), and impairments in functioning persist into adulthood (Barkley et al., 2006; Klein et al., 2012).
In general, adolescence is a sensitive life period in which the foundation is laid for adult functioning in different areas, for example regarding educational and occupational achievements, the development of adult relationships, and building a sense of identity and stable self-esteem (Brahmbhatt et al. 2016). Adolescents assume more responsibility relative to elementary school-age children, e.g., for their educational achievements, need to develop plans for the future, become increasingly independent of their caregivers, and have a growing need for privacy (Brahmbhatt et al. 2016; Merkt & Petermann, 2015; Wolraich et al., 2005). ADHD symptoms complicate these processes in various ways (for an overview, see Brahmbhatt et al. 2016; Chan et al., 2016). For instance, poor organization and planning associated with inattentive symptoms may impede the accomplishment of tasks at school, and impulsivity may lead to abrupt decisions without considering long-term consequences (Brahmbhatt et al. 2016).
Given the high comorbidity rates and potential adverse outcomes of adolescent ADHD, adequate treatment is crucial. National and international guidelines recommend pharmacological and non-pharmacological interventions (e.g., parent training, behavioral/cognitive-behavioral interventions) or a combination of both approaches. The patient’s age, severity of symptoms and potential comorbidities should be considered when selecting particular interventions (Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie, Psychosomatik und Psychotherapie [German Society of Child and Adolescent Psychiatry, Psychosomatics and Psychotherapy; DGKJP] et al., 2018; Taylor et al., 2004). Previous research has mostly demonstrated large effects of pharmacological treatment, especially stimulant medication, in both children and adolescents with ADHD (Barkley, 2004; Brahmbhatt et al. 2016; Chan et al., 2016). However, medication adherence may be low in adolescence (Buitelaar, 2017).
The majority of research on the treatment of ADHD concentrates on preschool- or school-age children (e.g., Daley et al., 2014; Sonuga-Barke et al., 2013). However, there is a range of studies on psychosocial interventions for adolescent ADHD. These largely focused on multicomponent interventions, predominantly including behavior therapy (e.g., parent or teacher training incorporating contingency management methods; e.g., Sibley et al., 2013), adolescent-directed skills training (e.g., Evans et al., 2016), and adolescent-directed cognitive-behavioral interventions (e.g., Boyer et al., 2015; Vidal et al., 2015; for systematic reviews on psychosocial interventions in adolescents with ADHD, see Chan et al., 2016; Evans et al., 2018). Most of these studies showed small to moderate treatment effects on parent-rated ADHD symptoms as well as comorbid emotional or behavioral symptoms, but moderate to large effects on functional outcomes such as organizational skills (see Chan et al., 2016). Based on the available evidence, Evans et al. (2018) conclude in their systematic review that behavioral parent training may be classified as “possibly efficacious treatment” for treating symptoms and impairment in adolescents with ADHD, while the evidence for combined training interventions is mixed (e.g., skills training combined with cognitive restructuring). Of note, Evans et al. (2018) regarded some of the interventions referred to as “cognitive-behavioral” above (Boyer et al., 2015; Vidal et al., 2015) as training interventions due to their focus on teaching skills. To sum up, some evidence especially supports the use of behavioral parent management training in the treatment of adolescents with ADHD (e.g., Evans et al., 2018). However, it differs from parent management training for preschool- or school-age children in that the adolescents may also attend sessions, and in that rules and contingencies are negotiated and laid down in a behavior contract (e.g., Evans et al., 2018; Wolraich et al., 2019). Moreover, problem-solving and communication training are considered as important treatment components, which mainly serve to reduce adolescent-parent conflicts (Brahmbhatt et al. 2016; Taylor et al., 2004; Wolraich et al., 2019).
Although there is some evidence for the benefit of psychosocial interventions for adolescents with ADHD, in Germany, a high percentage of children and adolescents with mental health problems do not utilize treatment (Klasen et al., 2017). This might be due to different barriers. First, there is a shortage of face-to-face treatment options in Germany and other European countries (Children’s Commissioner, 2016; Hintzpeter et al., 2014). Moreover, besides this structural barrier, personal barriers like limited time resources or fear of stigmatization might prevent adolescents and their caregivers from treatment utilization (Kazdin et al., 1997; Reardon et al., 2017). Low-threshold self-help interventions might help to overcome some of these barriers (e.g., Kazdin & Blase, 2011). They can be administered in case of limited local treatment options (e.g., in rural areas) or during waiting times for face-to-face treatment, and are suitable for adolescents and/or caregivers who are afraid of stigmatization. Compared to face-to-face treatment, self-help interventions are time- and cost-efficient. Moreover, self-help interventions were considered as useful during the COVID-19 pandemic due to their potential to improve treatment accessibility (Cortese et al., 2020).
Self-help interventions may be differentiated by the degree of additional therapist contact (Glasgow & Rosen, 1978). Interventions may be considered as “self-administered” if they are provided without any therapist contact. Minimal-contact interventions involve some therapist contact, but are primarily based on the self-help materials. Therapist-administered interventions include regular contacts with a therapist, which serve to clarify or elaborate on the self-help materials (Glasgow & Rosen, 1978).
Self-help parenting interventions for parents of preschool- and school-age children have demonstrated positive effects on parent-rated externalizing behavior and harsh and lax parenting behavior as well as mood, stress, and self-efficacy of the parents (Tarver et al., 2014). The effects were slightly larger when interventions with additional therapist contact were included into the analyses (Tarver et al., 2014).
Although individual therapy becomes more important as the child or adolescent grows older, parent training is still recommended for the treatment of adolescent ADHD (Taylor et al., 2004) and, as outlined above, probably shows some efficacy in this age group. However, to the best of our knowledge, no study to date has examined self-help parenting interventions for caregivers of adolescents with ADHD. The current proof-of-concept study aimed to examine the feasibility and effectiveness of a therapist-administered, telephone-assisted self-help (TASH) intervention for caregivers of adolescents with ADHD aged 13 to 17 years using a pre-post design. The intervention aims at reducing the adolescents’ ADHD and ODD symptoms as well as associated impairments in functioning and quality of life by teaching their caregivers techniques of negotiating rules and contingency management, communication skills and problem-solving skills. The caregivers are encouraged to use these techniques to help their adolescents to deal with their behavior problems and to reduce adolescent-caregiver conflicts. Previous observational studies examined an intervention very similar to that used in the present study, but with a focus on the needs of preschool- and school-age children. The findings demonstrated a reduction of ADHD and ODD symptoms during the intervention (Kierfeld & Döpfner, 2006; Mokros et al., 2015), with effects remaining stable in the longer term (Döpfner et al., 2021; Ise et al., 2015). Moreover, in two randomized controlled trials, the intervention was found to be effective in preschool-age children with externalizing behavior problems (Kierfeld et al., 2013) and in school-age children with residual functional impairment under methylphenidate medication (Dose et al., 2017). Furthermore, in the sample considered for the latter study, caregivers indicated a reduction of individually defined target problems during the intervention (Dose et al., 2020).
In the current study, we first aimed to explore the caregivers’ adherence to the intervention as well as the caregivers’ and referring physicians’ satisfaction with the intervention as indicators of the feasibility of the TASH intervention in routine care. Moreover, second, we performed a preliminary analysis on the effectiveness of the TASH intervention, analyzing changes in symptoms and associated variables during the intervention. We examined changes in symptoms, which are usually considered as primary outcome variable in psychotherapy research, but also changes in functional impairment and quality of life, as these concepts are often related to the need for treatment or seeking treatment (Epstein & Weiss, 2012). Moreover, as previous research on parent-directed self-help interventions in preschool- and school-age children has yielded effects on parent-related variables (Tarver et al., 2014), we examined changes in the caregivers’ self-efficacy. As we considered these analyses to be preliminary (also with regard to the pre-post design of our study), the aforementioned variables were analyzed in an explorative manner.
Method
The study was registered at clinicaltrials.gov (identifier: NCT01660464; URL: https://clinicaltrials.gov/ct2/show/study/NCT01660464) and approved by the Medical Ethics Committee of the University Hospital Cologne. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participating caregivers provided written informed consent.
Participants and Recruitment
Participants were caregivers, mostly mothers, of adolescents with ADHD. Caregivers were eligible for the study if their adolescent was aged 13 to 17 years and had been diagnosed with ADHD by a treating physician (pediatrician or child and adolescent psychiatrist), and if no comorbid condition required priority treatment (clinician rating based on interview with a caregiver). The planned overall sample size was n = 50, based on a power analysis assuming the detection of moderate effects (Cohen’s d = 0.50), an alpha error probability of 5% and a power of 95%, and accounting for potential dropouts.
The mean age of the adolescents was 14.29 years (SD = 0.93 [two missing values]; 86.4% male); the mean age of the participating caregivers was 44.76 years (SD = 4.78 [two missing values]). Most of the participants were the biological mothers of the children (n = 60; 90.9%). In three cases (4.5%), the biological father participated in the study; in the three remaining cases (4.5%), participants were adoptive mothers or foster mothers.
Participant recruitment was primarily undertaken by field staff of a pharmaceutical company, who informed pediatricians and child and adolescent psychiatrists across Germany about the study. Additionally, the study was promoted on the internet. The patients were diagnosed with ADHD by their local physicians and the physicians saw a need to support the families. Physicians registered families for the study, were informed about whether a family participated in the intervention and received a final report for their patient, which included information on the development of ADHD and ODD symptom severity as well as the development of individually defined problem behaviors during the intervention period. Apart from that, the physicians were not actively involved in the study. That is, members of the study staff reviewed more detailed study information with the participants, obtained informed consent from the participants, provided the self-help intervention and were responsible for data collection.
Study Design
The study used an observational design. Participating caregivers (n = 66) received a 12-month TASH intervention as an adjunct to ongoing routine clinical care, which included pharmacological treatment (65% of the patients were receiving pharmacological treatment at baseline). Assessments took place at baseline (pre-assessment) and after the 12-month intervention period (post-assessment).
Telephone-Assisted Self-Help Intervention
The caregivers participated in a 12-month behavioral TASH intervention for caregivers of adolescents with ADHD. The intervention consists of eight self-help booklets, which comprise information about ADHD and (cognitive-)behavioral interventions to deal with associated problems. In particular, the booklets cover the following subjects: (1) psychoeducation about ADHD, comorbidities and associated problems, causes of ADHD and different treatment options, (2) analysis and definition of individual target problems for treatment, psychoeducation on coercive caregiver-adolescent interactions, (3) encouragement of positive caregiver-adolescent interactions and promotion of communication skills, (4) re-evaluation of family rules, (5) discussion of family rules and problem-solving techniques, (6) clear demands and the reinforcement of desired behaviors, (7) adequate negative consequences for rule-breaking behaviors and contingency contracts, and (8) stress management techniques for caregivers (Kinnen et al., 2015). The booklets were sent to the caregivers on a fortnightly basis and the caregivers were asked to read the booklets and to implement the interventions described therein in their daily lives. To further support the caregivers, they additionally received 10 telephone consultations lasting for 30–40 min each in the first six months of the intervention and four booster telephone consultations in the second six months. These consultations served to further clarify and elaborate on the contents of the self-help materials and to support the caregivers in implementing the interventions, for example, by discussing problems or barriers to implementation. As outlined in the introductory section, interventions very similar to the one used in the current study, but focusing on the needs of preschool-age and school-age children, have been evaluated previously (e.g., Dose et al., 2017; Kierfeld & Döpfner, 2006; Kierfeld et al., 2013; Mokros et al., 2015). Compared to these previous interventions, the TASH intervention for caregivers of adolescents focused more on the negotiation of family rules and contingencies (with more active participation of the adolescent) as well as on problem-solving techniques and communication skills, which were mainly used to reduce caregiver-adolescent conflicts. Instead of token systems (which were included in the versions for preschool-age and school-age children), the TASH intervention for caregivers of adolescents addressed contingency contracts.
The consultations were provided by therapists in training to become cognitive-behavioral psychotherapists for children and adolescents. To ensure treatment integrity, the consultations were audiotaped and supervised regularly. Moreover, the therapists completed a checklist on treatment integrity after each session to assess which contents of the booklets had been dealt with (booklets 1 to 3 and booklet 8), how well the parents understood the contents of the booklets, and how well the parents implemented the interventions. The therapists indicated that on average, 96.7% of the contents of the booklets were discussed and 1.6% were “partially” discussed. The results for the parent-related variables (how well they understood the contents and how well thy implemented the interventions) are presented under the heading “adherence” in the results section.
Outcome Measures
Most outcome measures were rated by the participating caregiver. Questionnaires for the assessment of ADHD and ODD symptoms, behavior problems and strengths, adolescent quality of life, and self-efficacy of the caregivers were completed before the beginning of the intervention (baseline) and after the 12-month intervention period (post-assessment). Moreover, the caregivers’ and referring physicians’ satisfaction with the intervention was assessed at post-assessment. The respective questionnaires were sent to the caregivers and returned by mail. Where possible, any missing data were collected by telephone.
Symptom Checklist for Attention-Deficit/Hyperactivity Disorder (FBB-ADHS) and Symptom Checklist for Oppositional Defiant Disorder and Conduct Disorder (FBB-SSV), caregiver rating
The German symptom checklists FBB-ADHS (German: “Fremdbeurteilungsbogen für Aufmerksamkeitsdefizit-/Hyperaktivitätsstoerungen”; Döpfner et al., 2008) and FBB-SSV (German: “Fremdbeurteilungsbogen für Störungen des Sozialverhaltens”; Döpfner et al., 2008) assess ADHD symptoms or symptoms of ODD and conduct disorder, respectively, according to DSM-IV and ICD-10 criteria. The FBB-ADHS consists of 20 items that can be aggregated to a total score and two subscales (Inattention, Hyperactivity-Impulsivity). Both the subscale scores and the total score were considered in the present analyses. From the FBB-SSV, only the nine-item ODD subscale was considered in the current study. Moreover, the symptom-related overall functional impairment, functional impairment in relationships with adults and functional impairment in relationships with other children/adolescents were assessed with three items ([1] “on an overall level, the behavior problems are very stressful”, [2] “the behavior problems impact relationships with adults”, [3] “the behavior problems impact relationships with other children/adolescents”). In the present study, these three items were summarized in a Functional Impairment score. All items were rated on a 4-point Likert-type scale ranging from 0 (“not true”) to 3 (“completely true”), with higher scores indicating higher symptom severity or higher competences, respectively. Scale scores were calculated by averaging the associated item scores. All scale scores have demonstrated satisfactory internal consistency (α > 0.80) and factorial validity (Döpfner et al., 2008; Erhart et al., 2008; Görtz-Dorten et al., 2014). In the present sample, the internal consistency was α > 0.80 for the FBB-ADHS subscales, α = 0.86 for the FBB-ADHS total score, and α = 0.82 for the FBB-SSV ODD scale. The internal consistency of the three-item functional impairment scale was α = 0.65.
Strengths and Difficulties Questionnaire (SDQ), caregiver rating
The SDQ (Goodman, 1997) is a widely used questionnaire to assess behavioral problems and strengths. It consists of 25 items that are rated on a 3-point scale (“not true”, “somewhat true” or “certainly true”). The items can be aggregated to the five subscales Hyperactivity, Emotional Symptoms, Conduct Problems, Peer Problems, and Prosocial Behavior. Moreover, a total difficulties score can be calculated from the item scores related to hyperactivity, emotional symptoms, conduct problems, and peer problems. In the present study, we considered all SDQ subscale scores as well as the total difficulties score; scale scores were computed by averaging the associated item scores. The SDQ has demonstrated factorial validity, internal consistency, test-retest reliability, discriminative validity, and construct validity in various studies in a large number of countries (e.g., Becker et al., 2004; Goodman, 2001; He et al., 2013; Rothenberger et al., 2008). In the current sample, Cronbach’s α was not satisfactory for the subscales assessing conduct problems (α = 0.58), hyperactivity (α = 0.60), and prosocial behavior (α = 0.62). Therefore, the respective results for the present study have to be interpreted with caution. For the remaining subscales and the total difficulties score, the internal consistency was satisfactory (Emotional Problems: α = 0.72, Peer Problems: α = 0.77, Total Difficulties score: α = 0.74).
Parenting Self-Efficacy Questionnaire (FSW), caregiver rating
The Parenting Self-Efficacy Questionnaire (German: “Fragebogen zur Selbstwirksamkeit in der Erziehung”, FSW; Kliem et al., 2014) is a nine-item questionnaire to assess self-efficacy of caregivers. It is based on the Parenting Sense of Competence Scale (Johnston & Mash, 1989), the Self Efficacy for Parenting Task Index (Coleman & Karraker, 2000), and generalized measures of self-efficacy (Schwarzer & Jerusalem, 1999). The items are rated on a 4-point Likert-type scale ranging from 0 (“not true”) to 3 (“completely true”). For the present study, we considered a total score, which was computed by averaging the item scores. The FSW has shown satisfactory internal consistency, test-retest reliability, factorial validity, and convergent validity in a German sample of parents of children aged 2.5–6.5 years (Kliem et al., 2014). In the present sample, the internal consistency was also satisfactory (α = 0.73).
German Questionnaire for Measuring Health-related Quality of Life (KINDL), Caregiver Rating
The caregiver version of the KINDL (Ravens-Sieberer & Bullinger, 1998a, b) encompasses 24 items assessing health-related quality of life in children and adolescents. The items are rated on a 5-point Likert-type scale ranging from 1 (“never”) to 5 (“always”) and are associated with six dimensions (Physical Well-Being, Emotional Well-Being, Self-Esteem, Family, Friends, and Everyday Functioning [School]). For the present study, we only used the KINDL total score. This score was calculated by averaging the 24 item scores. The KINDL has demonstrated factorial validity. Moreover, each subscale and the total score have been shown to be internally consistent (α ≥ 0.70; Ravens-Sieberer & Bullinger, 1998a). In the current sample, Cronbach’s α for the total score was 0.81.
Client Satisfaction Questionnaire – revised (CSQ-R), Caregiver Rating
At the end of the treatment period, the caregivers rated their satisfaction with the intervention using a modified German translation of the CSQ (e.g. Plant & Sanders, 2007). The CSQ-R consists of 13 items that are rated on a 7-point scale ranging from 1 to 7, with higher scores indicating a higher level of satisfaction. A total satisfaction score is computed by averaging the individual item scores. The original English version of the CSQ (e.g. Plant & Sanders, 2007) and the German adaptation have demonstrated high internal consistency (α > 0.90). In the present sample, Cronbach’s α lay at 0.89.
Physician Satisfaction Questionnaire, physician rating
The referring physicians indicated their perception of treatment success (four items) and their satisfaction with the program (six items) using a self-developed questionnaire. The items were rated on a 4-point scale ranging from 1 (“not at all”) to 4 (“particularly satisfied”). A subscale score for the overall satisfaction with the intervention was computed by averaging the scores of the six associated items (Cronbach’s α = 0.83). Due to the low internal consistency of the scale derived from the items on treatment success (Cronbach’s α = 0.59), the results for these items were only considered on the item level.
Caregiver Adherence Checklist, therapist rating
During each telephone consultation, the therapists rated two aspects of the caregivers’ adherence: the degree to which caregivers implemented the interventions (i.e., the interventions described in the booklet they had worked through before the respective telephone counseling session, and the interventions described in the previously completed booklets) and the caregivers’ understanding of the contents of the booklets. Depending on the contents, the number of items considered in the Implementation scale varied per booklet; overall, 54 items were rated on a 3-point scale ranging from 0 to 2 (“not or hardly implemented”, “partly implemented”, “completely implemented”). The internal consistency of the Implementation scale was α = 0.96 in the current sample. Moreover, the therapists rated two items on how well caregivers had understood the contents of the booklets and on how well they had implemented the interventions after each session (3-point scale: poorly, moderately, well). The internal consistency of the Understanding scale, including all associated items and across all sessions, was α = 0.88.
Statistical Analyses
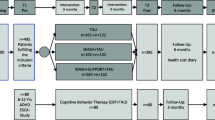
All analyses were performed using the Statistical Package for the Social Sciences, SPSS version 22.0. For the main analyses, we followed both an intention-to-treat and a per-protocol approach. For intention-to-treat analyses, we considered all 66 participants who met the inclusion criteria and agreed to participate in the study, regardless of whether they dropped out of the study, of how many telephone consultations they received and of whether they provided post-assessment data. On the other hand, the per-protocol sample included only families who completed the study as defined by the study protocol. That is, in this case, the per-protocol sample included all families who received all eight booklets, participated in at least nine telephone consultations (the minimum number of consultations needed to discuss all booklets) and completed the post-assessment (n = 43; see Fig. 1). The per-protocol sample is part of the intention-to-treat sample: Of the 66 families who were included into the study (as they met the inclusion criteria and agreed to participate), 43 completed the intervention (per-protocol sample). The remaining 23 families discontinued the intervention early and were considered as drop-outs (drop-out sample). As the present study was a proof-of-concept study, which sought to gain a first impression of the feasibility and potential benefits of the TASH intervention for caregivers of adolescents with ADHD, we considered the per-protocol analyses on the completing families as the primary analytical approach.
For the per-protocol analyses, the data set was nearly complete: At baseline, there were two items of the KINDL, which assesses quality of life, with two missing values each and two KINDL items with one missing value each. Moreover, there were three SDQ items with one missing value each and one item of the FBB-SSV subscale for the assessment of oppositional symptoms with one missing value. At post-assessment, there was one KINDL item with one missing value. Due to the low number of missing values in the per-protocol sample, scale scores were computed by averaging the available item scores.
In the intention-to-treat sample, there were nine additional cases with missing baseline data for the questionnaires on ADHD symptoms and oppositional symptoms. Moreover, only seven of the families who had discontinued the intervention provided post-assessment data for these two questionnaires. No post-assessment data on child quality of life, behavioral symptoms as assessed with the SDQ, and caregiver self-efficacy were available from the discontinuing families. Missing values in the intention-to-treat sample were imputed using a multiple imputation model, including completion status (completing vs. non-completing family), age, gender, and available baseline and post-assessment data for the outcome variables as predictors. The imputation was based on available baseline data of all 66 families as well as post-assessment data of the 43 families from the per-protocol sample and of the 7 families with early discontinuation who completed the post-assessment.
Caregiver adherence as rated by the therapists, and caregivers’ and referring physicians’ satisfaction with the intervention were analyzed on a descriptive basis. Pre-post differences in ADHD symptoms, oppositional symptoms, behavioral symptoms, child quality of life, and caregiver self-efficacy were analyzed using dependent samples t-tests. The Bonferroni-Holm procedure was applied to control for the familywise error rate in analyses involving subscales of the same questionnaire (Holm, 1979). The effect sizes d and their associated confidence intervals were computed using the formula provided by Algina and Keselman (2003). We applied the “Noncentral Distribution Calculator” (NDC; see Steiger, 2004) to determine confidence intervals for the noncentrality parameters of the t-distribution of our t-tests; confidence intervals for d could then be calculated on the basis of the confidence intervals for the noncentrality parameters (Algina & Keselman, 2003). Following Cohen (1988), effect sizes of 0.20 were considered as small, 0.50 as moderate, and 0.80 as large.
To gain an impression of the clinical significance of the per-protocol results for the symptom-based measures and quality of life, we combined the reliable change index (RCI) introduced by Jacobson and Truax (1991) with normative comparisons. The reliable change index indicates whether the observed pre-post change represents a psychometrically sound improvement that is not simply due to imprecision of the instrument used. The cut-off score for a reliable change is an absolute value of 1.96. For the normative comparisons, we considered the percentage of adolescents whose symptom severity or impairment in quality of life fell within the clinical range at post-assessment based on available norms for the respective instruments. For the questionnaires on ADHD symptoms and oppositional symptoms (FBB-ADHS and ODD scale of the FBB-SSV), age- and gender-adjusted Stanine values ≥ 8 were considered to be within the clinical range (Döpfner et al., 2008). For behavioral symptoms (SDQ), a total mean score > 0.8 was considered to be in the clinical range (Woerner et al., 2002). For the questionnaire on child quality of life (KINDL), values smaller than one standard deviation below the age- and sex-specific mean of a norm sample were considered to be in the clinical range (Ravens-Sieberer et al., 2008). Based on the combined consideration of the RCI and the normative comparisons, participants were assigned to one of five categories per measure: (1) improved (as indicated by the RCI) and in a normal range at post-assessment (as indicated by normative comparisons), (2) improved and in a clinical range, (3) unchanged and in a normal range, (4) unchanged and in a clinical range, (5) worsened. The analyses concerning the clinical significance of the results were performed both in the complete per-protocol sample and in subsamples of participants whose baseline scores fell within the clinical range for the respective instrument.
As there were no study-related restrictions regarding the use and change of medication during the intervention period, we analyzed pre-post changes in the use of medication to get an impression of whether the TASH intervention might be effective in reducing medication dosages and whether changes in medication might bias our symptom-related results. More precisely, we considered the percentage of adolescents using medication at baseline and at post-assessment and analyzed the percentages of adolescents whose medication dosage remained constant, was reduced or was increased during the intervention period. Moreover, we analyzed potential changes in methylphenidate dosage and atomoxetine dosage from baseline to post-assessment using dependent samples t-tests.
Results
Participant Flow and Baseline Data
The participant flow is displayed in Fig. 1. Of the 76 families who were initially registered for the study and met the inclusion criteria, 66 gave their informed consent to participate after receiving detailed information about the study procedure. Twenty-one families discontinued the intervention during the six-month intensive phase and two more families dropped out during the subsequent six-month booster phase. Reasons for discontinuation were no need for further treatment (n = 4) or personal reasons, health problems, or lack of time for the intervention (n = 14). One child was taken into custody; four families did not specify reasons for discontinuation. All families who completed the intervention provided post-assessment data. Thus, the per-protocol sample comprised 43 families. Compared to the caregivers who discontinued participation, those who completed the intervention indicated a higher level of emotional symptoms of their adolescent (subscale of the SDQ) and a lower level of adolescent quality of life (KINDL total score). No other baseline group differences between completers and non-completers were found (see Table 1).
Caregiver Adherence
On average, completing caregivers participated in 12.70 (SD = 1.34) telephone counseling sessions (out of 14 possible sessions, with 9 sessions considered as sufficient to complete the program; see statistical analyses section). Moreover, 66% of the counseling sessions were held on the originally arranged date. The average duration of the sessions in the per-protocol sample was 34.78 min (SD = 3.05).
The average therapist-rated caregiver adherence regarding the degree of implementation of single interventions was 1.50 (SD = 0.32) on a 3-point scale ranging from 0 “(intervention) not or hardly implemented” to 2 “(intervention) completely implemented”. Moreover, the therapists reported high levels of caregiver adherence in terms of a global understanding of the booklets’ contents and the global quality of the implementation of the interventions (average rating of 1.65 [SD = 0.32]).
Satisfaction with the Intervention
Twenty-eight of the 43 caregivers who completed the intervention (65%) provided ratings on their satisfaction with the program. In general, they expressed high satisfaction with most aspects of the intervention, e.g., they reported high satisfaction with the quality of the program, were satisfied with the amount of help received, and stated that the intervention had helped them to deal with their adolescent’s behavior more effectively (see Table S1). These aspects are particularly interesting as they hint at the acceptance of the self-help format and the perceived benefit of the intervention with regard to the adolescent’s behavior problems. Lower satisfaction was reported regarding the effect of the program on the caregivers’ partnership, which is understandable given that the program did not particularly target this aspect.
Of the 23 caregivers who discontinued participation, 11 caregivers provided ratings on the CSQ. In general, their satisfaction ratings were lower than those of the completing caregivers. Interestingly, they also reported high satisfaction with the quality of the program and the amount of help received, and indicated that they would come back to the program if they needed to seek help again in the future. However, compared to the completing families, these caregivers provided lower ratings on the item indicating the extent to which the program had helped them to deal with their adolescent’s behavior more effectively (see Table S1).
Twelve of the referring physicians of the completing families provided satisfaction ratings. They indicated high overall satisfaction, satisfaction with the quality of the program, and satisfaction with the information about the program, as well as with the information about the treatment progress of a specific referred family (see Table S2). The vast majority of the physicians expressed a wish for the program to be continued for the further referral of families. Moreover, the physicians reported high values in terms of the reduced burden the intervention brought about for their own practice with the respective family. However, ratings were lower for items on the physicians’ perceptions of reduced burden within the family, of the child’s symptom reduction, and of the improvement in medication compliance since the beginning of the intervention. Similar to the non-completing caregivers’ ratings, the referring physicians’ satisfaction related to the non-completing families (drop-out sample) was lower than that related to the completing families (per-protocol sample).
Pre-post Changes in Symptoms, Quality of Life, and Caregiver Self-efficacy
In the per-protocol sample (families who completed the study), dependent samples t-tests revealed significant changes from baseline to post-assessment for all outcome variables (ADHD symptoms, ODD symptoms, emotional and behavioral symptoms, quality of life, self-efficacy of the caregivers). Effect sizes were mostly moderate to high (see Table 2).
At the beginning of the intervention, 29 of the 43 adolescents in the per-protocol sample showed ADHD symptoms in the clinical range on the FBB-ADHS (age- and gender-adjusted Stanine value ≥ 8). Of these, 13 adolescents (45%) showed improvement and normalization, whereas three adolescents (10%) showed a reliable improvement based on the RCI but still had values in the clinical range. Of the 13 adolescents for whom the RCI did not indicate a reliable change, 11 still showed a caregiver-rated ADHD symptom severity in the clinical range at post-assessment (see Table S3). In addition, 47% of the 26 adolescents with baseline ODD symptoms (FBB-SSV) in the clinical range showed either a reliable improvement (three adolescents, i.e., 12%), a shift of symptom severity into a normal range (three adolescents, i.e., 12%), or both (six adolescents, i.e., 23%; see Table S3). Regarding emotional and behavioral symptoms as measured with the SDQ, the analyses revealed both a reliable improvement and post-assessment values in the normal range for about a third of the 32 adolescents with clinically relevant symptoms at baseline. Moreover, two adolescents (6%) showed a reliable improvement but still had symptoms in the clinical range. For a further five adolescents (16%), the RCI demonstrated no reliable change, but the normative comparisons indicated that their symptoms had shifted into a normal range (see Table S3). Caregivers reported reduced quality of life for 31 adolescents at baseline; for five (16%) of these adolescents, the analyses revealed a reliable improvement, for five adolescents (16%), the ratings shifted to the normal range during the intervention, and for eight adolescents (26%) there was both a reliable improvement and a shift to the normal range (see Table S3). Notably, on all measures, only individual adolescents demonstrated a reliable deterioration as indicated by the RCI (see Table S3).
In the intention-to-treat sample (all families who had been included into the study), significant pre-post changes emerged for caregiver ratings of ADHD symptoms on all scales of the FBB-ADHS, for the Functional Impairment scale associated with the FBB-ADHS/FBB-SSV, for the total difficulties score as well as the Hyperactivity, Emotional Symptoms, and Conduct Problems scores of the SDQ, and for quality of life as rated on the KINDL total scale. The effect sizes were mostly moderate. For oppositional symptoms as rated on the FBB-SSV ODD scale, caregiver self-efficacy (FSW), and the Peer Problems and Prosocial Behavior subscales of the SDQ, we did not detect any significant pre-post changes in the intention-to-treat sample (see Table S4).
Medication Changes
At baseline, 32 adolescents from the per-protocol sample were receiving pharmacological treatment (one missing value). Twenty-four adolescents were treated with methylphenidate alone, two with atomoxetine alone, and four adolescents received both methylphenidate and atomoxetine (two missing values for active substance). The mean methylphenidate dosage at baseline was 28.93 mg (SD = 22.18; range: 0–72; three missing values) and the mean atomoxetine dosage was 5.75 mg (SD = 14.61; range: 0–60; three missing values). Nine adolescents did not receive ADHD medication either at baseline or at post-assessment. For 12 adolescents the medication dosage was held constant during the intervention, for four adolescents the dosage increased, and for 13 adolescents the dosage was reduced (including six cases with discontinued medication; five missing values for medication status at post-assessment). The mean methylphenidate dosage at post-assessment was 20.05 mg (SD = 23.35; range: 0–70) and the mean atomoxetine dosage was 5.24 mg (SD = 15.81, range: 0–65). For methylphenidate, the dosage reduction was significant (methylphenidate: t = 2.79, df = 37, p < 0.01; atomoxetine: t = 1.30, df = 37, p = 0.10).
Discussion
The present study examined the feasibility and effectiveness of a TASH intervention for caregivers of 13–17-year-old adolescents with ADHD. The analyses revealed high caregiver adherence and high caregiver satisfaction with the intervention in the per-protocol sample, which included all families who had completed the study (i.e., who received all eight booklets, participated in at least nine telephone consultations and completed the post-assessment). This supports the feasibility of the intervention. Moreover, per-protocol analyses in this sample revealed a moderate to large reduction in ADHD and ODD symptom severity, functional impairment, and further emotional and behavior problems as well as a moderate increase in caregiver self-efficacy and a large increase in quality of life during the intervention period. These improvements cannot be explained by changes in the use of medication and were broadly in line with the pre-post changes observed during a one-year self-help intervention for caregivers of 6–12-year-old children with ADHD (Mokros et al., 2015). Intention-to-treat analyses, which included all families who met the inclusion criteria and agreed to participate, revealed a significant moderate reduction of ADHD symptom severity and emotional and behavior symptoms as well as a moderate increase in quality of life; however, no significant changes were observed for ODD symptom severity and caregiver self-efficacy in these analyses. The results indicate that the telephone-assisted, caregiver-directed self-help intervention might be a useful treatment for ADHD and associated problems. However, this interpretation should be made with caution, as the within-subject design (i.e., the lack of a control group) does not allow for a causal attribution of the observed changes to the intervention.
In terms of clinical significance, the results indicate that a substantial proportion of the adolescents showed either reliable improvement, a return to normal functioning, or both with regard to symptom-related measures and quality of life. Depending on the respective variable, between about a fifth and nearly half of the adolescents with baseline values in the clinical range experienced both reliable improvement and normalization. On the other hand, however, an even greater proportion continued to show elevated symptom levels at post-assessment. In other words, despite the statistical significance of the pre-post changes on all outcomes in the per-protocol sample, these changes did not lead to normalization in a high percentage of cases, indicating the need for further, possibly more intense treatment of the affected adolescents. The use of (assisted) self-help interventions as part of a stepped-care process is conceivable, with mild to moderate cases being treated at this low-threshold level and more intense treatment subsequently being offered to adolescents with residual symptoms or impairment.
A further observation was that in about a third of the adolescents in the per-protocol sample, the pharmacological treatment was discontinued or the dosage was reduced; only four adolescents were taking a higher dosage of their respective medication at post-assessment. It is possible that this reduction may be attributable to the intervention, as increased competencies of the caregivers and the adolescents in terms of managing ADHD-related problems might have enabled a reduction in medication. However, there might be other plausible explanations as well. For instance, the finding might also reflect a declining medication compliance in some of the cases. Randomized controlled trials are necessary to further illuminate this finding.
Caregivers in the non-completing families (drop-out sample) indicated a lower level of co-occurring emotional problems and a higher quality of life of their adolescent at the beginning of the study that caregivers in the completing families (per-protocol sample). Thus, in the current study, the caregivers of more severely affected adolescents were more likely to complete the intervention. This is in contrast to findings from the aforementioned studies examining a telephone-assisted self-help intervention for caregivers of younger children. These studies revealed that non-completing families had a higher percentage of single-parent families, a higher percentage of children under medication, and higher scores on the SDQ total scale and the SDQ Peer Problems scale (Döpfner et al., 2021; Mokros et al., 2015), as well as a lower level of prosocial behavior, a higher number of children living in the same household, and a lower number of years of education of the participating caregivers (Dose et al., 2017). Thus, stressors of the caregivers might be more relevant for the discontinuation of self-help interventions in childhood than in adolescence, while the psychological strain posed by the adolescents’ emotional symptoms and low quality of life might be factors that keep families in the program. However, this finding requires replication and further examination in future research.
The completing caregivers (per-protocol sample) expressed high satisfaction with different aspects of the intervention. For example, they were especially satisfied with the quality of the program and with the amount of help received, which supports the delivery of the treatment in a self-help format. Moreover, they were particularly satisfied with how the intervention helped them to deal with their adolescents’ behaviors, hinting at the perceived efficacy of the program. It should be noted that satisfaction ratings were only available for 28 caregivers who had completed the intervention. It might be possible that caregivers who were less satisfied with the TASH intervention did not provide satisfaction ratings, and that the actual average satisfaction was lower than indicated by the available ratings. Interestingly, the available satisfaction ratings of caregivers who discontinued the intervention indicated somewhat lower but nevertheless still high satisfaction with the intervention, although again, ratings were only provided by half of the non-completing families. Despite the limitation of the missing questionnaires, the overall high satisfaction hints at the acceptability and feasibility of the intervention in self-help format. Moreover, caregivers showed rather high levels of adherence, further supporting the feasibility of the intervention.
In clinical practice, telephone-assisted interventions should be easy to administer given that their implementation requires little technical equipment. However, despite scientific evidence for the efficacy of (assisted) self-help interventions in children with externalizing behavior disorders and potential advantages of this kind of intervention (e.g., cost effectiveness, accessibility in case of limited local treatment options), telephone-assisted self-help has not yet found its way into routine clinical care in Germany. For adolescents with ADHD, as outlined above, research on the efficacy and effectiveness of caregiver-directed self-help interventions is scarce, and there is a lack of randomized controlled trials demonstrating their efficacy. Thus, further research is required to examine their efficacy and practical utility in adolescents, including an analysis of their cost effectiveness. In this context, a comparison of the telephone-assisted intervention with the mere provision of the self-help materials (i.e., a purely self-administered intervention) could also be informative.
Several strengths and limitations of the study should be mentioned. A particular strength is that – to our knowledge – the study is the first to examine a telephone-assisted self-help intervention specifically tailored to the needs of caregivers of adolescents with ADHD. Besides the consideration of symptom-based measures, the adolescents’ quality of life was assessed as an outcome, which is in line with current recommendations (e.g., Coghill et al., 2009). Moreover, the intervention was carried out in routine care, with few restrictions regarding the composition of the sample, leading to a high external validity of the results.
On the other hand, several limitations have to be considered. First, and most importantly, the lack of a control group prevents us from drawing causal conclusions. Thus, while the current study revealed positive changes during the TASH intervention, further research is needed to clarify whether these changes can be attributed to the intervention and may not be explained by regression to the mean, the usual development of symptoms in adolescence, or other possible confounding influences. However, given that, to the best of our knowledge, no other study has considered a telephone-assisted self-help intervention in a sample of caregivers of adolescents with ADHD, the present study provides valuable first evidence for the feasibility and effectiveness of the intervention.
Second, the results of the intention-to-treat analyses might be biased by the high percentage of missing values for families with early discontinuation. Although we attempted to impute missing values with a state-of-the art model and included completion status as a predictor into the imputation model, we cannot fully rule out bias in favor of the intervention.
Third, all outcome variables were rated by the participating caregivers. As previous research has highlighted only low to moderate agreement between different raters in the assessment of psychiatric symptoms (e.g., De Los Reyes et al., 2015; Rescorla et al., 2013), it might be helpful to additionally consider the perspectives of the adolescents themselves. Although the TASH intervention addresses caregivers, it aims at reducing behavioral symptoms, associated functional impairment, and quality of life in adolescents, and it would be interesting to assess whether the youths themselves also perceive changes during the intervention period. This especially relates to functional impairment and reduced quality of life as indicators of the adolescents’ psychological strain. On the other hand, when it comes to symptomatic changes, caregiver ratings seem to be a more reliable source for the assessment of behavioral symptoms in adolescence than self-reports (Kuhn et al., 2017), and adolescents’ ratings of their symptoms should be considered as additional information to caregiver ratings rather than a substitute for them. As caregivers might tend to consider the intervention to be effective in order to justify the effort they have put into it, future research should also include blinded ratings (e.g., by a blinded clinician). Nevertheless, as caregivers receiving treatment in routine care are also unblinded, the present findings might well reflect the perception of changes during the intervention when applied in routine care. Moreover, the consideration of teacher ratings might be an important addition to future research, as these ratings could provide insight into the effects of the intervention on functioning in the school domain.
Forth, about 35% of the families did not complete the intervention. A recent study identified several barriers to the implementation of self-help interventions as perceived by caregivers, such as distractions by household chores and childcare (Tarver et al., 2021). The barriers specific to the implementation of self-help parenting interventions for caregivers of adolescents with ADHD remain to be explored.
Fifth, the fact that a pharmaceutical company was involved into recruitment and that most of the participants were registered by physicians might have limited the accessibility of the self-help intervention in this study (although the study was additionally promoted on the internet). This might have affected the external validity of the results. Finally, and in line with this, analyses of the sociodemographic characteristics suggest that the sample might not be representative of all families with an adolescent with ADHD, which may limit the generalizability of the results. Mokros et al. (2015) found that participants of a self-help program for caregivers of school-age children with ADHD had a higher socioeconomic status compared to a representative norm sample. Although we did not compare our sample to a representative sample, the percentage of families with a migration background (9% in the per-protocol sample) seems rather low, while the educational level seems rather high (a mean of 13 years of education is equivalent to the German high school graduation or a comparable university entrance-level qualification). Future research needs to clarify for which caregiver characteristics self-help interventions are most suitable. In this regard, it could be useful to have a closer look at the characteristics which moderate treatment outcome. In the current sample, comparisons of adolescents demonstrating both clinically reliable improvement (as indicated by the RCI) and normalization (as indicated by normative comparisons) with adolescents without such improvement did not yield any significant differences in baseline symptom severity, age and sex (results not presented in this article). However, this might be due to the small sample size, especially regarding the groups with reliable improvement and normalization. The identification of families for whom (telephone-assisted) self-help is helpful remains an important direction for future research in larger samples.
Conclusions
The present study provides support for the feasibility of TASH for caregivers of adolescents with ADHD and yields initial support for its effectiveness. The analyses indicate positive changes in caregiver-rated ADHD symptoms, co-occurring ODD symptoms, as well as emotional and behavioral problems, quality of life and caregiver self-efficacy during the intervention. TASH might help to improve treatment accessibility, for example in the scope of a stepped-care process. However, the efficacy and benefits of the intervention need to be examined further using randomized controlled trials and including non-treated or active control conditions. Moreover, as direct therapy is increasingly important the older the child or adolescent becomes, the development of self-help programs directly addressing adolescents with ADHD could be considered.
References
Algina, J., & Keselman, H. J. (2003). Approximate confidence intervals for effect sizes. Educational and Psychological Measurement, 63, 537–553. https://doi.org/10.1177/0013164403256358.
Barkley, R. A. (2004). Adolescents with attention-deficit/hyperactivity disorder: An overview of empirically based treatments. Journal of Psychiatric Practice, 10, 39–56. https://doi.org/10.1097/00131746-200401000-00005.
Barkley, R. A., Fischer, M., Smallish, L., & Fletcher, K. (2006). Young adult outcome of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child & Adolescent Psychiatry, 45(2), 192–202. https://doi.org/10.1097/01.chi.0000189134.97436.e2.
Barkley, R. A., Fischer, M., Edelbrock, C. S., & Smallish, L. (1990). The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 546–557. https://doi.org/10.1097/00004583-199007000-00007
Becker, A., Woerner, W., Hasselhorn, M., Banaschewski, T., & Rothenberger, A. (2004). Validation of the parent and teacher SDQ in a clinical sample. European Child and Adolescent Psychiatry, 13, 11–16. https://doi.org/10.1007/s00787-004-2003-5.
Boyer, B. E., Geurts, H. M., Prins, P. J., & Van der Oord, S. (2015). Two novel CBTs for adolescents with ADHD: The value of planning skills. European Child and Adolescent Psychiatry, 24, 1075–1090. https://doi.org/10.1007/s00787-014-0661-5.
Brahmbhatt, K., Hilty, D. M., Hah, M., Han, J., Angkustsiri, K., & Schweitzer, J. (2016). Diagnosis and treatment of ADHD during adolescence in the primary care setting: Review and future directions. Journal of Adolescent Health, 59, 135–143. https://doi.org/10.1016/j.jadohealth.2016.03.025.
Buitelaar, J. K. (2017). Optimising treatment strategies for ADHD in adolescence to minimise ‘lost in transition’ to adulthood. Epidemiology and Psychiatric Sciences, 26, 448–452. https://doi.org/10.1017/S2045796017000154.
Bussing, R., Mason, D. M., Bell, L., Porter, P., & Garvan, C. (2010). Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 595–605. https://doi.org/10.1016/j.jaac.2010.03.006.
Chan, E., Fogler, E. M., & Hammerness, P. G. (2016). Treatment of attention-deficit/hyperactivity disorders in adolescence. A systematic review. Clinical Review & Education, 315, 1997–2008.
Children’s Commissioner (2016). Lightning review: Access to child and adolescent mental health services. https://www.childrenscommissioner.gov.uk/wp-content/uploads/2017/06/Childrens-Commissioners-Mental-Health-Lightning-Review.pdf. Accessed 25 October 2022.
Coghill, D., Danckaerts, M., Sonuga-Barke, E., & Sergeant, J., ADHD European Guidelines Group. (2009). Practitioner review: Quality of life in child mental health—conceptual challenges and practical choices. Journal of Child Psychology and Psychiatry, 50, 544–561.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, London: Erlbaum.
Coleman, P. K., & Karraker, K. H. (2000). Parenting self-efficacy among mothers of school-aged children: conceptualisation, measurement and correlates. Family Relations, 49, 13–24. https://doi.org/10.1111/j.1741-3729.2000.00013.x.
Cortese, S., Asherson, P., Sonuga-Barke, E., Banaschewski, T., Brandeis, D., Buitelaar, J., Coghill, D., Daley, D., Danckaerts, M., Dittmann, R. W., Doepfner, M., Ferrin, M., Hollis, C., Holtmann, M., Konofal, E., Lecendreux, M., Santosh, P., Rothenberger, A., Soutullo, C., & Simonoff, E. (2020). ADHD management during the COVID-19 pandemic: Guidance from the European ADHD Guidelines Group. The Lancet Child & Adolescent Health, 4, 412–414. https://doi.org/10.1016/S2352-4642(20)30110-3.
Daley, D., Van der Oord, S., Ferrin, M., Danckaerts, M., Doepfner, M., Cortese, S., & Sonuga-Barke, E., on behalf of the European ADHD Guidelines Group. (2014). Behavioral interventions in attention-deficit/hyperactivity disorder: A meta-analysis of randomized controlled trials across multiple outcome domains. Journal of the American Academy of Child and Adolescent Psychiatry, 53, 835–847. https://doi.org/10.1016/j.jaac.2014.05.013.
Deutsche Gesellschaft für Kinder- und Jugendpsychiatrie, Psychosomatik und Psychotherapie (DGKJP), Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde, & Deutsche Gesellschaft für Sozialpädiatrie und Jugendmedizin. (2018). Langfassung der interdisziplinären evidenz- und konsensbasierten (S3) Leitlinie “Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (ADHS) im Kindes-, Jugend- und Erwachsenenalter” [Long version of the interdisciplinary evidence- and consensus-based (S3) guideline “Attention-Deficit/Hyperactivity Disorder (ADHD) in children, adolescents and adults”]. Retrieved from www.awmf.org/uploads/tx_S3_ADHS_2018-06.pdf.
Döpfner, M., Görtz-Dorten, A., & Lehmkuhl, G. (2008). Diagnostik-System für Psychische Störungen nach ICD-10 und DSM-IV für Kinder und Jugendliche - II [Diagnostic System for Mental Disorders in Childhood and Adolescence According to ICD-10 and DSM-5]. Bern: Verlag Hans Huber.
Döpfner, M., Hautmann, C., Görtz-Dorten, A., Klasen, F. & Ravens-Sieberer, U. (2015). Long-term course of ADHD symptoms from childhood to early adulthood in a community sample. European Child and Adolescent Psychiatry, 24, 665–673. https://doi.org/10.1007/s00787-014-0634-8.
Döpfner, M., Liebermann-Jordanidis, H., Kinnen, C., Hallberg, N., Mokros, L., Benien, N., Mütsch, A., Schürmann, S., Wolf Metternich-Kaizman, T., Hautmann, C., & Dose, C. (2021). Long-term effectiveness of guided self-help for parents of children with ADHD in routine care - an observational study. Journal of Attention Disorders, 25, 265–274. https://doi.org/10.1177/1087054718810797.
Dose, C., Waschau, F., von Wirth, E., & Döpfner, M. (2020). The improvement of individually defined problem behaviors during a telephone-assisted self-help intervention for parents of pharmacologically treated children with ADHD. Zeitschrift für Kinder- und Jugendpsychiatrie, 48, 215–223. https://doi.org/10.1024/1422-4917/a000726.
Dose, C., Hautmann, C., Bürger, M., Schürmann, S., Woitecki, K., & Döpfner, M. (2017). Telephone-assisted self-help for parents of children with attention-deficit/hyperactivity disorder who have residual functional impairment despite methylphenidate treatment: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 58, 682–690. https://doi.org/10.1111/jcpp.12661.
Epstein, J. N., & Weiss, M. D. (2012). Assessing treatment outcomes in attention-deficit/hyperactivity disorder: A narrative review. The Primary Care Companion for CNS Disorders, 14. https://doi.org/10.4088/PCC.11r01336.
Erhart, M., Döpfner, M., & Ravens-Sieberer, U., BELLA Study Group. (2008). Psychometric properties of two ADHD questionnaires: Comparing the Conners’ scale and the FBB-HKS in the general population of German children and adolescents – results of the BELLA study. European Child and Adolescent Psychiatry, 17, 106–115. https://doi.org/10.1007/s00787-008-1012-1.
Evans, S. W., Owens, J. S., Wymbs, B. T., & Ray, A. R. (2018). Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 47, 157–198. https://doi.org/10.1080/15374416.2017.1390757.
Evans, S. W., Langberg, J. M., Schultz, B. K., Vaughn, A., Altaye, M., Marshall, S. A., & Zoromski, A. K. (2016). Evaluation of a school-based treatment program for young adolescents with ADHD. Journal of Consulting and Clinical Psychology, 84, 15–30. https://doi.org/10.1037/ccp0000057.
Faraone, S. V., Biederman, J., & Mick, E. (2006). The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine, 36, 159–165. https://doi.org/10.1017/S003329170500471X.
Glasgow, R. E., & Rosen, G. M. (1978). Behavioral bibliotherapy: A review of self-help behavior therapy manuals. Psychological Bulletin, 85, 1–23. https://doi.org/10.1037/0033-2909.85.1.1.
Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1337–1345. https://doi.org/10.1097/00004583-200111000-00015.
Görtz-Dorten, A., Ise, E., Hautmann, C., Walter, D., & Döpfner, M. (2014). Psychometric properties of a German parent rating scale for oppositional defiant and conduct disorder (FBB-SSV) in clinical and community samples. Child Psychiatry and Human Development, 45, 388–397. https://doi.org/10.1007/s10578-013-0409-3.
He, J. P., Burstein, M., Schmitz, A., & Merikangas, K. R. (2013). The Strengths and Difficulties Questionnaire (SDQ): The factor structure and scale validation in U.S. adolescents. Journal of Abnormal Child Psychology, 41, 583–595. https://doi.org/10.1007/s10802-012-9696-6.
Hintzpeter, B., Metzner, F., Pawils, S., Bichmann, H., Kamtsiuris, P., Ravens-Sieberer, U., & Klasen, F., BELLA study group. (2014). Inanspruchnahme von ärztlichen und psychotherapeutischen Leistungen durch Kinder und Jugendliche mit psychischen Auffälligkeiten. Ergebnisse der BELLA-Studie [Medical and psychotherapeutic health care utilization of children and adolescents with mental health problems: Results of the BELLA Study]. Kindheit und Entwicklung, 23, 229–238.
Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6, 65–70.
Ise, E., Kierfeld, F., & Döpfner, M. (2015). One-year follow-up of guided self-help for parents of preschool children with externalizing behavior. Journal of Primary Prevention, 36, 33–40. https://doi.org/10.1007/s10935-014-0374-z.
Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. https://doi.org/10.1037/0022-006X.59.1.12.
Johnston, C., & Mash, E. J. (1989). A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology, 18, 167–175. https://doi.org/10.1207/s15374424jccp1802_8.
Kazdin, A. E., & Blase, S. L. (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science, 6, 21–37. https://doi.org/10.1177/1745691610393527.
Kazdin, A. E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65, 453–463. https://doi.org/10.1037/0022-006X.65.3.453.
Kierfeld, F., & Döpfner, M. (2006). Bibliotherapie als Behandlungsmöglichkeit bei Kindern mit externalen Verhaltensstörungen [Bibliotherapy as a self-help program for parents of children with externalizing problem behavior]. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie, 34, 377–386. https://doi.org/10.1024/1422-4917.34.5.377.
Kierfeld, F., Ise, E., Hanisch, C., Goertz-Dorten, A., & Döpfner, M. (2013). Effectiveness of telephone-assisted parent-administered behavioural family intervention for preschool children with externalizing problem behavior: A randomised controlled trial. European Child and Adolescent Psychiatry, 22, 553–565. https://doi.org/10.1007/s00787-013-0397-7.
Kinnen, C., Rademacher, C., & Döpfner, M. (2015). ADHS-Coaching für Eltern (13–18): Ein Selbsthilfeprogramm für Eltern von Jugendlichen im Alter von 13 bis 18 Jahren [ADHD coaching for parents: A self-help program for parents of adolescents aged 13 to 18 years]. Cologne, Germany: Department of Child and Adolescent Psychiatry, Psychosomatics and Psychotherapy at the University Hospital Cologne.
Klasen, F., Meyrose, A. K., Otto, C., Reiß, F., & Ravens-Sieberer, U. (2017). Psychische Auffälligkeiten von Kindern und Jugendlichen in Deutschland [Mental problems of children and adolescents in Germany]. Monatsschrift Kinderheilkunde, 165, 402–407.
Klein, R. G., Mannuzza, S., Olazagasti, M. A. R., Roizen, E., Hutchison, J. A., Lashua, E. C., & Castellanos, F. X. (2012). Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Archives of General Psychiatry, 69, 1295–1303. https://doi.org/10.1001/archgenpsychiatry.2012.271.
Kliem, S., Kessemeier, Y., Heinrichs, N., D”pfner, M., & Hahlweg, K. (2014). Der Fragebogen zur Selbstwirksamkeit in der Erziehung (FSW) [The Parenting Self-Efficacy Questionnaire (FSW)]. Diagnostica, 60, 35–45. https://doi.org/10.1026/0012-1924/a000107.
Kuhn, C., Aebi, M., Jakobsen, H., Banaschewski, T., Poustka, L., Grimmer, Y., & Steinhausen, H. C. (2017). Effective mental health screening in adolescents: should we collect data from youth, parents or both. Child Psychiatry & Human Development, 48, 385–392. https://doi.org/10.1007/s10578-016-0665-0.
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A. G., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141, 858–900. https://doi.org/10.1037/a0038498.
Merkt, J., & Petermann, F. (2015). ADHS bei Jugendlichen und jungen Erwachsenen [ADHD in adolescents and young adults]. Zeitschrift für Psychiatrie, Psychologie und Psychotherapie, 63, 187–196. https://doi.org/10.1024/1661-4747/a000239.
Mokros, L., Benien, N., Mütsch, A., Kinnen, C., Schürmann, S., Wolf Metternich-Kaizman, T., … & Döpfner, M. (2015). Angeleitete Selbsthilfe für Eltern von Kindern mit Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung: Konzept, Inanspruchnahme und Effekte eines bundesweiten Angebotes – eine Beobachtungsstudie [Guided self-help interventions for parents of children with ADHD - concept, referral and effectiveness in a nationwide trial. An observational study]. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie, 43, 275–288. https://doi.org/10.1024/1422-4917/a000348.
Plant, K. M., & Sanders, M. R. (2007). Reducing problem behavior during care-giving in families of preschool-aged children with developmental disabilities. Research in Developmental Disabilities, 28, 362–385. https://doi.org/10.1016/j.ridd.2006.02.009.
Polanczyk, G. V., Salum, G. A., Sugaya, L. S., Caye, A., & Rohde, L. A. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56, 345–365. https://doi.org/10.1111/jcpp.12381.
Ravens-Sieberer, U., & Bullinger, M. (1998a). Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Quality of Life Research, 7, 399–407. https://doi.org/10.1023/a:1008853819715.
Ravens-Sieberer, U., & Bullinger, M. (1998b). News from the KINDL-questionnaire: A new version for adolescents. Quality of Life Research, 7, 653.
Ravens-Sieberer, U., Erhart, M., Wille, N., & Bullinger, M. (2008). Health-related quality of life in children and adolescents in Germany: Results of the BELLA study. European Child & Adolescent Psychiatry, 17, 148–156. https://doi.org/10.1007/s00787-008-1016-x.
Reardon, T., Harvey, K., Baranowska, M., O’Brien, D., Smith, L., & Creswell, C. (2017). What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. European Child & Adolescent Psychiatry, 26, 623–647. https://doi.org/10.1007/s00787-016-0930-6.
Rescorla, L. A., Ginzburg, S., Achenbach, T. M., Ivanova, M. Y., Almqvist, F., Begovac, I., & Verhulst, F. C. (2013). Cross-informant agreement between parent-reported and adolescent self-reported problems in 25 societies. Journal of Clinical Child & Adolescent Psychology, 42, 262–273. https://doi.org/10.1080/15374416.2012.717870.
Rothenberger, A., Becker, A., Erhart, M., Wille, N., & Ravens-Sieberer, U., BELLA study group. (2008). Psychometric properties of the Parent Strengths and Difficulties Questionnaire in the general population of German children and adolescents: Results of the BELLA study. European Child and Adolescent Psychiatry, 17(Suppl 1), 99–105. https://doi.org/10.1007/s00787-008-1011-2.
Schwarzer, R. & Jerusalem, M. (Ed.) (1999). Skalen zur Erfassung von Lehrer- und Schülermerkmalen. Dokumentation der psychometrischen Verfahren im Rahmen der Wissenschaftlichen Begleitung des Modellversuchs Selbstwirksame Schulen [Scales for the assessment of teacher and pupil characteristics]. Berlin: Freie Universität Berlin.
Sibley, M. H., Pelham, W. E. J., Derefinko, K. J., Kuriyan, A. B., Sanchez, F., & Graziano, P. A. (2013). A pilot trial of Supporting Teens’ Academic Needs Daily (STAND): A parent-adolescent collaborative intervention for ADHD. Journal of Psychopathology and Behavioral Assessment, 35, 436–449. https://doi.org/10.1007/s10862-013-9353-6.
Sonuga-Barke, E. J., Brandeis, D., Cortese, S., Daley, D., Ferrin, M., & Holtmann, M., European ADHD Guidelines Group. (2013). Nonpharmacological interventions for ADHD: Systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170, 275–289. https://doi.org/10.1176/appi.ajp.2012.12070991.
Steiger, J. H. (2004). Beyond the F-test: Effect size confidence intervals and tests of close fit in the analysis of variance and contrast analysis. Psychological Methods, 9, 164–182. https://doi.org/10.1037/1082-989X.9.2.164.
Tarver, J., Daley, D., Lockwood, J., & Sayal, K. (2014). Are self-directed parenting interventions sufficient for externalising behaviour problems in childhood? A systematic review and meta-analysis. European Child and Adolescent Psychiatry, 23, 1123–1137. https://doi.org/10.1007/s00787-014-0556-5.
Tarver, J., Daley, D., & Sayal, K. (2021). A self‐help version of the New Forest Parenting Programme for parents of children with attention deficit hyperactivity disorder: A qualitative study of parent views and acceptability. Child and Adolescent Mental Health. Advance online publication. https://doi.org/10.1111/camh.12476.
Taylor, E., Döpfner, M., Sergeant, J., Asherson, P., Banaschewski, T., Buitelaar, J., & Zuddas, A. (2004). European clinical guidelines for hyperkinetic disorder–first upgrade. European Child & Adolescent Psychiatry, 13(1), i7–i30. https://doi.org/10.1007/s00787-004-1002-x.
Vidal, R., Castells, J., Richarte, V., Palomar, G., Garc¡a, M., Nicolau, R., & Ramos-Quiroga, J. A. (2015). Group therapy for adolescents with attention-deficit/hyperactivity disorder: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 275–282. https://doi.org/10.1016/j.jaac.2014.12.016.
Woerner, W., Becker, A., Friedrich, C., Klasen, H., Goodman, R., & Rothenberger, A. (2006). Normierung und Evaluation der deutschen Elternversion des Strengths and Difficulties Questionnaire (SDQ): Ergebnisse einer repräsentativen Felderhebung [Normative data and evaluation of the German parent-rated Strengths and Difficulties Questionnaire (SDQ): Results of a representative field study]. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie, 30, 105–112.
Wolraich, M. L., Wibbelsman, C. J., Brown, T. E., Evans, S. W., Gotlieb, E. M., Knight, J. R., & Wilens, T. (2005). Attention-deficit/hyperactivity disorder among adolescents: A review of the diagnosis, treatment, and clinical implications. Pediatrics, 115, 1734–1746. https://doi.org/10.1542/peds.2004-1959.
Wolraich, M. L., Hagan, J. F., Allan, C., Chan, E., Davison, D., Earls, M., & Zurhellen, W. (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 144(4), e20192528.
Funding
The study was supported by Eli Lilly and Company (unrestricted grant). Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Christina Dose performed the analyses and wrote the first draft of the manuscript. Christopher Hautmann was involved in the development of the study-related materials and provided methodological advice during the conduct of the study. Claudia Kinnen and Christiane Rademacher supervised the therapists conducting the telephone coaching, Tina Roschmann conducted the telephone coaching and the assessment, Manfred Döpfner developed the intervention and the study design. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Manfred Döpfner received income as head, supervisor, and lecturer of the School of Child and Adolescent Cognitive Behavior Therapy at the University Hospital Cologne and as a consultant for child behavior therapy at the National Association of Statutory Health Insurance Physicians (Kassenärztliche Bundesvereinigung). He also received royalties from treatment manuals, books and psychological tests published by Beltz, Elsevier, Enke, Guilford, Hogrefe, Huber, Kohlhammer, Schattauer, Springer, Wiley. Christina Dose received royalties from a publishing company (Hogrefe) as an author of self-help books for parents of preschool- and school-age children with ADHD similar to the program examined in this study. Claudia Kinnen and Christiane Rademacher received income as supervisors and lecturers of the School of Child and Adolescent Cognitive Behavior Therapy at the University Hospital Cologne and received royalties from treatment manuals published by Beltz and Hogrefe. Christopher Hautmann and Tina Roschmann are not aware of any conflict of interest that might be perceived as influencing the objectivity of the manuscript.
Ethics approval
The study was approved by the Medical Ethics Committee of the University Hospital Cologne, Cologne, Germany. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
All participating caregivers provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dose, C., Roschmann, T., Kinnen, C. et al. Telephone-Assisted Self-Help for Caregivers of Adolescents with Attention-Deficit/Hyperactivity Disorder: An Observational Proof-of-Concept Study. J Child Fam Stud 33, 1752–1767 (2024). https://doi.org/10.1007/s10826-024-02831-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-024-02831-0