Abstract
Purpose
To investigate the effect of climatic parameters in the mesothermal climate area on clinical pregnancy and live birth following fresh single blastocyst transfer.
Methods
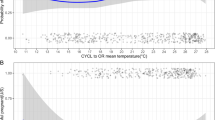
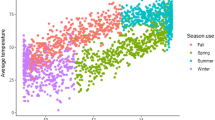
This study investigated clinical pregnancies and live births that resulted from 555 ovarian stimulation cycles followed by fresh single blastocyst transfer. The samples were stratified according to climatic conditions (low T, temperature < 12.9 °C; middle T, 12.9 °C ≤ temperature < 22.6 °C; high T, temperature ≥ 22.6 °C; low H, relative humidity < 62.1%; middle H, 62.1% ≤ relative humidity < 66.5%; high H, relative humidity ≥ 66.5%; short S, sunlight duration < 5.2 h; middle S, 5.2 h ≤ sunlight duration < 6.7 h; long S, sunlight duration ≥ 6.7 h). Clinical pregnancy and live birth rates among three groups from each climatic parameter were compared. Multivariable analyses were performed to investigate the effects of climatic conditions on blastocyst development, endometrial thickness, clinical pregnancy, and live birth.
Results
A statistically significant difference was found in pregnancy rates among low T (48.8%), middle T (37.3%), and high T (36.6%) groups. Multivariable analyses revealed that temperature was associated with clinical pregnancy and live birth rates with adjustment for patient age, BMI, type of ovarian stimulation, endometrial thickness, and expansion grade of the transferred blastocyst. The association between climatic parameters and blastocyst development and endometrial thickness was not confirmed.
Conclusions
This study suggests that lower temperatures in the mesothermal climate area could favorably affect the rates of clinical pregnancy and live birth achieved by fresh single blastocyst transfer.


Similar content being viewed by others
Data availability
Correspondence and requests for data and material should be addressed to H. M.
Code availability
Not applicable.
References
Smits LJ, Van-Poppel FW, Verduin JA, Jongbloet PH, Straatman H, Zielhuis GA. Is fecundability associated with month of birth? An analysis of 19th and early 20th century family reconstitution data from The Netherlands. Hum Reprod. 1997;12:2572–8.
Mathers CD, Harris RS. Seasonal Distribution of Births in Australia. Int J Epidemiol. 1983;12:326–31.
Casper RF, Erskine HJ, Armstrong DT, Brown SE, Daniel SA, Graves GR, et al. In vitro fertilization: diurnal and seasonal variation in luteinizing hormone surge onset and pregnancy rates. Fertil Steril. 1988;49:644–8.
Kivelä A, Kauppila A, Ylöstalo P, Vakkuri O, Leppäluoto J. Seasonal, menstrual and circadian secretions of melatonin, gonadotropins and prolactin in women. Acta Physiol Scand. 1988;132:321–7.
Levine RJ, Bordson BL, Mathew RM, Brown MH, Stanley JM, Star TB. Deterioration of semen quality during summer in New Orleans. Fertil Steril. 1988;49:900–7.
Yie SM, Brown GM, Liu GY, Collins JA, Daya S, Hughes EG, et al. Melatonin and steroids in human pre-ovulatory follicular fluid: seasonal variations and granulosa cell steroid production. Hum Reprod. 1995;10:50–5.
Rojansky N, Benshushan A, Meirsdorf S, Lewin A, Laufer N, Safran A. Seasonal variability in fertilization and embryo quality rates in women undergoing IVF. Fertil Steril. 2000;74:476–81.
Fleming C, Nice L, Hughes AO, Hull MG. Apparent lack of seasonal variation in implantation rates after in-vitro fertilization. Hum Reprod. 1994;9:2164–6.
Stolwijk AM, Reuvers MJ, Hamilton CJ, Jongbloet PH, Hollanders JM, Zielhuis GA. Seasonality in the results of in-vitro fertilization. Hum Reprod. 1994;9:2300–5.
Farland LV, Correia KFB, Missmer SA, Racowsky C. Seasonal variation, temperature, day length, and IVF outcomes from fresh cycles. J Assist Reprod Genet. 2020;37:2427–33.
Kimberly L, Case A, Cheung AP, Sierra S, AlAsiri S, Carranza-Mamane B, et al. Advanced reproductive age and fertility: no.269 November 2011. Int J Gynaecol Obstet. 2012;117:95–102.
García-Ferreyra J, Carpio J, Zambrano M, Valdivieso-Mejía P, Valdivieso-Rivera P. Overweight and obesity significantly reduce pregnancy, implantation, and live birth rates in women undergoing In Vitro Fertilization procedures. JBRA Assist Reprod. 2021;25:394–402.
Al-Inany HG, Abou-Setta AM, Aboulghar M. Gonadotrophin-releasing hormone antagonists for assisted conception: a Cochrane review. Reprod Biomed Online. 2007;14:640–9.
Mizuno S, Matsumoto H, Hashimoto S, Brahmajosyula M, Ohgaki A, Tarui S, et al. A novel embryo quality scoring system to compare groups of embryos at different developmental stages. J Assist Reprod Genet. 2021;38:1123–32.
Xu J, Zhang S, Jin L, Mao Y, Shi J, Huang R, et al. The effects of endometrial thickness on pregnancy outcomes of fresh IVF/ICSI embryo transfer cycles: an analysis of over 40,000 cycles among five reproductive centers in China. Front Endocrinol (Lausanne). 2022;12:788706.
Hashimoto S, Nakano T, Yamagata K, Inoue M, Morimoto Y, Nakaoka Y. Multinucleation per se is not always sufficient as a marker of abnormality to decide against transferring human embryos. Fertil Steril. 2016;106:133–9.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: fertility and genetics beyond 1999: the plenary proceedings of the 11th World Congress on In Vitro Fertilization & Human Reproductive Genetics. New York: Parthenon; 1999. pp. 378–88.
Past weather data of Japan. Tokyo, Japan: Japan Meteorological Agency, Ministry of Land, Infrastructure, Transport and Tourism. Available from: https://www.data.jma.go.jp/risk/obsdl/ Accessed 1 Sep 2021.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Zhao M, Zhang H, Waters THB, Chung JPWC, Li TC, Chan DYLC. The effects of daily meteorological perturbation on pregnancy outcome: follow-up of a cohort of young women undergoing IVF treatment. Environ Health. 2019;18:103.
Chang SY, Lan KC, Chen CW, Huang FJ, Tsai MY, Chang CY. The influences of weather on patients with different ovarian responses in the treatment of assisted reproductive technology. J Assist Reprod Genet. 2005;22:191–8.
Claustrat B, Leston J. Melatonin: Physiological effects in humans. Neurochirurgie. 2015;61:77–84.
Webley GE, Luck MR. Melatonin directly stimulates the secretion of progesterone by human and bovine granulosa cells in vitro. J Reprod Fertil. 1986;78:711–7.
Nishihara T, Hashimoto S, Ito K, Nakaoka Y, Matsumoto K, Hosoi Y, et al. Oral melatonin supplementation improves oocyte and embryo quality in women undergoing in vitro fertilization-embryo transfer. Gynecol Endocrinol. 2014;30:359–62.
Dunphy BC, Anderson-Sykes S, Brant R, Pattinson HA, Greene CA. Human embryo implantation following in-vitro fertilization: is there a seasonal variation? Hum Reprod. 1995;10:1825–7.
Kirshenbaum M, Ben-David A, Zilberberg E, Elkan-Miller T, Haas J, Orvieto R. Influence of seasonal variation on in vitro fertilization success. PLoS ONE. 2018;13:e0199210.
Xiao Y, Wang M, Liu K. The influence of seasonal variations on in vitro fertilization and fresh/frozen embryo transfer: a retrospective study. Arch Gynecol Obstet. 2018;298:649–54.
Liu X, Bai H, Mol BW, Shi W, Gao M, Shi J. Seasonal variability does not impact in vitro fertilization success. Sci Rep. 2019;9:17185.
Correia KFB, Farland LV, Missmer SA, Racowsky C. The association between season, day length, and temperature on clinical outcomes after cryopreserved embryo transfer. Fertil Steril. 2022;117:539–47.
Politoff L, Birkhauser M, Almendral A, Zorn A. New data confirming a circannual rhythm in spermatogenesis. Fertil Steril. 1989;52:486–9.
Centola GM, Eberly S. Seasonal variations and age-related changes in human sperm count, motility, motion parameters, morphology, and white blood cell concentration. Fertil Steril. 1999;72:803–8.
Wach-Gygax L, Burger D, Malama E, Bollwein H, Fleisch A, Jeannerat E, et al. Seasonal changes of DNA fragmentation and quality of raw and cold-stored stallion spermatozoa. Theriogenology. 2017;99:98–104.
Crespo F, Quiñones-Pérez C, Ortiz I, Diaz-Jimenez M, Consuegra C, Pereira B, et al. Seasonal variations in sperm DNA fragmentation and pregnancy rates obtained after artificial insemination with cooled-stored stallion sperm throughout the breeding season (spring and summer). Theriogenology. 2020;148:89–94.
Ausejo R, Martínez JM, Soler-Llorens P, Bolarín A, Tejedor T, Falceto MV. Seasonal Changes of Nuclear DNA Fragmentation in Boar Spermatozoa in Spain. Animals (Basel). 2021;11:465.
Simon L, Zini A, Dyachenko A, Ciampi A, Carrell DT. A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J Androl. 2017;19:80–90.
McQueen DB, Zhang J, Robins JC. Sperm DNA fragmentation and recurrent pregnancy loss a systematic review and meta-analysis. Fertil Steril. 2019;112:54–60.
Setti AS, Braga DPAF, Provenza RR, Iaconelli A Jr, Borges E Jr. Oocyte ability to repair sperm DNA fragmentation: the impact of maternal age on intracytoplasmic sperm injection outcomes. Fertil Steril. 2021;116:123–9.
Acknowledgements
The authors would like to thank Dr. Avila A for the English language review.
Author information
Authors and Affiliations
Contributions
H. M. designed the study, analyzed the clinical data, interpreted the results, and wrote the manuscript with help from all authors. S. H. and S. M. were involved in the analysis of clinical data, interpretation of the results, and writing the manuscript. A. F. and Y. M. were involved in IVF, interpretation of the results, and supervised the project.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional review board of IVF Osaka Clinic.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsumoto, H., Hashimoto, S., Mizuno, S. et al. Influence of climatic conditions in the mesothermal climate area on pregnancies following elective fresh single blastocyst transfer. J Assist Reprod Genet 39, 2789–2797 (2022). https://doi.org/10.1007/s10815-022-02668-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02668-w