Abstract
Purpose
To study patient satisfaction with new patient telehealth visits in a reproductive endocrinology and infertility (REI) office.
Methods
A cross-sectional study in a university-based fertility clinic was completed including all new patients seen via telehealth between March 1, 2021, and August 19, 2021. Primary outcomes were perceived patient satisfaction, access, and preferences to telehealth visits.
Results
A total of 351 participants were contacted, 61.8% (n = 217) agreed to participate in the study, and 28.8% (n = 101) completed the survey. There were no significant differences in age, BMI, distance from clinic, or length of infertility with response to survey. Ninety-three percent of responders would use telehealth services again and were satisfied with the telehealth system. Telehealth improved access to healthcare for 88% and travel time for 96%. The median distance from clinic was 24 miles, and there was no significance difference in preference for telehealth visits over in person visits (p = 0.696).
Conclusions
In the era of COVID-19, healthcare implementation has dramatically changed with a drastic increase in telehealth services. Based on our survey, majority of patients were satisfied with telehealth visits and believed it saved travel time while improving access to REI care. Despite no differences in patient preference for in person versus telehealth depending on their distance from clinic, this is reassuring because patients are satisfied with telehealth for reasons other than distance from clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Telehealth’s long-standing history was first described in the Lancet in 1879 which discussed using a telephone to decrease office visits [1]. Healthcare has irrefutably changed due to the COVID-19 pandemic, and, with the pandemic, many of the barriers to telehealth’s expansion were both temporarily and, in some cases, permanently lifted. The declaration of a public health emergency (PHE) and passing of the Coronavirus Preparedness and Response Supplemental Appropriations Act and subsequent Coronavirus Aid, Relief and Economic Security Act (CARES Act) in the early pandemic expanded reimbursement of telehealth services which had not been previously done. These changes to the telehealth structure and billing have made it an accessible way to deliver specialty care [2]. According to the CDC, from July to October 2021, 20% of all US citizens had a telehealth appointment in the last 4 weeks which demonstrates significant use of these services [3].
Fertility workup differs from most office visits because a typical consultation lasts over 45 min and involves an extensive history and review of systems of the individual or couple [4]. Fertility counseling is complex, and its success relies on establishing a good relationship between the physician and patient. Poor access to fertility services can hinder the patient-physician connection, and lower socioeconomic status as well as lack of fertility insurance coverage can decrease treatment access and success [5, 6]. To better understand health delivery and policy, researchers out of University of Wisconsin-Madison refined and validated data from the 2009–2013 US Census American Community Survey data to create the Area Deprivation Index (ADI) [7]. The ADI can help to represent socioeconomic status (SES) depending on geographic location with a higher number (from 0 to 100) indicating higher disadvantage. The ADI has been previously used to compare trait differences in patients undergoing telehealth versus in person visits in a fertility practice [8].
Although telehealth access is more widespread, there is a paucity of data about patient preferences of visit type in specialty clinics, specifically in REI practices. The Fertility and Reproductive Medicine Center at Washington University School of Medicine/Barnes Jewish Hospital allows patients to choose telehealth versus in person visits; however, patients are encouraged to have telehealth visits. Currently 95% of our new patient consults and return follow-up counseling visits have been via telehealth since April 2020. Investigating patient preferences to this change in practice and overall patient satisfaction is important to improve patient care moving forward. Therefore, our primary aim was to evaluate patient satisfaction with new patient telehealth visits in a REI academic practice.
Materials and methods
Study design and patients
This study was approved by the St. Louis Institutional Review Board (IRB) at Washington University School of Medicine. We conducted a cross sectional study involving all new patient visits at Washington University’s REI clinic from March 1st to August 19th, 2021. Study eligibility criteria included any new consult at our office which included those for infertility or non-infertility indications such as recurrent pregnancy loss, PCOS, or Mullerian anomalies. Patients must also be English speaking and can provide informed consent. Exclusion criteria included patients who requested in person visits and required an interpreter at time of consult.
Any potential patient who had a telehealth visit during this time and met inclusion criteria was called within 2 weeks of their appointment and verbally consented by telephone to participate in the study. If they agreed to participate, a link to the one-time online survey was sent to the patient’s email address. If the patient did not agree to participate, the patient was not contacted further. If the patient did not answer, one subsequent call was done and if still no answer, the patient was not contacted again. Survey data collection and management were done using REDCap electronic data capture tools.
Measures
The 25-question survey included a modified telehealth usability questionnaire (TUQ) survey, a previously published tool to evaluate usability and quality of telehealth interactions, along with REI-specific questions [9]. The TUQ survey is a comprehensive questionnaire evaluating multiple utility and usability factors of telehealth visits and has been rigorously validated and previously used in other studies [10, 11]. The six categories of 3–4 questions were usefulness, ease of use and learnability, interface quality, interaction quality, reliability, and satisfaction and future use. Five questions were removed or modified from the TUQ survey to reduce survey length because nine additional questions were added specific to the REI office with three new categories — follow-up, comfort level, and trainees. Added categories gaged patient understanding of the follow-up plan and their comfort level discussing sensitive manners via telehealth, potentially with trainees (medical students, residents, and fellows). The full survey can be found in supplemental Table 1.
Statistical analysis
All data was analyzed using IBM SPSS v28.0 software (IBM Corp., Armonk, NY, USA). Univariate associations between those that did and did not complete the survey were assessed by chi square or Fisher’s exact tests for categorical variables and t-test or Mann–Whitney U-tests for continuous variables depending on if data was parametric or non-parametric, respectively.
P values < 0.05 were considered statistically significant. Survey results were considered a categorical data and not ordinal data given the data was skewed toward one side.
Results
Patient characteristics
A total of 351 participants were contacted between March 1st and August 19th, 2021, and 217 (61.8%) verbally agreed to participate in the study, and, of those, 101 (46.5%) completed the survey. Five surveys were excluded because the same patient filled out the survey twice. Table 1 demonstrates patient characteristics in those who did and did not complete the survey. All demographic data was similar between groups except for length of infertility at presentation, those that took the survey had a median infertility length of 12 months compared to 23 months in those who did not complete the survey (P < 0.001). However, age, race/ethnicity, distance from clinic, and the national and state area deprivation scores were not significantly different between groups.
Survey responses
For ease of describing the data, if a patient responded “agree” to “strongly agree” to the questions, then it was a positive response; if they responded “no opinion,” then it was a neutral response; and if they responded “disagree” or “strongly disagree,” then it was a negative response. Please see supplemental table 2 for complete responses.
In the 101 patient surveys, 93% of respondents felt comfortable communicating with the clinician and were overall satisfied with the system. Only 3% were neutral and 3% were negative toward the system. Telehealth improved access to healthcare for 88% of respondents and travel time for 96%. Only 4% did not believe telehealth was an acceptable way to receive healthcare services. For interface and interaction quality, 93% thought the system was pleasant and 84% liked using the system. The system was simple and easy to understand for 97% of participants. Ninety-three percent report being able to effectively express themselves while on the telehealth visits. However, 16% did not believe the system could do everything they wanted it to do and did not like using the system.
Of those REI-specific questions, 96% felt comfortable discussing sensitive matters related to the visit via telehealth and only 2% of respondents felt embarrassed during the visit. Most patients felt comfortable with learners present, and 88% and 80% were comfortable with fellows and residents, respectively. Twenty-eight percent of respondents report they would prefer future appointments to only be with the providers they are scheduled with and 30.4% had a neutral opinion.
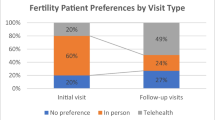
For reliability of the system, 68% of respondents said they believe the telehealth system is the same as in-person visits. Ninety-three percent would use telehealth services again and only 3% said they would not use it again. For follow-up, 61% would prefer telehealth visits over in-person, while 21% had no opinion and 18% would prefer in-person visits.
A post hoc analysis was done to evaluate if there were differences in responses at a higher or lower age than the mean (32.8 years old) and closer or further from the median distance from clinic (24.0 miles). As demonstrated in Fig. 1, there was no significant difference on patient perception of telehealth being the same as in person at ages above and below the mean. When dividing the patients based on median distance from clinic, there was no difference in patient preference for telehealth visits over in person visits (Fig. 2).
Discussion
Overall, our findings suggest patients are satisfied with telehealth, and its implementation has saved our respondents’ time and improved their access to care. There were no differences in respondents who did and did not take the survey except for length of infertility which demonstrates a diverse group. We speculate that those with a longer infertility journey may be less interested in volunteer research surveys or are coming for a second opinion and may have already experienced telehealth visits so did not feel they would add to the survey. Even after post hoc analysis comparing different age groups and geographic distances, patients were still overall satisfied with telehealth.
One consideration is that patients had similar satisfaction rates independent if they lived closer to or further from the median distance from clinic. We believe this demonstrates telehealth having qualities fertility patients might find appealing other than simply obtaining healthcare access and saving time. For example, patients have less commuter stress, more location independence, and can more easily include a significant other in the consultation. Patients, especially those living in rural areas, have more freedom in their visits and flexibility with other responsibilities, such as work or childcare. Also, a concern for telehealth in REI is the lack of establishing good connections to discuss sensitive subjects; however, with telehealth, patients can choose an environment where they feel safe and comfortable instead of an often-unfamiliar office setting. Remote work has been shown to decrease physiological and physical stress responses [12] so telehealth for fertility care stands to better improve mental health during the fertility journey. This is especially important for our population given that Ramezanzadeh et al. demonstrated in a cohort of 370 women undergoing fertility treatment, 86.8% had anxiety and 40.8% had depression [13]. Standardization of telehealth may be one tool used to ameliorate the physical and physiological burden of undergoing fertility care.
This study fulfills an increasing need to describe patient satisfaction of telehealth within the REI field. As part of the ASRM strategic plan for 2014–2019, a focus was on “access to care” because an estimated 39.6% of the US population has limited ART access [14, 15]. Telehealth can facilitate access to care [8]; however, with this survey, we demonstrated an arguably more important point: patients are satisfied with telehealth and preferred it in most cases. Currently 30 states have parity laws which ensure health insurance companies have equivalent reimbursement for in-person and telehealth services. At time of this writing, a temporary PHE is still in place and was renewed April 2022; however, if and when this act is eventually lifted, there is the potential for a back shift in many of the policies that improved telehealth access. For this reason, many societies have supported legislative changes to solidify the use of telehealth in standard medical practice. The American College of Obstetrics and Gynecology (ACOG) has supported telehealth with its release of committee opinions to help guide telehealth implantation [16] and both ACOG and the American Medical Association (AMA) have issued statements advocating to ensure expanded coverage with telehealth continues once the PHE is lifted. Continued support for this expansion is necessary to have adequate coverage and reimbursement by insurance companies so practices can continue to offer patient-centered telehealth services.
The REI field would benefit from expansion of telehealth due to the nature of its practice patterns. A Spanish study demonstrated that telehealth could reduce time to infertility treatment and indirectly increase the number of patients treated in a given time [17]. Because REI patients often need to be in a specific phase of the menstrual cycle for workup, it is beneficial to have a new-patient telehealth visit and then the patient can more efficiently travel to the office in the appropriate phase for workup and testing. Although this study investigates only new patient visits, telehealth is also helpful for follow-up visits which predominately discusses treatment outcomes and next steps which do not need to be in-person. Although some visits will have to be in-person to complete diagnostic workup and exams, visits which do not require these services can be performed by telehealth.
This study does have several limitations. First, surveys were done at a single Midwest institution which may not be generalizable to other geographic regions. Second, all patients are encouraged to have telehealth appointments; however, randomization of telehealth versus in-person visits may better evaluate patient satisfaction. Thirdly, there is risk of bias related to patient surveys including sampling bias, response bias, and order bias. We attempted to alleviate bias by including every new patient and the survey could only be submitted if all questions were answered so there are no missing variables. Finally, telehealth theoretically could provide an opportunity to improve access, comfort, and convenience for non-English speaking patients; however, during the pandemic, this population was less likely to access care and complete telehealth visits [18]. While excluding non-English speakers was a limitation in our study, we note that telehealth could support this population, and this should be an area of future research. The strengths of our study included using a previously validated TUQ survey with addition of questions specific to fertility care which provides unique subject matter. To our knowledge, this is the first study evaluating patient satisfaction with telehealth fertility visits.
Conclusion
Healthcare delivery has dramatically changed due to COVID-19, particularly among those seeking fertility care. Our specialty was already seeing a movement toward increased telehealth utilization but questions lingered about patient satisfaction. Our study addresses these questions about patient satisfaction by demonstrating that most fertility patients were satisfied with telehealth visits. Given there were no differences in satisfaction and access to services between those further than and closer to the median clinic distance, telehealth has qualities patients find appealing besides obtaining access and saved time. Patient satisfaction surveys demonstrate feasibility and non-inferiority of telehealth services for new patient visits. We conclude that telehealth is a valuable and popular tool to provide medical care and reimbursement by insurance companies and its use should continue in the future. Future directions on this subject would include randomizing patients to in-person versus telehealth to better compare satisfaction and adding more centers to increase geographic generalizability.
References
Lustig TA. The role of telehealth in an evolving health care environment. Washington, DC: The National Academies Press; 2012.
Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed E-Health. 2020;26(5):571–3.
Telemedicine Use - Household Pulse Survey - COVID-19 in health care access, telemedicine, and mental Health. National Center of Health Statistics. 2021. Available from: https://www.cdc.gov/nchs/covid19/pulse/telemedicine-use.htm. Accessed 14 Nov 2021
Lee S, Hitt WC. Clinical applications of telemedicine in gynecology and women’s health. Obstet Gynecol Clin North Am. 2020;47(2):259–70.
Kelley AS, Qin Y, Marsh EE, Dupree JM. Disparities in accessing infertility care in the United States: results from the National Health and Nutrition Examination Survey, 2013–16. Fertil Steril. 2019;112(3):562–8.
Bedrick BS, Anderson K, Broughton DE, Hamilton B, Jungheim ES. Factors associated with early in vitro fertilization treatment discontinuation. Fertil Steril. 2019;112(1):105–11.
University of Wisconsin School of Medicine and Public Health. Area Deprivation Index v2.0. Neighborhood Atlas. 2015. Available from: https://www.neighborhoodatlas.medicine.wisc.edu/. Accessed 14 Nov 2021
Alexander VM, Schelble AP, Omurtag KR. Traits of patients seen via telemedicine versus in person for new-patient visits in a fertility practice. F S Rep. 2021;2(2):224–9. https://doi.org/10.1016/J.XFRE.2021.04.001
Parmanto B, Lewis AN Jr, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ). Int J Telerehabilitation. 2016;8(1):3–10.
Schutte JL, McCue MP, Parmanto B, McGonigle J, Handen B, Lewis A, et al. Usability and reliability of a remotely administered adult autism assessment, the autism diagnostic observation schedule (ADOS) module 4. Telemed J E Health. 2015;21(3):176–84. Available from: https://doi.org/10.1089/TMJ.2014.0011
Yu DX, Parmanto B, Dicianno BE, Watzlaf VJ, Seelman KD. Accessibility needs and challenges of a mHealth system for patients with dexterity impairments. Disabil Rehabil Assist Technol. 2017;12(1):56–64. Available from: https://doi.org/10.3109/17483107.2015.1063171
Shimura A, Yokoi K, Ishibashi Y, Akatsuka Y, Inoue T. Remote work decreases psychological and physical stress responses, but full-remote work increases presenteeism. Front Psychol. 2021;12:4190.
Ramezanzadeh F, Aghssa MM, Abedinia N, Zayeri F, Khanafshar N, Shariat M, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(1). Available from: https://doi.org/10.1186/1472-6874-4-9
Harris JA, Menke MN, Haefner JK, Moniz MH, Perumalswami CR. Geographic access to assisted reproductive technology health care in the United States: a population-based cross-sectional study. Fertil Steril. 2017;107(4):1023–7.
Reindollar RH. Surfing the waves of change in reproductive medicine: past, present and future. A presentation of the 2014 ASRM Strategic Plan. Fertil Steril. 2015;103(1):35–8.
ACOG COMMITTEE OPINION Number 798 Presidential Task Force on Telehealth Implementing Telehealth in Practice. The American College of Obstetricians and Gynecologists. 2020;135:73–9. Available from: https://doi.org/10.1097/AOG.0000000000003672
Hernández C, Valdera CJ, Cordero J, López E, Plaza J, Albi M. Impact of telemedicine on assisted reproduction treatment in the public health system. J Healthcare Qual Res. 2020;35(1):27–34.
Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Network Open. 2020;3(12):e2031640–e2031640. Available from: https://doi.org/10.1001/JAMANETWORKOPEN.2020.31640
Funding
Grant support: Supported by Clinical and Translational Science Award (CTSA) Grant (UL1 TR000448) and Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant (P30 CA091842). This grant supports Washington University’s use of the redcap data management system which was used for survey distribution and data collection in this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Anderson, K., Coskun, R., Jimenez, P. et al. Satisfaction with new patient telehealth visits for reproductive endocrinology patients in the era of COVID-19. J Assist Reprod Genet 39, 1571–1576 (2022). https://doi.org/10.1007/s10815-022-02539-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02539-4