Abstract
Purpose
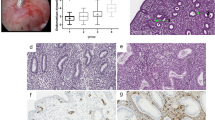
Treatment of Asherman syndrome (AS) presents a significant clinical challenge. Based on our in vitro data showing that PRP could activate endometrial cell proliferation and migration, we hypothesized that intrauterine infusion of autologous platelet-rich plasma (PRP) may improve endometrial regeneration and fertility outcomes in patients with moderate-severe AS.
Materials and methods
Subjects with moderate-severe AS were randomized to PRP or saline control administered following hysteroscopic adhesiolysis. Due to relative inability to randomize patients to the control group, after initial randomization of 10 subjects (6 in PRP and 4 in control groups), the remainder were prospectively enrolled in PRP group (n = 9), with 11 historic controls added to control group, for a total of 30 subjects (PRP n = 15; saline control n = 15). Right after hysteroscopy, 0.5–1 mL of PRP or saline was infused into the uterus via a Wallace catheter, followed by estrogen therapy. The primary outcomes were changes in endometrial thickness (EMT, checked in 3 weeks) and in menstrual flow; secondary outcomes were pregnancy and live birth rates. EMT and menstrual bleeding pattern were assessed before and after the intervention. Pregnancy was assessed over a 6-month period.
Results
There were no statistically significant differences in age, gravidity/parity, cause of AS, preoperative menses assessment, AS hysteroscopy score, and intrauterine balloon placement between the groups. There was no statistically significant difference (p = 0.79) in EMT pre-PRP infusion for control (5.7 mm, 4.0–6.0) and study arm (5.3 mm, 4.9–6.0). There was no statistically significant change (p = 0.78) in EMT after PRP infusion (1.4 mm, − 0.5–2.4) vs saline (1.0 mm, 0.0–2.5). Patients tolerated the procedure well, with no adverse effects. There was no difference in the predicted likelihood of pregnancy (p = 0.45) between the control (0.67, 0.41–0.85) and study arm (0.53, 0.29–0.76).
Conclusions
PRP was well accepted and tolerated in AS patients. However, we did not observe any significant EMT increase or improved pregnancy rates after adding PRP infusion, compared to standard treatment only. The use of intrauterine PRP infusion may be a feasible option, and its potential use must be tested on a larger sample size of AS patients.

Similar content being viewed by others
References
Asherman JG. Amenorrhoea traumatica (atretica). J Obstet Gynaecol Br Emp. 1948;11:23–30. https://doi.org/10.1111/j.1471-0528.1948.tb07045.x.
Dmowski WP, Greenblatt RB. Asherman’s syndrome and risk of placenta accreta. Obstet Gynecol. 1969;34(2):288–99.
March CM. Asherman’s syndrome. Semin Reprod Med. 2011;29(2):83–94. https://doi.org/10.1055/s-0031-1272470.
Hanstede MM, van der Meij E, Goedemans L, Emanuel MH. Results of centralized Asherman surgery, 2003–2013. Fertil Steril. 2015;104(6):1561-8 e1. https://doi.org/10.1016/j.fertnstert.2015.08.039.
The American Fertility Society classifications of adnexal adhesions. distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril. 1988;49:944–55. https://doi.org/10.1016/s0015-0282(16)59942-7.
Gargett CE, Masuda H. Adult stem cells in the endometrium. Mol Hum Reprod. 2010;16(11):818–34. https://doi.org/10.1093/molehr/gaq061.
Salazar CA, Isaacson K, Morris S. A comprehensive review of Asherman’s syndrome: causes, symptoms and treatment options. Curr Opin Obstet Gynecol. 2017;29(4):249–56. https://doi.org/10.1097/GCO.0000000000000378.
Santamaria X, Liu JH, Aghajanova L, Isaacson K, Movilla P, Fernandez H, Capmas P, Donnez J, Simon C. Should we consider alternative therapies to operative hysteroscopy for the treatment of Asherman syndrome? Fertil Steril. 2020;113(3):511–21. https://doi.org/10.1016/j.fertnstert.2020.01.022.
Schenker JG. Etiology of and therapeutic approach to synechia uteri. Eur J Obstet Gynecol Reprod Biol. 1996;65(1):109–13.
Fernandez H, Al-Najjar F, Chauveaud-Lambling A, Frydman R, Gervaise A. Fertility after treatment of Asherman’s syndrome stage 3 and 4. J Minim Invasive Gynecol. 2006;13(5):398–402. https://doi.org/10.1016/j.jmig.2006.04.013.
Pabuccu R, Atay V, Orhon E, Urman B, Ergun A. Hysteroscopic treatment of intrauterine adhesions is safe and effective in the restoration of normal menstruation and fertility. Fertil Steril. 1997;68(6):1141–3.
Fedele L, Bianchi S, Frontino G. Septums and synechiae: approaches to surgical correction. Clin Obstet Gynecol. 2006;49(4):767–88. https://doi.org/10.1097/01.grf.0000211948.36465.a6.
Xiao S, Wan Y, Xue M, Zeng X, Xiao F, Xu D, Yang X, Zhang P, Sheng W, Xu J, Zhou S. Etiology, treatment, and reproductive prognosis of women with moderate-to-severe intrauterine adhesions. Int J Gynaecol Obstet. 2014;125(2):121–4. https://doi.org/10.1016/j.ijgo.2013.10.026.
Valle RF, Sciarra JJ. Intrauterine adhesions: hysteroscopic diagnosis, classification, treatment, and reproductive outcome. Am J Obstet Gynecol. 1988;158(6 Pt 1):1459–70. https://doi.org/10.1016/0002-9378(88)90382-1.
Yu D, Li TC, Xia E, Huang X, Liu Y, Peng X. Factors affecting reproductive outcome of hysteroscopic adhesiolysis for Asherman’s syndrome. Fertil Steril. 2008;89(3):715–22. https://doi.org/10.1016/j.fertnstert.2007.03.070.
Lin XN, Zhou F, Wei ML, Yang Y, Li Y, Li TC, Zhang SY. Randomized, controlled trial comparing the efficacy of intrauterine balloon and intrauterine contraceptive device in the prevention of adhesion reformation after hysteroscopic adhesiolysis. Fertil Steril. 2015;104(1):235–40. https://doi.org/10.1016/j.fertnstert.2015.04.008.
Amer MI, Abd-El-Maeboud KH, Abdelfatah I, Salama FA, Abdallah AS. Human amnion as a temporary biologic barrier after hysteroscopic lysis of severe intrauterine adhesions: pilot study. J Minim Invasive Gynecol. 2010;17(5):605–11. https://doi.org/10.1016/j.jmig.2010.03.019.
Tsapanos VS, Stathopoulou LP, Papathanassopoulou VS, Tzingounis VA. The role of Seprafilm bioresorbable membrane in the prevention and therapy of endometrial synechiae. J Biomed Mater Res. 2002;63(1):10–4.
Hooker AB, de Leeuw R, van de Ven PM, Bakkum EA, Thurkow AL, Vogel NEA, van Vliet H, Bongers MY, Emanuel MH, Verdonkschot AEM, Brolmann HAM, Huirne JAF. Prevalence of intrauterine adhesions after the application of hyaluronic acid gel after dilatation and curettage in women with at least one previous curettage: short-term outcomes of a multicenter, prospective randomized controlled trial. Fertil Steril. 2017;107(5):1223-31 e3. https://doi.org/10.1016/j.fertnstert.2017.02.113.
Acunzo G, Guida M, Pellicano M, Tommaselli GA, Di Spiezio SA, Bifulco G, Cirillo D, Taylor A, Nappi C. Effectiveness of auto-cross-linked hyaluronic acid gel in the prevention of intrauterine adhesions after hysteroscopic adhesiolysis: a prospective, randomized, controlled study. Hum Reprod. 2003;18(9):1918–21.
Johary J, Xue M, Zhu X, Xu D, Velu PP. Efficacy of estrogen therapy in patients with intrauterine adhesions: systematic review. J Minim Invasive Gynecol. 2014;21(1):44–54. https://doi.org/10.1016/j.jmig.2013.07.018.
Guo J, Li TC, Liu Y, Xia E, Xiao Y, Zhou F, Yang X. A prospective, randomized, controlled trial comparing two doses of oestrogen therapy after hysteroscopic adhesiolysis to prevent intrauterine adhesion recurrence. Reprod Biomed Online. 2017;35(5):555–61. https://doi.org/10.1016/j.rbmo.2017.07.011.
Santamaria X, Cabanillas S, Cervello I, Arbona C, Raga F, Ferro J, Palmero J, Remohi J, Pellicer A, Simon C. Autologous cell therapy with CD133+ bone marrow-derived stem cells for refractory Asherman’s syndrome and endometrial atrophy: a pilot cohort study. Hum Reprod. 2016;31(5):1087–96. https://doi.org/10.1093/humrep/dew042.
Nagori CB, Panchal SY, Patel H. Endometrial regeneration using autologous adult stem cells followed by conception by in vitro fertilization in a patient of severe Asherman’s syndrome. J Hum Reprod Sci. 2011;4(1):43–8. https://doi.org/10.4103/0974-1208.82360.
Etulain J. Platelets in wound healing and regenerative medicine. Platelets. 2018;29(6):556–68. https://doi.org/10.1080/09537104.2018.1430357.
Alves R, Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord. 2018;4(1):18–24. https://doi.org/10.1159/000477353.
Nurden AT. Platelets, inflammation and tissue regeneration. Thromb Haemost. 2011;105(Suppl 1):S13-33. https://doi.org/10.1160/THS10-11-0720.
Stellos K, Kopf S, Paul A, Marquardt JU, Gawaz M, Huard J, Langer HF. Platelets in regeneration. Semin Thromb Hemost. 2010;36(2):175–84. https://doi.org/10.1055/s-0030-1251502.
Gawaz M, Vogel S. Platelets in tissue repair: control of apoptosis and interactions with regenerative cells. Blood. 2013;122(15):2550–4. https://doi.org/10.1182/blood-2013-05-468694.
Aghajanova L, Houshdaran S, Balayan S, Manvelyan E, Irwin JC, Huddleston HG, Giudice LC. In vitro evidence that platelet-rich plasma stimulates cellular processes involved in endometrial regeneration. J Assist Reprod Genet. 2018;35(5):757–70. https://doi.org/10.1007/s10815-018-1130-8.
Kim JH, Park M, Paek JY, Lee WS, Song H, Lyu SW. Intrauterine infusion of human platelet-rich plasma improves endometrial regeneration and pregnancy outcomes in a murine model of Asherman’s syndrome. Front Physiol. 2020;11:105. https://doi.org/10.3389/fphys.2020.00105.
Aghajanova L, Cedars MI, Huddleston HG. Platelet-rich plasma in the management of Asherman syndrome: case report. J Assist Reprod Genet. 2018;35(5):771–5. https://doi.org/10.1007/s10815-018-1135-3.
Chang Y, Li J, Chen Y, Wei L, Yang X, Shi Y, Liang X. Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med. 2015;8(1):1286–90.
Zadehmodarres S, Salehpour S, Saharkhiz N, Nazari L. Treatment of thin endometrium with autologous platelet-rich plasma: a pilot study. JBRA Assist Reprod. 2017;21(1):54–6. https://doi.org/10.5935/1518-0557.20170013.
Nazari L, Salehpour S, Hoseini S, Zadehmodarres S, Azargashb E. Effects of autologous platelet-rich plasma on endometrial expansion in patients undergoing frozen-thawed embryo transfer: a double-blind RCT. Int J Reprod Biomed (Yazd). 2019;17(6):443–8. https://doi.org/10.18502/ijrm.v17i6.4816.
Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2005;4:287–91.
Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–91. https://doi.org/10.1002/nur.20247.
Higham JM, O’Brien PM, Shaw RW. Assessment of menstrual blood loss using a pictorial chart. Br J Obstet Gynaecol. 1990;97(8):734–9. https://doi.org/10.1111/j.1471-0528.1990.tb16249.x.
Graham RA, Davis JA, Corrales-Medina FF. The adolescent with menorrhagia: diagnostic approach to a suspected bleeding disorder. Pediatr Rev. 2018;39(12):588–600. https://doi.org/10.1542/pir.2017-0105.
Guo EJ, Chung JPW, Poon LCY, Li TC. Reproductive outcomes after surgical treatment of asherman syndrome: a systematic review. Best Pract Res Clin Obstet Gynaecol. 2019;59:98–114. https://doi.org/10.1016/j.bpobgyn.2018.12.009.
Benor A, Gay S, DeCherney A. An update on stem cell therapy for Asherman syndrome. J Assist Reprod Genet. 2020;37(7):1511–29. https://doi.org/10.1007/s10815-020-01801-x.
Gao L, Huang Z, Lin H, Tian Y, Li P, Lin S. Bone marrow mesenchymal stem cells (BMSCs) restore functional endometrium in the rat model for severe Asherman syndrome. Reprod Sci. 2019;26(3):436–44. https://doi.org/10.1177/1933719118799201.
Funding
PRP kits were donated to the study by Isto Biologics, Hopkinton, MA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aghajanova, L., Sundaram, V., Kao, CN. et al. Autologous platelet-rich plasma treatment for moderate-severe Asherman syndrome: the first experience. J Assist Reprod Genet 38, 2955–2963 (2021). https://doi.org/10.1007/s10815-021-02328-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02328-5