Abstract
Recent advances in targeted therapy with monoclonal antibodies have significantly improved outcomes for people with cancer, sometimes allowing patients to avoid ovotoxic agents altogether. The current understanding is that monoclonal antibody cancer therapies that are not targeted to ovarian antigens should not impact ovarian reserve or increase the risk of primary ovarian insufficiency (POI). We present a case of rapid onset POI in a 23-year-old patient following chemotherapy for relapse/refractory B-cell acute lymphoblastic leukemia with a monoclonal antibody drug-conjugate, inotuzumab ozogamicin, that targets CD22. She was also treated with intrathecal methotrexate, cytarabine, and vincristine which are typically considered low risk for ovotoxicity. She was ovulatory with an AMH of 1.0 ng/mL prior to treatment and 2 months later was found to have an undetectable AMH. The patient experienced a canceled fertility preservation cycle due to an absent response to gonadotropins during ovarian stimulation. Consideration should be given to potential gonadal effects of monoclonal antibody therapies that may not have previously been explored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Future fertility is a significant concern for people with a recent cancer diagnosis [1]. In particular, people treated with certain cytotoxic agents or radiation are at risk for primary ovarian insufficiency (POI). The mechanisms of action for ovarian injury may include either follicular dysfunction, follicle depletion, or oocyte depletion [2]. Alkylating agents are a mainstay of many cancer chemotherapeutic regimens and are also known for being ovotoxic. The degree to which other chemotherapeutic agents may affect the ovaries is often compared to the alkylating agent cyclophosphamide [3]. Recent advancements in targeted therapy with monoclonal antibodies have significantly improved outcomes for people with cancer, sometimes allowing patients to avoid ovotoxic agents altogether [4], and are a promising treatment for sparing reproductive function. The current understanding is that monoclonal antibody cancer therapies that are not targeted to ovarian antigens should not impact ovarian reserve or increase the risk of POI.
We present a case of rapid onset POI in a patient following chemotherapy for relapse/refractory B-cell acute lymphoblastic leukemia (RR B-ALL) with a monoclonal antibody drug-conjugate, inotuzumab ozogamicin (IO). IO is a monoclonal anti-CD22 antibody conjugated to a cytotoxic agent, calicheamicin [5]. The CD22 antigen targeted by IO is a transmembrane sialoglycoprotein protein that is expressed in more than 90% of patients with B-ALL. Notably, the CD22 antigen is not expressed on non-B lineage cells nor hematopoietic stem cells, making it an attractive therapeutic target [5]. Furthermore, it is not known to be widely expressed in the ovary. Once IO is internalized within the target cell, calicheamicin is metabolized to form an enediyne diradical that induces DNA double-stranded breaks [5]. In a phase III clinical trial, IO demonstrated improved efficacy over standard care in the treatment of acute lymphoblastic leukemia [6]. IO therapy is reported as being well-tolerated, and to date, there are no human reports of an impact of IO therapy on the ovaries. Preclinical animal toxicology studies have raised concerns that IO may influence fertility at doses higher than the recommended maximal dose in humans. When rats were exposed to increasing levels of IO during the preconception period, mated female rats had a higher prevalence of resorbed embryos and a lower gravid uterus weight. Additionally, ovarian atrophy was demonstrated in cynomolgus monkeys when exposed to increasing doses of IO. However, no studies explicitly demonstrated ovotoxicity [7, 8]. Some monoclonal antibodies used for childhood cancers such as rituximab have not been associated with fertility impairment whereas other monoclonal antibody therapies like dinutuximab and atezolizumab have limited animal data or no data at all on their reproductive impacts [9]. Our case report raises questions of a potential adverse effect of IO on the ovarian reserve independently or in combination with ancillary chemotherapeutic agents.
Methods
Data were extracted from the electronic medical record of the patient and included the history of present illness, medical history, and evaluation necessary for planned fertility preservation. The University of Chicago Internal Review Board determined this case to be exempt from an extended review (IRB 22-0114).
Case presentation
A 23-year-old G0 woman presented to the University of Chicago Section of Reproductive Endocrinology and Infertility in January 2020 for a fertility preservation consultation prior to a preparative regimen and total body irradiation in anticipation of a stem cell transplant for treatment of RR-BALL.
Until her diagnosis with B-ALL, her medical history was unremarkable. The patient underwent menarche at age 12 with regular menstrual cycles and had no prior pregnancy history or attempts.
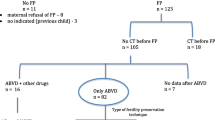
Upon initial diagnosis of B-ALL in 2011 at age 15, she underwent the Children’s Oncology Group Protocol AALL0232 [10]. She initiated treatment in December of 2011. Her protocol included a 4-week induction chemotherapy regimen of intrathecal (IT) cytarabine, intravenous (IV) vincristine, IV daunorubicin, IT methotrexate, and intramuscular (IM) PEG-asparaginase. In January of 2012, she was transitioned to consolidation therapy of IV cyclophosphamide, cytarabine, oral mercaptopurine, IV vincristine, IM PEG-asparaginase, and IT methotrexate. She received maintenance therapy from 2012 to 2014 which consisted of thioguanine, methotrexate, vincristine, cytarabine, and Erwinia asparaginase (Fig. 1). She completed therapy in 2014 at age 16. Notable complications of therapy included the development of deep vein thrombosis and an allergy to PEG-asparaginase that was subsequently substituted with Erwinia asparaginase. She did not undergo any fertility preservation prior to this treatment.
She experienced amenorrhea at age 15 during the B-ALL chemotherapy. Menstruation resumed at age 17 several months after treatment completion of maintenance treatment. Menstrual cycles were regular occurring approximately monthly.
She remained in remission until January 2020, when at age 23, recurrence of B-ALL was confirmed with bone marrow aspirate. Unfortunately, her recurrence included central nervous system involvement. After her recurrence was diagnosed, she had a consultation for fertility preservation. At the time, she had an anti-mullerian hormone level of 1.0 ng/mL, random follicle-stimulating hormone (FSH) level of 4.6 mIU/mL, luteinizing hormone (LH) of 8.3 IU/L, estradiol of 100 pg/mL, and an antral follicle count of 15 (Table 1). She was ovulatory at this time and had reported regular menstrual cycles since the discontinuation of her maintenance therapy at age 17.
While awaiting stem cell transplant, she initiated maintenance therapy with IT methotrexate 15 mg once at the start of therapy, followed by combination IT methotrexate 15 mg and cytarabine 40 mg on her 6th and 35th days of treatment. Additionally, she received inotuzumab 0.77 mg × intravenously on the 2nd and 16th days of treatment (Fig. 1). A plan was made to pursue fertility preservation after completion of maintenance therapy but prior to her preparative treatment and stem cell transplant.
Ovarian stimulation
Due to the start of the COVID-19 pandemic, her fertility preservation care was transferred to a collaborating clinic 6 weeks after her initial consultation. At her baseline evaluation for ovarian stimulation, her AMH was undetectable (< 0.08 ng/mL), FSH and E2 values were 15.7 mIU/mL and 100 pg/mL, respectively (Table 1), and transvaginal ultrasound detected an antral follicle count of 0. The patient also reported no menses since her last menstrual period on January 24, 2020, shortly after her initial fertility preservation consultation. The patient was counseled on the low likelihood of a successful egg retrieval if she were to pursue cryopreservation. However, the patient elected to proceed with ovarian stimulation. Despite gonadotropin stimulation with an FSH agent 300 IU which was increased to 450 IU, and also human menopausal gonadotropin of 150 IU, she experienced no follicular growth and her estradiol peaked at 47 pg/mL. Her cycle was canceled on day 11 for no follicular response.
One week following discontinuation of ovarian stimulation, the patient underwent transvaginal ultrasound which demonstrated an 18 mm and 9 mm ovarian cystic structure. She did not experience spontaneous menses after this evaluation. One month later, her FSH was 54.5, LH 39.2, and estradiol 32 pg/mL. Two months later, her gonadotropins continued to be elevated with an FSH of 78 IU/mL and an estradiol level < 10 (Table 1). She continued to be amenorrheic and began experiencing hot flashes and vaginal dryness.
She was diagnosed with primary ovarian insufficiency and started on hormone replacement therapy with estradiol 0.1 mg/24 h patch and micronized progesterone 200 mg nightly for 12 nights per month. The patient experienced an improvement in perimenopausal symptoms and began having regular withdrawal bleeds. Ultimately, she completed treatment for her R-BALL which included total body irradiation and a stem cell transplant. She is currently in remission.
Sixteen months later, she discontinued hormone replacement therapy. One month later, her AMH was retested and remained undetectable, FSH was 97.9, and estradiol was < 15 (Table 1). Anti-adrenal antibody testing was negative. She restarted hormone replacement therapy, and although she has been informed of her options for family building with donor oocytes, she is not currently interested in fertility. A summary timeline of events is provided in Fig. 1.
Discussion
We present a case of rapid onset primary ovarian insufficiency after treatment with chemotherapy thought to be relatively benign to the ovaries or with unknown impact on the ovary. This patient presented with borderline diminished ovarian reserve but with demonstrably functional ovaries and regular menstrual cycles prior to maintenance treatment for the recurrence of B-ALL. Adjunct agents used in her maintenance treatment including intrathecal methotrexate, and cytarabine, present a low risk of ovotoxicity which raises the possibility that IO may have contributed to this patient’s rapid onset POI [11, 12].
Inotuzumab
To date, IO has not been associated with primary ovarian insufficiency in human clinical trials. In a 2016 open-label, two-arm, randomized, phase 3 trial of inotuzumab compared to standard therapy for ALL, no reproductive adverse effects were reported [6]. IO is rapidly internalized and delivers the calicheamicin (cytotoxic antibiotic agent) intracellularly wherein it binds to the minor groove of DNA and induces double strand cleavage and subsequent apoptosis [5]. Double-stranded DNA breaks are known to cause injury to the ovarian follicular pool. An older study on a proposed chemotherapeutic agent with anti-CD22 activity linked to ricin demonstrated a significant decrease in ovarian size in mice [13]. In the 2016 Multiple-Discipline Review for the Center for Drug Evaluation and Research, it was reported that ovarian atrophy was seen in a colony of monkeys treated specifically with IO [8]. Altogether, limited animal data suggest that it is possible IO could lead to either granulosa cell or oocyte injury. It is also conceivable that IO may have a synergistic effect with one of the other agents included in this patient’s chemotherapeutic regimen. The patient also received intensive intrathecal cytarabine, methotrexate, and hydrocortisone. Although these agents are not typically associated with ovotoxicity, it is conceivable that they could have contributed to this patient’s POI. Potentially, one of the agents may allow the calicheamicin to be liberated prematurely in the vicinity of granulosa cells or oocytes. Another possibility is that although CD22 has not been described in the ovarian tissue thus far, it may in fact be expressed in the ovaries at certain stages of cellular growth that leave the cell more vulnerable to damage. Alternatively, it is possible that ovarian tissue may express an antigen similar to CD22 such that there is cross-reactivity with the conjugated antibody in IO.
Cytarabine
Cytarabine is an antimetabolite that inhibits DNA polymerase and can also inhibit DNA synthesis in the S phase of cell division [14]. This mechanism of action has not been shown to be particularly ovotoxic. By combining the knowledge of the reproductive effects of agents with known reproductive toxicity, such as cyclophosphamide, into regimens in which agents with less data appear, the reproductive impact of agents such as cytarabine may be inferred. In a case series of young women completing conditioning treatment in preparation for stem cell transplant, one patient, age 21, was treated with cytarabine (3 g/m2 BID for 4 days), and total body irradiation (TBI) with ovarian shielding. Notably, she received a calcineurin inhibitor and a short course of methotrexate, similar to our patient, for GVHD prophylaxis. She experienced amenorrhea after treatment but recovered menses nearly a year after treatment and had a demonstrable rise in AMH from undetectable to 0.39 ng/mL. Importantly, she also was able to conceive and had a live birth in the years following her treatment. Pretreatment AMH was not described in this case series [15]. In this case, a young woman who experienced potentially more ovotoxic treatment with TBI had reasonable resumption of ovarian function after treatment [15].
In a cohort of 7 women with various forms of leukemia or lymphoma, who received a hyper-CVAD protocol (cyclophosphamide, vincristine, doxorubicin, and dexamethasone followed by methotrexate and cytarabine), all but one had a resumption of ovarian function determined by menstrual activity [16]. While it is possible that cytarabine could negatively impact the ovaries, the mechanism of action is not commonly known to have serious ovotoxic effects. Furthermore, limited clinical data have demonstrated that women exposed to cytarabine as well as other more ovotoxic agents have experienced a resumption of ovarian function.
Methotrexate
Methotrexate is a widely used antimetabolite with an important role in oncology, rheumatology, and gynecology. By inhibiting dihydrofolic acid reductase, methotrexate impairs DNA synthesis and repair. It may also have anti-inflammatory or immunosuppressive actions as well [17]. Generally, antimetabolites like methotrexate and cytarabine are considered to have a low risk of ovotoxicity [11, 12]. Studies have demonstrated that even high doses of methotrexate have limited if any impact on ovarian function. In a case series from Shamberger et al., women receiving high dose methotrexate for the treatment of osteosarcomas continued to have menstrual cycles during and after treatment and gonadotropins remained in the normal range [18]. In a prospective study of women with a history of IVF who completed systemic methotrexate treatment for an ectopic pregnancy, pre- and post-treatment AMH levels and IVF outcomes did not differ [19].
Our case report presents some limitations. Although we did evaluate for anti-21-hydroxylase antibodies, we did not evaluate other autoimmune conditions, a karyotype, and other genetic conditions such as a fragile X premutation which are known to lead to POI. Given the temporal relationship between the onset of this patient’s POI and chemotherapy, we felt that many of the conditions that could result in POI were unlikely in this case.
The present case also makes it challenging to disentangle an independent influence of IO from other chemotherapeutic agents used during her initial treatment (consolidation and maintenance) or during maintenance treatment for her recurrence. Most would consider women with an AMH of 1.0 at the age of 23 as having diminished ovarian reserve. It is possible that her initial chemotherapeutic treatment, which included known ovotoxic agents such as cyclophosphamide, may have sensitized the ovary to negatively respond to her relapse maintenance therapy when such agents may not have typically resulted in POI. It is also possible that the initial therapy resulted in an expected reduction of her follicular pool. Having diminished ovarian reserve may have made her ovaries more vulnerable to IO with or without the methotrexate and cytarabine than might typically be expected in someone with a normal ovarian reserve. Although the data on the reproductive effects of IO are limited, and other monoclonal antibodies for pediatric cancers have limited or no reproductive consequences, there are animal data to support that some monoclonal antibodies could be ovotoxic. A 2021 study of checkpoint inhibitor pembrolizumab in a prepubertal mouse model found that PD-1 checkpoint blockade affects the ovarian reserve through a mechanism possibly involving inflammation-mediated follicle depletion. In contrast to IO, PDL-1 expression, the target antigen of pembrolizumab, was demonstrated in the murine ovary [20]. These findings support the role of either a direct effect of anti-PDL-1 treatment or resultant inflammatory responses on ovarian function. It is possible that alteration of circulating immune cells and systemic cytokine levels, in the absence of direct antigen-antibody interactions in the ovary, may directly impact fertility.
Beyond our patient’s diagnosis of RR-BALL, and a history of venous thromboembolism, she was healthy during the onset of her POI. However, we cannot exclude another underlying medical condition that could have predisposed this patient to POI. Importantly, we were able to capture an assessment of her ovarian reserve shortly before maintenance therapy that demonstrated a reasonable ovarian reserve and normal function, which may reduce the likelihood that there was an underlying medical condition influencing her ovaries. Because IO is relatively new and to date, there are no human clinical data on the fertility impacts of IO, our patient may have demonstrated an impact of IO that has only previously been described in animal data. Ultimately, we present a case report which was an isolated event, thus it is possible that multiple factors, or an agent independent of IO, may have contributed to this patient’s rapid onset POI.
Future studies may aim to evaluate the role of inotuzumab or CD22 expression in the ovary over time. More broadly, because the use of monoclonal antibodies and other cancer immunotherapies has expanded rapidly in recent years, additional data are needed on the role of these agents on ovarian function [21]. Additionally, any other cases of POI occurring with the use of inotuzumab or in combination with other maintenance agents such as intrathecal methotrexate and cytarabine should be reported to understand if the current case was an isolated occurrence or demonstrates a previously unknown mechanism of action of these drugs or a window of vulnerability for the ovary.
References
Young K, Shliakhtsitsava K, Natarajan L, et al. Fertility counseling before cancer treatment and subsequent reproductive concerns among female adolescent and young adult cancer survivors. Cancer. 2019;125(6):980–9. https://doi.org/10.1002/cncr.31862.
De Vos M, Devroey P, Fauser BCJM. Primary ovarian insufficiency. Lancet. 2010;376(9744):911–21. https://doi.org/10.1016/S0140-6736(10)60355-8.
Hao X, Anastácio A, Liu K, Rodriguez-Wallberg KA. Ovarian follicle depletion induced by chemotherapy and the investigational stages of potential fertility-protective treatments—a review. Int J Mol Sci. 2019;20(19):4720. https://doi.org/10.3390/ijms20194720.
Hafeez U, Parakh S, Gan HK, Scott AM. Antibody–drug conjugates for cancer therapy. Molecules. 2020;25(20):4764. https://doi.org/10.3390/molecules25204764.
Li L, Wang Y. Recent updates for antibody therapy for acute lymphoblastic leukemia. Exp Hematol Oncol. 2020;9:33. https://doi.org/10.1186/s40164-020-00189-9.
Kantarjian HM, DeAngelo DJ, Stelljes M, et al. Inotuzumab ozogamicin versus standard therapy for acute lymphoblastic leukemia. N Engl J Med. 2016;375(8):740–53. https://doi.org/10.1056/NEJMoa1509277.
Pfizer Inc. Besponsa (inotuzumab ozogamicin) [package insert]. U.S. Food and Drug Administration website. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761040s000lbl.pdf. Revised August 2017. Accessed Sep 29, 2021.
U.S. Food and Drug Administration. NDA/BLA multi-disciplinary review and evaluation: Besponsa (inotuzumab ozogamicin). 2017. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/761040Orig1s000MultidisciplineR.pdf. Accessed 29 Sep 2021.
Chakravarty EF, Murray ER, Kelman A, Farmer P. Pregnancy outcomes after maternal exposure to rituximab. Blood. 2011;117:1499–506.
Larsen EC, Devidas M, Chen S, et al. Dexamethasone and high-dose methotrexate improve outcome for children and young adults with high-risk B-acute lymphoblastic leukemia: a report from Children’s Oncology Group Study AALL0232. J Clin Oncol. 2016;34(20):2380–8. https://doi.org/10.1200/JCO.2015.62.4544.
Fleischer RT, Vollenhoven BJ, Weston GC. The effects of chemotherapy and radiotherapy on fertility in premenopausal women. Obstet Gynecol Surv. 2011;66(4):248–54. https://doi.org/10.1097/OGX.0b013e318224e97b.
Bedoschi G, Navarro PA, Oktay K. Chemotherapy-induced damage to ovary: mechanisms and clinical impact. Future Oncol. 2016;12(20):2333–44. https://doi.org/10.2217/fon-2016-0176.
Ghetie MA, et al. Antitumor activity of Fab’ and IgG-anti-CD22 immunotoxins in disseminated human B lymphoma grown in mice with severe combined immunodeficiency disease: effect on tumor cells in extranodal sites. Cancer Res. 1991;51:5876–80.
Hamada A, Kawaguchi T, Nakano M. Clinical pharmacokinetics of cytarabine formulations. Clin Pharmacokinet. 2002;41(10):705–18. https://doi.org/10.2165/00003088-200241100-00002.
Ashizawa M, et al. Updated clinical outcomes of hematopoietic stem cell transplantation using myeloablative total body irradiation with ovarian shielding to preserve fertility. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant. 2019;25:2461–7.
Seshadri T, Hourigan MJ, Wolf M, Mollee PN, Seymour JF. The effect of the hyper-CVAD chemotherapy regimen on fertility and ovarian function. Leuk Res. 2006;30(4):483–5. https://doi.org/10.1016/j.leukres.2005.08.014.
Maksimovic V, Pavlovic-Popovic Z, Vukmirovic S, et al. Molecular mechanism of action and pharmacokinetic properties of methotrexate. Mol Biol Rep. 2020;47(6):4699–08. https://doi.org/10.1007/s11033-020-05481-9
Shamberger RC, Rosenberg SA, Seipp CA, Sherins RJ. Effects of high-dose methotrexate and vincristine on ovarian and testicular functions in patients undergoing postoperative adjuvant treatment of osteosarcoma. Cancer Treat Rep. 1981;65:739–46.
Oriol B, et al. Systemic methotrexate to treat ectopic pregnancy does not affect ovarian reserve. Fertil Steril. 2008;90:1579–82.
Xu PC, Luan Y, Yu SY, Xu J, Coulter DW, Kim SY. Effects of PD-1 blockade on ovarian follicles in a prepubertal female mouse. J Endocrinol. 2021;252(1):15–30. https://doi.org/10.1530/JOE-21-0209.
Alesi LR, Winship AL, Hutt KJ. Evaluating the impacts of emerging cancer therapies on ovarian function. Curr Opin Endocrine Metab Res. 2021;18:15–28. https://doi.org/10.1016/j.coemr.2020.12.004.
Acknowledgements
We would like to thank Dr. Kara Goldman for reviewing our case report and for her clinical contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent for publication
The patient has consented to the submission of the case report to the journal.
Conflict of interest
Amanda J. Adeleye is a stake holder in Carrot and a consultant for Flo Health. Wendy Stock serves on advisory boards for Pfizer for which she has received speaking honorarium. Neither of the remaining authors have any competing nor financial interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maristany, S., DuVall, A.S., Stock, W. et al. Primary ovarian insufficiency secondary to chemotherapy with inotuzumab ozogamicin and other agents. J Assist Reprod Genet 39, 1733–1738 (2022). https://doi.org/10.1007/s10815-022-02548-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02548-3