Abstract
Purpose
The use of fertility preservation (FP) techniques has significantly increased in recent years in the assigned female at birth (AFAB) transgender population. Oocyte cryopreservation is the established method for FP, but ovarian tissue cryopreservation may be considered an alternative option, especially during gender-affirming surgery (GAS). The slow freezing (SF) cryopreservation technique is the standard method for human ovarian tissue, but recently, several studies have shown good results with the vitrification (VT) technique. The objective of this study was to compare the effectiveness of VT and SF techniques in ovarian tissue from AFAB transgender people.
Methods
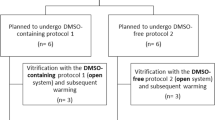
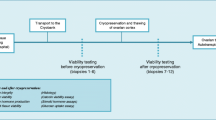
This was a prospective study including 18 AFAB transgender people after GAS. Ovarian tissue pieces from each ovary were cryopreserved by SF and VT and compared with fresh tissue. Study by light microscopy (LM) assessed follicular morphology and density. The percentage of surviving and degenerated follicles was studied with the tissue viability test. Oocytes, granulosa cells and stroma were analysed separately by transmission electron microscopy.
Results
The VT technique preserves follicle and stromal tissue as well as the SF method, but with some differences. Evaluation by LM showed better follicle preservation with VT, but the ultrastructural study showed the presence of minor damage with both techniques compared to fresh tissue.
Conclusion
Both cryopreservation techniques are accurate for maintaining the follicular population and stromal tissue. Further studies are needed to determine the impact of VT on ovarian tissue and the subsequent follicular activation mechanisms in AFAB ovarian tissue.








Similar content being viewed by others
References
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T'Sjoen GG. Endocrine treatment of gender-dysphoric/ gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(11):3869–903. https://doi.org/10.1210/jc.2017-01658.
Auer MK, Fuss J, Nieder TO, Briken P, Biedermann SV, Stalla GK, Beckmann MW, Hildebrandt T. Desire to have children among transgender people in Germany: a cross-sectional multi-center study. J Sex Med. 2018;15(5):757–67. https://doi.org/10.1016/j.jsxm.2018.03.083.
Neblett MF, Hipp HS. Fertility considerations in transgender persons. Endocrinol Metab Clin N Am. 2019;48(2):391–402. https://doi.org/10.1016/j.ecl.2019.02.003.
ESHRE Guideline Group on Female Fertility Preservation, Anderson RA, Amant F, Braat D, D’Angelo A, Chuva de Sousa Lopes SM, Demeestere I, Dwek S, Frith L, Lambertini M, Maslin C, Moura-Ramos M, Nogueira D, Rodriguez-Wallberg K, Vermeulen N. ESHRE guideline: female fertility preservation. Hum Reprod Open. 2020;2020(4):hoaa052. https://doi.org/10.1093/hropen/hoaa052.
Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022–33. https://doi.org/10.1016/j.fertnstert.2019.09.013.
Donnez J, Dolmans MM. Fertility preservation in women. N Engl J Med. 2017;377(17):1657–65. https://doi.org/10.1056/nejmra1614676.
Suzuki N, Yoshioka N, Takae S, Sugishita Y, Tamura M, Hashimoto S, Morimoto Y, Kawamura K. Successful fertility preservation following ovarian tissue vitrification in patients with primary ovarian insufficiency. Hum Reprod. 2015;30(3):608–15. https://doi.org/10.1093/humrep/deu353.
Nakano MS, Simoes RS, Baracat MCP, Lobel A, Shiroma ME, Igami DZ, Serafini PC, Soares JM Jr, Baracat EC. Live birth rate after ovarian tissue cryopreservation followed by autotransplantation in cancer patients: a systematic review. Gynecological and Reproductive. Endocrinol Metab. 2020;1(2):89–94.
Rodriguez-Wallberg KA, Oktay K. Recent advances in oocyte and ovarian tissue cryopreservation and transplantation. Best Pract Res Clin Obstet Gynaecol. 2012;26(3):391–405. https://doi.org/10.1016/j.bpobgyn.2012.01.001.
Devi L, Goel S. Fertility preservation through gonadal cryopreservation. Reprod Med Biol. 2016;15(4):235–51. https://doi.org/10.1007/s12522-016-0240-1.
Ikeda K, Baba T, Noguchi H, Nagasawa K, Endo T, Kiya T, Saito T. Excessive androgen exposure in female-to-male transsexual persons of reproductive age induces hyperplasia of the ovarian cortex and stroma but not polycystic ovary morphology. Hum Reprod. 2013;28(2):453–61. https://doi.org/10.1093/humrep/des385.
De Roo C, Lierman S, Tilleman K, Peynshaert K, Braeckmans K, Caanen M, Lambalk CB, Weyers S, T'Sjoen G, Cornelissen R, De Sutter P. Ovarian tissue cryopreservation in female-to-male transgender people: insights into ovarian histology and physiology after prolonged androgen treatment. Reprod BioMed Online. 2017;34(6):557–66. https://doi.org/10.1016/j.rbmo.2017.03.008.
Borrás A, Manau MD, Fabregues F, Casals G, Saco A, Halperin I, Mora M, Goday A, Barral Y, Carmona F. Endocrinological and ovarian histological investigations in assigned female at birth transgender people undergoing testosterone therapy. Reprod BioMed Online. 2021;43(2):289–97. https://doi.org/10.1016/j.rbmo.2021.05.010.
Rivas Leonel EC, Lucci CM, Amorim CA. Cryopreservation of human ovarian tissue: a review. Transfus Med Hemother. 2019;46(3):173–81. https://doi.org/10.1159/000499054.
Fabbri R, Venturoli S, Errico AD, Iannascoli C, Gabusi E, Valeri B, Seracchioli R, Grigioni WF. Ovarian tissue banking and fertility preservation in cancer patients : histological and immunohistochemical evaluation. Gynecol Oncol. 2003;89:259–66. https://doi.org/10.1016/S0090-8258(02)00098-7.
Kagawa N, Silber S, Kuwayama M. Successful vitrification of bovine and human ovarian tissue. Reprod BioMed Online. 2009;18(4):568–77. https://doi.org/10.1016/S1472-6483(10)60136-8.
Isachenko V, Lapidus I, Isachenko E, Krivokharchenko A, Kreienberg R, Woriedh M, Bader M, Weiss JM. Human ovarian tissue vitrification versus conventional freezing: morphological, endocrinological, and molecular biological evaluation. Reproduction. 2009. https://doi.org/10.1530/REP-09-0039.
Hreinsson J, Zhang P, Swahn ML, Hultenby K, Hovatta O. Cryopreservation of follicles in human ovarian cortical tissue. Comparison of serum and human serum albumin in the cryoprotectant solutions. Hum Reprod. 2003;18(11):2420–8. https://doi.org/10.1093/humrep/deg439.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
Ethics Committee of the American Society for Reproductive Medicine. Access to fertility services by transgender persons: an ethics committee opinion. Fertil Steril. 2015;104(5):1111–5. https://doi.org/10.1016/j.fertnstert.2015.08.021.
Shumer DE, Nokoff NJ, Spack NP. Advances in the care of transgender children and adolescents. Adv Pediatr Infect Dis. 2016;63(1):79–102. https://doi.org/10.1016/j.yapd.2016.04.018.
Tornello SL, Bos H. Parenting intentions among transgender individuals. LGBT Health. 2017;4(2):115–20. https://doi.org/10.1089/lgbt.2016.0153.
Wierckx K, Van Caenegem E, Pennings G, Elaut E, Dedecker D, Van de Peer F, Weyers S, De Sutter P, T'Sjoen G. Reproductive wish in transsexual men. Hum Reprod. 2012;27(2):483–7. https://doi.org/10.1093/humrep/der406.
Baram S, Myers SA, Yee S, Librach CL. Fertility preservation for transgender adolescents and young adults: a systematic review. Hum Reprod Update. 2019;25(6):694–716. https://doi.org/10.1093/humupd/dmz026.
Wierckx K, Stuyver I, Weyers S, Hamada A, Agarwal A, De Sutter P, T'Sjoen G. Sperm freezing in transsexual women. Arch Sex Behav. 2012;41(5):1069–71. https://doi.org/10.1007/s10508-012-0012-x.
Stöbel-Richter Y, Beutel ME, Finck C, Brähler E. The 'wish to have a child', childlessness and infertility in Germany. Hum Reprod. 2005;20(10):2850–7. https://doi.org/10.1093/humrep/dei121.
De Roo C, Tilleman K, T'Sjoen G, De Sutter P. Fertility options in transgender people. Int Rev Psychiatry. 2016;28(1):112–9. https://doi.org/10.3109/09540261.2015.1084275.
Light AD, Obedin-Maliver J, Sevelius JM, Kerns JL. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014;124(6):1120–7. https://doi.org/10.1097/AOG.0000000000000540.
Adeleye AJ, Cedars MI, Smith J, Mok-Lin E. Ovarian stimulation for fertility preservation or family building in a cohort of transgender men. J Assist Reprod Genet. 2019;36(10):2155–61. https://doi.org/10.1007/s10815-019-01558-y.
Amir H, Oren A, Klochendler Frishman E, Sapir O, Shufaro Y, Segev Becker A, Azem F, Ben-Haroush A. Oocyte retrieval outcomes among adolescent transgender males. J Assist Reprod Genet. 2020;37(7):1737–44. https://doi.org/10.1007/s10815-020-01815-5.
Amir H, Yaish I, Samara N, Hasson J, Groutz A, Azem F. Ovarian stimulation outcomes among transgender men compared with fertile cisgender women. J Assist Reprod Genet. 2020;37(10):2463–72. https://doi.org/10.1007/s10815-020-01902-7.
Leung A, Sakkas D, Pang S, Thornton K, Resetkova N. ART outcomes in female to male transgender patients: a new frontier in reproductive medicine. Fertil Steril. 2018;109(3):e35. https://doi.org/10.1016/j.fertnstert.2018.02.068.
Mattawanon N, Spencer JB, Schirmer DA, Tangpricha V. Fertility preservation options in transgender people: a review. Rev Endocr Metab Disord. 2018;19(3):231–42. https://doi.org/10.1007/s11154-018-9462-3.
Armuand G, Dhejne C, Olofsson JI, Rodriguez-Wallberg KA. Transgender men’s experiences of fertility preservation: a qualitative study. Hum Reprod. 2017;32(2):383–90. https://doi.org/10.1093/humrep/dew323.
Gandolfi F, Paffoni A, Papasso Brambilla E, Bonetti S, Brevini TAL, Ragni G. Efficiency of equilibrium cooling and vitrification procedures for the cryopreservation of ovarian tissue: comparative analysis between human and animal models. Fertil Steril. 2006;85(SUPPL. 1):1150–6. https://doi.org/10.1016/j.fertnstert.2005.08.062.
Keros V, Xella S, Hultenby K, Pettersson K, Sheikhi M, Volpe A, Hreinsson J, Hovatta O. Vitrification versus controlled-rate freezing in cryopreservation of human ovarian tissue. Hum Reprod. 2009;24(7):1670–83. https://doi.org/10.1093/humrep/dep079.
Shah JS, Sabouni R, Cayton Vaught KC, Owen CM, Albertini DF, Segars JH. Biomechanics and mechanical signaling in the ovary: a systematic review. J Assist Reprod Genet. 2018;35(7):1135–48. https://doi.org/10.1007/s10815-018-1180-y.
Shi Q, Xie Y, Wang Y, Li S. Vitrification versus slow freezing for human ovarian tissue cryopreservation: a systematic review and meta-anlaysis. Sci Rep. 2017;7(1):1–9. https://doi.org/10.1038/s41598-017-09005-7.
Shams Mofarahe Z, Ghaffari Novin M, Jafarabadi M, Salehnia M, Noroozian M, Ghorbanmehr N. Effect of human ovarian tissue vitrification/warming on the expression of genes related to folliculogenesis. Iran Biomed J. 2015;19(4):220–5. https://doi.org/10.7508/ibj.2015.04.005.
Fabbri R, Vicenti R, Macciocca M, Pasquinelli G, Paradisi R, Battaglia C, Martino NA, Venturoli S. Good preservation of stromal cells and no apoptosis in human ovarian tissue after vitrification. Biomed Res Int. 2014;2014:673537. https://doi.org/10.1155/2014/673537.
Bin Li Y, Zhou CQ, Yang QF, Wang Q, Dong Y. Modified vitrification method for cryopreservation of human ovarian tissues. Chin Med J. 2007;120(2):110–4. https://doi.org/10.1097/00029330-200701020-00007.
Rahimi G, Isachenko V, Kreienberg R, Sauer H, Todorov P, Tawadros S, Mallmann P, Nawroth F, Isachenko E. Re-vascularisation in human ovarian tissue after conventional freezing or vitrification and xenotransplantation. Eur J Obstet Gynecol Reprod Biol. 2010;149(1):63–7. https://doi.org/10.1016/j.ejogrb.2009.11.015.
Amorim CA, Dolmans MM, David A, Jaeger J, Vanacker J, Camboni A, Donnez J, Van Langendonckt A. Vitrification and xenografting of human ovarian tissue. Fertil Steril. 2012 Nov;98(5):1291–8.e1-2. https://doi.org/10.1016/j.fertnstert.2012.07.1109.
Isachenko V, Isachenko E, Reinsberg J, Montag M, van der Ven K, Dorn C, Roesing B, van der Ven H. Cryopreservation of human ovarian tissue: comparison of rapid and conventional freezing. Cryobiology. 2007;55(3):261–8. https://doi.org/10.1016/j.cryobiol.2007.08.008.
Oktem O, Alper E, Balaban B, Palaoglu E, Peker K, Karakaya C, Urman B. Vitrified human ovaries have fewer primordial follicles and produce less antimüllerian hormone than slow-frozen ovaries. Fertil Steril. 2011;95(8):2661–4.e1. https://doi.org/10.1016/j.fertnstert.2010.12.057.
Terren C, Fransolet M, Ancion M, Nisolle M, Munaut C. Slow freezing versus vitrification of mouse ovaries: from ex vivo analyses to successful pregnancies after auto-transplantation. Sci Rep. 2019;9(1):1–13. https://doi.org/10.1038/s41598-019-56182-8.
Lee S, Ryu KJ, Kim B, Kang D, Kim YY, Kim T. Comparison between slow freezing and vitrification for human ovarian tissue cryopreservation and xenotransplantation. Int J Mol Sci. 2019;20(13):3346. https://doi.org/10.3390/ijms20133346.
Sanfilippo S, Canis M, Smitz J, Sion B, Darcha C, Janny L, Brugnon F. Vitrification of human ovarian tissue: a practical and relevant alternative to slow freezing. Reprod Biol Endocrinol. 2015;13(1):1–7. https://doi.org/10.1186/s12958-015-0065-5.
Dolmans MM, Cordier F, Amorim CA, Donnez J, Vander LC. In vitro activation prior to transplantation of human ovarian tissue: is it truly effective? Front Endocrinol (Lausanne). 2019;10(August):1–9. https://doi.org/10.3389/fendo.2019.00520.
Fabbri R, Vicenti R, Macciocca M, Martino NA, Dell'Aquila ME, Pasquinelli G, Morselli-Labate AM, Seracchioli R, Paradisi R. Morphological, ultrastructural and functional imaging of frozen/thawed and vitrified/warmed human ovarian tissue retrieved from oncological patients. Hum Reprod. 2016;31(8):1838–49. https://doi.org/10.1093/humrep/dew134.
Herraiz S, Novella-Maestre E, Rodríguez B, Díaz C, Sánchez-Serrano M, Mirabet V, Pellicer A. Improving ovarian tissue cryopreservation for oncologic patients: slow freezing versus vitrification, effect of different procedures and devices. Fertil Steril. 2014;101(3):775–84. https://doi.org/10.1016/j.fertnstert.2013.11.016.
Silber S, Kagawa N, Kuwayama M, Gosden R. Duration of fertility after fresh and frozen ovary transplantation. Fertil Steril. 2010;94(6):2191–6. https://doi.org/10.1016/j.fertnstert.2009.12.073.
Kikuchi I, Kagawa N, Silber S, Kuwayama M, Takehara Y, Aono F, Kumakiri J, Kato O, Takeda S. Oophorectomy for fertility preservation via reduced-port laparoscopic surgery. Surg Innov. 2013;20(3):219–24. https://doi.org/10.1177/1553350612449074.
Chadha S, Pache TD, Huikeshoven JM, Brinkmann AO, van der Kwast TH. Androgen receptor expression in human ovarian and uterine tissue of long-term androgen-treated transsexual women. Hum Pathol. 1994;25(11):1198–204. https://doi.org/10.1016/0046-8177(94)90037-x.
Dunaif A, Scully RE, Andersen RN, Chapin DS, Crowley WF. The effects of continuous androgen secretion on the hypothalamic-pituitary axis in woman: evidence from a luteinized thecoma of the ovary. J Clin Endocrinol Metab. 1984;59(3):389–93. https://doi.org/10.1210/jcem-59-3-389.
Pache TD, Chadha S, Gooren LJ, Hop WC, Jaarsma KW, Dommerholt HB, Fauser BC. Ovarian morphology in long-term androgen-treated female to male transsexuals. A human model for the study of polycystic ovarian syndrome? Histopathology. 1991;19(5):445–52. https://doi.org/10.1111/j.1365-2559.1991.tb00235.x.
Spinder T, Spijkstra JJ, van den Tweel JG, Burger CW, van Kessel H, Hompes PG, Gooren LJ. The effects of long term testosterone administration on pulsatile luteinizing hormone secretion and on ovarian histology in eugonadal female to male transsexual subjects. J Clin Endocrinol Metab. 1989;69(1):151–7. https://doi.org/10.1210/jcem-69-1-151.
Hughesdon PE. Morphology and morphogenesis of the Stein-Leventhal ovary and of so-called "hyperthecosis". Obstet Gynecol Surv. 1982;37(2):59–77. https://doi.org/10.1097/00006254-198202000-00001.
Grynberg M, Fanchin R, Dubost G, Colau JC, Brémont-Weil C, Frydman R, Ayoubi JM. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod BioMed Online. 2010;20(4):553–8. https://doi.org/10.1016/j.rbmo.2009.12.021.
Loverro G, Resta L, Dellino M, Edoardo DN, Cascarano MA, Loverro M, Mastrolia SA. Uterine and ovarian changes during testosterone administration in young female-to-male transsexuals. Taiwan J Obstet Gynecol. 2016;55(5):686–91. https://doi.org/10.1016/j.tjog.2016.03.004.
Sterling J, Garcia MM. Fertility preservation options for transgender individuals. Transl Androl Urol. 2020;9(Suppl 2):S215–26. https://doi.org/10.21037/tau.2019.09.28.
Lierman S, Tilleman K, Braeckmans K, Peynshaert K, Weyer S. Fertility preservation for trans men : frozen-thawed in vitro matured oocytes collected at the time of ovarian tissue processing exhibit normal meiotic spindles. J Assist Reprod Genet. 2017;34(11):1449–56. https://doi.org/10.1007/s10815-017-0976-5.
De Roo C, Lierman S, Tilleman DS, P. In-vitro fragmentation of ovarian tissue activates primordial follicles through the Hippo pathway. Hum Reprod Open. 2020;2020(4):1–16. https://doi.org/10.1093/hropen/hoaa048.
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. In vitro maturation: a committee opinion. Fertil Steril. 2013;99(3):663–6. https://doi.org/10.1016/j.fertnstert.2012.12.031.
Telfer EE, Zelinsk MB. Ovarian follicle culture: advances and challenges for human and non-human primates. Fertil Steril. 2013;29(6):997–1003. https://doi.org/10.1016/j.fertnstert.2013.03.043.Ovarian.
Pavone ME, Hirshfeld-Cytron J, Tingen C, Thomas C, Thomas J, Lowe MP, Schink JC, Woodruff TK. Human ovarian tissue cortex surrounding benign and malignant lesions. Reprod Sci. 2014;21(5):582–9. https://doi.org/10.1177/1933719113506498.
Further reading
Committee Opinion No685. care for transgender adolescents. Obstet Gynecol. 2017;129(1):e11–6. https://doi.org/10.1097/AOG.0000000000001861.
Klocke S, Bündgen N, Köster F, Eichenlaub-Ritter U, Griesinger G. Slow-freezing versus vitrification for human ovarian tissue cryopreservation. Arch Gynecol Obstet. 2015;291(2):419–26. https://doi.org/10.1007/s00404-014-3390-6.
Funding
This study was supported by the grant “Premi Fi de Residencia Emili Letang 2011” from the Hospital Clinic of Barcelona and the grant “Fundación Dexeus Salud de la Mujer” in 2013–2015.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Josep Maria Calafell, Adela Saco and Aina Borrás. Data collection and analysis were performed by Aina Borrás, Inés Agustí, Sara Peralta and Gemms Casals. The original draft preparation was performed by Aina Borrás. The study supervision was performed by Dolors Manau, Francesc Fabregues and Francisco Carmona. All authors commented on previous versions of the manuscript and approved the final version of article submitted.
Corresponding author
Ethics declarations
It was conducted according to the Declaration of Helsinki for Medical Research involving Human Subjects [19]. The study protocol was approved by the Ethics Committee of the Hospital Clinic of Barcelona (registry number 2011/6272) in 2011. All subjects provided written, informed consent to participate in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borrás, A., Manau, D., Fabregues, F. et al. Comparison between slow freezing and vitrification of ovarian tissue cryopreservation in assigned female at birth transgender people receiving testosterone therapy: data on histological and viability parameters. J Assist Reprod Genet 39, 527–541 (2022). https://doi.org/10.1007/s10815-021-02386-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02386-9