Abstract
Recognizing the multifaceted and chronic demands on families of children with Autism Spectrum Disorder (ASD) and challenges in providing care matched to need, we adapted the Psychosocial Assessment Tool (PAT), a brief caregiver-report screener of family psychosocial risk, for this population. Study methods included literature review, focus groups with providers, and feedback from caregivers. The PAT-ASD is consistent with the original PAT, with new items reflecting core behavioral manifestations of ASD and parent and family challenges associated with chronicity. The PAT-ASD was implemented in a four-month pilot and was completed online by 59% of families. Although further testing of its validity is necessary, the PAT-ASD is a promising means of assessing family psychosocial risk for families of children with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism Spectrum Disorder (ASD) is a complex heterogenous neurodevelopmental disorder typically present from early childhood. It is characterized by difficulties in social communication and social interaction and associated with an array of behavioral concerns that impact the entire family system and require a sustained and multifaceted approach to care (Lord et al., 2022). While caregivers usually have pre-existing concerns about their child’s development and behavior, the formal diagnosis of ASD can facilitate engagement with intervention programs and identify and specify the types of care and providers needed. Families typically must work with multiple providers, educational and social service systems, and therapists to access and orchestrate the necessary care. Unfortunately, this process can be fragmented and confusing, and may not provide an ideal match of services to need.
The ASD literature has generally highlighted the broad and challenging impact on the family of having one child (or more) with ASD. These challenges include behavioral difficulties, stigma, parenting stress, financial burdens, and necessary modifications to the family’s physical and social worlds, among others (Bonis, 2016; Hayes & Watson, 2013; Rogge & Janssen, 2019; Samsell et al., 2022). Specific stressors related to ASD include uncertainty about the etiology of ASD, limited access to needed therapies and services, stigma and fear associated with unusual and unexpected behaviors manifested by the person with ASD, physical aggression and agitation associated with ASD, and the chronicity of the disorder (Brewer, 2018; Davis & Carter, 2008; Woodgate et al., 2008). Although this is a heterogeneous group of families, common psychosocial issues include readjusting daily routines and family roles in order to best meet the needs of the child which can result in financial and emotional hardships (Navot et al., 2016). Caregivers may also experience helplessness and social isolation (Woodgate et al., 2008). Some parents are at risk for depression and/or other mental health issues (Benson & Karlof, 2009). Siblings of children are also at higher risk for a range of behavioral and quality of life issues compared to siblings of typically developing children (Garrido, Carballo, & Garcia-Retamaro, 2020; Raza et al., 2020). However, there is also increased recognition of the resilience of families and the importance of taking a broad social ecological view of coping and adjustment when considering families of children with ASD (Gunty, 2021). At the same time there is not, to our knowledge, screeners of family psychosocial risk that take into account the breadth of factors impacting families of children with ASD.
To facilitate timely and evidence-based delivery of care inclusive of all families, Kazak (2006) proposed a model grounded in public health to understand psychosocial risk in families in healthcare settings. The Pediatric Psychosocial Preventative Health Model (PPPHM; Fig. 1) is relevant to ASD and may help guide the delivery of psychosocial care to these families. The PPPHM outlines three levels of family risk. The largest number of families fall into.
Pediatric Psychosocial Preventative Health Model. Reproduced with permission from the Center for Healthcare Delivery Science (CHDS) at Nemours Children?s Health System ? 2022. All rights reserved. The PPPHM image may not be reproduced in any form for any purpose without the express written permission of CHDS. To obtain permission to use or reproduce the most recent version of the PPPHM, please contact CHDS at psychosocialassessmenttool@nemours.org.
the Universal level (the base of the pyramid). While challenged and experiencing some difficulties related to their child’s condition, these families are generally resilient and able to cope with and adapt to their child’s condition with basic support and education. A smaller sized group, families at the Targeted level, have increased vulnerability to distress; their adjustment is more tenuous and requires specific forms of intervention. At the tip of the pyramid is the smallest group of families, Clinical, who present with more complex and chronic problems, often needing urgent, robust intervention. Identifying levels of risk allows for the delivery of care matched to the needs of the family (Kazak et al., 2015). Systematic psychosocial risk screening of families is recommended to assure that subsequent care provided is inclusive of all families.
The level of risk on the PPPHM can be identified using the Psychosocial Assessment Tool (PAT), a brief caregiver report screener of psychosocial risk in pediatrics (Kazak et al., 2018). Based on a social ecological framework, the PAT identifies a family’s areas of risk and resilience across seven domains (subscales) - Family Structure and Resources, Social Support, Family/Caregiver Problems, Child (patient) Problems, Sibling Problems, Stress Reactions, and Family Beliefs. Item responses are classified as risk or no-risk, based on research and clinical evidence. Scores are calculated for each subscale by summing the number of risk responses and dividing by the total number of items on the subscale, generating scores between 0.00 and 1.00. The seven subscale scores are summed to determine a total risk score between 0.00 and 7.00. The total score maps on to the PPPHM with scores < 1.00 considered Universal; 1.00–2.00 considered Targeted; and > 2.00 considered Clinical. The PAT takes approximately 10 min to complete, is written at a 4th grade reading level, and is available as a web-based tool in English and Spanish.
The PAT originated in pediatric oncology where its strong internal consistency, convergent validity with other measures of psychosocial functioning, and predictive validity with regards to utilization of psychosocial services has been established (Alderfer et al., 2009; Kazak et al., 2018, 2020; Pai et al., 2008). However, there is strong evidence for the use of a generic version of the PAT, suitable for all pediatric chronic illness conditions, and for adaptations of the PAT to specific patient groups with the addition of items (modules) relevant to psychosocial risk in those specific populations (e.g., Cousino et al., 2018; Crerand et al., 2018; Ernst et al., 2018; Law et al., 2019; Phan et al., 2018; Verma et al., 2020). In light of the evidence for the use of the PAT in a broad range of families in pediatrics, an adaption for ASD seemed timely and feasible. We anticipated that the resulting measure, while specific to ASD, would be very similar to other versions of the PAT, thus consider it an adaptation of the PAT, not a new measure.
Psychosocial risk screening for families of children with ASD is important and highly relevant given the known chronic demands of ASD on parenting and family life, the ongoing involvement with multiple medical, educational, and behavioral providers and systems, and challenges in providing equitable care matched to the needs of families. Thus, the primary aim of the current paper is to describe the process of adapting the PAT for ASD (Study 1). The secondary aim is to illustrate initial steps towards implementing the PAT-ASD in clinical practice (Study 2). The methods and results for the two studies are presented separately below, after a brief method overview, then integrated for discussion purposes.
METHOD (Overview)
This research was conducted in a partnership between two programs located at a children’s hospital in the mid-Atlantic region of the United States - a comprehensive autism center (AC) and a child health research center (RC). The research includes two studies. Study 1 is the adaptation of the PAT for ASD (PAT-ASD) and has four steps. Study 2 is a pilot of a clinical implementation of the newly adapted PAT-ASD. All research procedures for the two studies were reviewed and approved by the Institutional Review Board (IRB). Study 2, as a clinical implementation of the PAT-ASD, was determined by our IRB to not meet the definition of human subjects research according to federal regulations.
Study 1: Adaptation of the PAT for ASD (PAT-ASD)
Method
A well-established process was used to adapt the PAT for ASD. First, a literature review was conducted to appraise whether the PAT was thorough in covering family psychosocial risk for families of children with ASD. Next, focus groups with ASD providers were conducted to create draft content for new or revised items for the PAT-ASD. Third, caregivers of children with ASD responded to the draft PAT-ASD and provided qualitative feedback. Potential new items and changes to existing items were identified at each of these steps and reviewed and integrated by the study team into the completed adaptation, the PAT-ASD.
Step 1. Literature Review (August-October 2018)
Literature searches were performed in PubMed and PsycInfo for articles published from 1998 through September 2018. A medical research librarian assisted with the selection of search terms and search process. Search terms included the following: “autism,” “asperger,” “psychosocial,” “family,” parent”, “caregiver,” “stress,” “distress,” “risk.” A wildcard symbol (*) was used to ensure variations of the keywords were retrieved. To be eligible for inclusion in the review, articles had to meet the following criteria: (1) written in English, (2) published in peer-reviewed journals, and (3) focused on psychosocial issues among families of children (≤ age 21) with ASD. Articles were excluded if they failed to meet any of the inclusion criteria. Members of the study team (MAS and APR) screened the titles and abstracts of identified papers and removed from review those deemed irrelevant. Full-text versions of the remaining articles were reviewed by members of the study team (MAS, APR, DTD); relevant findings were summarized to identify psychosocial risks, stressors, and unique challenges experienced by families of children with ASD. The identified material was mapped onto the domains represented by the PAT subscales. After careful review and discussion, the study team modified items and drafted new ones to ensure items captured the risks identified in the literature.
Step 2. Provider Focus Groups (October-November 2018)
All autism healthcare providers associated with the Autism Center (n = 20) were invited to participate in focus groups to provide their perspective on the unique stressors and challenges that families of children with ASD experience and to collect feedback on the first draft of the PAT-ASD. Participating healthcare providers gave written informed consent and completed a brief demographic form. During the focus groups, psychosocial risk was defined prior to the discussion. The groups were provided with the PAT and the newly modified/drafted items. They were then guided to discuss whether any items were irrelevant and if any important risks were not captured in the items. Possible new items were generated to capture missing risks.
Focus groups sessions were recorded and professionally transcribed and qualitative content analysis was used to derive findings (Elo & Kyngas, 2008). The subscales of the PAT were used as a basis for the coding scheme for the open-ended beginning portions of the discussion. Codes capturing suggested item modifications or additions were developed. Transcripts were independently coded by two members of the research team trained in qualitative coding (MAS, APR) who then compared and reconciled their coding to ensure accuracy.
Step 3. Caregiver Interviews (May 2019 – February 2020)
Purposive sampling based on child age, gender, race/ethnicity, comorbidities, time since diagnosis and family structure was used to identify a demographically diverse group of caregivers of children with ASD to complete and provide feedback on the PAT-ASD draft. Inclusion criteria were: (a) a parent/caregiver (≥ age 18) of a child (ages 1–17 years) diagnosed with ASD and seen at the AC; (b) fluent in English; and, (c) cognitively able to complete study measures and procedures. Caregivers with known severe psychopathology (e.g., psychotic disorder, schizophrenia) were not eligible.
Potential participants were identified by AC social workers and the research coordinators confirmed eligibility by reviewing medical records. Identified families (n = 65) were mailed a recruitment letter inviting their participation in a study to better understand the challenges faced by families of children with ASD and to learn ways to better support them. Telephone contact to answer questions, and schedule study participation for those interested was attempted for all 65 families. Of these, 38 could not be reached by phone after repeated attempts or due to inaccurate numbers. Of the 27 remaining, 22 indicated interest in participation and 5 declined.
A total of 12 caregivers provided informed consent and participated in the interview either by phone or in-person. Ten interested participants did not enroll in the study despite repeatedly scheduled interviews. Participants completed the draft PAT-ASD via REDCap (Harris et al., 2019) and provided feedback on the measure guided by a semi-structured interview guide. Questions were asked regarding the content, length, delivery, and perceived clinical utility of the PAT-ASD measure. All interviews were recorded, professionally transcribed, and independently coded by two members of the research team (MAS, APR). Codes captured participants’ perceptions of each item (e.g., positive, negative, unclear) and suggestions for new items. Additional codes were used to summarize general feedback about the PAT, including the length, timing of administration, and delivery of the measure. Disagreements in coding were discussed among the two coders until consensus was reached. Findings were summarized and presented to the full study team. Changes to existing items and the development of new items occurred via discussion and consensus of the full study team. The resulting modifications were then trialed with an additional three families, at which point saturation (no new recommended changes) was achieved.
Step 4. Finalizing the PAT (PAT-ASD) November 2018-July 2020
Steps 1–3 resulted in a PAT-ASD adaptation ready for pilot administration. A detailed accounting of the changes and the reasons for each change was recorded in an audit trail.
Results
The process of revising the PAT was iterative, reflecting the input of multiple groups of stakeholders. During each step, new items were added and existing items were modified. Some items that were added at one step were removed in subsequent steps. In presenting the results, we summarize key findings from each step and the magnitude of proposed changes rather than document the details of each iteration.
Step 1. Literature Review
The search yielded 327 articles with 258 remaining after duplicates were removed. Of these, 98 were deemed “ineligible” and removed after screening; 160 articles were included in the review. Findings related to risk and protective factors for families of children with ASD were summarized around 12 areas (Table 1). Social isolation, child safety, lack of respite care, complex daily management and routines, and chronicity and worry about the child’s future (job, relationships, housing, independent living, etc.) seemed particularly important and potentially unique for families of children with ASD. Based on the topics identified in the literature review, the study team drafted 21 new questions and modified 16 existing questions. These items spanned all of the subscales of the PAT. Examples of new items (by associated subscale) included: Family Structure/Resources – “Is your home equipped to meet all of your child’s current needs (e.g., safety gates/locks)?”; Social Support – “Are there people who make it more difficult for you to deal with ASD?”; Child Problems – “Does your child: bite, hit or kick others?” or, “Bang his/her head or bite self?” Examples of modified items included: inclusion of therapy, educational and home care bills to a question about money problems; and, concerns about finding time for appointments. The study team removed 4 items from the general PAT that were determined to be inapplicable or inappropriate (e.g., friendships, behaviors that were potential symptoms of ASD, child’s awareness of their ASD).
Step 2. Provider Focus Groups
Of the 20 providers invited to participate, 12 (60%) enrolled. Three focus groups were held, ranging in size from 3 to 5 participants. Across the groups, multiple professional disciplines were represented, including psychology, medicine, genetic counseling, social work, and child life. All participants were women. Their years of experience working with families of youth with ASD ranged: less than 5 years (n = 3); 5–10 years (n = 4); and, more than 10 years (n = 5).
Items on the PAT were discussed within each subscale and considered for retention, removal, or editing. Participants were reminded that screening tools are not thorough evaluation tools and need to be brief. Further, each item was evaluated as to whether/which responses would clearly indicate risk. Thirteen new items were added, 13 were modified, and 12 were removed. Examples of new items added based on the provider focus groups were (by subscale): Family Structure/Resources - frequency of appointments; Social Support - transition planning support; and, Child Problems - child getting upset by noises or changes in routines. Most of the modifications were minor wording changes.
Step 3. Caregiver Interviews
Twelve caregivers of children with ASD completed the draft PAT-ASD and participated in feedback interviews (Table 2). Overall, the PAT-ASD was well received. Many caregivers shared that the PAT-ASD was comprehensive in terms of potential risk areas. While some caregivers had not experienced topics captured in the PAT-ASD, they acknowledged that items could denote risk for other families. No new items were added based on the caregiver interviews. Two items were removed. Most changes involved revising words and phrases or specifying a time frame for greater item clarity. The online delivery and format of the PAT-ASD were also well received. The length of the PAT-ASD was found acceptable. Participants reported that it would be convenient to receive the PAT-ASD via email prior to seeing their healthcare provider so they could discuss the results during the appointment.
The PAT-ASD adaptation
The PAT-ASD has 38 new and modified items, with many being minor shifts in wording (see Table 3). The changes focus largely on adding questions reflecting core behavioral manifestations of ASD, items reflecting the chronicity of ASD, and items capturing parenting challenges associated with medical, behavioral, and educational treatments. Changes are most evident in the Child Subscale (4 items removed, 11 items added), but are also reflected in new items for Family Structure and Resources and Caregiver Efficacy. The team also identified eight items as high risk or “red flags.” Footnote 1
Study 2: Implementation Pilot of the PAT-ASD
Method
Implementation of the PAT-ASD for clinical use in the AC was pilot-tested for four months (October 2020 – January 2021). Due to restrictions associated with the COVID-19 pandemic, the pilot was delayed and changed from the originally planned in-person administration to remote online screening.
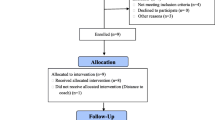
Participants
To focus the implementation effort and provide the most valuable clinical care information, all families with a child with ASD new to the AC and more than two weeks post autism diagnosis with a scheduled appointment during the project window were asked to complete the PAT-ASD. Eligible families were also required to have a caregiver capable of speaking and reading English, with access to an email account.
Procedure
AC staff identified eligible families by reviewing the clinic appointment calendar. Emails were sent inviting families to complete the PAT-ASD using a personalized REDCap link up to four weeks prior to their scheduled appointment. The email explained that their responses were part of clinical care and would help the clinical team because “learning about your family helps us better understand what you may need and how we might assist you.” Families received up to two reminders, no more than once weekly, to complete the PAT-ASD. Social workers at the AC received an automatic notification from REDCap when a family completed the PAT-ASD. They received the family’s responses and a Results Report that listed the family’s score on each of the subscales and the total score (see below). The report also listed endorsed “red flag” items, if any, and included PPPHM level and general recommendations for interventions based on the PPPHM level and consistent with current social work practices. For example, Universal interventions recommended included education about the psychosocial impact of ASD and its treatments, accessing services, and focusing on positive coping strategies and support-seeking. Targeted interventions recommended focus on providing resources and helping families meet housing, transportation and educational needs, and addressing specific behavioral and/or family problems. Clinical interventions include further mental health evaluation and more intensive services.
Internal validity and scoring
Consistent with the existing scoring metrics of the PAT, the research team determined how each new item would be scored as a binary (Yes/No) risk and assigned each item to an existing PAT subscale. Subscale scores were calculated as the number of items indicating risk divided by the total number of items on the subscale. Total scores were calculated by summing subscale scores. The range for each subscale score was 0.00–1.00 and 1.00–7.00 for the total score. Internal validity (Kuder Richardson 20 [KR-20] coefficients were calculated for the total score and the subscales. These scores were included in the reports shared with the clinical team.
Data analysis
Implementation was measured as the number of families that completed the PAT-ASD divided by the number that were provided a link to complete it. We calculated descriptive statistics (means, standard deviations, ranges) for the PAT-ASD total and subscale scores and tallied the distribution of total scores against the PPPHM framework (< 1.00, Universal; 1.00–2.00, Targeted; > 2.00 Clinical). Mindful of the new items on the PAT-ASD and the implications of these for scoring the screener, we examined distributions of responses for each item to identify which had discriminative power to identify families at risk in this population.
Results
Implementation
Caregivers of new patients scheduled for an appointment at the AC received requests to complete the PAT-ASD (n = 137). Of these, 85 caregivers accessed the PAT-ASD (62%). Four PAT-ASDs were incomplete, rendering a sample of 81 completed, 59.1% of the total. The PAT-ASD was most frequently completed by mothers or other female caregivers (91.4%). Most were white (72.8%), non-Hispanic (87.7%), and married/partnered (71.6%).Footnote 2 Most families (75.3%) had other children in the home, and nearly a third of those (29.5%) had another child with ASD (Table 4).
Internal validity
Internal consistency for the PAT-ASD total score was strong (KR20 = 0.84). KR20s for the subscales were mostly acceptable to good (Table 5). The sample scores fell into the PPPHM categories as follows: Universal − 27.2%; Targeted − 48.1%; and Clinical 24.7%. As anticipated, the Child Problems subscale was elevated due to the prevalence of behavioral concerns in this population.
Genearal Discussion
Family psychosocial risk is a highly relevant and clinically important issue for families of children with ASD and developing a means by which risk can be identified and integrated into a clinical pathway is essential in comprehensive ASD care (Lord et al., 2022). The PAT-ASD is a brief caregiver report screener of family psychosocial risk that is promising for early identification of multiple risks across the child and family’s social ecology. It can facilitate the development and delivery of evidence-based psychosocial care for families of children with ASD, matched to the needs of each child and family. Although the PAT is used across a range of pediatric health conditions, prior to the current adaptation it had not been used with families of children with ASD and their providers. This adaptation is specific to the risks experienced by families of children with ASD yet is a relatively minor modification of the PAT. New items address key experiences of families related to child behavior and chronicity.
Recognizing that ASD has distinct behavioral manifestations and demands on the entire family system, we applied a detailed multi-step process used previously in other adaptations in order to assure appropriateness for families of children with ASD. This rigorous process begins with a review of existing literature, and the input of provider and family stakeholders to closely and inclusively evaluate whether the existing questions and scales are appropriate. Then new items are added as needed to reflect important themes from the literature, and from the “lived experiences” of both families and providers.
Because the adaptation started from a “generic” PAT screener, many of the existing items were relevant, and the additional items increased relevance for families of children with ASD. The new items focused on two areas: (1) child behaviors, assuring that items reflected frequent and broad ranging behaviors common to families of children with ASD; and (2) chronicity of ASD and ASD care, and the risks associated with the long-term demands placed on families across the life-span.
Based on data from Study 2, the PAT-ASD had strong internal consistency. The distribution of scores across the PPPHM was instructive. Nearly half of the sample scored in the Targeted tier of the PPPHM, with approximately one-quarter in the Universal and Clinical levels.
As a newly created instrument, it will be critical to evaluate the PAT-ASD in a larger and more diverse sample of families, using established measures to conduct analyses of its validity. This will also allow for determination of scoring metrics specific to the PAT-ASD. The demographics of the sample for this pilot study is a limitation of the research, as it was predominantly Caucasian, although representative of this setting. A larger scale study will allow for refinement of the scoring for the PAT-ASD, including validation of its scores with other measures of ASD outcomes, with clinicians’ impressions of the patient and family. Understanding how family psychosocial risk screening can also identify needs of families with more than one child with ASD and how repeated administrations may be helpful, given the chronicity of ASD, are important additional future areas for investigation.
Understanding how the PAT-ASD may be implemented in clinical practice is essential. Our pilot implementation showed that the PAT-ASD can be administered to families in an online survey format. The ~ 60% completion rate is acceptable given the circumstances of the COVID-19 pandemic and absence of any specific strategies to evaluate and improve uptake. It suggests the acceptability of the family psychosocial risk screening to families new to the diagnosis and its treatments. An important consideration for families of individuals with ASD is whether the screener can be used with parents of older individuals (over the age of 18). Although the PAT was originally developed for use in families of minor children, our experience is that it can be used by families of older children who are living at home and dependent upon their family, although this is an important area to address in future research.
With further research and establishment of the psychometric properties of the PAT-ASD, use of this screener may be seen as the first step in a clinical pathway for how the data can be used in clinical care, based on PPPHM level For example, families scoring at the Universal level may benefit from social workers identifying resources associated with risks. At the Targeted level social workers may initiate further assessment and determine if/what intervention is needed. If the family’s score were in the Clinical range and/or if they endorsed Red Flag Item(s), providers might consider following up with the family (either by phone or in-person) to discuss any immediate risk.
In conclusion, the PAT- ASD offers a brief and user friendly evidence based approach by which the social ecology of the family can be understood, with the goal of facilitating multidisciplinary care delivery based upon specific risks.
Notes
The red flag items were those related to suicidality, having been the victim of crime, abuse or domestic violence, or reporting an unstable living arrangement. Other red flags included a serious medical problem in caregiver(s) and a child or sibling who wanders. Two family beliefs, “This is a disaster” and “It’s my fault my child has ASD” were also categorized as red flags.
Using data from the electronic health record at our institution, the race/ethnicity, and patient age and gender are comparable to the broader patient population treated at this AC.
References
Alderfer, M., Mougianis, I., Barakat, L., Beele, D., DiTaranto, S., Hwang, W. T., Reilly, A., & Kazak, A. (2009). Family psychosocial risk, distress and service utilization in pediatric cancer: Predictive validity of the Psychosocial Assessment Tool. Cancer, 115, 4339–4349
Benson, P. R., & Karlof, K. L. (2009). Anger, stress proliferation, and depressed mood amongparents of children with ASD: A longitudinal replication. Journal of autism and developmental disorders, 39(2), 350–362
Bonis, S. (2016). Stress and parents of children with autism: A review. Issues in Mental Health Nursing, 37, 153–163
Brewer, A. (2018). “We were on our own”: Mothers’ experiences navigating the fragmented system of professional care for autism. Social Science & Medicine, 215, 61–68. https://doi.org/10.1016/j.socscimed.2018.08.039
Crerand, C. E., Kapa, H. M., Litteral, J., Pearson, G. D., Eastman, K., & Kirschner, R. E. (2018). Identifying psychosocial risk factors among families of children with craniofacial conditions: Validation of the psychosocial assessment tool–craniofacial version. The Cleft Palate-Craniofacial Journal, 55(4), 536–545. doi: https://doi.org/10.1177/1055665617748010
Cousino, M., Schumacher, J., Rea, K., Eder, S., Zamberlin, M., Jordan, J., & Fredericks, E. (2018). Psychosocial functioning in pediatric heart transplant recipients and their families. Pediatric transplantation. e13110
Davis, N. O., & Carter, A. S. (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of autsim and developmental disorders, 38(7), 1278
Elo, S., & Kyngas, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi: https://doi.org/10.1111/j.1365-2648.2007.04569.x
Ernst, M., Gardner, M., Mara, C., Delot, E., Fechner, P., Fox, M., Rutter, M., Speiser, P., Vilain, E., Weidler, E., Sandberg, D., & The DSD-Translational Research Network Leadership Group and Psychosocial Workgroup. (2018). and. Psychosocial screening in disorders/differences in sex development: Psychometric evaluation of the Psychosocial Assessment Tool (PAT). Hormone Research in Pediatrics, DOI: https://doi.org/10.1159/000496114
Gunty, A. (2021). Rethinking resilience in families of chidlren with autism spectrum disorders. Couple and Family Psychology: Research and Practice, 10, 87–102
Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O’Neal, L., & REDCap Consortium. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(3),629–642. https://doi.org/10.1007/s10803-012-1604-y
Kazak, A. E. (2006). Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice, and collaboration in pediatric family systems medicine. Families Systems & Health, 24(4), 381–395. doi: https://doi.org/10.1037/1091-7527.24.4.381
Kazak, A. E., Chen, F. F., Hwang, W. T., Askins, M. A., Vega, G., Kolb, E. A., Reilly, A., & Barakat, L. P. (2020). Stability and change in family psychosocial risk over 6 months in pediatric cancer and its association with medical and psychosocial healthcare utilization. Pediatric Blood & Cancer, 67(2), e28051. doi: https://doi.org/10.1002/pbc.28051
Kazak, A. E., Hwang, W. T., Chen, F. F., Askins, M. A., Carlson, O., Argueta-Ortiz, F., & Barakat, L. P. (2018). Screening for family psychosocial risk in pediatric cancer: Validation of the Psychosocial Assessment Tool (PAT) Version 3. Journal of Pediatric Psychology, 43(7), 737–748. doi: https://doi.org/10.1093/jpepsy/jsy012
Kazak, A. E., Schneider, S., Didonato, S., & Pai, A. L. (2015). Family psychosocial risk screening guided by the Pediatric Psychosocial Preventative Health Model (PPPHM) using the Psychosocial Assessment Tool (PAT). Acta Oncologica, 54(5), 574–580. doi: https://doi.org/10.3109/0284186X.2014.995774
Law, E. F., Powers, S. W., Blume, H., & Palermo, T. M. (2019). Screening Family and Psychosocial risk in pediatric migraine and tension-type headache: Validation of the Psychosocial Assessment Tool (PAT). Headache: The Journal of Head and Face Pain, 59(9), 1516–1529. doi: https://doi.org/10.1111/head.13599
Lord, C., et al. (2022). The Lancet Commission on the future of care and clinical resarch in autism. The Lancet, 399, 271–334
Navot, N., Jorgenson, A. G., Stoep, V., Toth, A., K., & Webb, S. J. (2016). Family planning and family vision in mothers after diagnosis of a child with autism spectrum disorder. Autism, 20(5), 605–615
Pai, A. L., Patiño-Fernández, A. M., McSherry, M., Beele, D., Alderfer, M. A., Reilly, A. T., Hwang, W. T., & Kazak, A. E. (2008). The Psychosocial Assessment Tool (PAT2.0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. Journal of Pediatric Psychology, 33(1), 50–62. doi: https://doi.org/10.1093/jpepsy/jsm053
Phan, T. L., Chen, F., Pinto, T., Cox, A., Robbins, C., J., & Kazak, A. (2018). Impact of psychosocial risk on attrition and weight outcomes among families seeking treatment for obesity. Journal of Pediatrics, 198, 110–116
Raza, S., Sacrey, L. A. R., Zwaigenbaum, L., et al. (2020). Relationship Between Early Social-Emotional Behavior and Autism Spectrum Disorder: A High-Risk Sibling Study. Journal of Autism and Developmental Disorders, 50, 2527–2539. https://doi.org/10.1007/s10803-019-03977-3
Rogge, N., & Janssen, J. (2019). The Economic costs of autism spectrum disorder: A Literature review. Journal of Autism and Developmental Disorders, 49(7), 2873–2900. https://doi.org/10.1007/s10803-019-04014-z
Samsell, B., Lothman, K., Samsell, E., & Ideiski, R. (2022). Parents’ experiences of caring for a child with Autism Spectrum Disorder in the United States: A systematic review and metasynthesis of qualitative evidence. Families Systems and Health, 40, 93–104
Verma, R., Mehdian, Y., Sheth, N., et al. (2020). Screening for caregiver psychosocial risk in children with medical complexity: a cross-sectional study. BMJ Paediatrics Open, 4, e000671. doi:https://doi.org/10.1136/bmjpo-2020-000671
Woodgate, R. L., Ateah, C., & Secco, L. (2008). Living in a world of our own: The experience of parents who have a child with autism. Qualitative health research, 18(8), 1075–1083
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors are at Nemours Children’s Health, Wilmington, DE. Drs. Kazak and Alderfer are also faculty at the Sidney Kimmel Medical School of Thomas Jefferson University, Philadelphia, PA. Correspondence may be sent to Dr. Kazak on behalf of all the authors at: Center for Healthcare Delivery Science, 1701 Rockland Road, Suite 160, Wilmington, DE. 19803. 302-298-7456 (v), 302-651-6899 (f), anne.kazak@nemours.org.
We thank the multidisciplinary staff of the Swank Autism Center for their participation in the focus groups, Emily Bernabe, Ph.D., Anne Meduri, M.D., Taylor Johnson, MSN, RN, CPNP-PC, PMHS, and Amy Wellings, B.A., B.S.N., R.N. for assisting with implementation and Brianna Smith for responding to families identified with risks.
This research was funded by a grant from the Theresa and Frank Caplan Foundation with additional support from the Swank Autism Center at Nemours Children’s Health-Delaware, and the Nemours Center for Healthcare Delivery Science at Nemours Children’s Health. The authors have no conflicts of interest to report.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kazak, A., Ramirez, A.P., Scialla, M.A. et al. Adaptation and pilot implementation of the Psychosocial Assessment Tool for Autism Spectrum Disorders (PAT-ASD). J Autism Dev Disord 53, 4308–4317 (2023). https://doi.org/10.1007/s10803-022-05713-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05713-w