Abstract
Purpose
Major depressive disorder (MDD) disproportionately affects those living with autism spectrum disorder (ASD) and is associated with significant impairment and treatment recidivism.
Methods
We studied the use of accelerated theta burst stimulation (ATBS) for the treatment of refractory MDD in ASD (3 treatments daily x 10 days). This prospective open-label 12-week trial included 10 subjects with a mean age of 21.5 years, randomized to receive unilateral or bilateral stimulation of the dorsolateral prefrontal cortex.
Results
One participant dropped out of the study due to intolerability. In both treatment arms, depressive symptoms, scored on the Hamilton Depression Rating Scale scores, diminished substantially. At 12 weeks post-treatment, full remission was sustained in 5 subjects and partial remission in 3 subjects. Treatment with ATBS, regardless of the site of stimulation, was associated with a significant, substantial, and sustained improvement in depressive symptomatology via the primary outcome measure, the Hamilton Depression Rating Scale. Additional secondary measures, including self-report depression scales, fluid cognition, and sleep quality, also showed significant improvement. No serious adverse events occurred during the study. Mild transient headaches were infrequently reported, which are expected side effects of ATBS.
Conclusion
Overall, ATBS treatment was highly effective and well-tolerated in individuals with ASD and co-occurring MDD. The findings support the need for a larger, sham-controlled randomized controlled trial to further evaluate efficacy of ATBS in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autistic individuals are disproportionately affected by major depressive disorder (MDD), which contributes to functional disability, including educational and vocational impairment, social withdrawal, and suicide across the lifespan (Cassidy et al., 2014; Hollocks et al., 2019; Hudson et al., 2019; Matson & Nebel-Schwalm, 2007). Suicidal ideation in ASD is also elevated, with over 72% of adults with ASD scoring above the recommended cut-off for suicide risk on the Suicide Behaviors Questionnaire-Revised (SBQ-R) which was significantly correlated with reported non-suicidal self-injury, camouflaging, and number of unmet support needs (Cassidy et al., 2018). Though MDD is prevalent in ASD regardless of cognitive ability, autistic individuals without intellectual disability disorder (IDD) are more likely to receive the diagnosis, likely due to clearer communication of internal states and more canonical presentations (Pezzimenti et al., 2019).
A major challenge in treating MDD among those with ASD is the high rates of treatment recidivism and relapse (Hirvikoski et al., 2016). It is estimated that treatment-resistant MDD in ASD individuals likely exceeds that of the general population (> 30%) based on prevalence rates and polypharmacy (Feroe et al., 2021; Rosenberg et al., 2010; Zheng et al., 2021). This is consistent with observations that standard-of-care medications for mood disorders can be unpredictable in ASD and may at times even be counterproductive in ameliorating symptoms (McCracken et al., 2021; Williams et al., 2013). Despite the urgent need for support for this population, little research exists targeting novel interventions for depression and suicidality in ASD.
Repetitive transcranial magnetic stimulation (rTMS) is an evidence-based intervention for MDD in typically developing populations (Razza et al., 2018). rTMS involves brief, high-intensity electrical currents passing through a coil placed near the scalp. This induces a rapidly changing magnetic field that induces an electrical current in local brain parenchyma, leading to both local inhibitory or excitatory neuronal changes as well as changes in connected brain regions (Terao & Ugawa, 2002). Though meta-analysis of rTMS randomized sham-controlled trials demonstrate efficacy in treatment of MDD severity and remission rates, several factors limit the feasibility of the conventional form of treatment in autistic individuals (Sehatzadeh et al., 2019). First, although patients remain awake during the procedure and require no aftercare, traditional rTMS stimulation is delivered above resting motor threshold (RMT) and can lead to headaches, scalp pain, muscle twitching, and eye discomfort. In ASD cohorts, where sensory hypersensitivity is more common, the prevalence of AEs associated with TMS is estimated to be at 25% (Huashuang et al., 2022). Moreover, a conventional rTMS treatment course typically involves daily 45-minute treatment sessions spanning four to six weeks, requiring a significant investment of time and logistical coordination.
Recent advances in rTMS protocols, namely theta burst stimulation (TBS) may help improve tolerability in which sensory hypersensitivity or duration of treatment may be a limiting factor (Elmaghraby et al., 2022; Hong et al., 2015). Since TBS protocols use a higher frequency pulse (> 30 Hz), they only involve several minutes of stimulation and can be performed at or below RMT, minimizing overall sensation (Huang et al., 2005b). Additionally, multiple treatments of TBS or accelerated TBS (ATBS) can be performed in a single day which can dramatically shorten the overall duration of treatment to one to ten days (Duprat et al., 2016; Fitzgerald et al., 2020; Weissman et al., 2018a). So far, TBS protocols (with or without acceleration) are comparable in safety and efficacy to conventional rTMS, but they offer advantages in tolerability, treatment capacity, and cost-effectiveness (Blumberger et al., 2018; Cai et al., 2023). The US Food and Drug Administration (FDA, 2011) cleared the use of TBS in 2018 and ATBS in 2022 as an alternative to conventional rTMS for MDD (Neuteboom et al., 2023).
No RCTs evaluating the efficacy of any form of TMS treatment of MDD in individuals with ASD are available. However, a recent open-label trial of conventional rTMS for MDD in adults with ASD (n = 10) found that 70% of participants responded to treatment and 40% reached remission (Gwynette et al., 2020). Two participants withdrew due to intolerability. Participants with sensitivity to stimulation were started on a lower stimulation intensity and gradually titrated to the full dose or used a < 1 mm foam barrier at the stimulation site. While these results are promising, we hypothesized that the abbreviated course and reduced stimulation intensity of ATBS may be better suited for individuals with ASD.
We conducted a prospective open-label accelerated TBS on treatment-refractory MDD in transition-aged youth with ASD (ages 12–26 years). The Hamilton Depression Rating Scale (HRDS-17) was used as the primary outcome, and we assessed changes from baseline at 1-, 4-, and 12-weeks post-treatment. To investigate stimulation parameters, we randomized participants either unilateral (UL) left dorsolateral prefrontal cortex (DLPFC) stimulation or bilateral stimulation (BL) DLPFC based on recent literature suggesting potential advantages of bilateral stimulation (Blumberger et al., 2012; Chistyakov et al., 2015). Our hypothesis was that bilateral stimulation would enhance the treatment efficacy but may also negatively affect tolerability. Additionally, we administered NIH Cognitive Toolbox measures at each timepoint hypothesizing that changes in scores may reflect prefrontal cortex engagement and predict MDD treatment response (Crane et al., 2017).
Methods
Ethics Statement
This study was approved by the institutional review board at Cincinnati Children’s Hospital Medical Center (CCHMC) and registered with ClinicalTrials.gov (NCT01609374). Recruitment took place between November 2021 and November 2022 through clinician referrals, community flyers, emails, and clinics at a tertiary academic pediatric hospital. All participants provided written informed consent or assent for all study procedures.
Diagnosis of MDD and co-occurring conditions was determined by the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) for participants under 18 years of age (Sheehan et al., 1998) and the Structured Clinical Interview for DSM-5 Disorders (SCID-5) for those 18 and older (Spitzer et al., 1992). Treatment-resistant MDD was determined using the Antidepressant Treatment History Form (Sackeim et al., 2019). Diagnostic assessments were conducted by qualified experienced raters, including licensed clinical psychologists (ADOS-2, MINI-KID) or board-certified child and adolescent psychiatrists (MINI-KID, ATHF).
Participants
Inclusion criteria for participants included: (1) age 12–26 years, (2) diagnosed with ASD (and confirmed by Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2) (Lord et al., 2012), (3) currently meeting Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for a unipolar major depressive disorder or persistent depressive disorder, 3) exhibiting treatment resistance to at least one evidence-based antidepressant medication, (4) Global Assessment of Function (GAF) score ≤ 60, (5) 17-item Hamilton Depression Rating Scale (HDRS-17) or Beck Depression Inventory II (BDI-II) score in the clinically depressed range (≥ 20) that was sustained over the two-week lead-in period.
Exclusion criteria included any of the following: (1) significant psychiatric or neurological disease unrelated to ASD or MDD within the last six months, (2) use of investigational drugs, (3) any contraindications to TMS (Rossi et al., 2021) (4) Intelligence Quotient < 80 per the Wechsler Abbreviated Scale of Intelligence, 2nd Edition (Wechsler, 1999), (5) active pregnancy (confirmed by urine test), (6) active suicidality, (7) history of epilepsy or use of antiepileptic drugs, (8) prior rTMS treatment, (9) changes in psychiatric medicines two weeks before TMS treatment, 11) substance use or substance dependence disorder (confirmed by urine toxicology).
Study Design
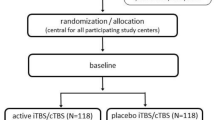
This open-label prospective clinical trial involved 30 TBS sessions over a period of ten days (Fig. 1). Following the screening visit, eligible participants were randomly assigned to receive either standard, unilateral intermittent TBS (iTBS) to the left dorsolateral prefrontal cortex (DLPFC) (FDA, 2011) or bilateral stimulation with iTBS to the left DLPFC and continuous TBS (cTBS) to the right DLPFC. Following randomization, participants had to maintain eligibility for a two-week lead-in period prior to the first treatment session. Additional assessments were conducted at days 5 and 10 of the intervention and 1-, 4-, and 12-weeks post-treatment.
Intervention
A Magstim Horizon Performance stimulator (Magstim, Whitland, UK) with a 70mmm figure-eight EZ cool coil was used for all treatment sessions. Coil placement was determined using the BEAM-F3 method (Beam et al., 2009). A separate figure-eight coil was used to establish RMT. RMT was defined as the lowest TMS intensity needed to produce a contralateral thumb twitch in at least three of six trials (Horvath et al., 2010). For participants in the BL group, RMT was determined for each hemisphere. All iTBS and cTBS sessions consisted of triplet 50 Hz pulses repeated in 5 Hz bursts for a total of 600 pulses per session at 90% of RMT (Huang et al., 2005a). During iTBS 20 trains were applied in 2-second bursts with 8-second pauses, while cTBS involved a continuous pulse train for a total duration of 53 s. TBS was delivered in three sessions daily over ten days, with 50 min intervals between sessions (Cai et al., 2023). To account for participants with sensory hypersensitivity we titrated up to target (90%) stimulation intensity over the first two treatment days, starting at 50% RMT and increasing by 10–20% each session, depending on each subject’s tolerance.
Outcome Measures
The primary outcome measure was change in scores on the HDRS-17 (Hamilton, 1986). Secondary depression measures (for validation) included BDI-II (Osman et al., 2004) and Quick Inventory of Depressive Symptomatology (QIDS) (Rush et al., 2003). Suicidal behavior was assessed by physician-administered Columbia-Suicide Severity Rating Scale (C-SSRS) (Posner et al., 2008) at screening and self-report Suicide Behavior Questionnaire (SBQ) (Osman et al., 2001) at screening, intervention days 5 and 10, and all follow-up visits. Changes in anxiety symptoms were assessed using the Generalized Anxiety Disorder-7 item (GAD-7) (Spitzer et al., 2006). Changes in sleep were measured using the Pittsburgh Sleep Quality Inventory (PSQI) (Buysse et al., 1989), and social functioning was measured using the Social Responsiveness Scale (SRS) (Bruni, 2014). Neurocognitive function was assessed using the NIH Cognitive Toolbox (processing speed, working memory, language, and executive function i.e., inhibitory control, set shifting) (Weintraub et al., 2013) and neuromuscular function using the Grip Strength Test from the NIH Toolbox Motor Battery (Reuben et al., 2013).
Safety Outcomes
To assess adverse events (AEs) related to TMS, a 16-point systematic review of systems was conducted at the beginning and end of each treatment day.
Statistical Analysis
Given the exploratory nature of this pilot study, we present data at the individual level and used streamlined statistical modeling to discern overarching trends and effects. No outliers were detected. For each outcome measure, we provide a three-panel figure depicting:
-
1.
Main Effect Plot: This plot displays the mean values of the measure across different time points.
-
2.
Group Interaction Plot: This plot illustrates the interaction effect between time and stimulation site. The mean values of the measure are plotted, stratified by treatment.
-
3.
Subject-level Plot: This plot provides insights into individual variability by plotting each subject’s mean value for the measure across time.
We conducted a linear mixed-effects analysis using the lmerTest package in R 4.3 to identify any main effects of time or treatment arm, as well as their potential interaction effect on each outcome measure. To account for the repeated measures design, we incorporated random intercepts for subjects.
Mathematically, the model can be represented as:
Where:
-
\({Y}_{ijk}\) is the dependent variable (e.g., a specific measure for a given subject at a particular time in a certain group).
-
\(\mu\) is the overall mean.
-
\({\alpha }_{i}\) represents the effect of the ith level of factor A (Time).
-
\({\beta }_{j}\) denotes the effect of the jth level of factor B (Group).
-
\((\alpha \beta {)}_{ij}\) stands for the interaction effect between the ith level of factor A and the jth level of factor B.
-
\({\gamma }_{k}\) is the random effect of the kth subject (or individual).
-
\({\epsilon}_{ijk}\) is the random error associated with the kth observation under the ith level of factor A and jth level of factor B.
Following model estimation, we extracted the ANOVA table to ascertain if a main or interaction effect was present. Depending on the effect, post-hoc tests were carried out to assess pairwise differences between baseline and post-treatment time points, while also using false discovery rate (FDR) to adjust for multiple comparisons. An adjusted p value less than or equal to 0.05 was considered statistically significant.
Results
Ten participants (2 females; min age = 17, max age = 26.2, median age = 22) with ASD and treatment refractory MDD (mean failed antidepressant trials = 3.44 ± 1.7) were randomized to either UL or BL ATBS treatment. Demographics and baseline clinical measures (including MDD severity) were similar between treatment arms (Table 1). One subject disclosed additional history during the trial that supports a diagnosis of borderline personality disorder. While the subject was included in all the main analysis models, they were excluded from the exploratory correlation analysis. Consolidated Standards of Reporting Trials (CONSORT) flow diagram showing the selection of participants from initial screening to final analysis (Fig. 2).
Clinical and Behavioral Outcomes
Summary results of the effects from each LME model are displayed in Table 2. For models that showed a significant main or interaction effect, post-hoc testing results are presented in Table 3.
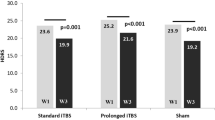
Depression: Primary and Secondary Outcomes
The main effect of time was significant for the primary outcome of interest, HRDS-17, F(3, 21) = 28.49, p < 0.001, EF = 1.976, indicating a large Cohen’s treatment effect size (EF). For HRDS-17 Total Score, significant differences from baseline were observed at all three time points: Week 1, t(21) = 7.09, p < 0.001, estimated change = -11.43; Week 4, t(21) = 7.80, p < 0.001, estimated change = -12.58; Week 12, t(21) = 7.68, p < 0.001, estimated change = -12.38. By week 4, 7 out of 9 subjects showed a significant treatment response (≥ 50% reduction from baseline HDRS-17 score). Treatment effects were largely sustained through the 12-week follow-up period (Fig. 3); at this timepoint, five subjects met the criteria for full remission of depression and three achieved partial remission (American Psychiatric Association & Association, 2013).
Only the main effect of time was significant for BDI-II Total, F(3, 20) = 9.36, p < 0.001, EF = 1.181, also indicating a large treatment effect. Similarly, for QIDS Total, only the main effect of time was significant, F(3, 21) = 7.72, p = 0.001, EF = 1.037. Post-hoc tests (Table 3) demonstrated that BDI and QIDS saw significant improvements from baseline at Weeks 1, 4, and 12 (p < 0.01 for each).
Trajectories on depression scales (HDRS-17 Total Score, BDI-II Total, QIDS Total) over 12 weeks following ATBS treatment. Timepoint 0: baseline; Timepoints 1, 4, and 12: post-treatment follow-ups, numbered by week. Left: group means with significance; center: Bilateral vs. Unilateral group averages; right: individual progressions (S1-S9). Significance levels: * p < 0.05, ** p < 0.01, *** p < 0.001
Anxiety
For GAD-7 Total, the main effect of time was significant, F(3, 21) = 3.71, p = 0.028, EF = 0.721 (Fig. 4). Post-hoc tests showed a significant difference from baseline observed at Week 12: t(21) = 2.93, p = 0.039, estimated change = 4.27, but not for Week 1 or 4.
Longitudinal score changes for various clinical measures (GAD-7 Total, PSQI Score, SRS Total, Fluid Cognition Raw Score) over 12 weeks following ATBS treatment. Timepoint 0: baseline; Timepoints 1, 4, and 12: post-treatment follow-ups, numbered by week. Left: group means with significance; center: Bilateral vs. Unilateral group averages; right: individual progressions (S1-S9). Significance levels: * p < 0.05, ** p < 0.01, *** p < 0.001
Sleep
For PSQI Score, the main effect of time was significant, F(3, 19) = 4.27, p = 0.018, EF = 0.799 and demonstrated a large treatment effect (Fig. 4). Post-hoc tests demonstrated a significant improvement in sleep ratings at Week 4: t(19) = 3.19, p = 0.023, estimated change = 4.38 and trending improvement at Week 12.
Social
For SRS Total, neither the main effect of time, F(3, 21) = 0.80, p = 0.51, EF = 0.337, nor the interaction between time and group, F(3, 21) = 0.87, p = 0.47, EF = 0.350, were significant (Fig. 4). Neurocognitive.
For Fluid Cognition, only the main effect of time was significant, F(3, 21) = 10.00, p < 0.001, EF = 1.174, indicating a large effect size (Fig. 4). Post-hoc testing found a trending improvement in Fluid Cognition from baseline to Week 1 and significant improvement from baseline were observed at Week 4, t(21) = -3.03, p = 0.031, estimated change = -8.05, and Week 12, t(21) = -5.47, p < 0.001, estimated change = -14.50.
Neuromuscular
For Grip Strength, neither the main effect of time, F(3, 21) = 1.19, p = 0.34, EF = 0.394, nor the interaction between time and group, F(3, 21) = 0.86, p = 0.48, EF = 0.335, were significant, but the main effect of group was trending, F(1, 7) = 5.65, p = 0.05, EF = 0.497.
Exploratory Biomarker
An exploratory analysis was conducted to investigate the relationship between changes in Fluid Cognition scores (NIH Toolbox) and changes in depressive symptomatology (measured by HRDS-17) at Week 12. The results indicated a significant correlation between improvement in Fluid Cognition scores at week 4 and reduction in depression symptoms at 12 (Fig. 5).
Safety Outcomes
The ATBS intervention was completed by nine subjects (UL = 5; BL = 4). However, one participant in the bilateral group was unable to tolerate the stimulation and withdrew from treatment. Five subjects (n = 2 UL; n = 3 BL) required titration to reach target stimulation intensity. Overall, adverse events were mild and self-limiting. Over the 90 treatment days (10 days per subject), a total of 6 headaches were reported, resulting in a 7% incidence rate. All headaches were associated with bilateral treatment and were described by participants as mild in severity and spontaneously resolved.
Discussion
This open-label trial demonstrates the efficacy and safety of ATBS in transition-aged autistic youth with treatment-refractory MDD. Treatment-resistant MDD in ASD is a challenging condition to manage, often necessitating polypharmacy or therapeutic approaches associated with higher side effects. Though the efficacy of rTMS for MDD is well established, adapting the intervention at scale for ASD individuals poses unique challenges. The primary purpose of this study was to identify optimal design parameters and outcome measures to advance into a larger pivotal RCT. We observed a robust and sustained treatment in most participants following ATBS regardless of stimulation site. The observed statistically significant improvement across various MDD scales immediately post-treatment suggests ATBS may elicit rapid antidepressant effects, especially in comparison to antidepressant medications or psychotherapy and especially notable in a treatment-refractory sample.
It is important to consider the limitations of our study design, non-controlled studies have shown large effects in depression trials (Wager & Atlas, 2015; Walsh et al., 2002). Nevertheless, recent research on the placebo effect has suggested that it may activate similar areas of the brain as actual antidepressant treatment, and strong placebo effects may indicate regression to the mean. To mitigate these potential confounding factors and identify potential mechanisms, we collected high-resolution electroencephalography to assess changes in brain activity (in preparation) and the inclusion of a lead-in period to account for spontaneous remission of depression symptoms. There is considerable existing evidence that TMS treatment in depression is superior to sham stimulation in typically developing cohorts, albeit with recent meta-analyses lowering the effect size in some populations. (Brini et al., 2023). As the current FDA-cleared rTMS protocol does not exclude individuals with ASD, it remains an evidence-based treatment for MDD when typical therapies are ineffective(Zemplenyi et al., 2022). ATBS may be particularly well suited in cases where there is a high risk of adverse outcomes associated with prolonged depressive episodes, intolerability to typical rTMS, or when the next proximal step is electroconvulsive therapy.
We observed no significant difference in efficacy between Unilateral (UL) and Bilateral (BL) stimulation. However, BL stimulation was associated with a higher incidence of side effects and involved a greater number of procedures. The question of relative effectiveness of BL vs. unilateral rTMS in MDD treatment remains unclear; however, empirical data suggests that stimulation parameters, patient population, and tolerability should be considered (Blumberger et al., 2016; Fitzgerald et al., 2012, 2013; Trevizol et al., 2019; Weissman et al., 2018b). Taking into account the practical considerations which we observed and the present lack of evidence-based treatments, future RCTs may be well-served to focus on UL stimulation in ASD populations.
We administered serial computerized neurocognitive testing, hypothesizing that changes in performance on these tests could serve as biomarkers of prefrontal target engagement and predict later treatment effects (de Boer et al., 2021). Following ATBS treatment, we observed, in the majority of participants, a marked improvement in fluid cognition scores (NIH Toolbox) which was predictive of treatment response on the HRDS-17 at 12 weeks. The neurocognitive tests underlying these findings, such as the Flanker task and card sorting tasks, have been consistently linked to the efficiency of frontal-parietal cortical networks (Kim et al., 2017). However, in our sample, these findings are potentially confounded by concurrent improvements in MDD and associated pseudodementia (Kim et al., 2019).
Even if improvements of fluid cognition are unrelated to ATBS and instead secondary to the amelioration of MDD, assessing fluid cognition in ASD MDD may still serve as an indicator of the duration or response of treatment. Intriguingly, several studies have reported that, in comparison to typically developed individuals, those with ASD exhibit increased activity in temporal and occipital networks, but decreased activity in frontal-parietal networks during fluid reasoning tasks (Simard et al., 2015; Soulières et al., 2009). This suggests that independent studies of accelerated theta-burst stimulation for improving fluid cognition by engaging potentially underactive frontal-parietal networks in ASD may be worth exploring.
Limitations
Several limitations to our study must be considered in context with the strong treatment effects. First and foremost, the potential of expectancy effects, widely observed in rTMS studies, particularly with younger subjects (Oberman et al., 2021; Xu et al., 2023), is important to consider. However, the observed changes in fluid cognition provide an objective marker of treatment response, thus reducing the likelihood of expectancy effects significantly influencing our results. Second, sample size and the exclusion of autistic individuals with IDD reduces the power, generalizability of these results, and our ability to identify subgroups of patients who may benefit most from ATBS compared to other forms of treatment. For example, one participant disclosed during treatment additional history and symptoms consistent with co-occurring personality disorder and did not demonstrate any treatment effects. This result is consistent with the typical treatment refractoriness of personality disorders (Abraham & Calabrese, 2008). Another limitation is accurately diagnosing and assessing the severity of MDD in ASD populations, where clinical presentation may be atypical and standardized measures may not be validated. To assess depression severity, we used clinician and self-report measures, including input from caregivers when available. This approach aligns with previous studies that suggest a multi-informant assessment in ASD captures complex symptoms and experiences more effectively (Sandercock et al., 2020).
Conclusion
This exploratory study provides support for the safety and efficacy of ATBS in addressing treatment resistant MDD in autistic individuals. We observed rapid and large treatment effects across multiple domains that endured over time, with 56% (5/9) of subjects meeting criteria for remission at 12-weeks post-treatment. The distinctive treatment challenges posed by autistic populations, such as sensory hypersensitivities and the necessity of multi-informant outcome assessments, underscore the need for a nuanced approach to adapting ATBS protocols. Our findings suggest that neurocognitive testing could be an objective biomarker for predicting treatment response and potentially individualizing treatment. However, larger, sham-controlled studies are necessary to validate these findings. If successful, ATBS could emerge as an evidence-based intervention for MDD in ASD, an area that currently lacks effective treatments.
Code Availability
The code is available at https://github.com/cincibrainlab.
References
Abraham, P. F., & Calabrese, J. R. (2008). Evidenced-based pharmacologic treatment of borderline personality disorder: A shift from SSRIs to anticonvulsants and atypical antipsychotics? Journal of Affective Disorders, 111(1), 21–30.
American Psychiatric Association, D., &, & Association, A. P. (2013). Diagnostic and statistical manual of mental disorders: DSM-5, (Vol. 5). American Psychiatric Association Washington, DC.
Beam, W., Borckardt, J. J., Reeves, S. T., & George, M. S. (2009). An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimulation, 2(1), 50–54. https://doi.org/10.1016/j.brs.2008.09.006
Blumberger, D. M., Mulsant, B. H., Fitzgerald, P. B., Rajji, T. K., Ravindran, A. V., Young, L. T., Levinson, A. J., & Daskalakis, Z. J. (2012). A randomized double-blind sham-controlled comparison of unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant major depression. The World Journal of Biological Psychiatry : The Official Journal of the World Federation of Societies of Biological Psychiatry, 13(6), 423–435.
Blumberger, D. M., Maller, J. J., Thomson, L., Mulsant, B. H., Rajji, T. K., Maher, M., Brown, P. E., Downar, J., Vila-Rodriguez, F., Fitzgerald, P. B., & Daskalakis, Z. J. (2016). Unilateral and bilateral MRI-targeted repetitive transcranial magnetic stimulation for treatment-resistant depression: A randomized controlled study. Journal of Psychiatry and Neuroscience, 41(4), E58–66. https://doi.org/10.1503/jpn.150265
Blumberger, D. M., Vila-Rodriguez, F., Thorpe, K. E., Feffer, K., Noda, Y., Giacobbe, P., Knyahnytska, Y., Kennedy, S. H., Lam, R. W., Daskalakis, Z. J., & Downar, J. (2018). Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): A randomised non-inferiority trial. Lancet, 391(10131), 1683–1692. https://doi.org/10.1016/S0140-6736(18)30295-2
Brini, S., Brudasca, N. I., Hodkinson, A., Kaluzinska, K., Wach, A., Storman, D., Prokop-Dorner, A., Jemioło, P., & Bala, M. M. (2023). Efficacy and safety of transcranial magnetic stimulation for treating major depressive disorder: An umbrella review and re-analysis of published meta-analyses of randomised controlled trials. Clinical Psychology Review, 100, 102236. https://doi.org/10.1016/j.cpr.2022.102236
Bruni, T. P. (2014). Test review: Social responsiveness scale–second edition (SRS-2). Journal of Psychoeducational Assessment, 32(4), 365–369. https://doi.org/10.1177/0734282913517525
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Cai, D. B., Qin, Z. J., Lan, X. J., Liu, Q. M., Qin, X. D., Wang, J. J., Goya-Maldonado, R., Huang, X. B., Ungvari, G. S., Ng, C. H., Zheng, W., & Xiang, Y. T. (2023). Accelerated intermittent theta burst stimulation for major depressive disorder or bipolar depression: A systematic review and meta-analysis. Asian Journal of Psychiatry, 85, 103618. https://doi.org/10.1016/j.ajp.2023.103618
Cassidy, S., Bradley, P., Robinson, J., Allison, C., McHugh, M., & Baron-Cohen, S. (2014). Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: A clinical cohort study. Lancet Psychiatry, 1(2), 142–147. https://doi.org/10.1016/S2215-0366(14)70248-2
Cassidy, S., Bradley, L., Shaw, R., & Baron-Cohen, S. (2018). Risk markers for suicidality in autistic adults. Mol Autism, 9, 42. https://doi.org/10.1186/s13229-018-0226-4
Chistyakov, A. V., Kreinin, B., Marmor, S., Kaplan, B., Khatib, A., Darawsheh, N., Koren, D., Zaaroor, M., & Klein, E. (2015). Preliminary assessment of the therapeutic efficacy of continuous theta-burst magnetic stimulation (cTBS) in major depression: A double-blind sham-controlled study. Journal of Affective Disorders, 170, 225–229. https://doi.org/10.1016/j.jad.2014.08.035
Crane, N. A., Jenkins, L. M., Bhaumik, R., Dion, C., Gowins, J. R., Mickey, B. J., Zubieta, J. K., & Langenecker, S. A. (2017). Multidimensional prediction of treatment response to antidepressants with cognitive control and functional MRI. Brain, 140(2), 472–486. https://doi.org/10.1093/brain/aww326
de Boer, N. S., Schluter, R. S., Daams, J. G., van der Werf, Y. D., Goudriaan, A. E., & van Holst, R. J. (2021). The effect of non-invasive brain stimulation on executive functioning in healthy controls: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 125, 122–147. https://doi.org/10.1016/j.neubiorev.2021.01.013
Duprat, R., Desmyter, S., Rudi, D. R., van Heeringen, K., Van den Abbeele, D., Tandt, H., Bakic, J., Pourtois, G., Dedoncker, J., Vervaet, M., Van Autreve, S., Lemmens, G. M. D., & Baeken, C. (2016). Accelerated intermittent theta burst stimulation treatment in medication-resistant major depression: A fast road to remission? Journal of Affective Disorders, 200, 6–14. https://doi.org/10.1016/j.jad.2016.04.015
Elmaghraby, R., Sun, Q., Ozger, C., Shekunov, J., Romanowicz, M., & Croarkin, P. E. (2022). A systematic review of the safety and tolerability of theta burst stimulation in children and adolescents. Neuromodulation: Technology at the Neural Interface, 25(4), 494–503. https://doi.org/10.1111/ner.13455
FDA (2011). Repetitive Transcranial Magnetic Stimulation (rTMS) Systems - Class II Special Controls Guidance for Industry and FDA Staff. U.S. Food and Drug Administration Retrieved from https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/repetitive-transcranial-magnetic-stimulation-rtms-systems-class-ii-special-controls-guidance
Feroe, A. G., Uppal, N., Gutiérrez-Sacristán, A., Mousavi, S., Greenspun, P., Surati, R., Kohane, I. S., & Avillach, P. (2021). Medication use in the management of comorbidities among individuals with autism spectrum disorder from a large nationwide insurance database. JAMA Pediatr, 175(9), 957–965. https://doi.org/10.1001/jamapediatrics.2021.1329
Fitzgerald, P. B., Hoy, K. E., Herring, S. E., McQueen, S., Peachey, A. V., Segrave, R. A., Maller, J., Hall, P., & Daskalakis, Z. J. (2012). A double blind randomized trial of unilateral left and bilateral prefrontal cortex transcranial magnetic stimulation in treatment resistant major depression. Journal of Affective Disorders, 139(2), 193–198. https://doi.org/10.1016/j.jad.2012.02.017
Fitzgerald, P. B., Hoy, K. E., Singh, A., Gunewardene, R., Slack, C., Ibrahim, S., Hall, P. J., & Daskalakis, Z. J. (2013). Equivalent beneficial effects of unilateral and bilateral prefrontal cortex transcranial magnetic stimulation in a large randomized trial in treatment-resistant major depression. International Journal of Neuropsychopharmacology, 16(9), 1975–1984. https://doi.org/10.1017/S1461145713000369
Fitzgerald, P. B., Chen, L., Richardson, K., Daskalakis, Z. J., & Hoy, K. E. (2020). A pilot investigation of an intensive theta burst stimulation protocol for patients with treatment resistant depression. Brain Stimulation, 13(1), 137–144. https://doi.org/10.1016/j.brs.2019.08.013
Gwynette, M. F., Lowe, D. W., Henneberry, E. A., Sahlem, G. L., Wiley, M. G., Alsarraf, H., Russo, S. B., Joseph, J. E., Summers, P. M., Lohnes, L., & George, M. S. (2020). Treatment of adults with autism and major depressive disorder using transcranial magnetic stimulation: An open label pilot study. Autism Research, 13(3), 346–351. https://doi.org/10.1002/aur.2266
Hamilton, M. (1986). The Hamilton Rating Scale for Depression. In N. Sartorius & T. A. Ban (Eds.), Assessment of Depression, (pp. 143–152). Springer Berlin Heidelberg. https://doi.org/10.1007/978-3-642-70486-4_14
Hirvikoski, T., Mittendorfer-Rutz, E., Boman, M., Larsson, H., Lichtenstein, P., & Bolte, S. (2016). Premature mortality in autism spectrum disorder. British Journal of Psychiatry, 208(3), 232–238. https://doi.org/10.1192/bjp.bp.114.160192S0007125000279385 [pii].
Hollocks, M. J., Lerh, J. W., Magiati, I., Meiser-Stedman, R., & Brugha, T. S. (2019). Anxiety and depression in adults with autism spectrum disorder: A systematic review and meta-analysis. Psychological Medicine, 49(4), 559–572. https://doi.org/10.1017/S0033291718002283
Hong, Y. H., Wu, S. W., Pedapati, E. V., Horn, P. S., Huddleston, D. A., Laue, C. S., & Gilbert, D. L. (2015). Safety and tolerability of theta burst stimulation vs. single and paired pulse transcranial magnetic stimulation: A comparative study of 165 pediatric subjects. Frontiers in Human Neuroscience, 9, 29. https://doi.org/10.3389/fnhum.2015.00029
Horvath, J. C., Mathews, J., Demitrack, M. A., & Pascual-Leone, A. (2010). The neurostar TMS device: conducting the FDA approved protocol for treatment of depression. Journal of visualized experiments : JoVE, (45), 2345. https://doi.org/10.3791/2345
Huang, Y. Z., Edwards, M. J., Rounis, E., Bhatia, K. P., & Rothwell, J. C. (2005a). Theta burst stimulation of the human motor cortex. Neuron, 45(2), 201–206. https://doi.org/10.1016/j.neuron.2004.12.033
Huang, Y. Z., Edwards, M. J., Rounis, E., Bhatia, K. P., & Rothwell, J. C. (2005b). Theta burst stimulation of the human motor cortex. Neuron, 45(2), 201–206. https://doi.org/10.1016/j.neuron.2004.12.033
Huashuang, Z., Yang, L., Chensheng, H., Jing, X., Bo, C., Dongming, Z., Kangfu, L., & Shi-Bin, W. (2022). Prevalence of adverse effects associated with transcranial magnetic stimulation for autism spectrum disorder: A systematic review and meta-analysis. Frontiers in Psychiatry, 13, 875591. https://doi.org/10.3389/fpsyt.2022.875591
Hudson, C. C., Hall, L., & Harkness, K. L. (2019). Prevalence of depressive disorders in individuals with autism spectrum disorder: A meta-analysis. Journal of Abnormal Child Psychology, 47(1), 165–175. https://doi.org/10.1007/s10802-018-0402-1
Kim, N. Y., Wittenberg, E., & Nam, C. S. (2017). Behavioral and neural correlates of executive function: Interplay between inhibition and updating processes. Front Neurosci, 11, 378. https://doi.org/10.3389/fnins.2017.00378
Kim, T. D., Hong, G., Kim, J., & Yoon, S. (2019). Cognitive enhancement in neurological and psychiatric disorders using transcranial magnetic stimulation (TMS): A review of modalities, potential mechanisms and future implications. Exp Neurobiol, 28(1), 1–16. https://doi.org/10.5607/en.2019.28.1.1
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule: ADOS-2. Western Psychological Services Los Angeles.
Matson, J. L., & Nebel-Schwalm, M. (2007). Assessing challenging behaviors in children with autism spectrum disorders: A review. Research in Developmental Disabilities, 28(6), 567–579. https://doi.org/10.1016/j.ridd.2006.08.001
McCracken, J. T., Anagnostou, E., Arango, C., Dawson, G., Farchione, T., Mantua, V., McPartland, J., Murphy, D., Pandina, G., & Veenstra-VanderWeele, J. (2021). Drug development for autism spectrum disorder (ASD): Progress, challenges, and future directions. European Neuropsychopharmacology, 48, 3–31. https://doi.org/10.1016/j.euroneuro.2021.05.010
Neuteboom, D., Zantvoord, J. B., Goya-Maldonado, R., Wilkening, J., Dols, A., van Exel, E., Lok, A., de Haan, L., & Scheepstra, K. W. (2023). Accelerated intermittent theta burst stimulation in major depressive disorder: A systematic review. Psychiatry Research, 115429.
Oberman, L. M., Hynd, M., Nielson, D. M., Towbin, K. E., Lisanby, S. H., & Stringaris, A. (2021). Repetitive transcranial magnetic stimulation for adolescent major depressive disorder: A focus on neurodevelopment. Frontiers in Psychiatry, 12, 642847. https://doi.org/10.3389/fpsyt.2021.642847
Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The suicidal behaviors questionnaire-revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. https://doi.org/10.1177/107319110100800409
Osman, A., Kopper, B. A., Barrios, F., Gutierrez, P. M., & Bagge, C. L. (2004). Reliability and Validity of the Beck Depression Inventory–II With Adolescent Psychiatric Inpatients [https://doi.org/10.1037/1040-3590.16.2.120]
Pezzimenti, F., Han, G. T., Vasa, R. A., & Gotham, K. (2019). Depression in youth with autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America, 28(3), 397–409. https://doi.org/10.1016/j.chc.2019.02.009
Posner, K., Brent, D., Lucas, C., Gould, M., Stanley, B., Brown, G., Fisher, P., Zelazny, J., Burke, A., & Oquendo, M. (2008). Columbia-suicide severity rating scale (C-SSRS). Columbia University Medical Center.
Razza, L. B., Moffa, A. H., Moreno, M. L., Carvalho, A. F., Padberg, F., Fregni, F., & Brunoni, A. R. (2018). A systematic review and meta-analysis on placebo response to repetitive transcranial magnetic stimulation for depression trials. Progress in Neuropsychopharmacology and Biological Psychiatry, 81, 105–113. https://doi.org/10.1016/j.pnpbp.2017.10.016
Reuben, D. B., Magasi, S., McCreath, H. E., Bohannon, R. W., Wang, Y. C., Bubela, D. J., Rymer, W. Z., Beaumont, J., Rine, R. M., Lai, J. S., & Gershon, R. C. (2013). Motor assessment using the NIH toolbox. Neurology, 80(11 Suppl 3), S65–75. https://doi.org/10.1212/WNL.0b013e3182872e01
Rosenberg, R. E., Mandell, D. S., Farmer, J. E., Law, J. K., Marvin, A. R., & Law, P. A. (2010). Psychotropic medication use among children with autism spectrum disorders enrolled in a national registry, 2007–2008. Journal of Autism and Developmental Disorders, 40(3), 342–351. https://doi.org/10.1007/s10803-009-0878-1
Rossi, S., Antal, A., Bestmann, S., Bikson, M., Brewer, C., Brockmöller, J., Carpenter, L. L., Cincotta, M., Chen, R., Daskalakis, J. D., Di Lazzaro, V., Fox, M. D., George, M. S., Gilbert, D., Kimiskidis, V. K., Koch, G., Ilmoniemi, R. J., Lefaucheur, J. P., Leocani, L., & Hallett, M. (2021). Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: Expert guidelines. Clinical Neurophysiology, 132(1), 269–306. https://doi.org/10.1016/j.clinph.2020.10.003
Rush, A. J., Trivedi, M. H., Ibrahim, H. M., Carmody, T. J., Arnow, B., Klein, D. N., Markowitz, J. C., Ninan, P. T., Kornstein, S., & Manber, R. (2003). The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583.
Sackeim, H. A., Aaronson, S. T., Bunker, M. T., Conway, C. R., Demitrack, M. A., George, M. S., Prudic, J., Thase, M. E., & Rush, A. J. (2019). The assessment of resistance to antidepressant treatment: Rationale for the antidepressant treatment history form: Short form (ATHF-SF). Journal of Psychiatric Research, 113, 125–136. https://doi.org/10.1016/j.jpsychires.2019.03.021
Sandercock, R. K., Lamarche, E. M., Klinger, M. R., & Klinger, L. G. (2020). Assessing the convergence of self-report and informant measures for adults with autism spectrum disorder. Autism, 24(8), 2256–2268. https://doi.org/10.1177/1362361320942981
Sehatzadeh, S., Daskalakis, Z. J., Yap, B., Tu, H. A., Palimaka, S., Bowen, J. M., & O’Reilly, D. J. (2019). Unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant depression: A meta-analysis of randomized controlled trials over 2 decades. Journal of Psychiatry and Neuroscience, 44(3), 151–163. https://doi.org/10.1503/jpn.180056
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33quiz34. https://www.ncbi.nlm.nih.gov/pubmed/9881538
Simard, I., Luck, D., Mottron, L., Zeffiro, T. A., & Soulières, I. (2015). Autistic fluid intelligence: Increased reliance on visual functional connectivity with diminished modulation of coupling by task difficulty. NeuroImage: Clinical, 9, 467–478. https://doi.org/10.1016/j.nicl.2015.09.007
Soulières, I., Dawson, M., Samson, F., Barbeau, E. B., Sahyoun, C. P., Strangman, G. E., Zeffiro, T. A., & Mottron, L. (2009). Enhanced visual processing contributes to matrix reasoning in autism. Human Brain Mapping, 30(12), 4082–4107. https://doi.org/10.1002/hbm.20831
Spitzer, R. L., Williams, J. B., Gibbon, M., & First, M. B. (1992). The structured clinical interview for DSM-III-R (SCID): I: History, rationale, and description. Archives of General Psychiatry, 49(8), 624–629.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Terao, Y., & Ugawa, Y. (2002). Basic mechanisms of TMS. Journal of Clinical Neurophysiology, 19(4), 322–343. https://doi.org/10.1097/00004691-200208000-00006
Trevizol, A. P., Goldberger, K. W., Mulsant, B. H., Rajji, T. K., Downar, J., Daskalakis, Z. J., & Blumberger, D. M. (2019). Unilateral and bilateral repetitive transcranial magnetic stimulation for treatment-resistant late-life depression. International Journal of Geriatric Psychiatry, 34(6), 822–827. https://doi.org/10.1002/gps.5091
Wager, T. D., & Atlas, L. Y. (2015). The neuroscience of placebo effects: Connecting context, learning and health. Nature Reviews Neuroscience, 16(7), 403–418. https://doi.org/10.1038/nrn3976
Walsh, B. T., Seidman, S. N., Sysko, R., & Gould, M. (2002). Placebo response in studies of major depression: Variable, substantial, and growing. Journal of the American Medical Association, 287(14), 1840–1847.
Wechsler, D. (1999). Wechsler Abbreviated Scale of Intelligence. Psychological Corporation.
Weintraub, S., Dikmen, S. S., Heaton, R. K., Tulsky, D. S., Zelazo, P. D., Bauer, P. J., Carlozzi, N. E., Slotkin, J., Blitz, D., Wallner-Allen, K., Fox, N. A., Beaumont, J. L., Mungas, D., Nowinski, C. J., Richler, J., Deocampo, J. A., Anderson, J. E., Manly, J. J., Borosh, B., & Gershon, R. C. (2013). Cognition assessment using the NIH toolbox. Neurology, 80(11 Supplement 3), S54–S64. https://doi.org/10.1212/WNL.0b013e3182872ded
Weissman, C. R., Blumberger, D. M., Brown, P. E., Isserles, M., Rajji, T. K., Downar, J., Mulsant, B. H., Fitzgerald, P. B., & Daskalakis, Z. J. (2018a). Bilateral repetitive transcranial magnetic stimulation decreases suicidal ideation in depression. Journal of Clinical Psychiatry, 79(3). https://doi.org/10.4088/JCP.17m11692
Weissman, C. R., Blumberger, D. M., Brown, P. E., Isserles, M., Rajji, T. K., Downar, J., Mulsant, B. H., Fitzgerald, P. B., & Daskalakis, Z. J. (2018b). Bilateral repetitive transcranial magnetic stimulation decreases suicidal ideation in depression. Journal of Clinical Psychiatry, 79(3). https://doi.org/10.4088/JCP.17m11692
Williams, K., Brignell, A., Randall, M., Silove, N., & Hazell, P. (2013). Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD). Cochrane Database Systematic Review, (8), CD004677. https://doi.org/10.1002/14651858.CD004677.pub3
Xu, Y., Zhang, Y., Zhao, D., Tian, Y., & Yuan, T. F. (2023). Growing placebo response in TMS treatment for depression: A meta-analysis of 27-year randomized sham-controlled trials. Nature Mental Health, 1(10), 792–809. https://doi.org/10.1038/s44220-023-00118-9
Zemplenyi, A., Jozwiak-Hagymasy, J., Kovacs, S., Erdosi, D., Boncz, I., Tenyi, T., Osvath, P., & Voros, V. (2022). Repetitive transcranial magnetic stimulation may be a cost-effective alternative to antidepressant therapy after two treatment failures in patients with major depressive disorder. Bmc Psychiatry, 22(1), 437. https://doi.org/10.1186/s12888-022-04078-9
Zheng, S., Kim, H., Salzman, E., Ankenman, K., & Bent, S. (2021). Improving social knowledge and skills among adolescents with autism: Systematic review and meta-analysis of UCLA PEERS® for adolescents. Journal of Autism and Developmental Disorders, 51(12), 4488–4503. https://doi.org/10.1007/s10803-021-04885-1
Author information
Authors and Affiliations
Contributions
E.J.B.: writing (original draft and review), data curation, data analysis, and project administration. D.L.G.: conceptualization, investigation, and manuscript review. S.W.W.: conceptualization, investigation, and manuscript review. T.L.: manuscript review and project administration. R.E.: study design and manuscript review. R.L.: statistical analysis. E.S.: investigation and manuscript review. G.W.: manuscript review and project administration. Y.L.: manuscript review and project administration. P.S.H.: statistical analysis. E.G.: data curation, and manuscript review. J.A.S.: study design and conceptualization. C.A.E.: conceptualization, investigation, and manuscript review. E.V.P.: conceptualization, investigation, data analysis, writing (original draft and review), and project administration.
We must note the unfortunate passing of one of our esteemed co-authors, Dr. John Sweeney. Dr. Sweeney contributed significantly to the conception and design of our study prior to his untimely death. We include him as a co-author to acknowledge his valuable contributions and to honor his commitment to advancing our understanding of autism and developmental disorders. The remaining authors have assumed responsibility for the final content of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest (either financial or non-financial interest) with the present submitted manuscript described by the Journal of Autism and Developmental Disorders policy. The present study was federally funded by the Cincinnati Children’s Hospital Research Foundation. We have opted to provide full disclosures of all authors’ external commitments for the editor’s review for transparency. The basis of our disclosure was made after review of after review of these activities.
The corresponding author, Dr. Pedapati reports no conflicts of interest and is supported by an NIH K23 Clinical Development Award (K23MH112936) and has received past research support from the American Academy of Child and Adolescent Psychiatry, and Cincinnati Children’s Hospital Research Foundation and textbook royalties from Springer. In the past he has consulted for Eccrine Systems, Forge Therapeutics, P&G, and Autism Speaks. The senior author Dr. Erickson is the principal investigator of the human portion of the NIH FXS Center. He has received compensation from Confluence Pharma, Novartis, F. Hoffmann-La Roche Ltd., Seaside Therapeutics, Riovant Sciences, Inc., Fulcrum Therapeutics, Forge Therapeutics, Neuren Pharmaceuticals Ltd., Alcobra Pharmaceuticals, Neurotrope, Zynerba Pharmaceuticals, Inc., and Ovid Therapeutics Inc. to consult on trial design or development strategies and/or conduct clinical trials in neurodevelopmental disorders. Dr. Erickson is additionally the inventor or co-inventor on several patents held by Cincinnati Children’s Hospital Medical Center and Indiana University School of Medicine describing methods of treatment of neurodevelopmental disorders. Dr. Wu receives research support from NIH, Quince Therapeutics, and Emalax Biosciences. Dr. Sweeney consults to VeraSci and has received support from NIH and Sichuan University. Dr. Horn has no conflicts of interest to disclose. Dr. Gilbert has received compensation for expert testimony for the U.S. National Vaccine Injury Compensation Program, through the Department of Health and Human Services. He has received payment for medical expert opinions through TeladocHealth International. He has served as a paid consultant for Emalex Biosciences. He has received research support from the United States National Institutes of Health (Tourette Syndrome, ADHD research) and the Department of Defense (Neurofibromatosis research). He has received salary compensation through Cincinnati Children’s for work as a clinical trial site investigator from Emalex (clinical trial, Tourette Syndrome), PTC Therapeutics (registry and clinical trial, Amino Acid Decarboxylase Deficiency). He has received book/publication royalties from Elsevier and Wolters Kluwer. Dr. Larsh has received research and travel support from the Tourette Association of America (TAA), as well as travel support and honoraria from the Child Neurology Society (CNS). Dr. Elmaghraby, Dr. Liu, and Dr. Smith have no disclosures of funding or external compensation.
Finally, we acknowledge that Dr. Craig Erickson serves as an Associate Editor for the Journal of Autism and Developmental Disorders.
Ethics Approval and Consent
This study was approved by the institutional review board at Cincinnati Children’s Hospital Medical Center (CCHMC) and registered with ClinicalTrials.gov (NCT01609374). Recruitment took place between November 2021 and November 2022 through clinician referrals, community flyers, emails, and clinics at a tertiary academic pediatric hospital. All participants provided written informed consent or assent for all study procedures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blank, E., Gilbert, D.L., Wu, S.W. et al. Accelerated Theta Burst Transcranial Magnetic Stimulation for Refractory Depression in Autism Spectrum Disorder. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06244-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s10803-024-06244-2