Abstract
Clinical anxiety is a common comorbidity in autistic people. Due to the prevalence of anxiety in the autism population and the adverse effects it causes, there is a critical need to develop effective interventions which address anxiety symptoms for autistic people. Therefore, the purpose of this systematic review was to examine the effectiveness of the use of physical activity as an intervention to reduce anxiety in autistic people. Three databases PubMed, PsychInfo, and Cochrane RCTs, were searched utilizing key terms. PRISMA systematic search procedures identified 44 studies meeting predetermined inclusion criteria. Participant characteristics, the type of physical activity performed, the nature of the physical activity program/delivery, anxiety-related outcomes, and research methodology was evaluated for each study. Each paper included was appraised and scored for risk of bias using Cochrane Handbook for Systematic Reviews of Interventions risk of bias tool. Titles and abstracts of 44 articles were reviewed and 8 articles met inclusion criteria which evaluated interventions. Evidence from 8 studies suggests that yoga, a community-based football program, an app-assisted walking program, group exercise programs, and horseback riding interventions reduced anxiety for autistic people. The studies included in this systematic review provide strong-to-moderate evidence that physical activity can reduce anxiety for autistic children and adults. However, additional research is needed to identify which mode of physical activity is most beneficial for anxiety reduction. Further, future research should evaluate frequency, duration, and intensity and their effects on anxiety for autistic people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2023, the Centers for Disease Control and Prevention (CDC) reported 1 in 36 children and 1 in 45 adults in the United States are diagnosed with autism (CDC, 2023). Autism is a neurodevelopmental disorder characterized by persistent deficits in social interaction and communication, as wells as restricted, repetitive patterns of behavior, activities, or interests (American Psychiatric Association, 2013). Autism affects people who are diagnosed differently; learning, thinking, and problem-solving abilities in individuals with autism can range from gifted abilities to severe deficits (CDC, 2023).
According to a caregiver-reported national survey, 40% of autistic children experience anxiety (Kerns et al., 2020), and 20% of autistic adults have been diagnosed with anxiety (Nimmo-Smith et al., 2020). A number of explanations have been developed to explain the increased levels of anxiety for autistic people. First, it is theorized that anxiety may be due to an aversion to situational change or experiencing unfamiliar environments (Gillott et al., 2001; White et al., 2009). Autistic individuals may have difficulty processing unfamiliar and changing environments that lead to feelings of uncertainty (Gillott et al., 2001). Gillott et al. (2001) suggests that stereotypical behaviors like twirling, rocking, or hand flapping, and complex behaviors like repetitive questioning are triggered by anxiety for autistic people. These behaviors are considered a response by the individual to attempt to calm themselves in response to unfamiliar environments (Gillott et al., 2001).
Another proposed theory to describe the relationship between anxiety and autism is the individual’s self-awareness (Gillott et al., 2001). Anxiety in autistic individuals may be mediated by one’s level of self-awareness or self-perceived disability (Gillott et al., 2001). Many autistic people are aware of their difficulties understanding situations and environments and their social disconnectedness (White et al., 2009). The awareness of the impact of autism on their life may be associated with increased anxiety and exacerbate social isolation, awkward social interaction, and avoidance of social situations (Gillott et al., 2001; White et al., 2009). Increased social isolation may also be due to some autistic people’s fear of being inaccurately perceived by the general population, this fear caused by people’s innate desire to be accepted by others (Mitchell et al., 2021). Additionally, the general population may not be able understand autistic individuals due to lack of insight into the culture and minds of autistic people, the combination of these misunderstandings and fears has been referred to as the ‘double empathy’ problem (Mitchell et al., 2021). Autistic people have identified belonging to be a critical component of overall well-being, and this fear of being misunderstood or misperceived combined with the general population’s lack of insight can lead to a detrimental impact on mental health (Mitchell et al., 2021). Behavioral manifestations of anxiety, self-perceived disability, and the double empathy problem may lead to increasing social isolation, creating a cycle of progressively negative effects on the individual’s mental and social health (Gillott et al., 2001; Mitchell et al., 2021; White et al., 2009). Due to the prevalence of anxiety for autistic people and its adverse effects, there is a critical need to develop effective interventions which address anxiety symptoms for autistic people and interrupt the anxiety cycle.
In the general population, two common methods for managing anxiety include medication and psychotherapy. Both methods can produce positive outcomes, such as potentially aiding in the relief of anxiety symptoms, but they also have some notable drawbacks. Medications and therapy can be expensive and difficult to access. Additionally, medication may cause unwanted side effects, including poor concentration, motor incoordination, drowsiness, mental confusion, vertigo, and muscle weakness, which can negatively influence mental health or daily function (Longo & Johnson, 2000). Also, nearly one third of patients do not respond to medication, therapy, or the combination of both (Kandola et al., 2018).
Physical activity has been shown to lower anxiety in the general population by chemically altering the brain, decreasing anxiety sensitivity, increasing self-efficacy, and improving quality of life (DeBoer et al., 2012). Physical activity can aid with regulation of the stress response via the hypothalamic–adrenal axis or glucocorticoid circulation, and it stimulates a broad range of neurogenic processes which promote proper brain functioning, particularly in brain regions that are associated with anxiety and stress (Kandola et al., 2018). According to a study by Broman-Fulks et al. (2004), both high-intensity physical activity and low-intensity physical activity was noted to decrease anxiety sensitivity in the general population. Anxiety sensitivity often causes a person to misinterpret and catastrophize physiological sensations, which can lead to a sense of panic (Broman-Fulks et al., 2004). Physical activity mimics some of the physiological symptoms associated with anxiety such as rapid breathing, sweating, and increased heartbeat, and it is believed that exposure to these physical sensations in a positive, healthy environment can be associated with lower anxiety sensitivity over time (Broman-Fulks et al., 2004). Physical activity can improve self-efficacy and elevate mood by increasing feelings of mastery after completing a goal task (Mikkelsen et al., 2017). Physical activity has been shown to improve quality of life in the general population by supporting weight management, reducing depression and anxiety, promoting better sleep, reducing the risk for more than 25 chronic medical conditions, improving cognitive performance, and improving academic performance (Erickson et al., 2019; Kandola et al., 2018; Warburton & Bredin, 2017).
If physical activity is an affordable and accessible alternative for managing anxiety for the general population, we should investigate if autistic individuals gain the same benefits from physical activity (Broman-Fulks et al., 2004). Intervention strategies designed for autistic individuals who experience anxiety are lacking, and current intervention methods are most often limited to cognitive behavior therapy, self-calming techniques from professionals, and pharmaceutical management (Adams et al., 2019; Trembath et al., 2012). Given the prevalence of anxiety in autistic individuals, there is a need for evidence-based, accessible, and cost-effective interventions to manage anxiety and related symptoms. Therefore, the aim of this systematic review is to review the literature describing the impact physical activity on anxiety symptoms for autistic individuals.
Methods
This systematic review focused on what is the effectiveness of physical activity interventions for relieving anxiety symptoms for autistic people. We utilized Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to guide our methodology (Page et al., 2021). First, we identified our PICO (population, intervention, comparison, outcome) question (Yamada et al., 2019). Then, we performed an exhaustive search on three databases, PsychInfo, Cochrane RCTs, and PUBMED. After the search was completed, we collected and assessed over 1000 articles. The protocol for this systematic review was not registered.
Inclusion and Exclusion Criteria
The search inclusion criteria were as follows: any publish year, any age for participants, any design involving a physical activity intervention, any setting involving physical activity, and any duration of follow up. The studies extracted from the databases (e.g., PsychInfo, Cochrane RCTs, and PUBMED) must meet the criteria set by the PICO question to be included in the review. The population is autistic people, the intervention is physical activity, there is no requirement for a comparison group, and the outcomes are measures of anxiety. The exclusion criteria were if a study did not have the previously stated population, intervention, or outcome.
Search Procedures
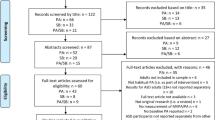
The primary investigator conducted a search in three databases during March of 2023, PsychInfo, Cochrane RCTs, and PUBMED. The search was limited to studies with human subjects and peer-reviewed journals, but publication year was not restricted. We utilized the following “population” key words to search all databases: autism, autism spectrum disorder, developmental disability, “intervention” key words: physical activity, regimen, physical task, training, workout, movement, performance, gym, aerobic, strength, lifting, walking, running, cycling, swimming, and “outcome” key words anxiety symptoms, anxiety sensitivity, anxiety, mood, mood disorders, mental health, anxiety disorder, generalized anxiety disorder, post-traumatic stress disorder, PTSD, separation anxiety, emotions, temperament, and cortisol. We used the advanced search option on the databases to utilize the ‘AND’ feature and search all the combinations of these words, three at a time. The combination would be a “population” key word, an “intervention” key word, and an “outcome” key word (“autism” AND “training” AND “anxiety”). This process was replicated for each of the three databases, PsychInfo, Cochrane RCTs, and PUBMED. We found 2489 studies. After removing duplicates, 1598 studies remained (Fig. 1). Two members of the research team read the abstracts and the titles of all 1598 papers to determine if they met the inclusion and exclusion criteria (Fig. 1).
Record Selection
The following PRISMA criteria were followed: screen based on titles/abstract, multiple, independent reviewers, and report how disagreements were resolved (Brennan & Munn, 2021). After removing duplicates, 1598 papers were included and assessed for the inclusion/exclusion criteria by reading the title and the abstracts by two authors, independently. Conflicts were resolved by a third author, and a consensus discussion of all three reviewers yielded 44 records for full text review. The 44 records underwent full text review using the same inclusion and exclusion criteria as stated in section “Inclusion and Exclusion Criteria”. After reviewing the 44 records, 8 studies met the inclusion and exclusion criteria and are included in this review. After full text review, 36 records were eliminated because they did not include the correct population or outcome measures, they were not a study (book, treatment protocol), or an English version of the article was not available. Eight studies met the inclusion and exclusion criteria and were included in the analysis.
Quality Assessment
The data extracted from the articles by the primary investigator for this systematic review included the authors of the articles, the year of publication of the articles, the levels of evidence, the number of participants, the participants’ ages, the sex of the participants (if reported), inclusion criteria (if reported), exclusion criteria (if reported), intervention procedures, control group procedures (if included), outcome measures, and results. After the primary investigator organized the data for extraction into an evidence table (Table 1), the studies were evaluated for quality, and then evaluated for risk of bias. The quality of evidence for each study was evaluated by examining the levels of evidence for each article using Sackett’s levels of evidence (Sackett, 1989):
-
Level I: Systematic reviews, meta-analyses, randomized controlled trials (RCT).
-
Level II: Two groups, nonrandomized studies (e.g., cohort, case–control).
-
Level III: One group, nonrandomized (e.g., before and after, pretest and posttest).
-
Level IV: Descriptive studies that include analysis of outcomes (single-subject design, case series).
-
Level V: Case reports and expert opinion that include narrative literature reviews and consensus statements.
We have included an evidence table (Table 1) that identifies the authors, the year, level of evidence, participants, inclusion criteria, intervention and control groups, outcome measures, and results. We evaluated the risk of bias using a format adapted from the Cochrane Handbook for Systematic Reviews of Interventions (Green & Higgins, 2023) and the data from that assessment is included in Table 2. In this table the grading criteria were as follows: low risk of bias (+), unclear risk of bias (?), high risk of bias (−) (Table 2). Low risk of bias means the study included a valid approach for allocation, a low dropout rate, actively attempted to prevent bias in measure outcomes and reporting (Shaw et al., 2013). Unclear risk of bias means the study could be susceptible to some bias but not enough to invalidate the results, these may not include appropriate allocation techniques, high drop-out rates, or biases in reporting (Shaw et al., 2013). Finally, high risk of bias means the study may have significant bias that could invalidate the results, this may be due to a combination of lack of allocation techniques, no means to prevent bias, and a high drop-out rate (Shaw et al., 2013). Two authors reviewed the quality of the evidence and the risk of bias independently. Then, the authors discussed their results, and there were no disagreements to resolve. After the primary author gathered and organized the data into the evidence table, each author reviewed the evidence table for accuracy.
Results
The original search of the three databases in March of 2023, resulted in 2489 articles for review. After removing duplicates, 1598 studies remained. Two members of the research team reviewed all abstracts and interrater reliability was moderate agreement (k = 0.66) (McHugh, 2012). The original two reviewers met with a third reviewer to discuss disagreements, 58 total disagreements. Finally, the abstracts that were agreed upon by the original reviewers, as well as the articles the third reviewer chose to include had their full-text reviewed. The number of full-text manuscripts reviewed was 44. Figure 1 presents the PRISMA flow chart for study selection. The eight records that met the criteria for inclusion and are included in this review included two level 1 RCT, three level II non-randomized studies with two groups, and three level III one group non-randomized studies. These studies also included a range of anxiety measures including salivary cortisol levels, the State-Trait Anxiety Inventory (STAI), the Anxiety Scale for Children-ASD (ASC-ASD), the Screen for Child Anxiety Related Disorders (SCARED), the Aberrant Behavior Checklist-Community (ABCC), hair cortisol content (HCC), the Child Behavior Checklist (CBCL) with the Diagnostic Statistical Manual of Mental Disorders-5 (DSM-5) anxiety subscale, the Human–Equips-Interaction on Mental activity scale (HEIM), and the Beck Anxiety Inventory (BAI) (Carey et al., 2022; Gehricke et al., 2022; Hillier et al., 2011; Howells et al., 2020; Keino et al., 2009; Lee et al., 2022; Peters et al., 2021; Tanksale et al., 2021). Results from these studies suggest there is strong evidence that engagement in community organized football programs (Howells et al., 2020; Level II) and yoga programs (Tanksale et al., 2021; Level I RCT) reduces anxiety in autistic children. We conclude that this is strong evidence based on the levels of evidence included, Level II and a Level I. In addition, there is moderate evidence that motor interventions involving horseback riding reduces anxiety in autistic children (Keino et al., 2009; Level III; Peters et al., 2021, Level I RCT). We conclude that this is moderate evidence based on the levels of evidence included, Level III and a Level I. Also, there is moderate evidence to support the use of general physical activity programs to reduce anxiety of autistic adults and children (Carey et al., 2022, Level III; Gehricke et al., 2022; Level II; Hillier et al., 2011, Level III; Lee et al., 2022, Level II). We conclude that this is moderate evidence based on the levels of evidence included, two Level IIIs and two Level IIs. The total sample considered in the resulting studies included 304 total participants, 47 females, 145 males, and gender for 130 participants were not reported (Table 3). Additional sample characteristics are outlined in Table 3.
There is strong evidence suggesting the structured, community organized physical activity program reduces anxiety for autistic individuals (Howells et al., 2020; Tanksale et al., 2021). Howells et al. (2020) performed a study that included 40 autistic children. Nineteen autistic children were assigned to the intervention group because they were participating in a football program at local Auskick clubs, and 21 autistic children were in the comparison group (Howells et al., 2020). Though not involved in the football program, those in the comparison group could participate in their typical routines (Howells et al., 2020). The football program included sessions where children were given the opportunity to practice fundamental motor and football related skills in a group setting (Howells et al., 2020). These sessions occurred for 60–90 min once a week, and participants completed a minimum of 5 sessions (Howells et al., 2020). Parents completed the CBCL which included the DSM-Oriented Anxiety and Depressive Problems, and social functioning and communication were assessed through the Vineland Adaptive Behavior Scale-third edition (Vineland-3) (Howells et al., 2020). Decreases in total problem behaviors, social problems, and internalizing problems as measured by the CBCL were reported post-intervention for the intervention group compared to the control group (Howells et al., 2020). Also, DSM-oriented anxiety problems for the intervention group showed a significant decrease in scores post-intervention compared to the control group (Howells et al., 2020).
One study utilized yoga as an intervention. Tanksale et al. (2021) recruited 61 autistic children, aged 8–12 years, and their parents, 31 completed the intervention and 30 were assigned to the control group and placed on a waitlist for the intervention. The program took place once a week, for 1 h, for 6 weeks, and included breath-centered postures that both the parents and children took part in, games and activities that promoted mindfulness for the children, and parents attended an educational session on how to facilitate home practice (Tanksale et al., 2021). The primary outcomes were measured pre-intervention, post-intervention, and at follow-up (Tanksale et al., 2021). Measures included the parent reported Behavior Rating Inventory of Executive Function (BRIEF), Children’s Sleep Habits Questionnaire (CSHQ), the ASC-ASD parent report, Goal Attainment Scale (GAS), and the child reported Emotion Awareness Questionnaire (EAQ), and the ASC-ASD self-report (Tanksale et al., 2021). According to the post-intervention results for the BRIEF significant group differences were reported for the global executive composite, cognitive regulation index, behavior regulation index, inhibit, and organization of material subscales, suggesting improvements in executive function for the intervention group (Tanksale et al., 2021). According to the post-intervention results for the CSHQ there was a significant difference between groups for bedtime resistance, sleep onset delay, and sleep anxiety, showing improved sleeping habits for children post-intervention (Tanksale et al., 2021). According to the EAQ, there was significant improvement post-intervention for verbal sharing of emotions and analysis of emotions or willingness to understand one’s emotions for the intervention group compared to the control group (Tanksale et al., 2021). According to ASC-ASD—self-report, there was a significant decrease for performance anxiety at the follow-up data collection for the intervention group compared to the control group (Tanksale et al., 2021). There were no other significant results reported (Tanksale et al., 2021).
Moderate evidence supports motor interventions involving horseback riding as a means to reduce anxiety in autistic children (Keino et al., 2009; Peters et al., 2021). Keino et al. (2009) performed a study with a Pyscho-Educational Horseback Riding Program (PEHR) intervention and included two autistic children and two children with pervasive developmental disorder. The PEHR program provides individualized planned psychological and educational care for each child while they are riding horseback, riding the horse on paths with no other conditions, psycho-educational games on the horse, and behavioral and psychological tasks on the horse (Keino et al., 2009). They used the Human–Equips-Interaction on Mental activity (HEIM) scale, a behavioral scale for evaluating the effect of human–equine relationships on mental activity (Keino et al., 2009). They reported a significant difference post-intervention for part eight of the HEIM scale which rated fear or nervousness as the child was presented with the horse they were going to ride. Each child decreased their level of anxiety when comparing their results from pre- and post-intervention as observed and graded by the investigators (Keino et al., 2009). Also, there were statistical differences reported post intervention for the measures of human relationship, imitation, emotional expression, adaptation to change, visual response, and verbal communication subscales of the HEIM (Keino et al., 2009). No significant differences were noted in the sudden movement, fixation behavior, and nonverbal communication subscales of the HEIM (Keino et al., 2009). Another study included a 10-week occupational therapy intervention program in an equine environment called OTee HORSPLAY (Peters et al., 2021). This study included 20 autistic children, randomized into either the OTee HORSPLAY group, which included 10 weeks of occupational therapy in an equine environment once a week for 60 min, or the waitlist control group, which participated in 10 weeks of didactic training and modeling led by OT graduate students. The control group also completed the OTee HORSPLAY intervention after the first group completed it and data were collected (Peters et al., 2021). Outcome measures included the GAS, Pediatric Evaluation of Disability Inventory Computer Adaptive Test, Autism Spectrum Disorder Module (PEDI-CAT ASD), HCC, the irritability and hyperactivity subscales of the ABC-C, the Social Responsiveness Scale Second Edition (SRS-2), and a survey for the parents that included three open-ended questions about the best and worst aspects of OTee HORSPLAY for their child. Peters et al. (2021) reported improvements in goal performance progress, occupational performance goals, social motivation for the intervention group. They also report significantly reduced irritability for the intervention group (Peters et al., 2021). No other significant results were reported post-intervention for the OTee HORSPLAY group (Peters et al., 2021).
Several studies included general physical activity programs as their intervention and provide moderate support for this intervention in anxiety reduction for autistic individuals (Carey et al., 2022; Gehricke et al., 2022; Hillier et al., 2011; Lee et al., 2022). One study included an 8-week physical activity program that included aerobics, flexibility, balance, strength training, and team activities was used as an intervention for 18 autistic young adults, ages 13–27 (Hillier et al., 2011). This study analyzed the effects of the intervention on stress and anxiety for autistic young adults, therefore they measured salivary cortisol levels as well as participant-reported STAI (Hillier et al., 2011). They reported significant reductions in salivary cortisol levels before and after each training session, but not across the 3 weeks, from week 4 to week 6 or week 2 to week 4 (Hillier et al., 2011). Also, there was a significant reduction in self-reported anxiety before and after each training session, but not a significant reduction in self-reported anxiety across the 8-weeks, as reported by the STAI (Hillier et al., 2011). A study by Carey et al. (2022) included a 16-week exercise program intervention, the sessions occurred three times a week for 1 h and included activities focused on developing and progressing fundamental motor skills like balancing, jumping, and catching, and group games. Participants level of anxiety was measured by the ASC-ASD, completed by parents, teachers, or both to evaluate the participant’s anxiety both in the home and school setting (Carey et al., 2022). According to the ACS-ASD reported by teachers, there was a significant decrease in total ACS-ASD scores when comparing baseline to the final session, but there was no significant decrease in total ACS-ASD scores reported by parents when comparing baseline to the final session (Carey et al., 2022). Another study by Gehricke et al. (2022) compared two groups of autistic children, one group of 53 completed 8 weeks of three physical activity sessions a week for around 50 min, and the other group of 64 completed 8 weeks of 3 LEGO or Minecraft sessions a week for 45 min. For each group the CBCL with the DSM-5 anxiety subscale, SCARED, the parent-rated CSHQ, Physical Activity Questionnaire for Older Children (PAQ-C), and salivary cortisol were collected at baseline, week 3, week 6, week 8, and a follow-up at week 16 (Gehricke et al., 2022). Both the physical activity and sedentary activity groups had significant improvements in anxiety at weeks 3, 6, and 8 as rated by the CBCL with the DSM-5 anxiety subscale, and the exercise intervention group had nominally larger improvements than the sedentary group (Gehricke et al., 2022). At 8 weeks, the SCARED measure reported significant improvements for both groups with a larger improvement in the sedentary group (Gehricke et al., 2022). According to the CSHQ results, sleep quality was significantly improved for the physical activity group, but not the sedentary group (Gehricke et al., 2022). Also, there were no significant chronic or acute changes to salivary cortisol for both groups (Gehricke et al., 2022). Lee et al. (2022) performed an app-assisted walking intervention for 24 autistic adults. Participants were randomly assigned to using the Puzzlewalk app or Google Fit app group, both are apps that use visual aids and goals to promote physical activity (Lee et al., 2022). The intervention occurred for 8 weeks, but data was collected during the fourth and eighth week to reduce the novelty effect of the apps (Lee et al., 2022). Accelerometer data, a self-reported BAI, and a questionnaire that assessed the usefulness of the applications for participants were collected from the participants (Lee et al., 2022). Anxiety levels were not significantly reduced during this intervention, but results suggest that these applications are effective at promoting physical activity (Lee et al., 2022).
Discussion
The results of the systematic review provide evidence of the use of physical activity to address anxiety often observed in autistic individuals. The evidence provides support for the use of foundational and structured group sport activities, yoga programs, horseback riding, and general physical activity programs to reduce anxiety in autistic individuals that often results in avoidance of social interaction, isolation, and increased internalization of problems (Carey et al., 2022; Gehricke et al., 2022; Gillott et al., 2001; Hillier et al., 2011; Howells et al., 2020; Keino et al., 2009; Lee et al., 2022; Peters et al., 2021; Tanksale et al., 2021; White et al., 2009).
According to the evidence examined in this review, there is strong evidence to suggest that participation in yoga programs and community-based football programs reduce anxiety in autistic children (Howells et al., 2020; Tanksale et al., 2021). Howells et al. (2020) compared anxiety levels between the intervention group, those participating in their local Auskick program, and a control group, and the intervention group showed a significant decrease in anxiety post-intervention compared to the control group (Howells et al., 2020). Group sport activity has been shown to decrease depressive symptoms, improve social abilities, and increase self-esteem in the general population (Pluhar et al., 2019). Though more research is needed, evidence suggest the effects of group sport may be a mediator of anxiety for autistic individuals. Tanksale et al. (2021) included a yoga intervention for autistic children and reported a significant decrease in performance anxiety and sleep anxiety for the intervention group (Tanksale et al., 2021). Yoga has been shown to improve motor skills, imitation skills, happiness ratings, self-control, and motor skills for autistic people (Hourston & Atchley, 2017; Kaur & Bhat, 2019; Shanker & Pradhan, 2022). These benefits combined with the potential reduction in anxiety for autistic people promote the need for further investigation into yoga interventions as an effective and beneficial intervention for autistic individuals.
According to the evidence included in this review, there is moderate evidence to suggest motor interventions involving horseback riding can reduce anxiety for autistic children (Keino et al., 2009; Peters et al., 2021). Horseback riding interventions focus on engaging an individual’s cognitive, sensory, and neuromotor systems and helping people achieve certain functional outcomes (Srinivasan et al., 2018). These interventions have been shown to be effective for autistic people for improving social and communication skills, self-esteem, and motor skills (Srinivasan et al., 2018). The results of this systematic review suggest that horseback riding interventions may have a mediating effect on anxiety as well.
There is moderate evidence that general physical activity programs, including app-assisted walking, aerobic exercise, muscle strength activities, balance activities, group games, catching and throwing activities, and flexibility training, can reduce anxiety for autistic adults and children (Carey et al., 2022; Gehricke et al., 2022; Hillier et al., 2011; Lee et al., 2022). In the general population physical activity can decrease anxiety symptoms by altering the chemicals within the brain, decreasing anxiety sensitivity, increasing self-efficacy, acting as a break from a stressful day, improving quality of life, decreasing psychological distress, and improving physical health (DeBoer et al., 2012; Kandola et al., 2018). Although there is limited evidence in the literature to suggest a mechanism for the reduction in anxiety due to physical activity for autistic people, we can hypothesize that any or a combination of the mechanisms in place for the general population also occur for autistic individuals.
The physical activity intervention implemented by Carey et al. (2022) was delivered on a school campus, included groups of 6–10 children at a time, and the educator had appropriate experience with delivering exercise program to autistic children. These criteria eliminate several barriers to physical activity identified through research like transportation, lack of others to participate in exercise with, and lack of appropriate support (Boucher et al., 2022; Hillier et al., 2020). These type of physical activity interventions provide a way to overcome these between-person barriers, and early interventions of such programs can help reduce within-person barriers like negative experiences with physical activity by providing a safe, enthusiastic, enjoyable experience with physical activity early for autistic people (Boucher et al., 2022). Also, it been reported that physical activity can improve motor skills for autistic people (Ruggeri et al., 2020), which is another barrier reported by parents of autistic children. Therefore, participation in a small group, appropriately supervised program located on a school campus could eliminate several barriers to participation, and potentially help autistic children experience the benefits of physical activity like a decrease in anxiety, improved motor skills, decrease stereotypical behaviors, and improved communication skills, all of with have been reported to be affected by physical activity (Bahrami et al., 2016; Howells et al., 2022; Huseyin, 2019; Keller et al., 2021; Must et al., 2015; Shanok et al., 2019; Zhao & Chen, 2018). Hillier et al. (2011) implemented a physical activity intervention for young autistic adults and autistic children, which resulted in significant changes in anxiety, and successfully recruited and retained 18 participants throughout the 8-week intervention. Although the methodology does not include attempts to overcome barriers in participation, they did recruit from a sample of people who were already participating in a physical activity program (Hillier et al., 2011). Future research could compare groups of those participating in physical activity programs and those who are not participating in physical activity programs to better understand why the barriers are overcome by some but not by others. App assisted physical activity interventions could serve as a way to overcome barriers like lack of physical activity enjoyment, by adding a gaming component, as well as lack of resources and transportation since it can be used almost anywhere, parks, neighborhoods, around a campus (Lee et al., 2022; Must et al., 2015). Overall, programs to increase physical activity participation for autistic people should focus on overcoming perceived barriers and improving feelings towards physical activity, so autistic people can receive the apparent of benefits of physical activity.
Study Strengths and Limitations
This is the first systematic review, to our knowledge, of the influence of physical activity intervention on anxiety for autistic people. There was a limited number of studies that included our population, intervention, and outcome criteria. Six out of the eight studies included a population criterion of the participants being aged 18 and below, even though the average lifespan of autistic individuals is 40–58 years, depending on severity (Sala et al., 2020). Among these studies anxiety measurement methods varied, as well as who completed the measures, self-report, parent-report, investigator report, or teacher report. As outlined by Table 3, the studies included did not consistently report certain demographic information or sample characteristics. For example, only one study reported race/ethnicity. This is a limitation because this information could have provided insight into the applicability of the results to other people diagnosed with autism. Lastly, none of the studies included a community engagement component to provide autistic people an opportunity to help shape the intervention, or to solicit feedback on the intervention.
Implications
The findings of this systematic review have the following implications:
-
The evidence indicates that autistic people who experience anxiety benefit from participation in varied physical activity as a means to mediate anxiety and its effects.
-
Autistic children and youth who experience anxiety should participate in general physical activity, specifically designed and structured physical activity, and/or sports on a regular basis.
-
Physical activity opportunities should be made available to children and youth throughout the school day, including but not limited to teaching physical activities/physical games during recess, sports programs offered before and after school, and yoga activities in the classroom.
-
Community programs should be developed to provide autistic children, youth, and adults with general physical activity and structured sports opportunities. Based on the results of this review these programs should focus on implementing programs involving group sport, yoga, motor interventions involving horseback riding, and/or general physical activity programs.
-
Future research should focus on:
-
Narrowing intervention type, duration, and intensity, so we can provide the most effective recommendations for mediating anxiety symptoms through physical activity for autistic people.
-
Identifying the most reliable outcome measures for anxiety for autistic people.
-
Community-engaged projects in which participants contribute to the design of the intervention.
-
Increasing the range of age of participants included, so we can have a better understanding of the influence of physical activity on anxiety for autistic people during all stages of life (Table 3).
-
Conclusion
Anxiety is a major concern for autistic people, it affects 40% of autistic children and 20% of autistic adults (Kerns et al., 2020; Nimmo-Smith et al., 2020). There is a potential for physical activity to be an effective, free intervention to relieve anxiety symptoms for autistic people. Physical activity as a means to reduce anxiety symptoms for the general population has been substantially investigated, however there is not as much research in this area for autistic people. This review compiled the literature currently available for this intervention, group, and outcome measures from three databases. We included a total of eight studies in this systematic review, and the results suggest there is moderate to strong evidence to support the use of different physical activity interventions for mediating anxiety symptoms for autistic children and adults.
References
Adams, D., Clark, M., & Keen, D. (2019). Using self-report to explore the relationship between anxiety and quality of life in children on the autism spectrum. Autism Research, 12(10), 1505–1515. https://doi.org/10.1002/aur.2155
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
Bahrami, F., Movahedi, A., Marandi, S. M., & Sorensen, C. (2016). The effect of karate techniques training on communication deficit of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 46(3), 978–986. https://doi.org/10.1007/s10803-015-2643-y
Boucher, T. Q., McIntyre, C. L., & Iarocci, G. (2022). Facilitators and barriers to physical activity involvement as described by autistic youth with mild intellectual disability. Advances in Neurodevelopmental Disorders, 1–13. https://doi.org/10.1007/s41252-022-00310-5
Brennan, S. E., & Munn, Z. (2021). Prisma 2020: A reporting guideline for the next generation of systematic reviews. JBI Evidence Synthesis, 19(5), 906–908. https://doi.org/10.11124/jbies-21-00112
Broman-Fulks, J. J., Berman, M. E., Rabian, B. A., & Webster, M. J. (2004). Effects of aerobic physical activity on anxiety sensitivity. Behaviour Research and Therapy, 42(2), 125–136. https://doi.org/10.1016/s0005-7967(03)00103-7
Carey, M., Sheehan, D., Healy, S., Knott, F., & Kinsella, S. (2022). The effects of a 16-week school-based exercise program on anxiety in children with autism spectrum disorder. International Journal of Environmental Research and Public Health, 19(9), 5471. https://doi.org/10.3390/ijerph19095471
Centers for Disease Control and Prevention. (2023, December 2). Autism spectrum disorder (ASD). Centers for Disease Control and Prevention. Retrieved August 9, 2023, from https://www.cdc.gov/ncbddd/autism/index.html
DeBoer, L. B., Powers, M. B., Utschig, A. C., Otto, M. W., & Smits, J. A. (2012). Exploring exercise as an avenue for the treatment of anxiety disorders. Expert Review of Neurotherapeutics, 12(8), 1011–1022. https://doi.org/10.1586/ern.12.73
Erickson, K. I., Hillman, C., Stillman, C. M., Ballard, R. M., Bloodgood, B., Conroy, D. E., Macko, R., Marquez, D. X., Petruzzello, S. J., & Powell, K. E. (2019). Physical activity, cognition, and brain outcomes: A review of the 2018 physical activity guidelines. Medicine and Science in Sports and Exercise, 51(6), 1242–1251. https://doi.org/10.1249/MSS.0000000000001936
Gehricke, J.-G., Lowery, L. A., Alejo, S. D., Dawson, M., Chan, J., Parker, R. A., Archibald, A., Lo, A., Benavidez, H., Saini, T., Kuhlthau, K., Trujillo, Y., Grigaux, O., Cadondon, S., Baconawa, M., Bellesheim, K., Sweeney, M., Haddad, F., & Radom-Aizik, S. (2022). The effects of a physical exercise program, LEGOR and Minecraft activities on anxiety in underserved children with autism spectrum disorder. Research in Autism Spectrum Disorders, 97, 102005. https://doi.org/10.1016/j.rasd.2022.102005
Gillott, A., Furniss, F., & Walter, A. (2001). Anxiety in high-functioning children with autism. Autism, 5(3), 277–286. https://doi.org/10.1177/1362361301005003005
Green, S., & Higgins, J. P. T. (2023). Preparing a Cochrane review. In: Cochrane handbook for systematic reviews of interventions (pp. 11–30). https://doi.org/10.1002/9780470712184.ch2
Hillier, A., Buckingham, A., & Schena, D., II. (2020). Physical activity among adults with autism: Participation, attitudes, and barriers. Perceptual and Motor Skills, 127(5), 874–890. https://doi.org/10.1177/0031512520927560
Hillier, A., Murphy, D., & Ferrara, C. (2011). A pilot study: Short-term reduction in salivary cortisol following low level physical exercise and relaxation among adolescents and young adults on the autism spectrum. Stress and Health, 27(5), 395–402. https://doi.org/10.1002/smi.1391
Hourston, S., & Atchley, R. (2017). Autism and mind-body therapies: A systematic review. Journal of Alternative and Complementary Medicine, 23(5), 331–339. https://doi.org/10.1089/acm.2016.0336
Howells, K., Sivaratnam, C., Lindor, E., He, J., Hyde, C., McGillivray, J., Wilson, R. B., & Rinehart, N. (2022). Can a community-based football program benefit motor ability in children with autism spectrum disorder? A pilot evaluation considering the role of social impairments. Journal of Autism and Developmental Disorders, 52(1), 402–413. https://doi.org/10.1007/s10803-021-04933-w
Howells, K., Sivaratnam, C., Lindor, E., Hyde, C., McGillivray, J., Whitehouse, A., & Rinehart, N. (2020). Can participation in a community organized football program improve social, behavioural functioning and communication in children with autism spectrum disorder? A pilot study. Journal of Autism and Developmental Disorders, 50(10), 3714–3727. https://doi.org/10.1007/s10803-020-04423-5
Huseyin, O. (2019). The impact of sport activities on basic motor skills of children with autism. Pedagogics, Psychology, Medical-Biological Problems of Physical Training and Sports, 23(3), 138–144. https://doi.org/10.15561/18189172.2019.0305
Kandola, A., Vancampfort, D., Herring, M., Rebar, A., Hallgren, M., Firth, J., & Stubbs, B. (2018). Moving to beat anxiety: Epidemiology and therapeutic issues with physical activity for anxiety. Current Psychiatry Reports, 20(8), 63. https://doi.org/10.1007/s11920-018-0923-x
Kaur, M., & Bhat, A. (2019). Creative yoga intervention improves motor and imitation skills of children with autism spectrum disorder. Physical Therapy, 99(11), 1520–1534. https://doi.org/10.1093/ptj/pzz115
Keino, H., Funahashi, A., Keino, H., Miwa, C., Hosokawa, M., Hayashi, Y., & Kawakita, K. (2009). Psycho-educational horseback riding to facilitate communication ability of children with pervasive developmental disorders. Journal of Equine Science, 20(4), 79–88. https://doi.org/10.1294/jes.20.79
Keller, R., Costa, T., Imperiale, D., Bianco, A., Rondini, E., Hassiotis, A., & Bertelli, M. O. (2021). Stereotypies in the autism spectrum disorder: Can we rely on an ethological model? Brain Sciences, 11(6), 762. https://doi.org/10.3390/brainsci11060762
Kerns, C. M., Rast, J. E., & Shattuck, P. T. (2020). Prevalence and correlates of caregiver-reported mental health conditions in youth with autism spectrum disorder in the United States. The Journal of Clinical Psychiatry, 82(1), 20m13242. https://doi.org/10.4088/JCP.20m13242
Lee, D., Frey, G. C., Cothran, D. J., Harezlak, J., & Shih, P. C. (2022). Effects of a gamified, behavior change technique-based mobile app on increasing physical activity and reducing anxiety in adults with autism spectrum disorder: Feasibility randomized controlled trial. JMIR Formative Research, 6(7), e35701. https://doi.org/10.2196/35701
Longo, L., & Johnson, B. (2000). Addiction: Part I. Benzodiazepines—Side effects, abuse risk and alternatives. American Family Physician, 61(7), 2121–2128.
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276–282.
Mikkelsen, K., Stojanovska, L., Polenakovic, M., Bosevski, M., & Apostolopoulos, V. (2017). Exercise and mental health. Maturitas, 106, 48–56. https://doi.org/10.1016/j.maturitas.2017.09.0k03
Mitchell, P., Sheppard, E., & Cassidy, S. (2021). Autism and the double empathy problem: Implications for development and mental health. The British Journal of Developmental Psychology, 39(1), 1–18. https://doi.org/10.1111/bjdp.12350
Must, A., Phillips, S., Curtin, C., & Bandini, L. G. (2015). Barriers to physical activity in children with autism spectrum disorders: Relationship to physical activity and screen time. Journal of Physical Activity and Health, 12(4), 529–534. https://doi.org/10.1123/jpah.2013-0271
Nimmo-Smith, V., Heuvelman, H., Dalman, C., Lundberg, M., Idring, S., Carpenter, P., Magnusson, C., & Rai, D. (2020). Anxiety disorders in adults with autism spectrum disorder: A population-based study. Journal of Autism and Developmental Disorders, 50(1), 308–318. https://doi.org/10.1007/s10803-019-04234-3
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (clinical Research Ed.), 372, n71. https://doi.org/10.1136/bmj.n71
Peters, B. C., Wood, W., Hepburn, S., & Moody, E. J. (2021). Preliminary efficacy of occupational therapy in an equine environment for youth with autism spectrum disorder. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-021-05278-0
Pluhar, E., McCracken, C., Griffith, K. L., Christino, M. A., Sugimoto, D., & Meehan, W. P., III. (2019). Team sport athletes may be less likely to suffer anxiety or depression than individual sport athletes. Journal of Sports Science and Medicine, 18(3), 490–496.
Ruggeri, A., Dancel, A., Johnson, R., & Sargent, B. (2020). The effect of motor and physical activity intervention on motor outcomes of children with autism spectrum disorder: A systematic review. Autism: The International Journal of Research and Practice, 24(3), 544–568. https://doi.org/10.1177/1362361319885215
Sackett, D. L. (1989). Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest, 95(2 Suppl), 2S-4S.
Sala, R., Amet, L., Blagojevic-Stokic, N., Shattock, P., & Whiteley, P. (2020). Bridging the gap between physical health and autism spectrum disorder. Neuropsychiatric Disease and Treatment, 16, 1605–1618. https://doi.org/10.2147/ndt.s251394
Shanker, S., & Pradhan, B. (2022). Effect of yoga on the motor proficiency of children with autism spectrum disorder and the feasibility of its inclusion in special school environments. Adapted Physical Activity Quarterly, 39(2), 247–267. https://doi.org/10.1123/apaq.2021-0108
Shanok, N. A., Sotelo, M., & Hong, J. (2019). Brief report: The utility of a golf training program for individuals with autism spectrum disorder. Journal of Autism and Developmental Disorders, 49(11), 4691–4697. https://doi.org/10.1007/s10803-019-04164-0
Shaw, R. J., McDuffie, J. R., Hendrix, C. C., Edie, A., Lindsey-Davis, L., & Williams, J. W., Jr. (2013). Effects of nurse-managed protocols in the outpatient management of adults with chronic conditions. Department of Veterans Affairs (US).
Srinivasan, S. M., Cavagnino, D. T., & Bhat, A. N. (2018). Effects of equine therapy on individuals with autism spectrum disorder: A systematic review. Review Journal of Autism and Developmental Disorders, 5(2), 156–175. https://doi.org/10.1007/s40489-018-0130-z
Tanksale, R., Sofronoff, K., Sheffield, J., & Gilmour, J. (2021). Evaluating the effects of a yoga-based program integrated with third-wave cognitive behavioral therapy components on self-regulation in children on the autism spectrum: A pilot randomized controlled trial. Autism, 25(4), 995–1008. https://doi.org/10.1177/1362361320974841
Trembath, D., Germano, C., Johanson, G., & Dissanayake, C. (2012). The experience of anxiety in young adults with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 27(4), 213–224. https://doi.org/10.1177/1088357612454916
Warburton, D. E. R., & Bredin, S. S. D. (2017). Health benefits of physical activity: A systematic review of current systematic reviews. Current Opinion in Cardiology, 32(5), 541–556. https://doi.org/10.1097/HCO.0000000000000437
White, S. W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229. https://doi.org/10.1016/j.cpr.2009.01.003
Yamada, T., Kondo, Y., & Momosaki, R. (2019). Pico and risk of bias navigator for evidence-based medicine. PeerJ Preprints. https://doi.org/10.7287/peerj.preprints.27684v1
Zhao, M., & Chen, S. (2018). The effects of structured physical activity program on social interaction and communication for children with autism. BioMed Research International, 2018, 1825046. https://doi.org/10.1155/2018/1825046
Acknowledgments
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by KR, PL, and BS. The first draft of the manuscript was written by KR and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kathryn Riis, Patricia Laverdure, and Brittany Samulski. The first draft of the manuscript was written by Kathryn Riis and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. No funding was received to assist with the preparation of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Riis, K., Samulski, B., Neely, K.A. et al. Physical Activity for Anxiety for Autistic People: A Systematic Review. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06356-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10803-024-06356-9