Abstract
Purpose
To evaluate patient satisfaction using telehealth for fertility care.
Methods
Cross-sectional survey using the validated telehealth usability questionnaire (TUQ) distributed nationally via fertility advocacy groups of fertility patients aged ≥ 18 years with self-reported use of telehealth for care. Patient satisfaction of telehealth for fertility care as determined by the TUQ questionnaire. The survey also included questions about telehealth related to usefulness, ease of use, effectiveness, reliability, and the option for patients to add open-ended comments related to their experiences using telehealth for fertility care.
Results
A total of 81 fertility patients completed the survey. Patients reported high rates of satisfaction (81.4%) with telehealth in areas of usefulness, ease of use, effectiveness, reliability, and satisfaction. However, many patients (60.5%) expressed a preference for in-person visits for their initial visit while the acceptability of telehealth increased for follow-up visits. Negative themes from respondent comments address that telehealth visits felt more impersonal and rushed.
Conclusion
Fertility patients reported high satisfaction using telehealth for care. Patients still preferred in-person visits for initial consultations. For follow-up visits, most respondents favored telehealth or had no preference. Incorporation of telehealth in fertility practices should continue though it may be helpful for patients to be given options for visit types.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic changed the landscape of healthcare delivery. Prior to the pandemic, telehealth had been trialed in a variety of healthcare fields but its practical, widespread use was limited due to reimbursement, regulation, and technology barriers along with lower patient and clinician acceptance [1]. Research conducted during the pandemic shows acceptance of telehealth has increased among patients [2-5]. Telehealth use across all outpatient healthcare visits has stabilized to 17% from its peak of 32% in April 2020 [6]. It is clear that telehealth is here to stay and is an important part of our field’s future [7, 8]. But data on its ideal use for fertility care is just starting to accumulate.
Since the pandemic, specialties such as obstetrics and rehabilitation medicine have integrated telehealth with overall positive patient experiences [9, 10]. But seeking care for infertility is a uniquely personal journey, and understanding this specific patient population’s attitudes toward telehealth is critical. One key aspect is understanding the effect of telehealth on patient satisfaction [2]. Available data indicates mixed perspectives from fertility patients toward telehealth. In the Netherlands, one study found that while telehealth was rated as a good alternative to in-person visits during the pandemic, only half of respondents described telehealth as a good replacement [11]. While in the USA at a single academic fertility center, patients reported high overall patient satisfaction and willingness to use telehealth again [4]. Conversely, at another academic fertility center, in a study mainly to investigate on fertility patients’ quality of life during COVID-19, patients reported low patient satisfaction with telehealth (<10%), and less than half of patients reported willingness to use telehealth again [12]. Both studies were limited in respondent size (101 and 66 respondents, respectively) [4, 12] and investigated patients confined to a single, urban fertility center.
Thus, more information is needed to ascertain factors from across the USA that influence fertility patient satisfaction and identify areas for improvement to critically understand telehealth’s role in fertility care. We aimed to evaluate a broad group of fertility patients to assess satisfaction toward telehealth visits through a nationally distributed survey using the validated telehealth usability questionnaire (TUQ) [13].
Materials and methods
A cross-sectional, anonymous web-based survey was distributed to national infertility patient groups between February 1st and April 31st, 2021. The survey was disseminated electronically through infertility advocacy groups to reach a wide-ranging, national sample of fertility patients which included posts on the national RESOLVE website, RESOLVE social media pages, RESOLVE New England social media pages, and email distribution through Colorado Fertility Advocates. RESOLVE is the National Infertility Association that participates in patient advocacy and offers support groups to patients. Given survey distribution methods, the number of patients who viewed the survey but chose not to respond is unknown.
Survey creation
The survey consisted of the validated Telehealth Usability Questionnaire (TUQ) administered in English [13]. The TUQ consists of 21 questions that address the usability of telehealth systems intended for either patients or clinicians. The TUQ was chosen to assess patient satisfaction based on a review of the literature to identify validated tools and its internal reliability [13, 14]. The questionnaire comprehensively covers telehealth usability factors such as usefulness, ease of use, effectiveness, reliability, and satisfaction [13]. The TUQ was created from existing validated telehealth questionnaires with robust content validity [13]. The TUQ does not generate a scoring system. Therefore, we assigned the TUQ question regarding overall satisfaction using telehealth as the primary outcome. Responses were assessed using a 7-point Likert scale (1: strongly disagree; 2: disagree; 3: somewhat disagree; 4: neutral; 5: somewhat agree; 6: agree; 7: strongly agree). Additional questions to the survey included demographic information, infertility treatment history, and future visit type preference. General free text comments regarding telehealth for fertility care were also solicited. A copy of the survey is available at https://redcap.ucdenver.edu/surveys/?s=YEYPMTLWFTPDEPMC. This study was deemed exempt by the Colorado Multiple Institutional Review Board.
Inclusion criteria were any respondent who self-reported previously using telehealth for fertility care, ≥18 years old, and lived in the USA. Respondents who started but did not complete the survey were excluded from analysis. Though the survey was answered anonymously, an individualized, nonidentifying respondent code using the respondent birth year and last four digits of their phone number was generated to discourage repeated survey entry. There was no incentive for participation.
Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at the University of Colorado. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for data integration and interoperability with external sources [15].
Statistical analysis
Descriptive statistics were used to characterize the study population and summarize patient responses to items in the TUQ. Using the primary outcome statement in the TUQ, “Overall, I am satisfied with the telehealth system,” respondents were defined as “satisfied” (Likert score 5–7) or “neutral/unsatisfied” (Likert score 1–4). We compared characteristics of participants who were satisfied with the telehealth system to those who were not using appropriate bivariate statistics including t-tests or non-parametric equivalents for continuous variables and chi-squared and Fisher’s exact tests for dichotomous and categorical variables. SAS 9.4 software was used for analysis. Qualitative comments were grouped by theme using the TUQ categories: usefulness, visit quality, reliability, satisfaction, and future use.
Results
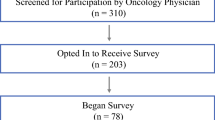
Number of respondents and demographics
A total of 115 respondents initiated the survey, with 81 respondents completing the full survey. The 81 completed surveys were included for analysis, and respondent demographics are listed in Table 1. All respondents were female. The mean age of respondents was 35.9 years old (standard deviation ± 4.1). Most respondents were Caucasian (77.8%), with an income of >$100,000 per year (76.5%). Respondents most commonly resided in the Midwest (30.9%) or the Rocky Mountain (25.9%) regions. Of the 81 respondents, 60 (61.7%) traveled less than 45 min to reach their physician’s office. Nearly three-fourths of the respondents (72.8%) had undergone fertility treatment during the pandemic, most commonly in vitro fertilization (IVF) with or without another form of assisted reproductive technology (ART), such as ovulation induction and/or intrauterine insemination (54.3%, n=44).
Overall satisfaction and TUQ responses
Most respondents reported high patient satisfaction with telehealth, with 81.4% (n=66; 95% CI 72.8–90.1%) responding they agree (Likert score ≥5) to the primary outcome item, “overall I am satisfied with the telehealth system” (Table 1). Of the 66 respondents with high satisfaction for telehealth, over half (59.1%, n=39) indicated they strongly agree (Likert score of 7). Only 12.3% (n=10) of respondents indicated dissatisfaction with telehealth (Likert score ≤3). A total of 6.2% (n=5) reported a neutral response (Likert score of 4).
Responses were positive toward telehealth in all categories of usefulness, ease of use, effectiveness, reliability, and satisfaction (Supplemental Figure I). Respondents reported the highest Likert score, strongly agree, with a frequency ranging from 25.9 to 76.5% per item. For example, 76.5% (n=62) agreed (Likert 5–7) that “telehealth improves my access to healthcare” and 81.4% (n=66) agreed that “telehealth is an acceptable way to receive health services.” The only TUQ item without an overall positive response (Likert 5–7) was to the item, “the system gave me error messages that clearly told me how to fix problems,” to which the majority response was a neutral score (39.3%, n=11 of 28 item responses). See Supplemental Figure I for full TUQ survey responses.
Patient characteristics and satisfaction
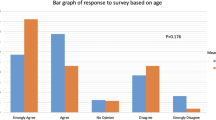
We assessed the relationship between satisfied vs neutral/unsatisfied respondents with income, insurance status, and age and found no association with satisfaction (all p values > 0.05). In addition, neither patients’ proximity to their provider’s office according to travel time required to see their physician nor living in a rural vs suburban/urban area impacted satisfaction (all p values > 0.05).
Non-TUQ items
Several questions were added to the telehealth survey that were negatively framed to match TUQ items. The responses to matched items were comparable, suggesting internal survey consistency among respondents. The most frequent response to the negatively framed items was strongly disagree (46.9–58.0%) (Supplemental Figure I). For example, 81.4% of respondents (66 of 81) disagreed with the negatively framed statement that they would not use telehealth again, which aligns with the 77.8% (63 of 81) who affirmed the positively framed TUQ question that they would use telehealth again.
Patient preferences
When given the option, 60.5% of patients (n=49) expressed a preference for in-person visits with fertility providers for their initial visit (Fig. 1). The remainder of the responses for initial visit preference were equally split between no preference (19.8%) and telehealth (19.8%). For follow-up visits, the proportion of patients who preferred in-person visits dropped to 23.5% (n=19), while more patients preferred telehealth visits (49.4%). The proportion of patients who had no preference for visit type remained similar for follow-up visits, 27.2% (n=22) (Fig. 1).
Themes from respondent comments
Respondents were given the opportunity to provide additional comments about their experiences with telehealth for fertility care. Comments and themes are summarized in Fig. 2. In general, comments were positive (22 of 37), with many respondents noting improved access to care, reduced travel time, and increased flexibility to incorporate healthcare visits within their work schedules with telehealth visits. Negative comments (n=15) noted that telehealth visits can seem rushed and more impersonal than in-person visits. Nine respondents noted dissatisfaction with telehealth visits specifically when a video was not incorporated.
Discussion
Our results demonstrate overall high levels of patient satisfaction and acceptability toward telehealth for fertility care and support its long-term role in our field. Respondents found telehealth to be useful, easy, effective, and reliable. Although satisfaction with telehealth was high and preferred for follow-up visits, our respondents still expressed a preference for face-to-face visits for initial consultations.
Comments solicited from this survey suggest that patients seeking fertility care value the initial connection with their provider. Respondents commented that telehealth appointments can feel more rushed, more robotic, and less personal. While we did not investigate visit lengths in this study, a prior single-site study found initial telehealth visits to be only 3 min shorter than in-person visits [16]. It remains unclear if the impression of feeling rushed is due to shorter visits or the nature of the visit type. Among comments, a negative theme emerged when patients were unable to see their provider’s face (either video turned off or due to technical difficulties). We did not elucidate platforms used for telehealth visits, which may impact patient ease of use and satisfaction. Also, some respondents noted being unable to feel their provider’s sincerity. By understanding patient perspectives toward telehealth, physicians practicing telehealth have an opportunity to mitigate the more impersonal and hurried feeling of visits, for example, asking more open-ended questions as patients can be more hesitant to speak up during appointments, keeping their camera on to increase patient rapport, and improving any technical issues in their communication platforms.
Nationally, access to fertility care is geographically inequal. Almost 40% of reproductive-aged women have limited or no geographic proximity to nearby assisted reproductive services [17], and ART clinics tend to be located in areas with greater socioeconomic status and increasing population density [18]. Telehealth can increase access for these patients by avoiding extensive travel and the potential need for time off work for at least the consultation portion of patient care. Cost savings because of avoided travel costs and time off work mean that patients’ savings can instead be allocated toward treatment. While there are a wide variety of forces limiting access to fertility care (emotional, sociocultural, bias) [19], the cost of care has been identified as an important barrier to fertility care which disproportionately affects racial and ethnic minorities [19, 20]. While estimates of cost savings with telemedicine for female patients seeking fertility care are unknown, a study of male infertility patients estimated that a patient saves a median of 97 min and $149–252 per clinic visit by avoiding travel and taking time off work [21]. Regarding travel time, studies in other specialties found that preference for telehealth increases when patients live more than 5 miles from the office [22]. However, previous studies examining fertility patients have demonstrated no preference for telehealth visits based on distance from the office [4]. In the current study, we did not see that distance from the fertility clinic impacted patient satisfaction in our survey, but the sample size was underpowered to detect this difference. The avoided commuter stress of telehealth visits or cost savings may not outweigh benefits of a face-to-face visit in our specific field, and additional work is needed to explore these factors in the context of fertility care.
It is known that patients with no insurance and lower income seek fertility care less frequently [23]. Thus, we examined if telehealth satisfaction may differ by patient income and insurance coverage. Reassuringly, in our respondents, we found that income and insurance coverage did not impact patient satisfaction with telehealth.
Our results are in line with the current limited data available on fertility patient perspectives toward telehealth. Anderson et al. demonstrated similar rates of high patient satisfaction using telehealth and reported a similar rate of patient preference (61%) for telehealth follow-up visits at a single academic fertility center [4]. Our respondents’ levels of satisfaction also mimic provider attitudes toward telehealth, which are in general quite high (>90%) [24], indicating acceptability toward telehealth on both sides of the screen. Our national survey study represents patient preferences that contributes to the currently scant field of telehealth and infertility research. In addition, we further delineated that retrospectively, many patients preferred their initial visits to be in-person and generated themes in patient perspectives based on open-ended responses.
Limitations of this study include the timeline of when this study was performed and the changing nature of the COVID-19 pandemic. This survey was distributed in the first few months after COVID-19 vaccines became commercially available. Patient perspectives and outlooks may evolve with increasing vaccination uptake and as generally milder strains of COVID emerge which may make in-person visits more palatable. Second, the generalizability of study findings is limited by the small sample size of survey respondents. In addition, our survey was distributed through national advocacy groups to reach a national sampling of patients; however, affiliation of our respondents with advocacy groups may bias our results toward patients who may be more passionate or more educated on the topic. Finally, our respondents were mostly Caucasian, had an average income higher than the national median, and were English-speaking. These demographics align with those in other fertility studies, which suggests our study respondents may be representative of patients seeking fertility care in the USA [25, 26]; however, additional research is needed to capture patient perspectives of other demographic groups utilizing telehealth for fertility care.
Strengths of our study include the use of a robustly validated TUQ survey which assesses specifically patient perspectives toward telehealth in categories of usefulness, ease of use, effectiveness, reliability, and satisfaction. Respondents answered the survey anonymously, which may provide more honest critiques of telehealth. In addition, because the statements posed in the TUQ are positively framed toward telehealth, we added several negatively framed statements to the end of the survey to assess for internal consistency of the respondents. Overall, these negatively framed statements demonstrated that respondents were answering consistently to the survey statements since responses to negatively framed statements were as expected and converse to the corresponding positive statement. Finally, this study adds to the limited available data on patient perspectives in the USA toward telehealth for infertility. While telehealth data is available on other medical specialties, the need to understand our patients deeper is critical, as fertility care is an inherently personal and sensitive field.
Future work is needed with larger sample sizes to elucidate other factors that may influence satisfaction, for example, a patient’s primary language and to determine if telehealth influences patients’ comprehension of their diagnosis and their treatment options. In addition, more research is needed on the economic benefits of telehealth for fertility care. While telehealth may reduce the direct and indirect cost burden of fertility care and reduce geographical inequalities, there remain other barriers to fertility care, such as sociocultural and emotional factors, which need to be explored in the setting of telehealth care. Future studies could consider utilizing a broader social media campaign, perhaps with age-targeted ads, to reach a larger and more diverse patient population.
Conclusion
Survey respondents who utilized telehealth for fertility care expressed high rates of overall satisfaction with virtual care. However, when given the option, most patients in the current study still prefer in-person visits to establish initial care. For follow-up visits, most respondents prefer telehealth or had no preference. Based on the findings of this study, incorporation of telehealth in fertility practices should continue, though it may be helpful for patients to be given options for visit types.
References
Uustal M, Blackmon L. Telemedicine technology and implications for reproductive office operations. Fertil Steril. 2020;114(6):1126–8.
Berg WT, Goldstein M, Melnick AP, Rosenwaks Z. Clinical implications of telemedicine for providers and patients. Fertil Steril. 2020;114(6):1129–34.
Ramaswamy A, Yu M, Drangsholt S, Ng E, Culligan PJ, Schlegel PN, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786.
Anderson K, Coskun R, Jimenez P, Omurtag K. Satisfaction with new patient telehealth visits for reproductive endocrinology patients in the era of COVID-19. J Assist Reprod Genet. 2022;39(7):1571–6.
Boehm K, Ziewers S, Brandt MP, Sparwasser P, Haack M, Willems F, et al. Telemedicine online visits in urology during the COVID-19 pandemic-potential, risk factors, and patients’ perspective. Eur Urol. 2020;78(1):16–20.
Oleg Bestsennyy GG, Alex Harris, Jennifer Rost. Telehealth: a quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company2021 [cited 2022 10/15/22]; Available from: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality.
Alvero R. Editorial: It was the best of times; it was the worst of times: the impact of the SARS-CoV2 (COVID-19) pandemic on reproductive endocrinology. Curr Opin Obstet Gynecol. 2021;33(4):324–6.
Parry JP, Chen SH, Ku L, Anderson K, Keller SL, Omurtag K, et al. Is telehealth a valuable resource in reproductive endocrinology and infertility? Fertil Steril. 2022;117(4):690–5.
Peahl AF, Powell A, Berlin H, Smith RD, Krans E, Waljee J, et al. Patient and provider perspectives of a new prenatal care model introduced in response to the COVID-19 pandemic. Am J Obstet Gynecol. 2020;224(4):384–e1.
Tenforde AS, Borgstrom H, Polich G, Steere H, Davis IS, Cotton K, et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am J Phys Med Rehabil. 2020;99(11):977–81.
Rosielle K, Bergwerff J, Schreurs AMF, Knijnenburg J, De Bie B, Maas JWM, et al. The impact of the COVID-19 pandemic on infertility patients and endometriosis patients in the Netherlands. Reprod Biomed Online. 2021;43(4):747–55.
Pearson H, Gerber RP, Brownridge SR, Goldman RH, Mullin C. Impact of COVID-19 on quality of life and patient satisfaction amongst patients seeking fertility evaluation and treatment. Fertil Steril. 2020;114(3):e178.
Parmanto B, Lewis AN Jr, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ). Int J Telerehabil. 2016;8(1):3–10.
Langbecker D, Caffery LJ, Gillespie N, Smith AC. Using survey methods in telehealth research: a practical guide. J Telemed Telecare. 2017;23(9):770–9.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Alexander VM, Schelble AP, Omurtag KR. Traits of patients seen via telemedicine versus in person for new-patient visits in a fertility practice. F&S Rep. 2021;2(2):224–9.
Harris JA, Menke MN, Haefner JK, Moniz MH, Perumalswami CR. Geographic access to assisted reproductive technology health care in the United States: a population-based cross-sectional study. Fertil Steril. 2017;107(4):1023–7.
Tierney KI. Geographic distribution of assisted reproductive technology clinics in the USA: a multilevel sociodemographic analysis. J Assist Reprod Genet. 2022;39(11):2505–19.
Adashi EY, Dean LA. Access to and use of infertility services in the United States: framing the challenges. Fertil Steril. 2016;105(5):1113–8.
Quinn M, Fujimoto V. Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril. 2016;105(5):1119–23.
Andino J, Zhu A, Chopra Z, Daignault-Newton S, Ellimoottil C, Dupree JM. Video visits are practical for the follow-up and management of established male infertility patients. Urology. 2021;154:158–63.
Satin AM, Shenoy K, Sheha ED, Basques B, Schroeder GD, Vaccaro AR, et al. Spine patient satisfaction with telemedicine during the COVID-19 pandemic: a cross-sectional study. Global Spine J. 2020;22:2192568220965521.
Kelley AS, Qin Y, Marsh EE, Dupree JM. Disparities in accessing infertility care in the United States: results from the National Health and Nutrition Examination Survey, 2013-16. Fertil Steril. 2019;112(3):562–8.
Dilday EA, Douglas CR, Al-Safi ZA. Telehealth provider experience in reproductive endocrinology and infertility clinics during the COVID-19 pandemic and beyond. J Assist Reprod Genet. 2022;39(7):1577–82.
Childress KJ, Lawson AK, Ghant MS, Mendoza G, Cardozo ER, Confino E, et al. First contact: the intersection of demographics, knowledge, and appraisal of treatment at the initial infertility visit. Fertil Steril. 2015;104(1):180–7.
Negris O, Lawson A, Brown D, Warren C, Galic I, Bozen A, et al. Emotional stress and reproduction: what do fertility patients believe? J Assist Reprod Genet. 2021;38(4):877–87.
Acknowledgements
We would like to thank all the individuals who participated in this study and Heather Aldrich, PhD, for proofreading our manuscript.
Funding
This publication was supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535 which provides RedCap access.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ivy Lersten, Jeanelle Sheeder, Christina Yannetsos, Angela Fought, and Cassandra Roeca. The first draft of the manuscript was written by Ivy Lersten, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Cassandra Roeca has been a paid advisor for Ferring Pharmaceuticals. Its contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Ethics approval
This is an observation study deemed exempt by the Colorado Multiple Institutional Review Board from requiring ethical approval.
Consent to participate
All participants in this study were voluntary and provided informed consent, and no identifying patient information is present in this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lersten, I., Fought, A., Yannetsos, C. et al. Patient perspectives of telehealth for fertility care: a national survey. J Assist Reprod Genet 40, 1369–1376 (2023). https://doi.org/10.1007/s10815-023-02811-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02811-1