Abstract
Young people can be reluctant to seek help for a mental health problem due to many factors, and research suggests that early and meaningful intervention within this demographic is essential to support improved quality of life and reduce youth death by suicide. The role of informal sources of help in youth mental health help-seeking pathways is an important subject however, there are no reviews on this topic. The aim of this scoping review was to map the existing literature regarding how informal sources of help affect young people’s access to, engagement with and maintenance in professional mental health care. Nine databases were searched for original peer-reviewed research published between 1994 and 2021 with young people aged 10–25 years. A thematic analysis was performed on 32 studies that met selection criteria. Two key themes were identified: 1. Informal helpers as supportive intermediaries and 2. Informal helpers as obstructive forces. This review found that informal sources of help are dynamic and essential pathway agents in helping or hindering young people with accessing and staying engaged in professional mental health care. Further research on this topic with young people about their actual help-seeking experiences is required. Through an improved understanding of how these interpersonal relationships function within a young person’s help-seeking process, on a spectrum of supportive to obstructive behaviour, services and practitioners can ensure the provision of responsive and appropriate support to young people and their families, facilitating service use and ensuring better outcomes for young people’s mental health and quality of life.
Highlights
-
This is the first known review that maps the evidence regarding the role of informal sources of help in young people’s (10–25 years) mental health help-seeking pathways.
-
Friends and family are central agents in young people’s mental health help-seeking pathways and can provide important facilitative resources or obstruct access to professional services.
-
Future research can directly inquire with young people about their actual help-seeking experiences and the role of informal supports in their help-seeking pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mental health problems are reported as first emerging during childhood and adolescence (Kessler et al. 2007) and it is estimated that approximately one in seven young people aged 10–19 years across the globe experience mental health conditions (World Health Organisation (WHO), 2021). The impact of poor mental health in youth has been linked with lower quality of life, educational difficulties, disability, and suicide across the lifespan (WHO, 2021; Bilsen, 2018; Finkelhor et al., 2015; Pompili, 2018; Patel et al. 2007). As such, youth mental health has become an important global healthcare issue (WHO, 2021) and despite the increase in awareness campaigns and service provision, as well as increased discussion around mental health in high-income countries, young people are described as reluctant to seek help with their problems (Goodwin et al. 2016). Accordingly, it is important to understand the different factors that are involved in youth mental health help-seeking processes that can facilitate engagement in appropriate and timely mental health interventions, which can support better outcomes for young people (WHO, 2021).
Help-seeking for a mental health problem is a complex process that involves problem solving through interpersonal interaction (Cornally & McCarthy, 2011; Chan, 2013). There are many models and approaches used when examining barriers and facilitators to help-seeking behaviour (Pearson & Hyde, 2021) and some research points to the need for specific models and approaches for younger people (Breslin et al. 2022). The term ‘young people’ or ‘youth’ can refer to individuals aged between 10 and 29 years however, this varies across culture and can be subject to regional economic conditions (UNESCO, 2010; Arnett, 2014; WHO, 2022; Patel et al. 2007). Youth can be regarded as a time of transition and as a distinct life-stage due to the rapid changes in personal, cognitive, physical, social, and sexual development (Best & Ban, 2021). In high-income countries, youth can be described as having two stages: firstly, the developmental stage of adolescence, which begins around 10 at the onset of puberty and ends somewhere between 19 and 21 years of age (Best & Ban, 2021); and secondly, emerging adulthood, a stage often mediated by economic opportunities that begins at the end of adolescence and lasts until after 26 years of age (Arnett, 2014). Group membership can be defined by developmental status, that the key physiological, psychological, and cognitive milestones that would classify an individual within Western paradigms as having entered ‘adulthood’ have not yet been reached (Arnett, 2014). As such, individuals experiencing this life-stage of youth can be viewed as belonging to a distinct cultural group of youth (Sawyer et al., 2018; Rickwood et al., 2019; Lynch et al. 2021).
The majority of research over the previous two decades has focused on identifying the factors in the help-seeking process that discourage young people from asking for help for a mental health problem. To date, research has identified the types of personal factors that can impact youth help-seeking pathways, such as the prioritising of self-reliance and self-management (Biddle et al. 2007; Loureiro et al. 2013; Burlaka et al. 2014; Rowe et al. 2014). Mental health literacy is considered to play an important role (Gulliver et al. 2010) as does attitudes towards professional help (Klineberg et al. 2011; Pheko et al. 2013; Pumpa & Martin, 2015) and beliefs about mental health care (Rothi & Leavey, 2006; Gulliver et al. 2010; Eisenberg et al. 2012). Much research has highlighted the important impact of previous negative or unsuccessful experiences of help-seeking, either personally or vicariously (Gilchrist & Sullivan, 2006; Charman et al. 2010; Wilson & Deane 2012; Rowe et al. 2014; Ryan et al. 2014). Research also points to issues with practical barriers such as access, unsuitable services, financial barriers, and a lack of services in rural areas (Rothi & Leavey, 2006; Hernan et al. 2010; Radez et al. 2021), all of which can be exacerbated for young people experiencing marginalisation (DeAnstiss et al. 2009; Collins and Barker 2009).
A consistent finding across youth mental health help-seeking literature regards the role of social factors. Stigma, community views of mental health and cultural expressions of distress have been found to have an important impact on help-seeking (Rothi & Leavey, 2006; Gulliver et al., 2010; Nam et al. 2010; Michelmore & Hindley, 2012; Rowe et al. 2014; Goodwin et al. 2016). Gatekeepers to services, such as youth workers, teachers or GP’s have been found to have an important role in young people accessing help (Rickwood et al. 2007; Kelly et al. 2011; Quinn et al. 2009; Leavey et al. 2011), especially for young people with refugee status (Ellis et al. 2010) or for those experiencing homelessness (Collins and Barker 2009). Social relationships are key to young people’s quality of life (Moen and Hall-Lord 2019; Mahsoon et al. 2020; Breslin et al. 2022) and it is well established that friends and family members are young people’s preferred sources of help for their mental health problems (Michelmore & Hindley, 2012; Rowe et al. 2014). However, the role that these close relationships play in young people’s help-seeking pathways is under researched and not well understood, presenting an important gap in the literature base (Mariu et al. 2012; Michelmore & Hindley, 2012; MacDonald et al. 2018). The mapping of evidence on this topic is thus highly important for ensuring that future research can address this gap and contribute to the theoretical development of youth specific help-seeking frameworks and models, which can then inform appropriate mental health care provision to facilitate youth engagement and participation in mental health care.
Aim and Scope of This Review
This scoping review aimed to collate and map the data from the available literature base on help-seeking, young people and mental health to answer the research question: how do informal sources of help affect young people’s access to, engagement with, and maintenance in professional mental health care? This review had two objectives: 1. To identify what is known about how informal relationships function in young people’s help-seeking pathways; 2. To examine what is known about the different roles that friends and family members play in help-seeking pathways.
Key Terms
This review uses the term “young people” to refer to people aged between 10 and 25 years. When referring to sources of help, the term “informal” refers specifically to a young person’s caregivers, family members and friends, as opposed to “formal” helpers who typically comprise of professionals providing mental health support or therapeutic interventions at a service. The term “mental health problem” is used throughout this review to refer to the range of personal distress and mental conditions that can affect an individual (Lynch et al. 2021).
Methodology
Review Design
As there is no review of any kind on the role of informal relationships in youth mental health help-seeking pathways, a scoping review approach was chosen as the most appropriate method to facilitate the systematic mapping of the literature on this topic (Munn et al. 2018). This scoping review was informed by guidance from the Joana Briggs Institute (JBI) Manual for Evidence Synthesis (Peters et al. 2020) which provides rigorous and transparent methods to identify how research was conducted, the types of evidence available, the identification of key characteristics and findings, and analysis of knowledge gaps to inform future research directions (Munn et al. 2022). In this section, a transparent account of searches, databases, and selection criteria are provided and include the provision of information on data extraction through a PRISMA diagram, quality appraisal, and data charting into appropriate tables for thematic synthesis and reporting of results.
Database Sources and Search Strategy
The first stage of this review involved a systematic search and retrieval of research from nine databases and included Psychinfo, Medline, ASSIA, CINAHL, Web of Science, Scopus, SAGE, Science Direct and Google Scholar (McFadden et al. 2012; Best et al. 2014; McGinn et al. 2016; Campbell et al. 2018). This procedure is provided in a PRISMA diagram (Fig. 1). For analytical searches, Boolean logic was used to establish search parameters and this procedure was adapted to suit each database search. The browsing method was used to manually search databases that did not have advanced search algorithms. After a pilot search, four key concept groupings were identified and included: (1) Young People (2) Help-seeking behaviour (3) Mental health and (4) Service Utilisation and is illustrated in Fig. 2. Deciding when to stop was guided by Kraft and Lee’s method (1979) which included (1) Satiation (2) Disgust and (3) Utility (Best et al. 2014).
Study Selection Criteria
Original research studies, excluding reviews, with empirical designs were included in this review and articles had to be published in a peer-reviewed journal between 1994 and 2021. This range was selected as it marks the beginning of the digital age and the widespread use of the internet (Cerf, 2009; Ono & Zavodny, 2002). Database searching took place in July 2021. All studies selected were English language only and contained direct reporting from young people on how informal sources of help affect young people’s access to, engagement with, and maintenance in professional mental health care services. Studies included young people aged between 10 and 25 years of age. Inclusion and exclusion criteria are detailed in Table 1. As this was a review, IRB approval and an informed consent statement were not applicable.
Initial database searching revealed that the vast majority of research on this topic, that met inclusion criteria, was being conducted in high income countries, with a noticeable absence of research from low-middle income countries. Pheko et al. (2013) and Mbuthia et al. (2018) attribute this disparity in part to the idea that help-seeking to a mental health professional for a personal problem is a Western cultural conceptualisation of mental health care. Considering that differing conceptualisations of mental health exist worldwide that can include traditional medicines and religion (Burlaka et al., 2014; Dogra et al., 2012; Mbuthia et al., 2018; Pheko et al., 2013) or that professional help-seeking for mental health can be taboo in some regions (Al-Krenawi et al. 2009; Bilican, 2013), it was decided to only review research from high-income countries with healthcare systems that share a common paradigm of formal mental healthcare provision.
Screening Process and Data Extraction
Database searching initially returned 2456 studies after the removal of 39 duplicates. After initial title and abstract screening, it was identified that there was no study that both researched this topic specifically and that met inclusion criteria. At this stage, 2129 records were excluded with 327 articles identified as potentially relevant for further screening (Fig. 1). The results or findings, discussion and conclusion sections of each study were read, to identify relevant data on the role of informal support in youth mental health help-seeking pathways. A further 295 records were excluded, and 32 studies met inclusion criteria (Table 1). Each study included in this review was recorded on a pre-formulated coding sheet according to their key study characteristics (Table 2). Cooper et al. (2021) states that there is a need for scoping reviews to include study appraisal tools to ensure quality, transparency, and reliability of findings. As this review included research with quantitative, qualitative, and mixed methods designs, two authors (L.L and A.M) independently appraised all included articles using the Mixed-Methods Assessment Tool (MMAT) (Hong et al. 2018). This tool uses five core quality criteria to support assessment and rather than determining quality using a single score, this approach recommends providing a description of the quality alongside quality ratings (Hong et al. 2018). For this review, studies were scored using a star system based on the five core quality criteria, 20% (*), 40% (**), 60% (***), 80% (****) or 100% (*****). In addition, this review also utilised the Scoping Review Checklist (SRC) by Cooper et al. (2021) to guide the reporting of the methodology used in this review. This review was self-appraised by the authors as meeting 19 out of 20 items on the SRC checklist, excluding stage 6.
Synthesis
As discussed, information on this topic was often reported as a secondary finding or obscured within the content of the article. Once relevant data on the topic of informal help was extracted from the findings, results, discussion or conclusion sections of articles, it was collated and thematically analysed using methodology by Braun & Clarke (2006). This data screening and extraction process included familiarisation with the data, coding for meaning and developing candidate themes. Themes were refined through further reading and analysis which supported the finalisation and naming of key themes.
Results
This section presents information on the results of this review and includes the key study characteristics, quality of evidence and the findings from the thematic analysis.
Study Characteristics
Study methodologies, participant information, location, year, sample size, settings of the studies selected for this review are summarised in this section and are detailed in Table 2.
Location and year
Selected research (n = 32) was published between 2005 and 2021. The most common country of research was Australia (n = 11) (Burns & Rapee, 2006; Gilchrist & Sullivan, 2006; Jorm et al. 2007; DeAnstiss & Ziaian, 2010; Hernan et al. 2010; Medlow et al. 2010; Yap et al. 2013; Lubman et al. 2017; Valibhoy et al. 2017; Maiuolo et al. 2019; Pearson & Hyde, 2021) followed by the United States of America (n = 6) (Draucker, 2005; Freedenthal & Stiffman, 2007; Ellis et al. 2010; Schmeelk‐Cone et al. 2012; Damian et al. 2018; Wang et al. 2020). The remaining studies included five from the United Kingdom (Fox & Butler, 2007; Quinn et al. 2009; Klineberg et al. 2011; Coleman-Fountain et al. 2020; Breslin et al. 2022), two from Turkey (Bilican 2013; Cakar & Savi, 2014), two from Sweden (Persson et al. 2017; Westberg et al. 2020) and single studies from New Zealand (Mariu et al. 2012); Portugal (Lourerio et al. 2013); Japan (Yamasaki et al. 2016); Norway (Moen and Hall-Lord 2019), Saudi Arabia (Mahsoon et al. 2020); and The Netherlands (Eigenhuis et al. 2021).
Methodologies
The most common methodology used was quantitative (n = 18) (Burns & Rapee, 2006; Freedenthal & Stiffman, 2007; Jorm et al. 2007; Hernan et al. 2010; Klineberg et al. 2011; Mariu et al. 2012; Schmeelk‐Cone et al. 2012; Bilican, 2013; Lourerio et al. 2013; Yap et al. 2013; Cakar & Savi, 2014; Yamasaki et al. 2016; Lubman et al. 2017; Maiuolo et al. 2019; Moen and Hall-Lord 2019; Mahsoon et al. 2020; Pearson & Hyde, 2021; Breslin et al. 2022). The rest included nine qualitative studies (Draucker, 2005; Gilchrist & Sullivan, 2006; DeAnstiss & Ziaian, 2010; Medlow et al. 2010; Valibhoy et al. 2017; Damian et al. 2018; Coleman-Fountain et al. 2020; Westberg et al. 2020; Eigenhuis et al. 2021) and five that used mixed methodologies (Fox & Butler, 2007; Quinn et al. 2009; Ellis et al. 2010; Persson et al. 2017; Wang et al. 2020). The quantitative research utilised surveys (n = 9) or questionnaires (n = 9) and the qualitative research employed either focus groups (n = 1) or interviews (n = 8). The mixed methodology research used focus groups or interviews with questionnaires or surveys (n = 4) with one study using interviews, focus groups and an interactive webspace.
Participants & sample size
Participants were aged between 10 and 25 years of age and studies were generally representative in terms of gender, with some studies having more female participants. While some studies included other research participants, such as parents or other adults, only data reported from young people that were presented separately were analysed and included in this review. Quantitative studies sample sizes ranged from 74 and 46,961 participants and qualitative studies had between 7 and 52 participants. In total, 91,020 participants took part in the included studies.
Study population
Studies focused on a range of research populations including young people who were in educational settings (n = 17) young people with actual help-seeking experience (n = 8), young people with refugee status (n = 3), young people who were recruited from the general population (n = 3), young people with autism (n = 1) and young people from Indigenous American communities (n = 1) (see Table 2).
Quality of Evidence
The quality appraisal of the studies included in this review were predominantly rated as four star (n = 16), followed by five star (n = 12). These articles had clear and appropriate study designs, with data and findings that were substantiated and coherent. Many quantitative studies did not provide information on the risk of nonresponse bias, and so were marked accordingly. Studies appraised as three star (n = 3) had additional issues with the reporting of data completeness, or a minor query over the representativeness of the sample. One article was rated as two star (n = 2), as the design had two sampling issues however, these were acknowledged by the author. In addition, sensitivity analysis indicated that the conclusions aligned well with the overall thematic synthesis and thus findings were included for regional and cultural perspective (Carroll et al. 2012). Overall, the studies included were predominantly high quality which in part might be explained by the intensive screening processes employed, which eliminated articles early on with questionable methodology (Hong et al. 2018). Although the studies in this review came from multiple disciplines and used various theoretical approaches to investigate this complex healthcare issue, the data was synthesised into clear and coherent themes.
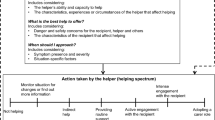
Thematic Analysis
A thematic analysis of the literature regarding how informal sources of help affect young people’s access to, engagement with, and maintenance in professional mental health care identified two key themes: 1. Informal helpers as supportive intermediaries and 2. Informal helpers as obstructive forces. These themes describe patterns from the data on how the behaviour of families and friends, as reported by young people, can support or obstruct their efforts to seek professional help for a mental health problem and are illustrated in Table 3.
Informal helpers as supportive intermediaries
The first theme describes how informal sources of help can support young people with their mental health and act as important facilitators to mental health services. The role of informal relationships is acknowledged by some research as an important factor in help-seeking for personal problems with it being proposed that professional help-seeking proceeds through stages, with informal help-seeking being a common and important first step after unsuccessful self-management (Gilchrist & Sullivan, 2006; Jorm et al. 2007; Yamasaki et al. 2016). Young people value and often prefer informal support with research finding that family and friends can offer comfort, a listening ear, guidance, or provide information about available resources for self-management (Draucker, 2005; Burns & Rapee, 2006; Freedenthal & Stiffman, 2007; Schmeelk‐Cone et al. 2012; Bilican, 2013; Cakar & Savi, 2014; Moen and Hall-Lord 2019; Mahsoon et al. 2020; Pearson & Hyde, 2021). Attending a formal service can cause a young person to feel discomfort, vulnerability, and a loss of autonomy whereas help-seeking to a pre-existing, easily accessed and trusting informal relationship can provide predictability and can cause less intrusion in their lives (Coleman-Fountain et al. 2020). When young people require a professional intervention, friends and family often initiate professional help-seeking by contacting services, assisting with transport and finance or through the provision of continued emotional support for the duration of their mental health care (Jorm et al. 2007; Ellis et al. 2010; Medlow et al. 2010; Loureiro et al. 2013; Lubman et al. 2017; Westberg et al. 2020; Eigenhuis et al. 2021). Through supportive experiences, young people can learn skills and build confidence to independently help-seek for mental health distress in the future when they need it (Draucker, 2005; Gilchrist & Sullivan, 2006; Medlow et al. 2010; Mariu et al. 2012; Schmeelk‐Cone et al. 2012; Yap et al. 2013b; Maiuolo et al. 2019; Eigenhuis et al. 2021).
Informal helpers as obstructive forces
The second theme describes how informal supports can create obstacles and exacerbate distress for young people seeking professional mental health care. Not all support offered within informal networks is helpful or sufficient, and research findings suggest that little is actually known about the effectiveness of informal support networks in helping young people resolve mental health problems (Draucker 2005; Gilchrist & Sullivan, 2006; Mariu et al. 2012; Bilican, 2013; Wang et al. 2020). Informal sources of help can have low mental health literacy, lack understanding, and are not always able to recognise when professional intervention is needed, sometimes stereotyping distress as a normal part of adolescence (Gilchrist & Sullivan, 2006; Fox & Butler, 2007; Quinn et al. 2009; Ellis et al. 2010; Lourerio et al. 2013; Bilican, 2013; Yap et al. 2013; Damian et al. 2018; Coleman-Fountain et al. 2020; Wang et al. 2020; Eigenhuis et al. 2021). Other research has shown that young people can conceal personal distress from their family and friends due to fears of stigma, rejection, confidence breaches or being misunderstood (Freedenthal & Stiffman, 2007; Fox & Butler, 2007; Quinn et al. 2009; De Anstiss & Ziaian, 2010; Yamasaki et al. 2016; Valibhoy et al. 2017; Wang et al. 2020). A lack of confidentiality from friends can exacerbate mental health problems and increase feelings of isolation and suspicion towards others (Draucker, 2005; Gilchrist & Sullivan, 2006). Problems can be further exacerbated when parents respond inappropriately to a young person’s distress, by either over-reacting and pressuring their child into treatment, minimising distress or opposing interventions completely (Draucker, 2005; Gilchrist & Sullivan, 2006; Persson et al. 2017; Mahsoon et al. 2020; Westberg et al. 2020). Family members, in an attempt to prevent family stigma as a result of having a child with a mental health problem, can obstruct professional help-seeking (Draucker 2005; Ellis et al. 2010). Research has also found that family support can be absent or limited as young people can experience a wide range of negative and traumatic life events related to their family circumstances including parental separation, bereavement, abandonment, asylum seeking, family violence, various types of abuse, parental mental illness, parental substance use and family criminal activities (Gilchrist & Sullivan, 2006; Draucker, 2005; De Anstiss & Ziaian, 2010; Damian et al. 2018). Findings also report that conflict in relationships is a major contributor to youth mental health problems and some young people can have limited or no prospects of familial support (Draucker, 2005; Fox and Butler 2007; Moen and Hall-Lord 2019; Mahsoon et al. 2020; Breslin et al. 2022).
Discussion
This aim of this scoping review was to map the available empirical evidence on how informal sources of help affect young people’s access to, engagement with, and maintenance in professional mental health care. This review has identified two key themes which were presented in a binary manner as ‘helpful’ or ‘unhelpful’ for the purpose of reporting and the organisation of data. However, the topic is complex and involves interpersonal dynamics, and therefore it is important to further discuss how informal relationships function in youth mental health help-seeking pathways and the different roles that family members and friends provide for young people seeking help for a mental health problem.
Informal Sources of Help as Important Pathway Agents
The first objective of this review was to identify what is known about how informal relationships function in young people’s mental health help-seeking pathways. For general life problems, help-seeking to family and friends during childhood is a normative part of daily life and involves problem-solving through ongoing, natural, and fluid interactions with individuals within a child’s community (Lindsay & Kalafat, 1998; Rickwood et al. 2005). Regarding problem-solving for mental health, research demonstrates that some young people can find satisfactory support within their informal networks, through listening, guidance and information (Draucker 2005; Freedenthal and Stiffman, 2007; Bilican, 2013). Research from Australia by Pearson & Hyde (2021) suggests that the preference to seek help from family and friends for a mental health problem might be due to barriers such as poor mental health literacy. However, other research would suggest that since young people have genuine fears about the unknown processes of mental health help-seeking with unfamiliar professionals in a service, this preference for help-seeking to family and friends might be due to the nature of informal relationships which often provide easy and immediate access to familiar, trusting, and predictable support (Lindsey & Kalafat, 1998; Freedenthal & Stiffman, 2007; Coleman-Fountain et al. 2020; Lynch et al. 2021). Furthermore, not all young people have access to professional services and so families and friends are often essential helpers for youth in rural communities (Hernan et al. 2010), youth experiencing marginalisation, or those who live in communities with differing conceptualisations of mental health living within a majority western culture (Freedenthal and Stiffman, 2007; De Anstiss & Ziaian, 2010; Ellis et al. 2010; Valibhoy et al. 2017). When young people are in a position to seek support from a formal service, informal supports play an essential role in providing resources and in assisting young people to access and stay engaged with services (Medlow et al. 2010; Valibhoy et al. 2017; Westberg et al. 2020; Eigenhuis et al. 2021).
Research has demonstrated that social relationships are vital to young people’s quality of life and that youth mental health problems are frequently connected to issues or conflict with family and friends (Gilchrist & Sullivan, 2006; Fox and Butler, 2007; Moen and Hall-Lord 2019; Westberg et al. 2020). An impossible situation can arise when a young person requires both a professional helper from outside of their social networks and the emotional, financial or logistical resources provided by friends and family to access and attend a mental health service. Fears related to discussing mental health problems with those causing or contributing to them, can result in no option but to not seek help (Fox and Butler, 2007). In addition, the personal and public costs of social rejection or exclusion which are risked upon disclosing mental health problems can have a strong influence on help-seeking decisions (Chan, 2013). A young person can avoid professional help-seeking if they fear being othered or stigmatised by their family or friends (Quinn et al, 2009; Medlow et al. 2010), if they perceive that help-seeking will not be supported by their social network (Schmeelk‐Cone et al. 2012), or if their problems contain highly stigmatised mental health conditions such as psychosis or alcohol abuse (Yap et al. 2013). Conversely, research has also demonstrated that when a young person holds a perception that they have no one to talk to, this can encourage professional help-seeking, assuming that there are no practical or financial barriers to overcome (Fox & Butler, 2007).
Mariu et al. (2012) and MacDonald et al. (2018) state that the role of informal sources of help in youth mental health help-seeking pathways is not well understood or acknowledged, which is perhaps due to the lack of explicit investigation on the topic. No research study was located that investigated the role of informal sources of help in youth mental health help-seeking pathways as a primary aim and the majority of evidence for this review emanated from secondary findings within broader youth mental health help-seeking research. Furthermore, youth mental health help-seeking can be approached from different theoretical viewpoints (Pearson & Hyde, 2021) and insight on this topic has been impacted by the lack of clarity or consistency in approach to how the topic is investigated (Table 2). This review found that research articles did not always provide clear information regarding the study’s theoretical underpinnings and that the role of informal supports was often assumed, implied or directly described as a barrier or a facilitator, depending on the viewpoint of the investigators. There is a need to move beyond categorical descriptors and Freedenthal and Stiffman (2007) argue for the reframing of informal sources of help as a legitimate option of help, as for some young people, they are “a constructive alternative, rather than a barrier” (p.72). Other studies promote viewing friends and family as the first point or stage of help in a professional help-seeking pathway (Quinn et al. 2009; Hernan et al. 2010; Yamasaki et al. 2016) while some studies describe informal roles as embedded within pathways and mediated by wider community and cultural factors (Damian et al. 2018; Moen and Hall-Lord 2019). Overall, this review found that young people have reported their family and friends as playing a central role in both their mental health and their professional help-seeking pathways (Burns & Rapee, 2006; Jorm et al. 2007; Bilican, 2013; Moen and Hall-Lord 2019). This important finding needs to be increasingly acknowledged and empirically researched to inform the development of youth help-seeking frameworks or models.
The Different Roles of Family and Friends
The second objective of this review was to examine what is known about the different roles that friends and family members play in help-seeking pathways and explore the important differences in these types of relationships.
The role of friends
This review found that in general young people’s preference for support gradually changes from family to friends across the life-stage of youth (Burns & Rapee, 2006; Medlow et al. 2010; Klineberg et al. 2011; Lubman et al. 2017; Yamasaki et al. 2016; Maiuolo et al. 2019) (See Fig. 3). Youth is an important time for acquiring knowledge and skills for adulthood (Laurerio et al. 2013), and young people do not always rate adults as having the necessary skills to help them solve age-related problems (Gilchrist & Sullivan, 2006; De Anstiss & Ziaian, 2010; Maiuolo et al. 2019). Findings indicate that friends can increase in importance as they might provide more trustworthy and understanding spaces in which young people can learn to solve common age-related problems away from adults who could react negatively, especially if concerns are related to taboo topics such as sex and drugs (Fox & Butler, 2007; Freedenthal & Stiffman, 2007). Young people also report that friends are important for initiating help-seeking, locating or signposting a peer to help, especially when suicidal (Schmeelk‐Cone et al. 2012). For young people who have experienced asylum seeking, research from America and Australia report that peer groups are critical for both support with mental health problems and for connecting with professional services (De Anstiss & Ziaian, 2010; Ellis et al. 2010).
Other research suggests that befriending peers with similar psychological problems can have drawbacks, especially when they encourage destructive self-management behaviours or due to their own negative experiences and attitudes, discourage professional help-seeking (Freedenthal & Stiffman, 2007; De Anstiss & Ziaian, 2010; Bilican, 2013; Eigenhuis et al. 2021). Further to this, when mental health problems are pervasive within peer groups, behaviours such as substance use, eating problems and suicidal talk, which an adult might view as problematic, can be normalised conversations and behaviours for young people (Draucker, 2005; Mariu et al. 2012). It is important to note that the preference for friends does not mean that young people will necessarily seek help from peers, as some research reports that they can be perceived as unreliable, untrustworthy, lack resources, lack understanding and empathy (Gilchrist & Sullivan, 2006; Fox and Butler, 2007; De Anstiss & Ziaian, 2010; Laureiro et al. 2013). Young people experiencing severe psychological problems can avoid confiding in friends out of fear of ridicule, threats to self-esteem, or doubts over friends’ ability to maintain confidentiality (Gilchrist & Sullivan, 2006; Quinn et al. 2009; Yap et al. 2013). Furthermore, friends and peers can be the source of mental health problems due to social rejection, conflict or bullying (Draucker, 2005; Gilchrist & Sullivan, 2006; Fox & Butler, 2007; Quinn et al. 2009). There is also evidence to suggest a gender disparity across the early and mid-adolescent years where girls can become increasingly socialised to use friends as a source of help and gradually reduce dependence on their parents and family, and boys appearing to be socialised to help-seek less from all sources of help (Pearson & Hyde, 2021).
The role of families
A young person’s family is an important source of help and can provide important resources and practical skills for help-seeking including locating and contacting services, providing transport to appointments, advocating and covering financial costs (Draucker, 2005; Burns & Rapee, 2006; Medlow et al. 2010; Lubman et al. 2017; Persson et al. 2017; Maiuolo et al. 2019; Coleman-Fontaine et al. 2020; Eigenhuis et al. 2021). Family member’s proximity can result in them first noticing that a young person is having difficulties, which can increase opportunities for suggesting problem-solving strategies or facilitating earlier interventions in mental health care (Maiuolo et al. 2019; Moen and Hall-Lord 2019). Whilst investigating factors facilitating young people into the Australian mental health care system, Medlow et al. (2010) found that families have the ability to offer “out of hours” support to young people during difficult periods involving suicidal risk or psychosis. When caregivers demonstrate psychological availability and structure a young person’s decision making by supporting autonomy and encouraging help-seeking, young people can learn important skills and are more likely to independently seek help in the future (Yap et al. 2013; Maiuolo et al. 2019). Findings from a large-scale national survey in Norway (Moen and Hall-Lord 2019) indicate that young people with high distress experience more conflict with caregivers and are less likely to seek help from those in their social network. Similar findings from Northern Ireland (Breslin et al. 2022) report that having a supportive family life was both significantly related to fewer mental health problems and that young people were more likely to seek help from their families for emotional distress. This scoping review found important data indicating that a high-quality caregiver-child relationship can be an important mediating factor in help-seeking, engagement with and maintenance in mental health care, not a barrier (Draucker 2005; Moen and Hall-Lord 2019; Maiuolo et al. 2019).
While young people can be supported by families practically and financially, the necessary and parallel emotional support is not always present (Damian et al. 2018). Some young people have reported that caregivers exacerbated a difficult time despite their best intentions to provide support, or that caregivers were not always approachable or equipped to deal with and recognise young people’s problems (Gilchrist & Sullivan, 2006; Lourerio et al. 2013; Wang et al. 2020; Eigenhuis et al. 2021). Due to expressional styles, communication issues and stereotyped expectations of development, research describes how caregivers can miss distress or underestimate their child’s problem, for example, when children internalise distress, parents can view this as ‘good’ behaviour or attribute externalising symptoms and signs of emotional distress to ‘normal’ adolescent behaviour (Gilchrist & Sullivan, 2006; Ellis et al., 2010; Lourerio et al. 2013; Damian et al. 2018). Combined with intergenerational divides, differing values and behavioural norms, young people can choose to seek help outside their family unit or not at all if there are too many barriers for independent help-seeking (Draucker, 2005; Fox & Butler, 2007; Yap et al. 2013; Maiuolo et al. 2019). Some young people have reported how parents can resist or be suspicious of requests for external support (Medlow et al. 2010; Wang et al. 2020). This is pertinent to young people under eighteen years of age, who are in a unique legal position of dependence on family for most aspects of their life, including access and consent to attend health services in some jurisdictions. Some young people have reported that caregivers became over-involved in their treatment or exerted pressure on them to attend a professional service, which interfered with autonomy and the development of a trusting therapeutic rapport, causing earlier health care exits and poorer outcomes (Gilchrist & Sullivan, 2006; Persson et al. 2017; Mahsoon et al. 2020). In-depth qualitative research with mental health service users by Draucker (2005) reported how young people can withhold information, conceal information or distress from therapists and parents, or pretend to be better in order manage involuntary attendance. This study also described how the impact of parental under-involvement contributed to earlier exits from services, and how dismissive attitudes towards healthcare could result in a lack of supervision or support in helping their child’s take medication as prescribed (Draucker 2005).
Not all young people view help-seeking outside of the family environment as appropriate or desirable (Valibhoy et al. 2017). Some studies found that young people can fear disapproval, embarrassment or punishment for going outside their family or from the invalidation that can be felt from having their family members trivialise or dismiss their problems (Yap et al. 2013b; Gilchrist & Sullivan, 2006; Fox & Butler, 2007; Valibhoy et al. 2017; Wang et al. 2020). Young people with asylum seeking experiences and living in Western countries, reported that discussing personal problems with a parent can disrupt the traditional family hierarchy and boundaries of the parent-child relationship (Ellis et al. 2010; DeAnstiss & Ziaian, 2010; Valibhoy et al. 2017). Young people reported not wanting to ask for help from parents who were recovering from traumatic experiences or who were too distressed to provide supportive or consistent parenting (Ellis et al. 2010; DeAnstiss & Ziaian, 2010). These findings might be analogous to young people who have parents with their own mental health concerns, trauma, financial difficulties, and other life problems (Gilchrist & Sullivan, 2006; Damian et al. 2018). Not all young people have supportive family backgrounds (Medlow et al. 2010) which can be due to bereavement, abandonment, abuse, or chaotic home environments and can disproportionately affect those in alternative care provision or who experience homelessness outside of their families (Draucker 2005; Damian et al. 2018). While research by Mariu et al. (2012) has found that coming from a family with high levels of economic stressors can increase the likelihood of service utilisation, Damian et al. (2018), who investigated improving services for youth with polytrauma, discussed how families can normalise trauma and accept distress, which can negatively impact their ability to view psychological problems as addressable or preventable.
Summary
Informal sources of support can be difficult to research or evaluate as the topic involves exploring patterns of nuanced interactions that happen in varying domestic and social contexts over time (Lindsey & Kalafat, 1998). How friends and families respond to a young person’s distress will vary depending on rapport, mental health literacy and cultural factors. The literature indicates that high quality relationships and caregiver psychological availability were found to be strongly linked with increased professional help-seeking, while conflict in relationships, family acceptance of distress and stigma were connected with the decreased likelihood of help-seeking (see Table 4). Importantly, some factors such as adequate social support, low or no social support, suicidal ideation or family and friends as the source of problems, were linked with both discouraging or encouraging help-seeking, depending on the young person’s situation. When informal supports can provide resources and model the skills needed for help-seeking, the likelihood of a young person seeking professional help will increase and young people without helpful informal supports can have delayed help-seeking or complete help-negation. This review demonstrates that young people seek help through relationships and that the role of informal sources of support is a pivotal component in professional help-seeking pathways, but that friends and family members can have different approaches and roles which can impact a young person’s overall participation in mental health care.
Limitations
This review has five limitations. Firstly, there was no research available that met both the inclusion criteria and that exclusively examined the role that informal sources of help have in relation to young people’s mental health help-seeking pathways and thus data on the topic were extracted from studies which had broader research aims around young people’s help-seeking behaviour. Secondly, much of the quantitative research reported findings from data collected from instruments that measured intentions to seek help as opposed to investigating actual experiences. The use of vignette characters in hypothetical situations was common, and while helpful for looking at broader patterns of attitudes has important limitations. Intentions to seek help are not the same as actual help-seeking behaviour, and thus any associations found between intentions and help-seeking need to be considered with caution (Hughes & Huby, 2004; Eisenberg et al. 2012). Qualitative research addressed this gap to some extent by exploring actual experiences and important dynamics, but also had limitations related to cultural factors, socio-economic status or age-group. Thirdly, grey literature and studies with unclear methodologies or the inclusion of people over 26 years of age were excluded which might have contained findings that provided further insight on the topic. This review included studies with young people who volunteered to participate in research and thus the experiences of young people who do not participate are not known. Fourthly, some studies did not define between different types of informal relationships when presenting findings, specifically, the grouping of data under the one heading ‘friends and family’ affected this review’s ability to distinguish further the specific roles and their impact in help-seeking. Finally, all studies included in this review were in the English language and from high-income countries which provides a limited understanding of the topic from a global perspective. While high-income countries are connected through a common conceptualisation of mental health and healthcare, they are not homogenous and culturally specific research is required.
Implications and Recommendations for Further Research, Practice and Policy
Research
As there was no study identified that researched this topic directly, the first recommendation would be to rectify this gap. In particular, further insight is needed into the cultural context of the family, the wider context of a young person’s social networks and the roles that individual family members play, including siblings and extended relatives. Additionally, future research can inquire about the specific preferences of social support across the age range 10–25 years, which might be connected to developmental needs, intergenerational disconnect or relationship quality. The preference for parental support is usually associated with younger children but some research with older adolescents has reported that family are an important source of help and provide essential resources. The levels of involvement and the specific types of support required among young people in later adolescence and emerging adulthood is still not well-known and requires further investigation (Draucker 2005; Rickwood et al. 2005; Burns & Rapee, 2006; Jorm et al. 2007; Medlow et al. 2010; Yap et al. 2013; Yamasaki et al. 2016). It is also critical that research actively includes young people who experience marginalisation and who have low or no social support, as well as those from different cultural or ethnic backgrounds. There were no studies that met selection criteria for this review for young people in the LGBTI + community, and so it is important that young people identifying as LGBTI + are included in research as suicide ideation is high in this community (Higgins et al., 2016). This review focused on data from high-income countries as there is limited research from the Global South (Odeh, 2010) on this topic. It is important to address this gap appropriately to further understanding of youth mental health from a global context and to ensure research from low to middle income countries is included in youth mental health discussions. Finally, for appropriate design of services and evidence-based interventions in youth mental health care, it is important that research is conducted with young people who have actual help-seeking experiences.
Practice and policy
As this is a scoping review, recommendations for practice and policy can be limited (Munn et al. 2018) however, as this is a critically under researched field, it is important to discuss patterns from the findings that can provide guidance for services on how to support young people to mental health care. For therapeutic purposes, practitioners can inquire about a young person’s social relationships and how they support or exacerbate their mental health problems. Understanding how young people relate in their social relationships can help set expectations, tailor support, and provide understanding around their ability to build rapport and engage in treatment, all of which can contribute to trauma informed care. Social inclusion is essential for young people’s development and wellbeing, and practitioners can consider how to support young people with navigating relationship conflict and in building positive and supportive connections. Practitioners supporting young people with more severe mental health problems need to consider how to help them manage social fears of stigma and rejection on an individual basis.
Young people are often dependent on others for transport, finance and time management skills to attend an appointment. Supporting caregiver planning around family needs and responsibilities, childcare and educational commitments is crucial to maintain young people in mental health care. When social support is low or absent, services need to be responsive, providing flexible policies and opening hours, out-reach, evaluation, suitable interventions, and appropriately youth trained staff (Lynch et al. 2021). When young people’s families are the source of their mental health problems or are not able to provide any support with mental health care, the role of the helper becomes paramount for providing much-needed comfort, guidance and skills to improve their life situations and well-being (Moen and Hall-Lord 2019). Before referring young people in low social support situations to other agencies, referrers must consider the suitability of the services and what additional support can be garnered from local community embedded organisations, such as youth workers, who can advocate and assist with some practical barriers as well as provide ongoing support (Rickwood et al. 2005).
Whether working cross-culturally or within-culturally, practitioners can ensure that they are providing tailored, relevant, and appropriate mental health care. Practitioners need to be competent in working with and understanding differing conceptualisations of mental health across and within high-income regions and countries. This is very important when working with young people who have experienced asylum seeking, have refugee status or are part of a minority community living within a majority Western culture and have differing conceptualisations of mental health (De Anstiss & Ziaian, 2010; Ellis et al. 2010).
Finally, practitioners need to inquire about young people’s participation, whether they are being encouraged or are being coerced into treatment by others. Establishing respectful boundaries with young people and prioritising confidentiality and privacy is very important and can support participation. Voluntary participation is crucial for a young person’s wellbeing and for respecting and nurturing their developing autonomy. Involuntary participation does not contribute towards a trusting rapport or successful treatment outcomes (Persson et al. 2017).
Conclusion
After unsuccessful self-management, it is through friends and family members that young people begin the process of looking for suitable help for their personal distress, and this scoping review has demonstrated that these informal relationships play a pivotal role in young people’s access to, engagement with, and maintenance in professional mental health care. This article has also helped elucidate how informal sources of support act as intrinsic pathway agents and has provided a summary of what is known about how these relationships can either encourage or discourage young people from help-seeking to professional services. Through an improved understanding of how these interpersonal relationships function within a young person’s help-seeking process, on a spectrum of supportive to obstructive behaviour, services and practitioners can ensure the provision of responsive and appropriate support to young people and their families, facilitating service use and ensuring better outcomes for young people’s mental health and quality of life.
References
Al-Krenawi, A., Graham, J. R., Al-Bedah, E. A., Kadri, H. M., & Sehwail, M. A. (2009). Cross-national comparison of Middle Eastern university students: Help-seeking behaviors, attitudes toward helping professionals, and cultural beliefs about mental health problems. Community mental health journal, 45(1), 26.
De Anstiss, H., & Ziaian, T. (2010). Mental health help-seeking and refugee adolescents: Qualitative findings from a mixed-methods investigation. Australian Psychologist, 45(1), 29–37.
De Anstiss, H., Ziaian, T., Procter, N., Warland, J., & Baghurst, P. (2009). Help-seeking for mental health problems in young refugees: A review of the literature with implications for policy, practice, and research. Transcultural Psychiatry, 46(4), 584–607.
Arnett, J. J. (2014). Emerging Adulthood: The Winding Road from the Late Teens Through the Twenties, Second Edition. Oxford University Press.
Best, O., & Ban, S. (2021). Adolescence: physical changes and neurological development. British Journal of Nursing, 30(5), 272–275.
Best, P., Taylor, B., Manktelow, R., & McQuilkin, J. (2014). Systematically retrieving research in the digital age: Case study on the topic of social networking sites and young people’s mental health. Journal of Information Science, 40(3), 346–356.
Biddle, L., Donovan, J., Sharp, D., & Gunnell, D. (2007). Explaining non-help-seeking amongst young adults with mental distress: a dynamic interpretive model of illness behaviour. Sociology of Health & Illness, 29(7), 983–1002.
Bilican, F. I. (2013). Help-seeking attitudes and behaviors regarding mental health among Turkish college students. International Journal of Mental Health, 42(2-3), 43–59.
Bilsen, J. (2018). Suicide and youth: risk factors. Frontiers in psychiatry, 9, 540.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Breslin, G., Shannon, S., Prentice, G., Rosato, M., & Leavey, G. (2022). Adolescent mental health help-seeking from family and doctors: applying the theory of planned behaviour to the Northern Ireland schools and wellbeing study. Child Care in Practice, 28(4), 522–535.
Burlaka, V., Churakova, I., Aavik, O. A., Staller, K. M., & Delva, J. (2014). Attitudes toward health-seeking behaviors of college students in Ukraine. International Journal of Mental Health and Addiction, 12(5), 549–560.
Burns, J. R., & Rapee, R. M. (2006). Adolescent mental health literacy: young people’s knowledge of depression and help seeking. Journal of Adolescence, 29(2), 225–239.
Cakar, F. S., & Savi, S. (2014). An Exploratory Study of Adolescent’s Help-Seeking Sources. Procedia-Social and Behavioral Sciences, 159, 610–614.
Campbell, A., Taylor, B. J., Bates, J., & O’Connor-Bones, U. (2018). Developing and applying a protocol for a systematic review in the social sciences. New Review of Academic Librarianship, 24(1), 1–22.
Carroll, C., Booth, A., & Lloyd-Jones, M. (2012). Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qualitative Health Research, 22(10), 1425–1434.
Cerf, V. G. (2009). The day the Internet age began. Nature, 461(7268), 1202–1203.
Chan, M. E. (2013). Antecedents of instrumental interpersonal help-seeking: An integrative review. Applied Psychology, 62(4), 571–59.
Charman, D., Harms, C., & Myles-Pallister, J. (2010). Help and e-help: Young people’s perspectives of mental healthcare. Australian Family Physician, 39(9), 663.
Coleman-Fountain, E., Buckley, C., & Beresford, B. (2020). Improving mental health in autistic young adults: a qualitative study exploring help-seeking barriers in UK primary care. British Journal of General Practice, 70(694), e356–e363.
Collins, P., & Barker, C. (2009). Psychological help-seeking in homeless adolescents. International Journal of Social Psychiatry, 55(4), 372–384.
Cooper, S., Cant, R., Kelly, M., Levett-Jones, T., McKenna, L., Seaton, P., & Bogossian, F. (2021). An evidence-based checklist for improving scoping review quality. Clinical Nursing Research, 30(3), 230–240.
Cornally, N., & McCarthy, G. (2011). Help-seeking behaviour: A concept analysis. International Journal of Nursing Practice, 17(3), 280–288.
Damian, A. J., Gallo, J. J., & Mendelson, T. (2018). Barriers and facilitators for access to mental health services by traumatized youth. Children and Youth Services Review, 85, 273–278.
Dogra, N., Omigbodun, O., Adedokun, T., Bella, T., Ronzoni, P., & Adesokan, A. (2012). Nigerian secondary school children’s knowledge of and attitudes to mental health and illness. Clinical child psychology and psychiatry, 17(3), 336–353.
Draucker, C. B. (2005). Processes of mental health service use by adolescents with depression. Journal of Nursing Scholarship, 37(2), 155–162.
Eigenhuis, E., Waumans, R. C., Muntingh, A. D., Westerman, M. J., van Meijel, M., Batelaan, N. M., & van Balkom, A. J. (2021). Facilitating factors and barriers in help-seeking behaviour in adolescents and young adults with depressive symptoms: A qualitative study. PloS ONE, 16(3), e0247516.
Eisenberg, D., Hunt, J., & Speer, N. (2012). Help seeking for mental health on college campuses: Review of evidence and next steps for research and practice. Harvard Review of Psychiatry, 20(4), 222–232.
Ellis, B. H., Lincoln, A. K., Charney, M. E., Ford-Paz, R., Benson, M., & Strunin, L. (2010). Mental health service utilization of Somali adolescents: religion, community, and school as gateways to healing. Transcultural Psychiatry, 47(5), 789–811.
Finkelhor, D., Shattuck, A., Turner, H., & Hamby, S. (2015). A revised inventory of adverse childhood experiences. Child Abuse & Neglect, 48, 13–21.
Fox, C. L., & Butler, I. (2007). ‘If you don’t want to tell anyone else you can tell her’: Young people’s views on school counselling. British Journal of Guidance & Counselling, 35(1), 97–114.
Freedenthal, S., & Stiffman, A. R. (2007). Suicidal behavior in urban American Indian adolescents: A comparison with reservation youth in a southwestern state. Suicide and Life-Threatening Behavior, 34(2), 160–171.
Gilchrist, H., & Sullivan, G. (2006). Barriers to help-seeking in young people: Community beliefs about youth suicide. Australian Social Work, 59(1), 73–85.
Goodwin, J., Savage, E., & Horgan, A. (2016). Adolescents’ and young Adults’ beliefs about mental health services and care: a systematic review. Archives of Psychiatric Nursing, 30(5), 636–644.
Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), 113.
Hernan, A., Philpot, B., Edmonds, A., & Reddy, P. (2010). Healthy minds for country youth: Help-seeking for depression among rural adolescents. Australian Journal of Rural Health, 18, 118–124.
Higgins, A., Doyle, L., Downes, C., Murphy, R., Sharek, D., DeVries, J., Begely, T., Sheerin, F., Smyth, S. and McCann, E., (2016). The LGBT Ireland Report: National study of the mental health and wellbeing of lesbian, gay, bisexual, transgender and intersex people in Ireland. Trinity College Dublin.
Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., & Pluye, P. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291.
Hughes, R., & Huby, M. (2004). The construction and interpretation of vignettes in social research. Social Work and Social Sciences Review, 11(1), 36–51.
Jorm, A. F., Wright, A., & Morgan, A. J. (2007). Where to seek help for a mental disorder? Medical Journal of Australia, 187(10), 556–560.
Kelly, C. M., Mithen, J. M., Fischer, J. A., Kitchener, B. A., Jorm, A. F., Lowe, A., & Scanlan, C. (2011). Youth mental health first aid: a description of the program and an initial evaluation. International Journal of Mental Health Systems, 5(1), 1–9.
Kessler, R. C., Angermeyer, M., Anthony, J. C., De Graaf, R. O. N., Demyttenaere, K., Gasquet, I., & Kawakami, N. (2007). Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6(3), 168.
Klineberg, E., Biddle, L., Donovan, J., & Gunnell, D. (2011). Symptom recognition and help seeking for depression in young adults: a vignette study. Social Psychiatry and Psychiatric Epidemiology, 46(6), 495–505.
Kraft, D. H., & Lee, T. (1979). Stopping rules and their effect of expected search length. Information Processing and Management, 15(1), 47–58.
Leavey, G., Rothi, D., & Paul, R. (2011). Trust, autonomy and relationships: the help-seeking preferences of young people in secondary level schools in London (UK). Journal of Adolescence, 34(4), 685–693.
Lindsey, C. R., & Kalafat, J. (1998). Adolescents’ views of preferred helper characteristics and barriers to seeking help from school-based adults. Journal of Educational and Psychological Consultation, 9(3), 171–193.
Loureiro, L. M., Jorm, A. F., Mendes, A. C., Santos, J. C., Ferreira, R. O., & Pedreiro, A. T. (2013). Mental health literacy about depression: a survey of portuguese youth. BMC Psychiatry, 13(1), 1–8.
Lubman, D. I., Cheetham, A., Berridge, B. J., & McKay-Brown, L. (2017). MAKINGtheLINK: a school-based intervention to improve helpseeking for substance use problems. Early Intervention in Psychiatry, 12(5), 915–921.
Lynch, L., Moorhead, A., Long, M., & Hawthorne-Steele, I. (2021). What type of helping relationship do young people need? Engaging and maintaining young people in mental health care—A narrative review. Youth & Society, 53(8), 1376–1399.
MacDonald, K., Fainman-Adelman, N., Anderson, K. K., & Iyer, S. N. (2018). Pathways to mental health services for young people: a systematic review. Social Psychiatry and Psychiatric Epidemiology, 53(10), 1005–1038.
Mahsoon, A., Sharif, L., Banakhar, M., Alasmee, N., Almowallad, E., Jabali, R., & Assur, S. (2020). Parental support, beliefs about mental illness, and mental help-seeking among young adults in Saudi Arabia. International Journal of Environmental Research and Public Health, 17(15), 5615.
Maiuolo, M., Deane, F. P., & Ciarrochi, J. (2019). Parental authoritativeness, social support and help-seeking for mental health problems in adolescents. Journal of Youth and Adolescence, 48(6), 1056–1067.
Mariu, K. R., Merry, S. N., Robinson, E. M., & Watson, P. D. (2012). Seeking professional help for mental health problems, among New Zealand secondary school students. Clinical Child Psychology and Psychiatry, 17(2), 284–297.
Mbuthia, J. W., Kumar, M., Falkenström, F., Kuria, M. W., & Othieno, C. J. (2018). Attributions and private theories of mental illness among young adults seeking psychiatric treatment in Nairobi: an interpretive phenomenological analysis. Child and Adolescent Psychiatry and Mental Health, 12(1), 28.
McFadden, P., Taylor, B. J., Campbell, A., & McQuilkin, J. (2012). Systematically identifying relevant research: Case study on child protection social workers’ resilience. Research on Social Work Practice, 22(6), 626–636.
McGinn, A. H., Taylor, B. J., McColgan, M., & McQuilkin, J. (2016). Social work literature searching: Current issues with databases and online search engines. Research on Social Work Practice, 26(3), 266–277.
Medlow, S., Kelk, N., Cohen, A., & Hickie, I. (2010). Facilitating early intervention: experiences of young people and implications for the shaping of headspace services. Australasian Psychiatry, 18(4), 335–339.
Michelmore, L., & Hindley, P. (2012). Help-seeking for suicidal thoughts and self-harm in young people: A systematic review. Suicide and Life-Threatening Behavior, 42(5), 507–524.
Moen, Ø. L., & Hall-Lord, M. L. (2019). Adolescents’ mental health, help seeking and service use and parents’ perception of family functioning. Nordic Journal of Nursing Research, 39(1), 1–8.
Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 1–7.
Munn, Z., Pollock, D., Khalil, H., Alexander, L., Mclnerney, P., Godfrey, C. M., & Tricco, A. C. (2022). What are scoping reviews? Providing a formal definition of scoping reviews as a type of evidence synthesis. JBI Evidence. Synthesis, 20(4), 950–952.
Nam, S. K., Chu, H. J., Lee, M. K., Lee, J. H., Kim, N., & Lee, S. M. (2010). A meta-analysis of gender differences in attitudes toward seeking professional psychological help. Journal of American College Health, 59, 110–116.
Odeh, L. E. (2010). A comparative analysis of global north and global south economies. Journal of Sustainable Development in Africa, 12(3), 338–348.
Ono, H., & Zavodny, M. (2002). Race, Internet usage, and e-commerce. The Review of Black Political Economy, 30(3), 7–22.
Patel, V., Flisher, A. J., Hetrick, S., & McGorry, P. (2007). Mental health of young people: a global public-health challenge. The Lancet, 369(9569), 1302–1313.
Pearson, S., & Hyde, C. (2021). Influences on adolescent help-seeking for mental health problems. Journal of Psychologists and Counsellors in Schools, 31(1), 110–121.
Persson, S., Hagquist, C., & Michelson, D. (2017). Young voices in mental health care: Exploring children’s and adolescents’ service experiences and preferences. Clinical Child Psychology and Psychiatry, 22(1), 140–151.
Peters, M. D., Godfrey, C., McInerney, P., Munn, Z., Tricco, A. C., & Khalil, H. (2020). Chapter 11: scoping reviews (2020 version). In Aromataris, E. Munn, Z. (Eds.), JBI Manual for Evidence Synthesis, JBI, 2020. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-12.
Pheko, M. M., Chilisa, R., Balogun, S. K., & Kgathi, C. (2013). Predicting intentions to seek psychological help among Botswana university students: The role of stigma and help-seeking attitudes. Sage Open, 3(3), 2158244013494655.
Pompili, M. (2018). The increase of suicide rates: the need for a paradigm shift. The Lancet, 392(10146), 474–475.
Pumpa, M., & Martin, G. (2015). The impact of attitudes as a mediator between sense of autonomy and help-seeking intentions for self-injury. Child and Adolescent Psychiatry and Mental Health, 9(1), 1–9.
Quinn, N., Wilson, A., MacIntyre, G., & Tinklin, T. (2009). ‘People look at you differently’: students’ experience of mental health support within Higher Education. British Journal of Guidance & Counselling, 37(4), 405–418.
Radez, J., Reardon, T., Creswell, C., Lawrence, P. J., Evdoka-Burton, G., & Waite, P. (2021). Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. European Child & Adolescent Psychiatry, 30(2), 183–211.
Rickwood, D., Deane, F. P., & Wilson, C. J. (2007). When and how do young people seek professional help for mental health problems? Medical Journal of Australia, 187, S35–S39.
Rickwood, D., Deane, F. P., Wilson, C. J., & Ciarrochi, J. (2005). Young people’s help-seeking for mental health problems. Australian e-journal for the Advancement of Mental Health, 4(3), 218–251.
Rickwood, D., Paraskakis, M., Quin, D., Hobbs, N., Ryall, V., Trethowan, J., & McGorry, P. (2019). Australia’s innovation in youth mental health care: the headspace centre model. Early Intervention in Psychiatry, 13(1), 159–166.
Rothì, D. M., & Leavey, G. (2006). Mental health help-seeking and young people: A review. Pastoral Care in Education, 24(3), 4–13.
Rowe, S. L., French, R. S., Henderson, C., Ougrin, D., Slade, M., & Moran, P. (2014). Help-seeking behaviour and adolescent self-harm: a systematic review. Australian & New Zealand Journal of Psychiatry, 48(12), 1083–1095.
Ryan, S. M., Toumbourou, J. W., & Jorm, A. F. (2014). Factors associated with service use for young adolescents with mental health problems: findings from an Australian longitudinal study. SAGE Open, 4(4), 2158244014556286.
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D., & Patton, G. C. (2018). The age of adolescence. The Lancet Child & Adolescent Health, 2(3), 223–228.
Schmeelk-Cone, K., Pisani, A. R., Petrova, M., & Wyman, P. A. (2012). Three scales assessing high school students’ attitudes and perceived norms about seeking adult help for distress and suicide concerns. Suicide and Life-Threatening Behavior, 42(2), 157–172.
UNESCO, (2010). Youth. Viewed 6th September 2021, https://en.unesco.org/youth.
Valibhoy, M. C., Szwarc, J., & Kaplan, I. (2017). Young service users from refugee backgrounds: their perspectives on barriers to accessing Australian mental health services. International Journal of Human Rights in Healthcare, 10(1), 68–80.
Wang, C., Barlis, J., Do, K. A., Chen, J., & Alami, S. (2020). Barriers to mental health help seeking at School for Asian–and Latinx–American adolescents. School Mental Health, 12(1), 182–194.
Westberg, K. H., Nygren, J. M., Nyholm, M., Carlsson, M., & Svedberg, P. (2020). Lost in space-an exploration of help-seeking among young people with mental health problems: a constructivist grounded theory study. Archives of Public Health, 78(1), 1–11.
Wilson, C. J., & Deane, F. P. (2012). Brief report: Need for autonomy and other perceived barriers relating to adolescents’ intentions to seek professional mental health care. Journal of Adolescence, 35(1), 233–237.
World Health Organisation. (2021). Adolescent mental health. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
Yamasaki, S., Ando, S., Shimodera, S., Endo, K., Okazaki, Y., Asukai, N., & Sasaki, T. (2016). The Recognition of Mental Illness, Schizophrenia Identification, and Help-Seeking from Friends in Late Adolescence. PloS ONE, 11(3), e0151298.
Yap, M. B. H., Reavley, N., & Jorm, A. F. (2013). Where would young people seek help for mental disorders and what stops them? Findings from an Australian national survey. Journal of Affective Disorders, 147(1–3), 255–261.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lynch, L., Moorhead, A., Long, M. et al. The Role of Informal Sources of Help In Young People’s Access To, Engagement With, And Maintenance In Professional Mental Health Care—A Scoping Review. J Child Fam Stud 32, 3350–3365 (2023). https://doi.org/10.1007/s10826-022-02498-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-022-02498-5